Abstract
Objective
To examine the longitudinal course of pediatric bipolar (BP)-I disorder in youth transitioning from childhood into adolescence.
Methods
We conducted a four-year prospective follow-up study of 78 youth with BP-I disorder 6-17 years old at ascertainment followed up into adolescent years (13.4±3.9 years). All subjects were comprehensively assessed with structured diagnostic interviews, neuropsychological testing, psychosocial, educational and treatment history assessments. BP disorder was considered persistent if subjects met full criteria for DSM-IV BP-I disorder at follow-up.
Results
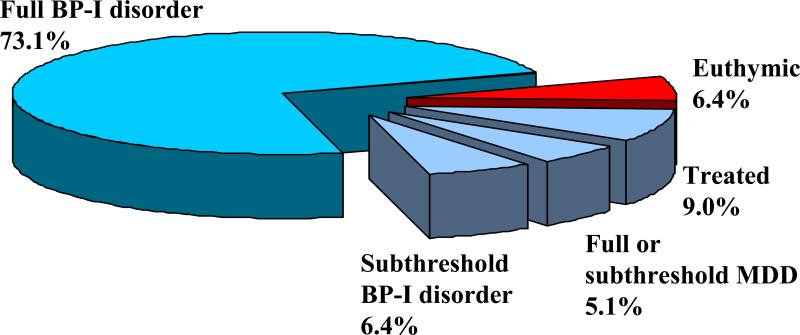
Of 78 BP-I participating youth subjects, 57 (73.1%), continued to meet full diagnostic criteria for BP-I Disorder. Of those with a non-persistent course, only 6.4% (n=5) were euthymic (i.e., syndromatic and symptomatic remission) at the 4-year follow-up and were not receiving pharmacotherapy for the disorder. The other non-persistent cases either continued to have subthreshold BP-I disorder (n=5, 6.4%), met full (n=3, 3.8%) or subthreshold (n=1, 1.3%) criteria for major depression, or were euthymic but were treated for the disorder (n=7, 9.0%). Full persistence was associated with higher rates of major depression and disruptive behavior disorders at the follow-up assessment and higher use of stimulant medicines at the baseline assessment. Non-Peristent BP-I was also characterized by high levels of dysfunction and morbidity.
Conclusions
This four-year follow-up shows that the majority of BP-I disorder youth continue to experience persistent disorder into their mid and late adolescent years and its persistence is associated with high levels of morbidity and disability. Persistence of subsyndromal forms of bipolar disorder was also associated with dysfunction and morbidity.
Keywords: bipolar disorder, children, adolescent, course, follow-up
1. Introduction
A converging body of research supports the validity of pediatric bipolar (BP)-I disorder including unique clinical features (Biederman 1995; Biederman et al. 2005a; Birmaher et al. 2006; Findling et al. 2001; Geller 1994; Geller & Cook 2000a; Geller et al. 2001; Geller et al. 2002a; Geller & Tillman 2005; Geller et al. 2008; Geller et al. 2004; Geller et al. 2000b; Geller et al. 2002b; Wozniak 2003; Wozniak et al. 1995; Wozniak et al. 2005), familial transmission (Faraone et al. 2003; Findling et al. 2001; Geller et al. 2006), selective treatment response to antimanic agents (Biederman et al. 2008; Biederman et al. 2005b; Biederman et al. 2007; Kafantaris et al. 2004; Pavuluri et al. 2004; Tohen et al. 2007), and characteristic neuroimaging findings (Chang et al. 2004; Chang et al. 2005a; Chang et al. 2005b; Leibenluft et al. 2007; Moore et al. 2007; Pavuluri et al. 2007). Children and adolescents with bipolar disorder have a disabling and severe clinical picture that fully satisfies the diagnostic criteria for bipolar-I disorder as defined by DSM-IV (Birmaher et al. 2006; Wozniak et al. 1995; Wozniak et al. 2005).
In parallel to pediatric studies, an emerging literature in adults documents that a majority of adults with bipolar-I disorder have an onset of their disorder in childhood and adolescence and a full third of them have an onset before the age of 12 years (Nierenberg et al. 2005; Perlis et al. 2009). Adults with early onset bipolar disorder have clinical features very similar to those observed in youth with bipolar disorder including high rates of psychiatric comorbidity with ADHD, antisocial and anxiety disorders as well as high levels of functional impairment and mixed states. Furthermore, findings from the National Comorbidity Replication study (Kessler et al. 2006) document that adults with bipolar-I disorder in the community have a significantly increased risk for ADHD and vice versa. Despite these compelling findings, questions remain as to the validity of pediatric bipolar disorder.
As proposed by Robins and Guze (1970), a cornerstone in establishing the validity of a psychiatric disorder is for the disorder to have a unique course. Yet, only a limited literature has addressed the longitudinal course of pediatric bipolar disorder. In one of a very few studies of its kind, Geller et al. (2008) found that 44% of children with BP-I continued to suffer from the full disorder by the age of 18 years. While this study represents the first major report on the long-term follow up of pediatric subjects with bipolar-I disorder, the study restricted recruitment to children meeting a phenotype based on the presence of euphoria or grandiosity, excluding other children who may have otherwise fully met DSM-IV bipolar-I disorder criteria. Unmodified DSM IV criteria requires either a week or longer of irritability or euphoria along with concurrent criterion B symptoms (any 3 if mood is euphoric, any 4 if mood is irritable). Birmaher et al. (2009) followed- up 413 youth with bipolar I, II and NOS disorders over a four year period and reported a chronic course with high rates of relapse and recovery (63% and 82%, respectively) as well as high rates of persistence of subsyndromal presentations and episodes of depression.
As proposed by Keck et al. (1998) delineating different patterns of remission in psychiatric samples is of high scientific and clinical interest. These authors proposed three levels of remission for psychiatric disorders: syndromatic remission (or loss of full diagnostic status), symptomatic remission (or loss of partial diagnostic status) and functional remission (full recovery, including functioning well). For bipolar disorder, the additional component of recovery includes remission from syndromes and symptoms of depression as well as mania, as many subjects with bipolar disorder may remit from mania, but continue to suffer from impairing states of depression. Thus, questions remain as to whether children who no longer satisfy full diagnostic criteria for BP-I disorder should be considered remitters despite manifesting persistent symptoms of subsyndromal mania or depression. Since these are frequently seen in adults with BP-I disorder, a comprehensive assessment of the course of pediatric BP-I needs to address these outcomes.
A better understanding of the course of pediatric BP-I disorder is of high clinical, public health and scientific importance. Understanding the degree to which pediatric BP-I persists in a naturalistic sample should help clinicians in the community understand the course of the disorder and whether its level of severity and persistence warrants early and aggressive treatment. Such knowledge should also encourage clinicians to carefully follow-up affected children with BP disorder and be mindful of the residual manifestations of the symptomatic picture over time. As described by Lewinsohn et al. (1995) in adolescent subjects and by Merikangas et al. (2007) in adult subjects, even subsyndromal forms of BP disorder are highly morbid, associated with significant dysfunction and merit clinical attention.
