Abstract
Background
Using data from the mandatory quality assurance program for stroke care in Hesse, we analyze regional differences in thrombolysis rates and infer some ways in which care can be improved.
Methods
We identified 7707 patients with acute ischemic stroke who were admitted to hospital within 3 hours of symptom onset in 2007 and 2008, and we determined the local thrombolysis rate district by district. In order to exclude the possibility that the observed local differences in thrombolysis rates might be accounted for, in large part, by off-label thrombolysis procedures, we further narrowed down the subgroup of patients who underwent thrombolysis to the 1108 patients admitted within 2 hours of symptom onset. We also analyzed the local thrombolysis rates for patients who were primarily referred to stroke units.
Results
The overall thrombolysis rate among patients admitted within 3 hours of symptom onset was 19%, varying locally from 6% to 35%. Among patients admitted within 2 hours of symptom onset, the local thrombolysis rate ranged from 13% to 85%. Even in patients primarily referred to stroke units, the local thrombolysis rate ranged from 8% to 44% in the 3-hour group and from 16% to 62% in the 2-hour group.
Conclusion
Local thrombolysis rates vary unexpectedly widely across the state of Hesse. The care of patients with acute stroke after they reach the hospital urgently needs critical reappraisal and improvement.
Since 2003, all hospitals in the German Federal State of Hesse that treat patients with acute stroke are legally obliged to participate in the quality assurance program for stroke treatment in Hesse. As part of this quality assurance program, in an evidence-based process a set of indicator variables was implemented that has been scientifically proven to be associated with the course or prognosis of a stroke and also measures the structure, process and effectiveness of the stroke treatment (1). Among these indicators, the performance of systemic thrombolytic therapy in patients with acute cerebral infarction is a very hard parameter, and one that is at the same time easy to measure. After appropriate adjustment, an individual hospital’s lysis rate reflects the effectiveness of the diagnostic and therapeutic chain in a particularly short time window, along with that individual hospital’s experience with thrombolytic therapy.
In addition to these points, it must not be forgotten that systemic thrombolysis within the first 3 hours after onset of symptoms is a licensed medical therapy that has been proven to be effective for acute cerebral infarction, and so far as possible all eligible patients should receive it (2).
Apart from the time window and the presence of a disabling neurological deficit, the most important feature for initial selection of patients for whom systemic thrombolysis is suitable is that intracranial hemorrhage has been ruled out on imaging.
Method
The quality assurance program for acute stroke treatment in Hesse requires that all patients aged 18 years or over who have a cerebral infarct (ICD-10 I63, I64) and are admitted to hospital for treatment must be documented within 7 days of the onset of symptoms. Since 2003, this quality assurance procedure has been mandatory for all acute hospitals (n = 89) involved in inpatient treatment for stroke. During the report period, only seven hospitals with ≤ 10 cases per year failed to carry out the required documentation. The documentation rate, which can be calculated on the basis of a comparison with billing records (taken as the target 100% rate), was 95.5% during the period under analysis (range 0–100%).
In this study, first all patients were identified who were admitted to hospital for treatment of acute cerebral infarction in Hesse during the reporting years 2007 and 2008 (n = 24 215) with a time from symptom onset to hospital admission of less than 3 hours (n = 7707) (3-h cohort). In a second step, these data were regionalized at rural or urban district level according to the patients’ documented home postal codes. Patients’ full (five-figure) postal codes are routinely recorded by all hospitals as part of the quality assurance procedure (coding error rate: <0.5%). The Hesse State Hospital Law contains a provision that allows the Hesse Quality Assurance Office (Geschäftsstelle Qualitätssicherung Hessen, GQH) to record such data legally. The publication of aggregate quality assurance data has also been cleared with the Hesse Data Protection Commissioner, so no data protection problem arises here either.
In the next step, for each district the percentage of systemic thrombolytic therapies carried out was compared with the percentage of patients in the 3-h cohort. To investigate whether the differences between districts would be mainly accounted for by off-label thrombolysis procedures, the analysis was then further narrowed to the group of patients who were admitted to hospital ≤2 hours after symptom onset, were aged between 18 and 80 years, and had a premorbid modified Rankin scale score ≤3 (i.e., patients who were able to walk before disease onset) (n = 1108, 2-h cohort). The National Institutes of Health Stroke Scale Score (NIHSS), which is used to grade the severity of the neurological deficit, is incompletely documented and cannot therefore be used as a filter.
