Abstract
Objective
Elucidation of clinically relevant subtypes has been proposed as a means of advancing treatment research, but classifying anorexia nervosa (AN) patients into restricting and binge-eating/purging types has demonstrated limited predictive validity. This study aimed to evaluate whether an approach to classifying eating disorder patients based on comorbid personality psychopathology has utility in predicting treatment response and readmission in patients with AN.
Method
Data were collected from 154 AN patients (M[SD] age = 25.6[9.4] years; 95.5% female; 96.8% Caucasian) at admission, discharge, and three months post-discharge from intensive treatment. Latent profile analysis of personality traits assessed at admission was performed to classify participants into personality subtypes, which were then used to predict outcomes at discharge and risk of readmission.
Results
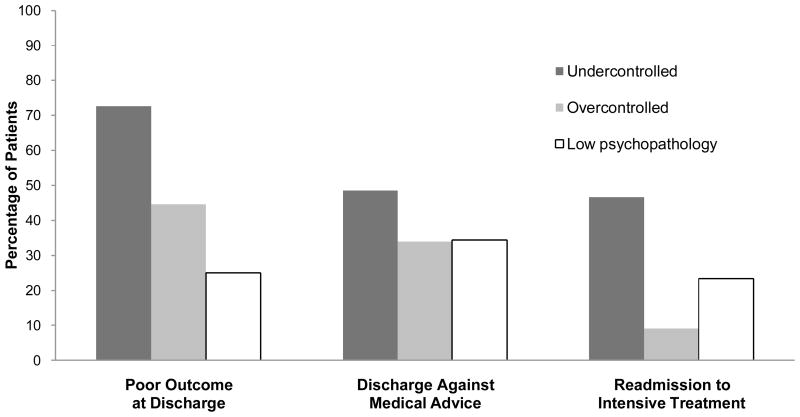
The best-fitting model identified three personality subtypes (undercontrolled, overcontrolled, low psychopathology) that contributed significantly to multivariate models predicting study outcomes. Undercontrolled patients were more likely to have a poor outcome at discharge than overcontrolled (OR = 3.56, p = .01) and low psychopathology patients (OR = 11.23, p <.001). Undercontrolled patients also had a greater risk of discharge against medical advice (HR = 2.08, p = .02) and readmission than overcontrolled patients (HR = 3.76, p = .009). Binge-eating/purging versus restricting subtypes did not predict discharge against medical advice or readmission in the multivariate models.
Conclusions
Findings support the clinical utility of personality subtypes in AN. Future work is needed to identify mechanisms that explain diminished treatment response in undercontrolled patients and to develop interventions for this high-risk group.
Keywords: anorexia nervosa, subtypes, personality, latent profile analysis, treatment
Anorexia nervosa (AN) is a serious eating disorder characterized by maintenance of a significantly low body weight, intense fear of gaining weight or becoming fat, and cognitive disturbances in the way in which body weight or shape are experienced (American Psychiatric Association [APA], 1994). Although it is relatively uncommon, with a lifetime prevalence of approximately 1% in women (Hoek & van Hoeken, 2003), AN is a critical public health concern for several reasons. First, AN is associated with serious medical complications including electrolyte disturbances, cardiovascular dysfunction, renal impairment, and osteoporosis (Sharp & Freeman, 1993). Second, AN often co-occurs with other psychiatric conditions, particularly mood disorders, anxiety disorders, substance misuse, and personality psychopathology (O’Brien & Vincent, 2003). Third, AN treatment is costly relative to other psychiatric disorders. Using an extensive insurance claim database, Striegel-Moore, Leslie, Petrill, Garvin, and Rosenheck (2000) found that one-year treatment costs for AN were comparable to those for schizophrenia. Fourth, AN frequently runs a chronic course (Steinhausen, 2002). Finally, AN is associated with substantial mortality consequent to malnutrition and suicide (Agras et al., 2004). Roughly 5% of individuals with AN die per decade of the illness (Sullivan, 1995); the standardized mortality ratio is 10.5 (Birmingham, Su, Hlynsky, Goldner, & Gao, 2005).