The main aim of the present study was to evaluate the longitudinal course of DSM-IV pediatric bipolar I (BP-I) disorder attending to different definitions of remission at follow-up including persistence of the full diagnosis of BP-I disorder as well as the presence of subsyndromal mania and depression. To this end, we conducted a four year longitudinal follow-up study of a large sample of systematically ascertained children and adolescents of both sexes fully satisfying DSM-IV diagnostic criteria for BP-I disorder based on clinical assessment and structured diagnostic interview, followed prospectively onto adolescence. We hypothesized that pediatric BP-I disorder would be a persistent disorder. To the best of our knowledge this study represents one of only three comprehensive longitudinal studies that examined the course of pediatric bipolar disorder. While two previous longitudinal studies have addressed the longitudinal course of bipolar disorder, ours differs from Geller et al. (2008) in that it selects subjects based on unmodified DSM-IV criteria and from Birmaher et al. (2009) in that it attends to both syndromatic and symptomatic remission of both mania and depression, as well as stratifies syndromatic remitters into those who are treated versus untreated.
2. Methods
2.1. Subjects
We recruited 105 youth in a longitudinal follow-up study of BP-I disorder. The participants were children and adolescents 6-17 years of age of both sexes meeting full diagnostic criteria for bipolar (BP)-I disorder on structured diagnostic interview. All BP-I diagnoses were corroborated by clinical assessment by the lead author (JW), a board certified child and adolescent psychiatrist with expertise in the diagnosis of pediatric onset bipolar disorder. The clinical assessment was 2 hours in length and included an interview with the parents and the child together and separately. The interview included history gathering, as well as a direct mental status exam of the child. In addition, the clinician completed the Young Mania Rating Scale. All study procedures were reviewed and approved by the subcommittee for human subjects of our institution. All subjects’ parents or guardians signed written informed consent forms and children older than 7 years of age signed written assent forms.
2.2 Ascertainment Methods
Potential BP-I disorder probands were ascertained from the Clinical and Research program in Pediatric Psychopharmacology at the Massachusetts General Hospital, referrals from local clinicians or self-referral in response to advertisements. Subjects were administered a phone screen reviewing symptoms of DSM-IV BP-I and, if criteria were met, were scheduled for a face-to- face structured diagnostic interview (described below). In addition to the structured diagnostic interview the lead author (JW) conducted a clinical interview of each potential BP-I proband and his or her parent(s) to confirm the clinical diagnosis of bipolar I disorder. We documented agreement in 97% of cases in interim analyses of the first 69 children assessed with this procedure (Wozniak 2003). To be included subjects must have had a full lifetime DSM-IV diagnosis of BP-I disorder plus active symptoms of the disorder at the time of study entry. Excluded were subjects with organic brain and mental retardation (IQ<70). Subjects were excluded at baseline if their bipolar disorder was due solely to a medication reaction. No social class strata or ethnic group were excluded.
2.3. Diagnostic Procedures
Psychiatric assessments of subjects younger than 18 years were made with the KSADS-E (Epidemiologic Version) (Orvaschel 1994) and assessments of those over age 18 were made with the Structured Clinical Interview for DSM-IV (SCID) (First et al. 1997), supplemented with modules from the KSADS-E to cover childhood disorders. Diagnoses were based on independent interviews with mothers and direct interviews with children older than 12 years of age. Data were combined such that endorsement of a diagnosis by either reporter resulted in a positive diagnosis. As more than one family assessment study was ongoing at the time of the baseline assessments, the clinical assessments at baseline were performed by raters blind to the study assignment and whether the subject was a proband or sibling. The follow-up assessments were performed by different raters.
Extensively trained and supervised psychometricians with undergraduate degrees in psychology conducted all interviews. This training involved several weeks of classroom instruction of interview mechanics, diagnostic criteria and coding algorithms. They also observed interviews by experienced raters and clinicians and were observed while conducting interviews during the final training period. They subsequently conducted at least six practice (non-study) interviews and at least three study interviews while being observed by senior interviewers. Trainees were not permitted to conduct interviews independently until they executed at least three interviews that achieved perfect diagnostic agreement with an observing senior interviewer. In addition, all diagnoses were reviewed by a sign-off committee of experienced board certified child and adolescent psychiatrists or clinical psychologists. The committee members were blind to the subjects’ ascertainment group, ascertainment site, and data collected from other family members. We computed kappa coefficients of agreement by having experienced clinicians diagnose subjects from audio taped interviews made by the assessment staff. Based on 500 interviews, the median kappa coefficient between raters and clinicians was 0.99 and for individual diagnoses was: ADHD (0.88), conduct disorder (1.0), major depression (1.0), mania (0.95), separation anxiety (1.0), agoraphobia (1.0), panic (.95), substance use disorder (1.0), and tics/Tourette's (0.89). The median agreement between individual clinicians and the clinical review committee chaired by the PI was 0.87 and for individual diagnoses was: ADHD (1.0), conduct disorder (1.0), major depression (1.0), mania (0.78), separation anxiety (0.89), agoraphobia (.80), panic (.77), substance use disorder (1.0), and tics/Tourette's (0.68).
In accordance with the KSADS-E, children were diagnosed with BP-I disorder according to DSM-IV criteria. The DSM-IV requires subjects to meet criterion A for a distinct period of extreme and persistently elevated, expansive or irritable mood lasting at least one week, plus criterion B, manifested by three (four if the mood is irritable only) of seven symptoms during the period of mood disturbance. To ensure that the B criterion symptoms were concurrent with the criterion A mood disturbance, subjects were directed to focus on the worst or most impairing episode of mood disturbance while being assessed for the presence of the confirmatory B criterion symptoms. That is, the subject was asked to consider the time during which the screen was at its worst for the purposes of determining whether the remaining symptoms were also evident at the same time as the screening item. The onset of first episode, the number of episodes, the offset of the last episode, and the total duration of the illness was also recorded. Any subject meeting criteria for BP-II or BP-NOS was not included in this study. To gauge a distinct episode our interviewers asked for ‘a distinct period (of at least one week) of extreme and persistently elevated, expansive or irritable mood and further required that the irritability endorsed in this module was ‘super’ and ‘extreme.’ To meet for a subthreshold diagnosis of mania, a child must have met criterion A for a period of four days or longer, and/or have at least two (three if the mood is irritable only) of the seven criterion B symptoms, and associated impairment.
Socioeconomic status (SES) was measured using the 5-point Hollingshead scale (Hollingshead 1975). To measure overall current (last month) and lifetime functioning, we used the DSM-IV Global Assessment of Functioning (GAF) (Orvaschel 1994). Social and environmental characteristics of families were measured with the Moos Family Environment Scale (Moos & Moos 1974). Additionally, questions regarding academic functioning (tutoring, repeated grades, placement in a special class), adverse perinatal experiences, and treatment history were asked during the interview. Medication variables included anticonvulsants (lamotrigine, tiagabine, topiramate, zonisamide, phenobarbital, gabapentin, phenytoin, oxcarbazepine), typical antipsychotics (haloperidol, loxapine, molindone, perphenazine, pimozide, thioridazine, trifluoperazine), atypical antipsychotics (clozapine, olanzapine, quetiapine, risperidone, ziprasidone, aripiprazole), traditional mood stabilizers (carbamazepine, divalproex, lithium carbonate), antidepressants (tricyclics, buproprion, SSRIs, mirtazapine, nefazodone, MAOIs, trazodone, venlafaxine), and stimulants.