Since the performance of thrombolysis is closely associated with admission to a specialist stroke unit, the next step was to examine admission to a stroke unit separately for the 3-h and the 2-h cohorts. The Hospital Requirements Plan for Hesse does not show stroke units separately. For this reason, we defined stroke units operationally as units that billed for patient treatment under the operation and medical procedure code OPS 8–981 (“complex neurological treatment of stroke”), which requires among other things that lytic therapy is available around the clock. In the final step, the relative frequency of lytic therapy in the 3-h and 2-h cohorts was evaluated exclusively for patients with primary referral to a stroke unit.
In addition to descriptive statistics, the data were analyzed by linear regression using the least square method. The Kendall rank correlation coefficient was calculated to correlate lysis rates with each other and with the total number of cases.
Results
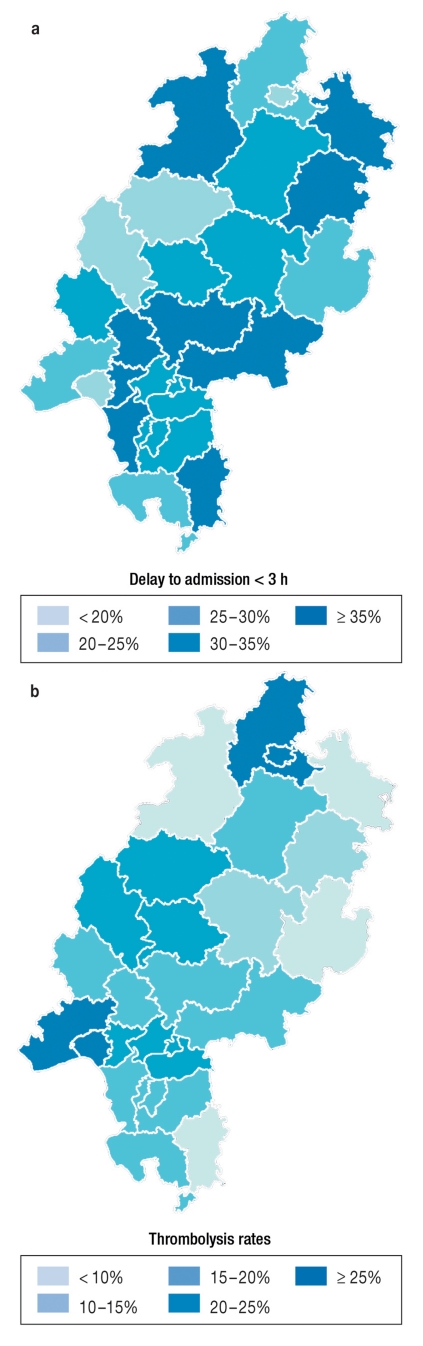
In Hessen in 2007 and 2008, overall 32.2% (7707) of all patients with acute cerebral infarction reached hospital within 3 hours after onset of their symptoms. This percentage varied regionally between 20.9% and 42.7% (Figure 1a). Related to the total number of patients, the thrombolysis rate in Hesse was 6.1%. In the 3-h cohort, the mean thrombolysis rate was 19.3% (n = 1488). The regional range in this group was 5.6% to 35.3% (Figure 1b). The 2-h cohort (n = 1108) accounted for 4.6% of all hospital admissions with acute cerebral infarction, with a regional range of 1.8% to 8.0%. A mean of 52.7% of these patients received lytic therapy (n = 587), with a regional variation in lysis rates between 13.0% and 85.3%. The total number of patients and the frequency of thrombolytic therapy in the 2-h and 3-h cohorts respectively did not correlate with each other (Kendall’s τ = –0.23; p = 0.25 and 0.17 respectively; p = 0.48).
Figure 1.