Despite the morbidity and mortality associated with AN, the development of effective treatments for this illness has been a challenge. Although structured behavioral interventions provided in intensive settings (e.g., inpatient, day hospital) are effective at restoring weight and reducing aberrant eating behaviors in the short-term (Attia & Walsh, 2007), longitudinal studies indicate that 30–50% of individuals who receive intensive treatment for AN relapse or require additional hospitalization in the year following discharge (Carter, Blackmore, Sutandar-Pinnock, & Woodside, 2004; Treat, McCabe, Gaskill, & Marcus, 2008). Research focused on the development of psychotherapeutic and pharmacologic interventions for AN also has been disappointing, with few treatments showing consistent benefits across studies (Bulik, Berkman, Brownley, Sedway, & Lohr, 2007). A number of factors have contributed to the difficulty in developing effective treatments for AN including the rarity of the illness, reluctance of many patients to seek treatment, and expense involved in providing the intensive care required for severely affected individuals (Attia, 2010). In addition, there are few consistent predictors of treatment response in AN to guide development of novel interventions. There is some evidence that individuals who present for treatment early in the course of illness, particularly those who are younger than age 18, have a better outcome (Agras et al., 2004). Conversely, patients who present for treatment at very low weight and those with a longer duration of illness or a history of psychiatric hospitalization fare more poorly (Agras et al., 2004; Treat et al., 2008). However, these predictors are difficult to modify and thus do not provide useful targets for intervention.
One strategy for advancing treatment research in AN is to determine whether there are any clinically relevant subtypes within the AN population. This approach is based on the premise that a better understanding of variability within populations carrying the same categorical diagnosis offers hope for maximizing the proportion of patients who achieve recovery (Angst & Cassano, 2005). Variations in treatment response among individuals with AN may be due, in part, to within-group differences in behavioral or biological factors that could be targeted by novel, subtype-specific interventions (National Institute of Mental Health [NIMH], 2008). Conversely, a failure to recognize to clinically relevant subtypes in AN may hinder treatment research if the interventions studied target a heterogeneous clinical population.
Patients with AN currently are classified into restricting (AN-R) and binge-eating/purging (AN-BP) subtypes, but this approach has had limited utility in informing treatment development (for review, see Peat, Mitchell, Hoek, & Wonderlich, 2009). Longitudinal research has found few differences between AN-R and AN-BP in treatment utilization, time to recovery, rates of relapse, or mortality (Eddy et al., 2002; Keel et al., 2002). Moreover, several studies have documented that a majority of patients with AN-R eventually develop binge/purge behaviors (Peat et al., 2009), suggesting that AN-R and AN-BP represent alternate phases in the course of illness rather than distinct subtypes (Eddy et al., 2002).
Another approach to identifying clinically relevant subtypes is to focus on comorbid psychopathology. For example, there is increasing interest in the utility of subtyping individuals with eating disorders based on patterns of within-group heterogeneity in personality psychopathology. With few exceptions (Thompson-Brenner et al., 2008; Wagner et al., 2006), studies have found three personality subtypes in patients with eating disorders: 1) an undercontrolled subtype characterized by impulsivity and behavioral or emotional dysregulation; 2) an overcontrolled subtype characterized by inhibition and constraint; and 3) a low psychopathology subtype characterized by normative levels of personality functioning (for review, see Wonderlich, Joiner, Keel, Williamson, & Crosby, 2007). Moreover, research has found differences among these subtypes in patterns of Axis I and II comorbidity, family history of psychopathology, rates of childhood abuse, and psychosocial functioning (Holliday, Landau, Collier, & Treasure, 2005; Steiger et al., 2010; Westen & Harnden-Fischer, 2001). Cross-sectional studies also have documented that individuals with the undercontrolled subtype are more likely to have a history of psychiatric hospitalization and are less likely to be rated by their therapists as recovered following treatment than the overcontrolled and low psychopathology subtypes (Thompson-Brenner & Westen, 2005; Westen & Harnden-Fischer, 2001).
There are several reasons to focus on personality subtypes as a strategy for identifying treatment targets in patients with AN. First, personality traits feature prominently in many models of the etiology and maintenance of anorexic symptoms (e.g., Schmidt & Treasure, 2006; Strober, 2004). Second, although the prototypical personality profile in AN emphasizes overcontrolled traits (Wonderlich, Lilenfeld, Riso, Engel, & Mitchell, 2005), many individuals with AN engage in behaviors that typically are associated with undercontrolled personality psychopathology (e.g., binge-eating or purging, self-injury, substance misuse) (Paul, Schroeter, Dahme, & Nutzinger, 2002; Peat et al., 2009; Root et al., 2010). Third, there is growing evidence that maladaptive personality traits are treatable and, in fact, may moderate the effects of psychotherapeutic and pharmacologic interventions (Krueger & Eaton, 2010). Finally, two studies have documented personality subtypes in patients with AN. For example, Strober (1983) reported preliminary evidence that adolescents with AN assigned to a personality subtype characterized by dependency, low frustration tolerance, and chronic dysphoria (similar to the undercontrolled subtype) gained less weight and showed less improvement in the psychological correlates of disordered eating during inpatient treatment than individuals classified in groups that resembled the overcontrolled and low psychopathology subtypes. More recently, Holliday et al. (2005) characterized personality subtypes in a sample of women with lifetime AN, and found that individuals with lower levels of personality psychopathology were more likely to have a family history of eating disorder than those with “broad” (p. 533) or avoidant personality dysfunction. However, the majority of participants in this report were in remission from AN symptoms, and no information about the clinical utility of personality subtypes in predicting response to treatment was provided.