2.4. Neuropsychological Assessments
The neuropsychological battery assessed domains of cognitive functioning including tests of executive functions, learning, and memory. The tests administered in a fixed order were: 1) the Rey-Osterrieth Complex Figure Copy(Rey 1941); 2) WISC- III (Wechsler 1991) Vocabulary, Digit Span; and Symbol Search; 3) the Rey-Osterrieth Recall; 4) WISC- III Block Design, Arithmetic and Coding/Digit Symbol subtests ; 5) the auditory CPT (Seidman et al. 1998); 6) the total words learned on the California Verbal Learning Test-C (Delis et al. 1994); 7) the computerized Wisconsin Card Sorting Test (WCST) (Heaton et al. 1993); and 8) the Stroop Test (Golden 1978). The test battery usually took approximately two hours on one day to administer. Rest periods were given during the testing sessions as needed.
The testers were recent college graduates who had undergraduate degrees in psychology; they were trained in neuropsychological assessment by a licensed neuropsychologist. Testers were trained to maintain the interest of subjects with positive rapport and sensitivity to fatigue. The psychometricians administering the tests are trained to administer the testing in an exact format without any variation from the written administration. They do not administer any tests that need interpretation, they do not interpret material and every subtest is taped and double-checked for precise administration and scoring.
2.5. Statistical Analysis
Persistence/remission of subjects returning for the 4-year follow-up was described as syndromatic persistence (full BP-I disorder criteria met in the past year), symptomatic persistence (subthreshold BP-I disorder or full or subthreshold major depression in the past year), syndromatic and symptomatic remission but treated for BP-I disorder in the past year, or syndromatic and symptomatic remission and not treated for the disorder in the past year. Statistical comparisons were made between subjects with syndromatic persistence (Persistent BP-I) and syndromatic remission (Non-Persistent BP-I) using two-sample t-tests (for continuous variables) or Pearson's chi-square (for categorical variables). All analyses were two tailed and statistical significance was defined at the 5% level. One-year prevalence was defined as positive if the subject met criteria for a given disorder in the year prior to the time of the 4-year follow-up.
3. Results
Of the 105 youth with BP-I disorder enrolled in a longitudinal follow-up study, 78 (74%) returned for follow-up assessments 4 years later (mean=3.6 years, standard deviation=1.2). There were no differences in baseline age (10.5±3.2 vs 9.8±3.5, p=0.36), sex (76% male vs 89% male, p=0.14) or functional impairment at baseline (GAF score 40.2±5.9 vs 38.8±6.5, p=0.30) between the probands who were followed and lost to follow-up, respectively. However, there was a statistically significant difference in socio-economic status (1.6±0.8 vs 2.4±1.2, p<0.001) and age at onset of bipolar disorder (4.9±3.5 vs 6.7±3.5 years of age, p=0.03) with the returning probands having an earlier age at onset and coming from a higher SES bracket. At follow-up, returning subjects were 13.4±3.9 years of age and had an average age at bipolar onset of 4.9±3.5 years. The duration of bipolar disorder at follow-up was 7.6±4.0 years with an average of 66.0±118.0 episodes of mania.
As shown in Figure 1, examination of findings at the follow-up assessment, only 6.4% (n=5) of children with BP-I disorder at baseline were euthymic (i.e., syndromatic and symptomatic remission) during the last year at the 4-year follow-up onto mid adolescence years and were not receiving pharmacotherapy for the disorder. The other 93.6% (n=73) of subjects either continued to meet full diagnostic criteria for BP-I Disorder (n=57, 73.1%), continued to have persistent subthreshold BP-I disorder (n=5, 6.4%) or full (n=3, 3.8%) or subthreshold major depression (n=1, 1.3%), or were euthymic but were treated for the disorder (n=7, 9.0%). Because of the small number of fully remitting cases (n=5), comparisons were made between subjects that continued to meet full diagnostic criteria for BP-I disorder (Persistent BP-I, n=57) and subjects with partial or full remission of BP-I disorder (Non-Persistent BP-I, n=21). Specifically, the Persistent BP-I group had syndromatic persistence (full diagnostic status) of BP-I disorder at some point in the year prior to their follow-up assessment. The Non-Persistent BP-I group was composed of subjects with syndromatic remission but symptomatic persistence in the past year (43%, n=9) and subjects with syndromatic and symptomatic remission in the past year (57%, n=7 treated, n=5 not treated).
Figure 1.
Persistence of DSM-IV BP-I in youth at 4-year Follow-up
As shown in Table 1, Persistent BP-I and Non-Persistent BP-I groups did not differ on age, gender, ethnicity, or socioeconomic status (Table 1). At baseline, the Persistent BP-I group had on average a two year longer duration of BP-I disorder compared to the Non-Persistent BP-I group (8.1 ± 3.6 vs. 6.2 ± 4.8, z=-2.34, p=0.02). There were no significant differences between the groups on age of onset (Non-Persistent=5.1 ± 3.5, Persistent=4.9 ± 3.5, z=0.40, p=0.69) or number of episodes (Non-Persistent=65.3 ± 110.0, Persistent=66.3 ± 121.8, z=0.08, p=0.93). At the 4-year follow-up, the Persistent BP-I group had a significantly more impaired current (last month) GAF score (49.2 ± 7.2 vs. 56.0 ± 7.0, t(75)=3.66, p<0.001). The Persistent and Non-Persistent BP-I groups did not significantly differ on a family history of BP-I disorder (28% versus 33%, respectively, χ2(1)=0.20, p=0.65) or major depression (81% versus 67%, respectively, χ2(1)=1.70, p=0.19).
Table 1.