Delay to admission and thrombolysis rate
Regional distribution of percentages of patients with a delay to admission <3 hours from symptom onset
Regional percentage of thrombolytic treatments carried out in patients with a delay to admission <3 hours after symptom onset
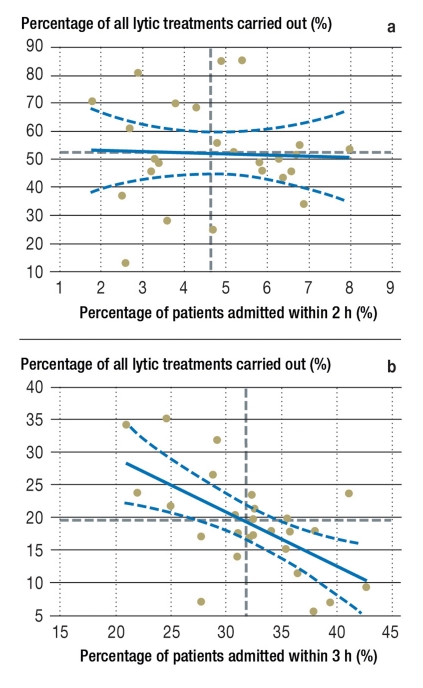
No correlation was found between the thrombolysis rate and the number of patients in the 2-h cohort (Figure 2a); by contrast, a statistically significant negative correlation was seen in the group with admission within 3 hours (r = –0.60 [95% confidence interval –0.90 to –0.38), p = 0.0012] (Figure 2b).
Figure 2.
Delay to admission and thrombolysis rates
Thrombolysis rates in the patient group admitted to hospital ≤ 2 hours after symptom onset, aged between 18 and 80 years, and with a modified Rankin Scale score ≤3 plotted for the individual districts in Hesse against admission delay.
Thrombolysis rates versus percentages of patients with hospital admission <3 hours after symptom onset.
The broken black horizontal and vertical lines show the respective means of the patient percentages and the percentages of thrombolytic treatments carried out. The regression line with 95% confidence interval is also shown.
Restricting the analysis only to districts with their own stroke unit did not change the results much: The mean lysis rate for patients admitted within 3 hours was 21.0% (range 7.2% to 35.3%), mean lysis rate for patients admitted up to 2 hours after onset was 53.0% (range 13.0% to 85.3%). Here too a negative trend was shown between the percentage of patients admitted within 3 hours and the lysis rate (r = –0.60 [95% confidence interval –1 to –0.32], p = 0.015), whereas no correlation was shown in the 2-h cohort.
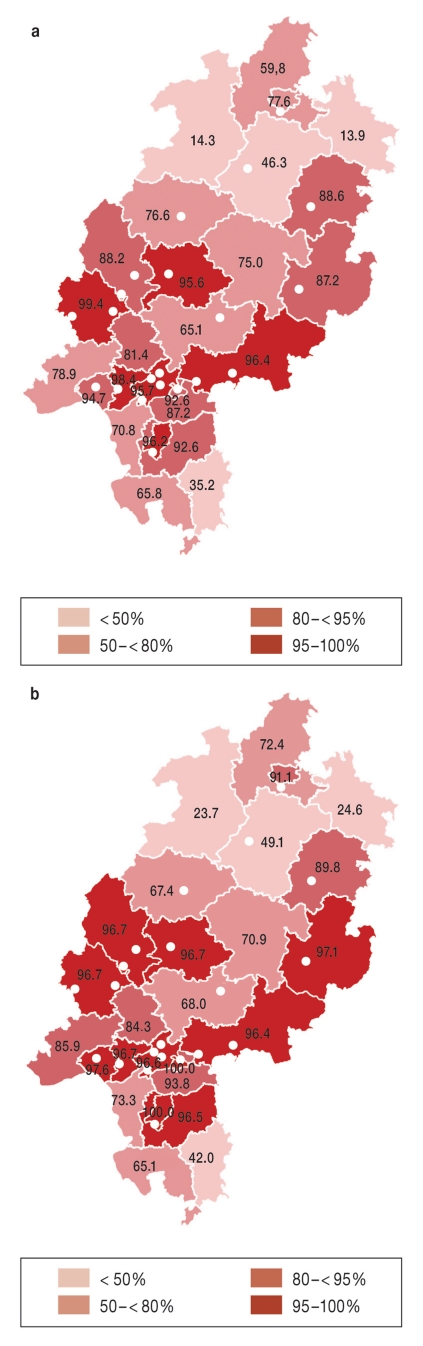
In total, in Hesse in 2007 and 2008, 70.3% of all patients with cerebral infarction were treated in a stroke unit. In 86.4% of cases the thrombolytic therapy was carried out in a specialist stroke unit. Figures 3a and 3b show region by region the relative proportions of patients in the 3-h and 2-h cohorts who were treated in a stroke unit. No statistically significant correlation was found between regional access to treatment in a stroke unit and either the percentages of the 3-h and 2-h cohorts (Kendall’s τ = 0.11; p = 0.44) or the respective regional thrombolysis rates (Kendall’s τ = 0.23; p = 0.09). Including only the patients referred to a stroke unit, the median regional lysis rate in the 3-h cohort was 21.4% (range 7.6% to 43.5%). The median lysis rate in the 2-h cohort was 36.8% (regional range 16.1% to 62.0%).