In summary, the identification of clinically relevant subtypes in patients with AN may have important implications for the development of novel interventions. Although personality subtypes have conceptual appeal as a means of classifying subgroups of AN patients, few studies have employed this approach in samples comprised exclusively of individuals with AN, and no research has used modern statistical methodology and a prospective design to evaluate the clinical utility of personality subtypes as predictors of treatment response in AN or other eating disorders. Accordingly, this study had three aims. First, we sought to characterize personality subtypes in patients with AN using latent profile analysis (LPA) (Vermut & Magidson, 2005). LPA confers certain advantages over other statistical techniques for identifying subgroups (e.g., cluster analysis) in that it uses a general probability model that allows for unequal variances in each group and provides formal statistical procedures for determining the optimal number of classes (Magidson & Vermunt, 2002). We hypothesized that there would be three personality subtypes in patients with AN and that they would show differences in clinical characteristics assessed at baseline, consistent with the undercontrolled, overcontrolled, and low psychopathology groups. Second, we sought to evaluate the clinical utility of personality subtypes as predictors of response to intensive treatment (i.e., inpatient or day hospital) for AN. Approximately 50% of AN patients require intensive treatment at some point during their illness (Agras et al., 2004); thus, identifying predictors of intensive treatment response has considerable generalizability in this population. We hypothesized that individuals assigned to the undercontrolled subtype would have poorer outcomes at discharge from intensive treatment and higher rates of readmission within three months of discharge than those assigned to the overcontrolled and low psychopathology subtypes. Readmission is a particularly important clinical outcome because it diminishes the cost-effectiveness of short-term intensive treatment (Wiseman, Sunday, Klapper, Harris, & Halmi, 2001) and is associated with a more protracted course of illness (Steinhausen, Grigoroiu-Serbanescu, Boyadjieva, Neumarker, & Winkler Metzke, 2008). Finally, because it is important to evaluate whether a novel classification scheme offers benefit over existing approaches (Wonderlich et al., 2007), we aimed to examine the utility of personality subtypes relative to AN-R and AN-B/P as predictors of intensive treatment response. We hypothesized that personality subtypes would be superior to restricting and binge-eating subtypes in predicting clinical outcomes.
Method
Participants
Participants were recruited from consecutive, unique admissions to the inpatient and day hospital eating disorder programs at an academic medical center between April 2008 and August 2010. Study inclusion criteria were: 1) age ≥ 16 years, 2) body mass index (BMI; kg/m2) < 18.5 or BMI percentile < 10 (patients aged 16–19 years) at admission, and 3) medically stable. Patients less than 16 years of age were excluded because some of the items on the personality measure we used are not appropriate for this age group (Clark et al, in press), and no comparable, age-appropriate personality measure was available. Medical stability was required to mitigate the effects of acute starvation on cognitive functioning (Attia, 2010). Patients were excluded from the study if they were psychotic or had a chart diagnosis of mental retardation (n = 4). Two hundred eight individuals were invited to participate. After the study was described, 154 patients (74.0%) signed consent forms approved by the local Institutional Review Board (assent for individuals under 18 years) and completed baseline study assessments.
Participants (N = 154) had a mean age of 25.6 years (SD = 9.4) and a mean BMI of 15.8 (SD = 1.7) at admission for intensive treatment. The sample was primarily female (95.5%) and Caucasian (96.8%). Approximately half the sample (n = 73; 47.4%) had a history of previous hospitalization for eating disorder; the mean duration of illness was 7.9 years (SD = 8.2).
Treatment
The inpatient and day hospital programs at our center have been have been described previously (Treat et al., 2008). The milieus are similar in that they are informed predominantly by cognitive behavioral (CBT) and dialectical behavioral therapy (DBT) principles, and the primary treatment modalities are group therapy and meal support. Examples of the CBT and DBT techniques employed include problem solving, cognitive restructuring, validation, and the acquisition of mindfulness, emotion regulation, and distress tolerance skills. The inpatient setting provides 24-hour care, while the day hospital program operates 32 hours per week. Many patients step-down to the day hospital program following inpatient treatment, but there are instances in which low-weight patients are managed exclusively with day hospital care (Attia & Walsh, 2007). Conversely, some individuals are treated only on the inpatient unit. Ninety-one participants (59.1%) received inpatient care only, 20 (13.0%) received day hospital care only, and 43 (27.9%) were treated in both the inpatient and day hospital programs.