Demographics and characteristics of bipolar disorder
| Non-Persistent BP-I (N=21) | Persistent BP-I (N=57) | Test statistic | p-value | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Male | 17 (81) | 43 (75) | χ2(1)=0.26 | 0.61 |
| Caucasian | 20 (95) | 56 (98) | χ2(1)=0.56 | 0.46 |
| Mean ± SD | Mean ± SD | |||
|---|---|---|---|---|
| Age at baseline | 10.0 ± 3.5 | 9.7 ± 3.6 | t(76)=0.36 | 0.72 |
| Age at follow-up | 13.9 ± 4.0 | 13.3 ± 3.9 | t(76)=0.64 | 0.52 |
| Socioeconomic status | 1.8 ± 1.0 | 1.8 ± 1.0 | z=-0.10 | 0.92 |
| Onset | 5.1 ± 3.5 | 4.9 ± 3.5 | z=0.40 | 0.69 |
| Baseline Duration | 3.1 ± 3.4 | 4.0 ± 3.4 | z=-1.32 | 0.19 |
| Lifetime Duration | 6.2 ± 4.8 | 8.1 ± 3.6 | z=-2.34 | 0.02 |
| Baseline number of episodes | 22.4 ± 36.8 | 41.4 ± 95.5 | z=0.62 | 0.54 |
| Lifetime number of episodes | 65.3 ± 110.0 | 66.3 ± 121.8 | z=0.08 | 0.93 |
| Baseline number of symptoms | 7.2 ± 1.4 | 7.5 ± 1.3 | z=-0.72 | 0.47 |
| Baseline GAF score (lifetime) | 41.2 ± 5.3 | 39.8 ± 6.0 | t(76)=0.36 | 0.72 |
| Follow-up GAF score (last month) | 56.0 ± 7.0 | 49.2 ± 7.2 | t(75)=3.66 | p<0.001 |
| N (%) | N (%) | |||
|---|---|---|---|---|
| % with severe impairment (baseline) | 14 (67) | 39 (68) | χ2(1)=0.02 | 0.88 |
3.1. Symptoms of Mania at Baseline and Follow-up by Persistence Status
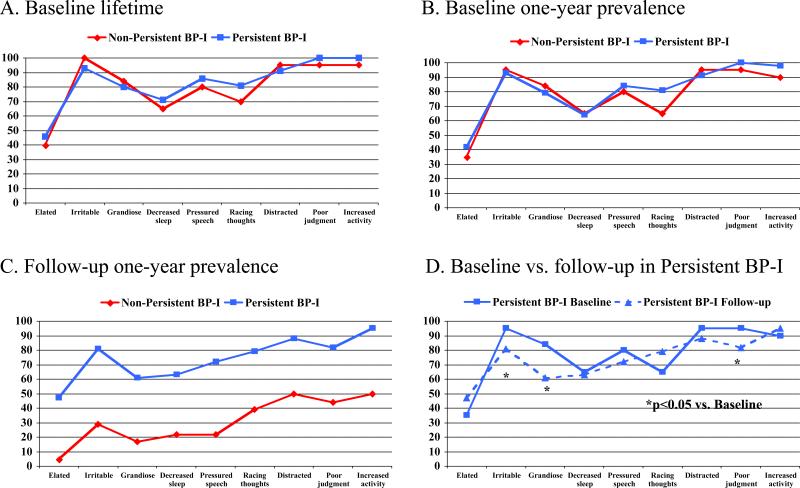
As shown in Figure 2, there were no significant differences between the groups on rates of individual symptoms of mania at baseline either lifetime (2A) or one-year prevalence (2B). Although persistent BP-I group had higher rates of symptoms at follow-up than Non-Persistent BP-I cases, many symptoms of mania persisted in the Non-Persistent BP-I group (Figure 2C). A very similar pattern of symptoms of mania was observed at baseline and follow-up in the Persistent BP-I group (Figure 2D).
Figure 2.
Mania symptoms
3.2. Psychiatric Disorders at Baseline and Follow-up by Persistence Status
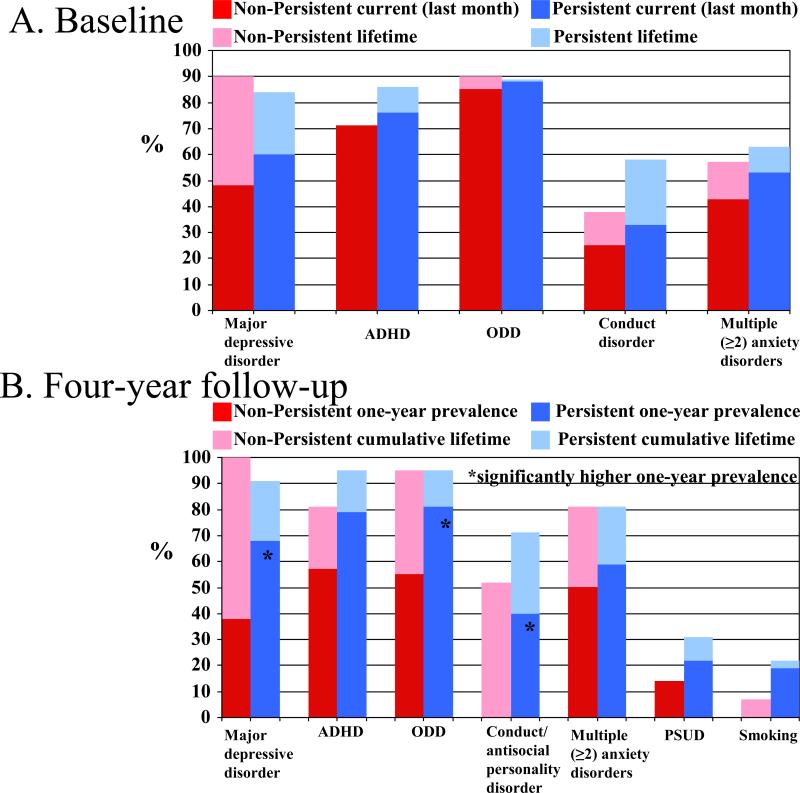
There were no meaningful differences at baseline in rates of psychiatric disorders either lifetime or last year between Persistent BP-I and Non-Persistent BP-I groups (Figure 3A). At the follow-up assessment, the Persistent BP-I group had significantly higher one-year prevalences of major depressive disorder, oppositional defiant disorder, and conduct disorder/antisocial personality disorder compared to the Non-Persistent BP-I group (Figure 3B).
Figure 3.
Comorbid Disorders
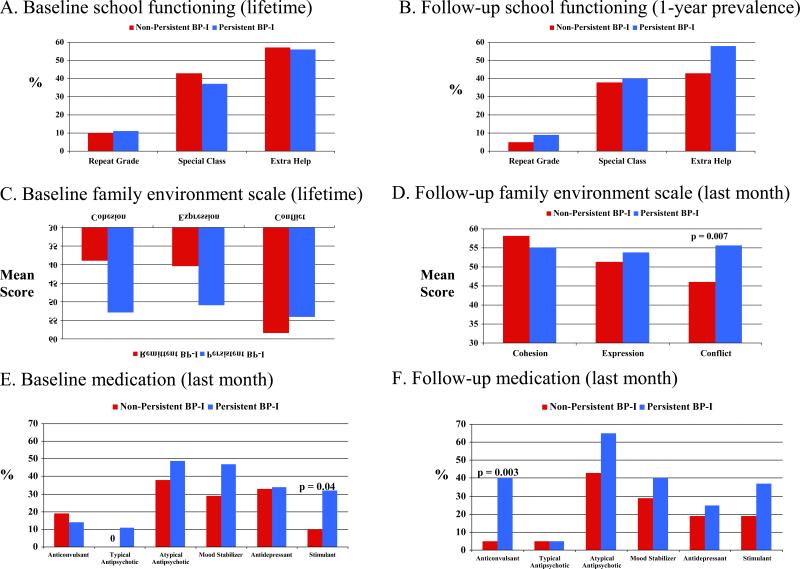
3.3. School Functioning, Family Environment, and Medication History by Persistence Status
Rates of educational impairments (Figure 4A and 4B) were equally high and did not differ between Persistent and non-Persistent cases at baseline and follow-up. At baseline, the Persistent BP-I subjects were in significantly more cohesive and expressive families as measured by the FES (Figure 4C) whereas at follow-up, the Persistent BP-I subjects had significantly higher family conflict scores compared to the Non-Persistent BP-I subjects (Figure 4D). Both at baseline and follow-up, the Persistent BP-I subjects were more likely to currently be on a stimulant medication compared to the Non-Persistent BP-I subjects but the difference reached statistical significance only at baseline (Figure 4E and 4F). At the 4-year follow-up, Persistent BP-I subjects were significantly more likely to currently be taking anticonvulsants compared to the Non-Persistent group (Figure 4F). Neither perinatal variables nor family history of psychopathology at baseline predicted persistent BP-I disorder. With the exception of the Persistent BP-I group at follow-up having a significantly poorer failure to maintain set score on the WCST compared to the Non-Persistent BP-I group (1.2 ± 1.5 vs. 1.9 ± 2.5, t(75)=3.66, p<0.001), no other neuropsychological scores differed at either baseline or follow-up assessments between the Persistent BP-I and Non-Persistent BP-I cases (Table 2).