Figure 3.
Treatment in a stroke unit and thrombolysis rates
Percentages of patients admitted within 3 hours of symptom onset who were treated in a stroke unit
Percentages of patients admitted within ≤2 hours of symptom onset, aged between 18 and 80 years, and with a modified Rankin scale score ≤3 who were treated in a stroke unit.
The numbers are medians; points mark the locations of the stroke units
Because of multiple testing, Bonferroni correction was carried out and a p-value <0.008 taken to be significant.
Discussion
The results of this study, which rely on data from the mandatory quality assurance of stroke treatment in Hesse, reveal unexpectedly large regional differences in early stroke care in Hesse.
Considerable differences are obvious in the percentages of patients with early admission as well as in the thrombolysis rates, and these cannot be explained by geography alone. As Figures 1 and 2 show, there are districts with very high thrombolysis rates in the 2-h and 3-h cohorts, although the percentage of these patients in these cohorts at hospital admission is small. In contrast, some districts show a very high percentage of patients who might potentially be eligible for lytic therapy, but actually have only a very low thrombolysis rate in this group.
In the first case, improved patient education about the symptoms of stroke and optimization of patient transfer to hospital by the emergency services are obvious steps for improvement.
The second pattern—a relatively large percentage of patients transported to hospital early, but a disproportionately low rate of thrombolysis—cannot be explained by the available data.
The range of regional lysis rates for patients with up to a 3-h delay to admission was 6% to 35%. Limiting the study cohort to patients with the main inclusion criteria for potential candidates for thrombolysis according to license regulations in Germany resulted in a regional range of lysis rates at that time from 13% to 85%, meaning that off-label thrombolysis may be largely ruled out as an explanation for these enormous regional differences. What is actually astonishing is that even restricting the analysis to patients who received primary treatment in a stroke unit produces a similarly high regional range of lysis rates (3-h cohort: 8% to 44%; 2-h cohort: 16% to 62%). While it is known that even stroke experts weight and interpret the many exclusion criteria quite differently (3), it is hardly plausible that differences in the interpretation of inclusion and exclusion criteria can explain the regional differences observed here. Rather, what is needed is to take a long, hard look at the treatment pathways within the hospitals.
The total number of stroke patients during the observation period and the thrombolysis rate did not correlate with each other. No doubt it is of some relevance to the large regional discrepancies in lysis rates that patients are transported to hospitals that do not perform thrombolytic therapy, or are transported late to hospitals that do. The study data, which relate to where the patient lives (rather than where the treatment took place) show these discrepancies, even though they do not allow conclusions in detail about the actual reason on the ground. Another thing that affects the lysis rate is whether the treatment took place in a department primarily concerned with internal medicine or in a neurological department. On the other hand, 86.4% of all lyses were carried out in stroke units with neurological competence, so these effects cannot entirely explain the observed discrepancies, especially since restricting the analysis to patients who received primary treatment in stroke units does not, unfortunately, improve the picture.
Even the arrival of stroke patients at a primary stroke unit during the potential lysis window shows considerable variation (in the 3-h cohort, 13.9% to 99.4%, Figure 3a). In the short term this situation can only be improved by a stringent emergency services protocol for transporting acute stroke cases, such as already exists in many but not all districts of Hesse. This should also result in the implementation of plans for cross-district-boundaries emergency services provision. In the long term these data should be fed into the regulatory plan for hospital planning; this too has already been done in other federal states in Germany (Baden-Württemberg, Bremen, Bavaria, Hamburg, Mecklenburg–West Pomerania, North Rhine–Westphalia, Rhineland-Palatinate, Saarland, Saxony, Schleswig-Holstein). The lack of statistical correlation between the percentage of patients primarily transferred to a stroke unit and the regional lysis rates leads us to conclude that the reason for the strong regional discrepancies in relative thrombolysis rates is largely to be sought in the treatment pathways within the individual hospitals.