Procedure
As part of an ongoing longitudinal study, participants completed assessments conducted by research staff independent of the treatment team within approximately two weeks of admission for intensive treatment (M [SD] = 13.1 [10.9] days after admission), at discharge, and at a median of 93 days (IQR = 9.5) after discharge. Baseline assessments were delayed for two weeks after admission to enable participants to achieve medical stability prior to enrolling in the study. Assessors were bachelor’s-, master’s-, or doctoral-level clinicians who were trained and supervised by two licensed psychologists during weekly consensus meetings. Interviews were audiotaped, and 10% were re-rated by independent clinicians to establish reliability.
Measures
Baseline measures
An investigator-designed questionnaire was used to document demographics and treatment history, and participants were interviewed using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I) (First, Spitzer, Gibbon, & Williams, 2007) to diagnose eating, mood, anxiety, and substance use disorders. Diagnoses of AN were made using Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria with two exceptions: 1) amenorrhea was not required because this criterion has been shown to have limited validity (Attia & Roberto, 2009); and 2) 11 patients who entered intensive treatment with a BMI < 17.5, but denied fear of fatness were included, consistent with descriptions of “non-fat-phobic AN” (Becker, Thomas, & Pike, 2009). The psychometric properties of the SCID are well-documented (First, Gibbon, Spitzer, & Williams, 2002); inter-rater reliabilities in the current study ranged from κ = 0.86 for lifetime anxiety disorder to κ = 1.00 for AN, lifetime mood disorder, and lifetime substance use disorder.
AN diagnoses and the severity of eating disorder psychopathology were confirmed using the clinician-rated Eating Disorder Examination, 16th edition (EDE) (Fairburn, Cooper, & O’Connor, 2008). The EDE has acceptable internal consistency (α = 0.68–0.90) and inter-rater reliability (κ = 0.70–0.99) (Fairburn & Cooper, 1993). In the current study, we focused on the EDE Global score as a measure of the severity of eating disorder psychopathology at baseline and the frequency of binge-eating and purging (i.e., self-induced vomiting, laxative misuse, diuretic misuse) during the three months prior to assessment to diagnose AN-R versus AN-B/P. Patients were classified as having AN-B/P if they engaged in episodes of binge-eating or purging ≥ 1/month for the prior three months (Peat et al., 2009). Inter-rater reliabilities for the EDE Global score, number of binge-eating episodes, number of purging episodes, and AN-B/P diagnosis were ρ = 0.97, r = 0.98, r = 0.99, and κ = 1.00, respectively.
Personality psychopathology was measured using the Schedule for Nonadaptive and Adaptive Personality, 2nd edition (SNAP-2), a factor-analytically-derived, 390-item self-report questionnaire designed to assess personality characteristics in the normal and abnormal range (Clark, Simms, Wu, & Casillas, in press). Items are rated using a true-false format and summed to produce 15 trait and temperament scales. Many of the scales are bipolar; that is, both high and low scores indicate psychopathology. T-scores are provided to facilitate interpretation of results; extreme scores (T < 35 or T > 65) suggest the presence of psychopathology, while moderate scores (T = 35–45 or T = 55–65) suggest a tendency towards personality dysfunction. The SNAP-2 scales have demonstrated good to excellent internal consistency (median α = 0.85) and adequate test-retest reliability (median r = 0.68) in individuals seeking treatment for mental disorders (Clark et al., in press). Internal consistencies for the SNAP-2 scales in the current sample ranged from α = 0.78 to α = 0.89 (median α = 0.85).
Discharge measures
Participants’ medical records were reviewed to obtain information about: 1) height and weight at admission and discharge, 2) days in intensive treatment, 3) level of care (inpatient, day hospital, both), and 4) discharge type (planned, against medical advice). A modified version of the EDE designed to cover the period of time since the baseline assessment also was administered.1 Participants who discharged less than one week after the baseline assessment (n = 25) were not re-interviewed.