Figure 4.
School and family functioning and medication
Table 2.
Neuropsychology
| Non-Persistent BP-I | Persistent BP-I | Test statistic | p-value | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
|
BASELINE NEUROPSYCHOLOGY | ||||
| N=15 | N=47 | |||
| WISC-3 | ||||
| Full scale IQ | 104.3 ± 17.2 | 103.5 ± 13.6 | t(57)=0.17 | 0.87 |
| Vocabulary IQ | 110.8 ± 19.8 | 104.9 ± 14.8 | t(60)=1.24 | 0.22 |
| Performance IQ | 95.8 ± 14.5 | 102.2 ± 17.3 | t(58)=-1.28 | 0.21 |
| Arithmetic | 9.8 ± 4.4 | 9.5 ± 2.8 | t(59)=0.27 | 0.79 |
| Digit span | 9.1 ± 3.0 | 8.9 ± 2.6 | t(60)=0.27 | 0.79 |
| Digit symbol | 7.2 ± 3.4 | 6.9 ± 4.0 | t(58)=0.29 | 0.77 |
| Symbol search | 8.3 ± 3.2 | 8.2 ± 3.4 | t(59)=0.09 | 0.93 |
| CPT | ||||
| Vigilance | 10.2 ± 2.2 | 9.1 ± 2.8 | t(56)=1.33 | 0.19 |
| Memory | 15.2 ± 5.7 | 13.2 ± 5.4 | t(55)=1.18 | 0.24 |
| Interference | 20.8 ± 7.2 | 20.5 ± 6.6 | t(17)=0.11 | 0.91 |
| Stroop | ||||
| Color t-score | 38.1 ± 7.8 | 38.1 ± 7.4 | t(52)=-0.009 | 0.99 |
| Word t-score | 40.1 ± 8.5 | 42.7 ± 7.0 | t(52)=-1.14 | 0.26 |
| Color-word t-score | 40.5 ± 8.1 | 39.1 ± 7.9 | t(53)=0.55 | 0.58 |
| Interference t-score | 49.5 ± 6.2 | 47.7 ± 6.7 | t(52)=0.85 | 0.40 |
| Wisconsin Card Sorting Test | ||||
| Failure to maintain set | 1.7 ± 1.7 | 1.6 ± 1.6 | t(44)=0.28 | 0.78 |
| Categories completed | 4.1 ± 1.9 | 3.9 ± 2.0 | t(45)=0.30 | 0.77 |
| Perseverative errors | 26.3 ± 22.7 | 22.3 ± 12.3 | t(44)=0.74 | 0.46 |
| Non-perseverative errors | 16.9 ± 10.7 | 24.7 ± 16.4 | t(44)=-1.48 | 0.15 |
| Rey-Osterrieth | ||||
| Copy organization | 6.1 ± 3.0 | 6.3 ± 3.6 | t(55)=-0.15 | 0.88 |
| Delay organization | 6.8 ± 3.3 | 5.0 ± 3.6 | t(49)=1.46 | 0.15 |
| CVLT t-score | 41.8 ± 16.7 | 41.6 ± 13.6 | t(57)=0.03 | 0.97 |
| WRAT arithmetic | 95.0 ± 15.9 | 97.0 ± 13.9 | t(58)=-0.46 | 0.64 |
| WRAT reading | 102.3 ± 16.9 | 105.2 ± 13.9 | t(59)=-0.66 | 0.51 |
| FOLLOW-UP NEUROPSYCHOLOGY | ||||
|---|---|---|---|---|
| N=12 | N=33 | |||
| WISC-3 | ||||
| Full scale IQ | 106.9 ± 22.8 | 99.6 ± 12.4 | t(43)=1.38 | 0.17 |
| Vocabulary IQ | 111.3 ± 19.4 | 101.3 ± 13.2 | t(43)=1.97 | 0.06 |
| Performance IQ | 101.1 ± 25.8 | 98.0 ± 15.1 | t(43)=0.50 | 0.62 |
| Arithmetic | 9.6 ± 5.0 | 8.6 ± 3.3 | t(43)=0.74 | 0.47 |
| Digit span | 9.3 ± 3.1 | 7.7 ± 2.8 | t(42)=1.73 | 0.09 |
| Digit symbol | 6.5 ± 4.0 | 5.6 ± 2.8 | t(42)=0.88 | 0.39 |
| Symbol search | 9.0 ± 4.9 | 7.2 ± 3.2 | t(42)=1.47 | 0.15 |
| CPT | ||||
| Vigilance | 9.9 ± 2.7 | 9.2 ± 3.0 | t(41)=0.70 | 0.49 |
| Memory | 16.7 ± 4.9 | 14.4 ± 4.1 | t(41)=1.54 | 0.13 |
| Interference | 19.8 ± 10.2 | 18.9 ± 8.4 | t(20)=0.19 | 0.85 |
| Stroop | ||||
| Color t-score | 37.2 ± 9.8 | 36.1 ± 7.5 | t(38)=0.36 | 0.72 |
| Word t-score | 40.6 ± 11.5 | 39.7 ± 8.7 | t(38)=0.29 | 0.77 |
| Color-word t-score | 38.8 ± 12.1 | 39.0 ± 8.7 | t(39)=-0.06 | 0.95 |
| Interference t-score | 49.4 ± 7.8 | 48.8 ± 6.5 | t(39)=0.29 | 0.78 |
| Wisconsin Card Sorting Test | ||||
| Failure to maintain set | 2.5 ± 1.9 | 1.2 ± 1.5 | t(34)=2.25 | 0.03 |
| Categories completed | 4.7 ± 1.8 | 5.0 ± 1.7 | t(34)=-0.50 | 0.62 |
| Perseverative errors | 18.9 ± 11.7 | 18.1 ± 19.3 | t(34)=0.13 | 0.90 |
| Non-perseverative errors | 15.6 ± 9.8 | 14.6 ± 12.2 | t(34)=0.26 | 0.80 |
| Rey-Osterrieth | ||||
| Copy organization | 7.8 ± 3.2 | 6.7 ± 3.6 | t(41)=0.92 | 0.36 |
| Delay organization | 6.9 ± 3.8 | 5.0 ± 2.9 | t(40)=1.78 | 0.08 |
| CVLT t-score | 36.0 ± 13.2 | 38.8 ± 14.6 | t(41)=-0.58 | 0.57 |
| WRAT arithmetic | 90.1 ± 23.4 | 89.3 ± 13.6 | t(43)=0.13 | 0.89 |
| WRAT reading | 99.8 ± 19.5 | 98.2 ± 14.0 | t(43)=0.30 | 0.76 |
4. Discussion
This 4 year longitudinal follow-up study evaluated the course of DSM-IV pediatric bipolar-I disorder from childhood onto mid adolescence as well as its predictors and correlates. The majority of youth with BP-I disorder at baseline (73.1%) continued to meet full DSM-IV diagnostic criteria for BP-I disorder at follow-up (i.e., syndromatic persistence as defined by Keck et al. (1998)). In addition, the overwhelming majority of the non-persistent cases had either subthreshold (6.4%) BP-I disorder, full or subthreshold (5.1%) major depression or 2) were euthymic (i.e., syndromatic and symptomatic remissions) but receiving pharmacotherapy for their mood disorder (9.0%). Only 5 cases (6.4%) were euthymic and not receiving treatment for bipolar disorder and could be considered true remitters. These results further document the high persistence of BP-I spectrum symptomatology in BP-I youth and support efforts for early identification and treatment.