One further finding of this analysis relates mainly to the patients with a delay to admission of 2 to 3 hours after onset of symptoms. While no correlation was observed in the 2-h cohort between lysis rate and patient percentage (Figure 2a), in the 3-h cohort a significant negative correlation was seen (Figure 2b). That is, the higher the percentage of patients arriving at hospital up to 3 hours after symptom onset in a district, the lower the percentage of patients in this group in whom lytic therapy is carried out. The reason for this observation cannot be inferred from the database, because this documents the patients’ time window (interval from onset of symptoms to hospital admission) only in a categorized manner and does not record the reason why lysis was not carried out. It is possible that the high percentage of patients not receiving thrombolysis is due to those patients who just reach hospital within the 3-h window but cannot be lysed within that window. It is important to investigate in future whether these data will change with the extension of the lysis time window to 4.5 hours (4).
Naturally this study has numerous limitations. One important one is that it is unknown how many patients were treated outside Hesse. Patient transfer patterns by the emergency services also no doubt depend on the care level at the hospitals involved, so the data in Figure 2 must be interpreted with caution.
The intention of this study is not to wag the finger in public at individual districts in Hesse, but to achieve improvements by an open discussion. The goal should be that within a federal state such as Hesse all citizens have more or less the same chance of receiving optimal treatment should they suffer acute stroke.
Despite these limitations, the regional mandatory quality assurance program delivers data that are relevant to care provision, from which an urgent need for action can be inferred. Quality assurance is also, however, the way to monitor the process of improvement.
Key Messages.
Large regional differences exist in Hesse in the percentages of patients with stroke who are admitted to hospital early after the onset of symptoms.
There are also large regional differences in Hesse in the numbers of patient admitted for primary treatment in a stroke unit within the potential time window for lytic treatment.
Thrombolysis rates fluctuate strongly across Hesse, but there is no close correlation with either the regional percentage of patients admitted early or the percentage of patients treated in a stroke unit.
The presence of a stroke unit does not guarantee high thrombolysis rates. It is important to take a long hard look at the treatment pathways within the individual hospitals.
The mandatory quality assurance program is the instrument by which the process of improvement can be monitored at the regional and state level.
Acknowledgments
Translated from the original German by Kersti Wagstaff MA.
Footnotes
Conflict of interest statement
Professor Stolz has received lecture fees from Boehringer Ingelheim, Bracco and Sanofi-Aventis. In the course of clinical studies he has received support from Schering and Bracco. Research projects initiated by him have received funding from Sanofi-Aventis.
Professor Hamann has received consultancy fees from Boehringer, MSD Sharp & Dohme. He has received reimbursement of conference and continuing education registration fees and travel expenses from Sanofi-Aventis. He has also received lecture fees from Sanofi-Aventis and Boehringer.
Professor Kaps has received lecture fees from Sanofi-Aventis and Shire, and financial support in clinical studies from Boehringer Ingelheim, Shire, and Bracco. Research projects initiated by him have received funding from Boehringer Ingelheim and Bracco.
Dr. Misselwitz declares that he has no conflict of interest.
References
- 1.Heuschmann PU, Biegler MK, Busse O, et al. Development and implementation of evidence-based indicators for measuring quality of acute stroke care: the Quality Indicator Board of the German Stroke Registers Study Group (ADSR) Stroke. 2006;37:2573–2578. doi: 10.1161/01.STR.0000241086.92084.c0. [DOI] [PubMed] [Google Scholar]
- 2.Ringleb P, Schellinger PD Hacke W for the ESO Writing Committee. The European Stroke Organization (ESO) Executive Committee and the ESO Writing Committee: Guidelines for management of ischemic stroke and transient ischemic attack 2008. www.eso-stroke.org/recommendations.php?cid=9&sid=1, Last accessed on. 2011 Mar 15; [Google Scholar]
- 3.Dirks M, Niessen LW, Peter J, Koudstaal PJ, et al. Intravenous thrombolysis in acute ischaemic stroke: from trial exclusion criteria to clinical contraindications. An international Delphi study. J Neurol Neurosurg Psychiatry. 2007;78:685–689. doi: 10.1136/jnnp.2006.102798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 45 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]