The primary outcome at discharge was a categorical rating adapted from the Morgan-Russell criteria (Morgan & Russell, 1975) and more recent conceptualizations of symptom improvement in AN (Couturier & Lock, 2006). Participants with a “good” outcome had a BMI ≥ 18.5, no episodes of binge-eating or purging during the past 28 days, and an EDE Global score within two standard deviations of community norms (Fairburn et al., 2008). An “intermediate” outcome was assigned to participants who were partially weight-restored (BMI ≥ 17.5) and had fewer than four episodes of binge-eating or purging during the past 28 days. Finally, participants with a BMI ≤ 17.5 and those who reported ≥ 4 episodes of binge-eating or purging during the past 28 days were rated as having a “poor” outcome. We categorized patients with ≥ 4 episodes of binge-eating or purging during the past 28 days as having a poor outcome, regardless of weight status, because these frequencies reach threshold for proposed DSM-5 diagnoses of bulimia nervosa and binge eating disorder (Eating Disorders Work Group, 2011), and we reasoned that improvement in weight accompanied by crossover to another eating disorder was indicative of a poor response to intensive treatment.
Post-discharge measure
Treatment utilization during the three months after discharge was assessed using the McKnight Follow-up of Eating Disorders (M-FED), a clinician-administered measure that has been used in several multicenter and treatment studies to document service utilization (e.g., Agras, Crow, Mitchell, Halmi, & Bryson, 2009). Participants were queried regarding dates of admission to intensive treatment, reasons for intensive treatment, and receipt of outpatient psychotherapy and psychotropic medications. Inter-rater reliabilities for time to readmission and presence of readmission (rated yes/no) were r = 1.00 and κ = 1.00.
Statistical Analysis
Latent profile analysis (LPA), an extension of latent class analysis that allows for the use of continuous, ordinal, or categorical “indicator” variables to group individuals into unobserved (i.e., latent) classes based on the principle of conditional independence (Vermut & Magidson, 2005), was performed to identify personality subtypes in the current study. Indicator variables were T-scores on four SNAP-2 scales selected for their conceptual relevance in distinguishing between the undercontrolled and overcontrolled personality subtypes, as well as data indicating that they reflect basic dimensions of personality common to several models of personality functioning (Widiger, Livesley, & Clark, 2009): 1) Self-Harm (neuroticism versus emotional stability); 2) Exhibitionism (extraversion versus introversion); 3) Aggression (antagonism versus agreeableness); and 4) Impulsivity (undependability versus conscientiousness/constraint). Time to assessment was included as a covariate to minimize the influence of between-subject differences in the number of days between admission to treatment and initiation of study procedures. Prior to conducting the LPA, data were screened for skewness and outliers. The distribution for time to assessment was positively skewed; however, because results were similar using transformed and untransformed data, skewness was not corrected in the final model.
One- to 10-class models were fit using Latent GOLD version 4.5 (Statistical Innovations, Inc., Belmont, MA). Parameters were estimated using maximum likelihood. Determination of the number of classes was based on minimization of the Bayesian Information Criterion (BIC) (Schwarz, 1978) and Consistent Akaike Information Criterion (cAIC) (Bozdogan, 1987). The bootstrap likelihood ratio test was used to compare successive models; a significant change in −2 log-likelihood indicated that the model with the larger number of classes provided a better fit to the data (Vermut & Magidson, 2005). Assignment of class membership was based on posterior Bayesian probabilities. The conditional independence assumption (i.e., the assumption that indicators are uncorrelated within each class) was evaluated by examining the correlations between residual covariances for observed indicators (i.e., bivariate residuals). Finally, because the current sample is smaller than is typically used for LPA (Leoutsakos, Zandi, Bandeen-Roche, & Lyketsos, 2010), we performed a bootstrapping procedure developed to test the stability of LPA findings in small samples (Wonderlich, Crosby, et al., 2005). Specifically, separate LPAs were conducted on 100 consecutive random samples consisting of 90% of the original sample, and stability was evaluated in terms of the number of classes identified and a comparison of individual class membership between the original and bootstrapped samples.
Analysis of covariance (ANCOVA) with Bonferroni-corrected covariate-adjusted contrasts was performed to characterize personality psychopathology in the subtypes based on the LPA indicators, controlling for time to assessment. Differences among the subtypes in baseline demographic and clinical characteristics were examined using analysis of variance with Tukey’s HSD post-hoc tests (continuous variables) or chi-squares (categorical variables). To protect against Type I error, α was set at .01.