The finding that 73% of our BP- I subjects continued to have the full disorder at the four year follow-up re-assessment at mid adolescence is consistent with rates of persistence into adolescence reported by Geller et al. (Geller et al. 2004) in a four year follow-up children with BP-I disorder. These investigators reported that a bipolar disorder diagnosis occurred during 67% of total weeks during the follow-up and that their subjects spent 57% of the follow-up period with mania or hypomania (unipolar or mixed). Our results are also consistent with those of Birmaher et al. (2006) in their 2 year follow-up study of 152 children and adolescents with BP-that found that 50% of their subjects had at least 1 syndromal recurrence and had syndromal or subsyndromal symptoms 60% of the follow-up time. The present results are also consistent with findings of a 50% rate of persistence of BP-I disorder reported by our group (Biederman et al. 2004) in a longitudinal study of youth with ADHD and comorbid BP-I disorder over a 10-year period.
Subjects with a persistent course of BP-I disorder had, on average, a duration of BP-I disorder that was two years longer at baseline compared to those with a Non-Persistent BP-I course. These results are consistent with those of Birmaher et al. (Birmaher et al. 2006) who also reported that having had a longer duration of mood symptoms at baseline was predictive of a poorer outcome. If confirmed, this finding would suggest that a protracted period of aberrant and unstable mood in childhood predicts a chronic course of bipolar disorder with its attendant devastating consequences to the child and the family.
At the 4-year follow-up, the Persistent BP-I group had a significantly higher one-year prevalence of major depressive disorder, oppositional defiant disorder, and conduct disorder/antisocial personality disorder compared to the Non-Persistent BP-I group. Considering the high morbidity and disability associated with these psychiatric disorders, their presence add to the severity of the clinical picture associated with a persistent course of full BP-I disorder.
The higher family cohesion scores at baseline in the persistent cases counters the idea that poor family cohesion breeds bipolar mood symptoms in children. The elevated family conflict scores at follow-up in families of persistent cases highlight the emotional toll that pediatric bipolar disorder exacts on affected families. These findings further underscore the high level of dysfunction and morbidity associated with pediatric bipolar disorder.
Although reaching our threshold for statistical significance at the baseline assessment only, the Persistent BP-I subjects were more likely to currently be on a stimulant medication at both baseline and follow-up compared to the Non-Persistent BP-I subjects. If conformed, this finding would suggest that the use of stimulants in the treatment of bipolar youth increases the likelihood of a chronic protracted course of mood instability.
Our findings also show that the overwhelming majority of 21 not fully persistent cases with full BP-I disorder continued to be affected by either subthreshold BP-I disorder (n=5), full or subthreshold (n=4) major depression, or were euthymic but were treated for the disorder (n=7). Persistent and Non-Persistent cases had similarly high levels of psychiatric comorbidity, neuropsychological deficits, family dysfunction, and school dysfunction rates at the follow-up assessment. These findings indicate that subsyndromal cases continue to struggle with persistent morbidity and disability despite some reduction in the symptomatic picture of BP-I disorder. These results are consistent with studies in pediatric and adult psychiatry that document the morbidity and disability associated with subthreshold forms of BP-I disorder. Lewinsohn et al. (1995) reported, in a community sample, that adolescents who had subthreshold bipolar disorder had impairment, comorbidity and suicide attempts that were as severe as those with a full bipolar diagnosis. Similar findings were reported in the Course of Bipolar Youth (COBY) study (Birmaher et al. 2009; Birmaher et al. 2006), which assessed 263 youth with BP-I, BP-II and BP-NOS at 2 and 4 year follow-ups. This study found high rates of persistence in subthreshold BP-I cases, with 80% of these subjects spending 60% of the follow-up time with significant affective symptoms.
Likewise using data from the National Comorbidity Survey of over 9000 adults, Merikangas et al. (2007) reported that subthreshold bipolar disorder in adults is associated with high morbidity and disability. Recent findings in adults document that even minimal manic symptoms coexisting with otherwise full syndromal major depression are harbingers of treatment-emergent mania or hypomania from antidepressant treatment (Frye et al. 2009). Judd et al. (2003) gathered weekly mood symptom ratings from adult bipolar patients and documented the high frequency of depressive symptoms in bipolar adults. Altshuler et al. (2002) noted that persistent symptoms of depression in bipolar adults were associated with poor functioning, with a negative correlation between depression rating scale scores and global assessment of functioning scores, even in those without full syndromal depression. Taken together, these findings stress the clinical importance of identifying subsyndromal forms of BP-I disorder that can be disabling and worthy of clinical and scientific attention.
Our finding that less than 7% of our subjects attained true remission (syndromatic and symptomatic remission and were not receiving treatment) is consistent with our earlier study documenting the complex recovery process of youth with ADHD and comorbid BP-I disorder over a 10-year span (Biederman et al. 2004). That study showed that only 15% of bipolar subjects attained euthymia. In our current sample, 9% of our BP-I subjects attained euthymia while receiving psychopharmacological treatment for their mood disorder. More information is needed to better understand predictors of remission in studies of youth with bipolar disorder.
At the 4-year follow-up, Persistent BP-I subjects were significantly more likely to be taking anticonvulsants (Figure 4F). These results are consistent with results from a recent randomized clinical trial that failed to document separation from placebo for oxcarbazepine (Wagner et al. 2006), topiramate (Delbello et al. 2005) and divalproex sodium (Wagner et al. 2009).
Our findings should be considered in the context of methodological limitations. Although we did not administer structured diagnostic interviews directly to children younger than 12 years of age, a clinical diagnosis of BP-I in probands was corroborated by clinical assessment by an expert clinician (JW) prior to study inclusion (Wozniak et al. 2003). In addition, as the mean age at follow up was 14 years, most subjects underwent direct structured interview at follow-up. While 25% of the sample was lost to follow-up after 5 years, few differences (age of onset of bipolar disorder and SES) between those lost to follow-up and those included in the study were found. Because this sample was clinically referred and primarily Caucasian, these results may not generalize to non-referred children or to families of other ethnic groups. We did not have any Tanner staging data and therefore could not report on pubertal development. Our definition of persistence and remission by the presence of full or subthreshold syndromes of mania or depression occurring in the past year at the time of follow-up differed from those used by other investigators (Birmaher et al. 2009; Birmaher et al. 2006; Geller et al. 2008) who defined remission as an 8 week period of loss of full syndrome. While the establishment of the best definition of remission and persistence for pediatric BP-I disorder awaits additional research we believe that the definitions of persistence and remission used in our study are ecologically meaningful as they capture the spectrum of related conditions associated with BP-I disorder and embrace a clinically meaningful time period (previous year). Because of the small number of fully remitting cases (n=5), comparisons were made between subjects that continued to meet full diagnostic criteria for BP-I disorder (Persistent BP-I, n=57) and subjects with partial or full remission of BP-I disorder (Non-Persistent BP-I, n=21). Because there were statistically significant differences in socio-economic status and age at onset of bipolar disorder with the returning probands having an earlier age at onset and coming from a higher SES bracket, we do not know how these confounders affected our results.
Despite these limitations, this longitudinal 4 year follow-up study onto mid adolescence documents a high level of morbid persistence of pediatric BP-I disorder including not only its full syndromatic persistence, but also the persistence of subthreshold states of mania, full and subthreshold states of depression and those who attain euthymia, but in the presence of anti-manic pharmacotherapy. These results contribute to a growing scientific literature documenting the morbidity and persistence of pediatric BP-I disorder from childhood onto adolescent years. Our findings emphasize the critical need for early identification and appropriate interventions for children with DSM-IV BP-I and associated disorders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Altshuler L, Gitlin M, Mintz J, Leight K, Frye M. Subsyndromal depression is associated with functional impairment in patients with bipolar disorder. Journal of Clinical Psychiatry. 2002;63:807–811. doi: 10.4088/jcp.v63n0910. [DOI] [PubMed] [Google Scholar]
- Biederman J. Developmental subtypes of juvenile bipolar disorder. Harvard Review of Psychiatry. 1995;3:227–230. doi: 10.3109/10673229509017189. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Wozniak J, Mick E, Kwon A, Cayton GA, Clark SV. Clinical correlates of bipolar disorder in a large, referred sample of children and adolescents. Journal of Psychiatric Research. 2005a;39:611–622. doi: 10.1016/j.jpsychires.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Biederman J, Hammerness P, Doyle R, Joshi G, Aleardi M, Mick E. Risperidone treatment for ADHD in children and adolescents with bipolar disorder. Neuropsychiatric Disease and Treatment. 2008;4:203–207. doi: 10.2147/ndt.s1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, McDonnell MA, Wozniak J, Spencer T, Aleardi M, Falzone R, Mick E. Aripiprazole in the treatment of pediatric bipolar disorder: A systematic chart review. CNS Spectrums. 2005b;10:141–8. doi: 10.1017/s1092852900019489. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Faraone SV, Van Patten S, Burback M, Wozniak J. A Prospective Follow Up Study of Pediatric Bipolar Disorder in boys with attention deficit/hyperactivity disorder. Journal of Affective Disorders. 2004;82S:S17–S23. doi: 10.1016/j.jad.2004.05.012. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick E, Spencer T, Doyle R, Joshi G, Hammerness P, Kotarski M, Aleardi M, Wozniak J. An open-label trial of aripiprazole monotherapy in children and adolescents with bipolar disorder. CNS Spectr. 2007;12:683–9. doi: 10.1017/s1092852900021519. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Houck P, Ha W, Iyengar S, Kim E, Yen S, Hower H, Esposito-Smythers C, Goldstein T, Ryan N, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan N, Leonard H, Hunt J, Iyengar S, Keller M. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–83. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang K, Adleman NE, Dienes K, Simeonova DI, Menon V, Reiss A. Anomalous prefrontal-subcortical activation in familial pediatric bipolar disorder: a functional magnetic resonance imaging investigation. Arch Gen Psychiatry. 2004;61:781–92. doi: 10.1001/archpsyc.61.8.781. [DOI] [PubMed] [Google Scholar]
- Chang K, Barnea-Goraly N, Karchemskiy A, Simeonova DI, Barnes P, Ketter T, Reiss AL. Cortical magnetic resonance imaging findings in familial pediatric bipolar disorder. Biol Psychiatry. 2005a;58:197–203. doi: 10.1016/j.biopsych.2005.03.039. [DOI] [PubMed] [Google Scholar]
- Chang K, Karchemskiy A, Barnea-Goraly N, Garrett A, Simeonova DI, Reiss A. Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005b;44:565–73. doi: 10.1097/01.chi.0000159948.75136.0d. [DOI] [PubMed] [Google Scholar]
- Delbello MP, Findling RL, Kushner S, Wang D, Olson WH, Capece JA, Fazzio L, Rosenthal NR. A Pilot Controlled Trial of Topiramate for Mania in Children and Adolescents With Bipolar Disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:539–547. doi: 10.1097/01.chi.0000159151.75345.20. [DOI] [PubMed] [Google Scholar]
- Delis D, Kramer J, Kaplan E, Ober B. The california verbal learning test -children's version. Psychological Corporation; San Antonio: 1994. [Google Scholar]
- Faraone S, Glatt S, Tsuang M. The genetics of pediatric onset bipolar disorder. Biological Psychiatry. 2003;53:970–977. doi: 10.1016/s0006-3223(02)01893-0. [DOI] [PubMed] [Google Scholar]
- Findling RL, Gracious BL, McNamara NK, Youngstrom EA, Demeter CA, Branicky LA, Calabrese JR. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disorders. 2001;3:202–210. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Frye MA, Helleman G, McElroy SL, Altshuler LL, Black DO, Keck PE, Jr., Nolen WA, Kupka R, Leverich GS, Grunze H, Mintz J, Post RM, Suppes T. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164–72. doi: 10.1176/appi.ajp.2008.08030322. [DOI] [PubMed] [Google Scholar]
- Geller B. Phenomenology and course of pediatric bipolar disorders: Washington University School of Medicine. 1994.