To evaluate differences among the subtypes in response to intensive treatment, we focused on two indicators of negative treatment response: 1) poor outcome at discharge, and 2) discharge against medical advice (similar to treatment drop-out). As an initial step, univariate analyses were performed to identify covariates based on clinical relevance and previous research. Next, multivariate analyses were conducted using a sequential approach in which significant covariates were entered in the first step followed by planned contrasts comparing the personality subtypes in the second step. Binge-eating/purging versus restricting subtype was included as a covariate in all models to evaluate the incremental validity of personality subtypes relative to an existing classification scheme (Aim 3). Improvement in model fit from step 1 to step 2 served as an index of the utility of personality subtypes as predictors of treatment response relative to existing predictors. Poor outcome at discharge was predicted using logistic regression. Risk of discharge against medical advice was evaluated using Cox proportional hazards regression in which data were censored at the point at which participants terminated intensive treatment.
Finally, Cox proportional hazards regression was performed to examine differences among the personality subtypes with respect to readmission for intensive treatment within three months of discharge. Data were censored at the date of the follow-up interview or 93 days after discharge, whichever came first. The sequential regression procedure described above was used to evaluate the utility of personality subtypes relative to other predictors of readmission and poor outcome in AN. Analyses were performed using PASW version 18 (SPSS Inc., Chicago, IL).
Results
Characterization of Personality Subtypes
LPA of the full sample revealed a three-class solution, which was confirmed by all 100 bootstrap samples2 (see Table 1). As expected, the personality profiles of the groups conformed to the undercontrolled, overcontrolled, and low psychopathology subtypes (see Table 2). Individuals assigned to class 1 (n = 66; 42.9%) had elevated scores on the Self-Harm, Aggression, and Impulsivity scales, reflecting poor self-esteem, emotion regulation difficulties, trouble controlling anger, and recklessness (Clark, et al., in press) (undercontrolled). In contrast, patients assigned to class 2 (n = 56; 36.4%) had elevated scores on Self-Harm coupled with low scores on Exhibitionism and moderately low scores on Impulsivity, which suggest tendencies towards poor self-esteem, social inhibition, and constraint (Clark, et al., in press) (overcontrolled). Finally, individuals assigned to class 3 (n = 32; 20.8%) had normative scores on all four SNAP-2 scales, consistent with a low psychopathology subtype.
Table 1.
Information Criteria for 1- to 10-Class Latent Profile Analysis Models
| Number of Classes | Parameters | LL | BIC | cAIC |
|---|---|---|---|---|
| 1 | 8 | −2417.49 | 4875.28 | 4883.28 |
| 2 | 18 | −2347.06 | 4784.79 | 4802.79 |
| 3a | 28 | −2305.48 | 4751.99 | 4779.99 |
| 4 | 38 | −2281.10 | 4753.60 | 4791.60 |
| 5 | 48 | −2268.27 | 4778.32 | 4826.32 |
| 6 | 58 | −2255.54 | 4803.23 | 4861.23 |
| 7 | 68 | −2239.77 | 4822.06 | 4890.06 |
| 8 | 78 | −2221.80 | 4836.48 | 4914.48 |
| 9 | 88 | −2224.98 | 4893.2 | 4981.20 |
| 10 | 98 | −2214.82 | 4923.26 | 5021.26 |
Note. Bold text designates the best-fitting model. LL = Log-likelihood; BIC = Bayesian Information Criterion; cAIC = Consistent Akaike Information Criterion.
The bootstrap likelihood ratio test comparing the 3-class and 2-class models was significant, p < .001. Examination of the bivariate residuals (BVR) for the 3-class model indicated that the conditional independence assumption was adequately met (BVRs = 1.16–3.23).
Table 2.