- Geller B, Cook EH., Jr Ultradian rapid cycling in prepubertal and early adolescent bipolarity is not in transmission disequilibrium with val/met COMT alleles. Biological Psychiatry. 2000a;47:605–9. doi: 10.1016/s0006-3223(99)00251-6. [DOI] [PubMed] [Google Scholar]
- Geller B, Craney JL, Bolhofner K, DelBello MP, Williams M, Zimerman B. One-Year Recovery and Relapse Rates of Children With a Prepubertal and Early Adolescent Bipolar Disorder Phenotype. American Journal of Psychiatry. 2001;158:303–305. doi: 10.1176/appi.ajp.158.2.303. [DOI] [PubMed] [Google Scholar]
- Geller B, Craney JL, Bolhofner K, Nickelsburg MJ, Williams M, Zimerman B. Two-year prospective follow-up of children with a prepubertal and early adolescent bipolar disorder phenotype. American Journal of Psychiatry. 2002a;159:927–33. doi: 10.1176/appi.ajp.159.6.927. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R. Prepubertal and early adolescent bipolar I disorder: review of diagnostic validation by Robins and Guze criteria. Journal of Clinical Psychiatry. 2005;66(Suppl 7):21–28. [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65:1125–33. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B, Strauss NA, Kaufmann P. Controlled, blindly rated, direct-interview family study of a prepubertal and early-adolescent bipolar I disorder phenotype: morbid risk, age at onset, and comorbidity. Arch Gen Psychiatry. 2006;63:1130–8. doi: 10.1001/archpsyc.63.10.1130. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Craney JL, Bolhofner K. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61:459–67. doi: 10.1001/archpsyc.61.5.459. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, Delbello MP, Soutullo CA. Diagnostic characteristics of 93 cases of a prepubertal and early adolescent bipolar disorder phenotype by gender, puberty and comorbid attention deficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2000b;10:157–64. doi: 10.1089/10445460050167269. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Delbello MP, Bolhofner K, Craney JL, Frazier J, Beringer L, Nickelsburg MJ. DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. J Child Adolesc Psychopharmacol. 2002b;12:11–25. doi: 10.1089/10445460252943533. [DOI] [PubMed] [Google Scholar]
- Golden CJ. Stroop Color and Word Test: A Manual for Clinical and Experimental Use. Stoelting, Co.; Chicago: 1978. [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sort Test Manual: Revised and Expanded. Psychological Assessment Resources, Inc.; Odessa, FL: 1993. [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Yale Press; New Haven: 1975. [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, Solomon DA, Leon AC, Keller MB. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. 2003;60:261–9. doi: 10.1001/archpsyc.60.3.261. [DOI] [PubMed] [Google Scholar]
- Kafantaris V, Coletti DJ, Dicker R, Padula G, Pleak RR, Alvir JM. Lithium Treatment of Acute Mania in Adolescents: A Placebo-Controlled Discontinuation Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:984–993. doi: 10.1097/01.chi.0000129223.89433.74. [DOI] [PubMed] [Google Scholar]
- Keck P, McElroy S, Strakowski S, West S, Sax K, Hawkins J, Bourne M, Haggard P. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. American Journal of Psychiatry. 1998;155:646–652. doi: 10.1176/ajp.155.5.646. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. American Journal of Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, Rich BA, Vinton DT, Nelson EE, Fromm SJ, Berghorst LH, Joshi P, Robb A, Schachar RJ, Dickstein DP, McClure EB, Pine DS. Neural circuitry engaged during unsuccessful motor inhibition in pediatric bipolar disorder. Am J Psychiatry. 2007;164:52–60. doi: 10.1176/ajp.2007.164.1.A52. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P, Klein D, Seeley J. Bipolar disorders in a community sample of older adolescents: Prevalence, phenomenology, comorbidity, and course. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore CM, Biederman J, Wozniak J, Mick E, Aleardi M, Wardrop M, Dougherty M, Harpold T, Hammerness P, Randall E, Lyoo IK, Renshaw PF. Mania, glutamate/glutamine and risperidone in pediatric bipolar disorder: a proton magnetic resonance spectroscopy study of the anterior cingulate cortex. J Affect Disord. 2007;99:19–25. doi: 10.1016/j.jad.2006.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Manual for the Family Environment Scale. Consulting Psychologists Press; Palo Alto, CA: 1974. [Google Scholar]
- Nierenberg A, Henin A, Mick E, Ostacher M, Borrelli DJ, Gironde SVM, Marzilli G, Sachs GS, Biederman J. Relationship between comorbid psychopathology among adults with bipolar disorder and their offspring: phenotypic implications for genetic studies. Bipolar Disord. 2005;7:82. [Google Scholar]
- Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale: 1994. [Google Scholar]
- Pavuluri MN, Henry DB, Carbray JA, Sampson G, Naylor MW, Janicak PG. Open label prospective trial of risperidone in combination with lithium or divalproex sodium in pediatric mania. Journal of Affective Disorders. 2004;82:S103–111. doi: 10.1016/j.jad.2004.05.017. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, O'Connor M M, Harral E, Sweeney JA. Affective neural circuitry during facial emotion processing in pediatric bipolar disorder. Biol Psychiatry. 2007;62:158–67. doi: 10.1016/j.biopsych.2006.07.011. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Smoller JW, Ferreira MA, McQuillin A, Bass N, Lawrence J, Sachs GS, Nimgaonkar V, Scolnick EM, Gurling H, Sklar P, Purcell S. A genomewide association study of response to lithium for prevention of recurrence in bipolar disorder. Am J Psychiatry. 2009;166:718–25. doi: 10.1176/appi.ajp.2009.08111633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey A. L'examen psychologique dans les cas d'encephalopathie traumatique. Les Archives de Psychologie. 1941;28:286–340. [Google Scholar]
- Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. American Journal of Psychiatry. 1970;126:983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Biederman J, Weber W, Hatch M, Faraone SV. Neuropsychological function in adults with attention-deficit hyperactivity disorder. Biol Psychiatry. 1998;44:260–8. doi: 10.1016/s0006-3223(97)00392-2. [DOI] [PubMed] [Google Scholar]
- Tohen M, Kryzhanovskaya L, Carlson G, Delbello M, Wozniak J, Kowatch R, Wagner K, Findling R, Lin D, Robertson-Plouch C, Xu W, Dittmann RW, Biederman J. Olanzapine versus placebo in the treatment of adolescents with bipolar mania. Am J Psychiatry. 2007;164:1547–56. doi: 10.1176/appi.ajp.2007.06111932. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Kowatch RA, Emslie GJ, Findling RL, Wilens TE, McCague K, D'Souza J, Wamil A, Lehman RB, Berv D, Linden D. A double-blind, randomized, placebo-controlled trial of oxcarbazepine in the treatment of bipolar disorder in children and adolescents. Am J Psychiatry. 2006;163:1179–86. doi: 10.1176/ajp.2006.163.7.1179. [DOI] [PubMed] [Google Scholar]
- Wagner KD, Redden L, Kowatch RA, Wilens TE, Segal S, Chang K, Wozniak P, Vigna NV, Abi-Saab W, Saltarelli M. A double-blind, randomized, placebo-controlled trial of divalproex extended-release in the treatment of bipolar disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:519–32. doi: 10.1097/CHI.0b013e31819c55ec. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Manual for the Wechsler Intelligence Scale for Children. Third Edition The Psychological Corporation, Harcourt Brace Jovanovich, Inc.; San Antonio: 1991. [Google Scholar]
- Wozniak J. Pediatric bipolar disorder: the new perspective on severe mood dysfunction in children. J Child Adolesc Psychopharmacol. 2003;13:449–51. doi: 10.1089/104454603322724832. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kiely K, Ablon S, Faraone S, Mundy E, Mennin D. Mania-like symptoms suggestive of childhood onset bipolar disorder in clinically referred children. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:867–876. doi: 10.1097/00004583-199507000-00010. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Biederman J, Kwon A, Mick E, Faraone S, Orlovsky K, Schnare L, Cargol C, van Grondelle A. How cardinal are cardinal symptoms in pediatric bipolar disorder? An examination of clinical correlates. Biol Psychiatry. 2005;58:583–8. doi: 10.1016/j.biopsych.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Wozniak J, Monuteaux M, Richards J, Lail K, Faraone SV, Biederman J. Convergence between structured diagnostic interviews and clinical assessment on the diagnosis of pediatric-onset bipolar disorder. Biological Psychiatry. 2003;53:938–944. doi: 10.1016/s0006-3223(03)00344-5. [DOI] [PubMed] [Google Scholar]