Demographic and Clinical Characteristics of the Personality Subtypes
| Variable | Class 1: Undercontrolled (n = 66) | Class 2: Overcontrolled (n = 56) | Class 3: Low Psychopathology (n = 32) | Test Statistic | p | Effect Size† | |||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||||
| Self-Harm (SNAP-2 T-score) | 83.72a | 12.88 | 69.82b | 15.9 | 52.31c | 6.77 | F (3, 150) = 41.69 | <.001 | .46 |
| Exhibitionism (SNAP-2 T-score) | 47.62a | 9.53 | 37.25b | 3.20 | 54.44c | 9.56 | F (3, 150) = 35.83 | <.001 | .42 |
| Aggression (SNAP-2 T-score) | 61.44a | 13.07 | 46.85b | 5.49 | 47.63b | 6.07 | F (3, 150) = 30.40 | <.001 | .38 |
| Impulsivity (SNAP-2 T-score) | 58.35a | 10.68 | 43.04b | 4.63 | 47.51b | 6.28 | F (3, 150) = 38.82 | <.001 | .44 |
| Age (years) | 25.15 | 8.78 | 26.2 | 8.81 | 25.90 | 11.71 | F (2, 151) = 0.20 | .82 | .003 |
| Body mass index at admission | 16.02 | 1.64 | 15.54 | 1.90 | 15.98 | 1.66 | F (2, 151) = 1.28 | .28 | .02 |
| Duration of illness (years) | 8.45 | 8.22 | 7.84 | 7.57 | 6.81 | 9.49 | F (2, 151) = 0.43 | .65 | .006 |
| EDE Global score at baseline | 3.44a | 1.39 | 3.33ab | 1.34 | 2.54b | 1.40 | F (2, 151) = 4.92 | .009 | .06 |
| n | % | n | % | n | % | ||||
| Female | 65 | 98.48 | 53 | 94.64 | 29 | 90.63 | Χ2 (2) = 3.20 | .20 | .14 |
| Non-white ethnicity | 2 | 3.03 | 1 | 1.79 | 1 | 3.13 | Χ2 (2) = 0.24 | .89 | .04 |
| Binge-eating/purging subtype | 52 | 78.79a | 26 | 46.43b | 16 | 50.00b | Χ2 (2) = 15.41 | <.001 | .32 |
| ≥ 2 hospitalizations for ED | 38 | 57.58a | 27 | 48.21ab | 8 | 25.00b | Χ2 (2) = 9.20 | .01 | .24 |
| Lifetime mood disorder | 57 | 86.36 | 40 | 71.43 | 22 | 68.75 | Χ2 (2) = 5.52 | .06 | .19 |
| Lifetime anxiety disorder | 47 | 71.21 | 37 | 66.07 | 14 | 43.75 | Χ2 (2) = 7.25 | .03 | .22 |
| Lifetime substance use disorder | 36 | 54.55a | 14 | 25.00b | 10 | 31.25ab | Χ2 (2) = 12.13 | .002 | .28 |
Note. Subscripts that differ represent pairwise differences between the subtypes at p < .01. SNAP-2 = Schedule for Nonadaptive and Adaptive Personality, 2nd Edition; EDE = Eating Disorder Examination; ED = Eating disorder
Effect sizes for ANOVAs are partial η2; effect sizes for chi-squares are ϕ.
Demographic and clinical characteristics of the subtypes are reported in Table 2. Of note, there were no differences among the groups in age, BMI at admission for intensive treatment, or duration of illness, suggesting that the personality subtypes were not a proxy for AN severity or chronicity. Rates of AN-B/P were highest in the undercontrolled group, although approximately half of individuals in the overcontrolled and low psychopathology subtypes also met criteria for AN-B/P. Undercontrolled participants were more likely than overcontrolled participants to have a history of substance use disorder. Undercontrolled participants also had higher baseline EDE Global scores and were more likely to have a history of repeated hospitalizations for eating disorder than the low psychopathology subtype.
Personality Subtypes and Response to Intensive Treatment
Prior to examining the utility of personality subtypes as predictors of response to intensive treatment, we conducted a series of preliminary analyses to characterize treatment in the personality subtypes. There were no differences among the groups in rate of weight gain (p = .90), level of care (p = .16), or BMI at discharge (p = .11). Undercontrolled patients spent fewer days in treatment than overcontrolled and low psychopathology patients (M [SD] = 34.7 [20.7] versus 49.7 [23.2] and 50.0 [28.8]), but this effect was not significant after controlling for level of care and binge-eating/purging versus restricting subtype, F(2, 149) = 2.70, p = .07, partial η2=.04.
Next, we performed univariate analyses to identify covariates for the regressions predicting poor outcome at discharge and risk of discharge against medical advice. Seven variables emerged as significant univariate predictors of poor outcome at discharge (i.e., age, BMI at admission, AN-R versus AN-B/P, days in intensive treatment, duration of AN symptoms, discharge against medical advice, and repeated [i.e., ≥ 2] hospitalizations for eating disorder), and two variables emerged as significant univariate predictors of risk of discharge against medical advice (i.e., AN-R versus AN-B/P and repeated hospitalizations for eating disorder).3
After controlling for covariates, personality subtypes contributed significantly to the model predicting poor outcome at discharge from intensive treatment, Step 2 Χ2 (2) = 17.67, p < .001, Δ Cox and Snell R2 = .08; Overall Χ2 (9) = 74.16, p < .001, Cox and Snell R2 = .38. Planned contrasts revealed that individuals in the undercontrolled subtype were more likely than the overcontrolled (OR = 3.56, p = .01, 95% CI [1.31, 9.65]) and low psychopathology (OR = 11.23, p <.001, 95% CI [3.19, 39.52]) subtypes to have a poor outcome at discharge (Figure 1).
Figure 1.
Clinical outcomes among anorexia nervosa patients in the undercontrolled, overcontrolled, and low psychopathology personality subtypes. Sample sizes for poor outcome at discharge and discharge against medical advice are: undercontrolled (n = 66), overcontrolled (n = 56), and low psychopathology (n = 32). Sample sizes for readmission to intensive treatment are: undercontrolled: (n = 58), overcontrolled (n = 55), low psychopathology (n = 30).
Personality subtypes also contributed significantly to the model predicting risk of discharge against medical advice, Step 2 Χ2 (2) = 6.78, p < .05, Δ pseudo R2 = .01; Overall Χ2 (4) = 16.88, p < .01, pseudo R2 = .03. Specifically, undercontrolled patients were at greater risk for discharge against medical advice than overcontrolled patients (HR = 2.08, p = .02, 95% CI [1.14, 3.78]). However, the difference between undercontrolled patients and the low psychopathology group was not significant (HR = 1.96, p = .08, 95% CI [.92, 4.16]) (Figure 1).
Personality Subtypes and Readmission to Intensive Treatment
One hundred forty-three participants (92.9%) provided follow-up data, of whom 39 (27.3%) were readmitted to intensive treatment within three months of discharge. In addition, one undercontrolled patient died during the follow-up period, but was not included in the analyses because her treatment status was unknown. Reasons for readmission included exacerbation of eating disorder symptoms (n = 32), suicide attempts (n = 4), and substance use (n = 3). There were no differences among the personality subtypes in reasons for readmission (p = .08) or rate of follow-up (p = .09).4
Univariate analyses identified seven covariates for the Cox regression predicting risk of readmission to intensive treatment within three months of discharge: poor outcome at discharge, days in intensive treatment, AN-R versus AN-B/P, duration of AN symptoms, repeated (i.e., ≥ 2) hospitalizations for psychiatric disorder, lifetime mood disorder, and lifetime substance use disorder.5 After controlling for these variables, personality subtypes contributed significantly to the model predicting risk of readmission, Step 2 Χ2 (2) = 9.56, p < .01, Δ pseudo R2 = .03; Overall Χ2 (9) = 34.07, p < .001, pseudo R2 = .10. Planned contrasts documented that undercontrolled patients were at greater risk for readmission to intensive treatment than overcontrolled patients (HR = 3.76, p = .009, 95% CI [1.40, 10.07]). However, there was no difference between undercontrolled patients and those in the low psychopathology group with respect to risk of readmission (HR = 1.05, p = .91, 95% CI [.42, 2.65]) 6 (see Figure 1).
Clinical Utility of Personality Subtypes Relative to AN-R and AN-B/P
Binge-eating/purging versus restricting subtype was a significant predictor of poor outcome at discharge in the multivariate model (OR = 4.65, p = .002, 95% CI [1.79, 12.09]). However, even before controlling for personality subtypes, binge-eating/purging versus restricting subtype did not contribute significantly to models predicting discharge against medical advice (HR = 1.69, p = .06, 95% CI [.97, 2.93]) or readmission within three months of discharge (HR = 1.31, p = .53, 95% CI [.57, 3.04]).
Discussion
Tailoring interventions to clinically relevant subtypes has been proposed as a strategy for improving treatment response in psychiatric populations (Angst & Cassano, 2005; NIMH, 2008), but subtyping individuals with AN into restricting versus binge-eating/purging types has had limited predictive validity (Peat et al., 2009). This study provides the first evidence, to our knowledge, that an alternative approach to subtyping individuals with eating disorders based on comorbid personality psychopathology has utility in predicting clinical outcomes at discharge from intensive treatment for AN and patterns of treatment-seeking during short-term follow-up. These findings and their implications are discussed below.
The current study contributes to and extends extant research documenting the validity of personality subtypes in individuals with eating disorders. Using LPA, we identified three personality subtypes (undercontrolled, overcontrolled, low psychopathology) that differed with respect to baseline clinical characteristics and intensive treatment outcomes. Of note, our findings suggest that compared to overcontrolled AN patients, individuals with undercontrolled AN have a poorer initial response to intensive treatment and an elevated risk of readmission within three months of discharge, even after controlling for other predictors of negative treatment response and rehospitalization. In contrast, subtyping AN patients into restricting versus binge-eating/purging types was not associated with one index of negative treatment response (i.e., discharge against medical advice) or readmission to intensive treatment in the multivariate models. These findings converge with previous work, which suggests that a classification scheme based on comorbid personality psychopathology may have more clinical utility than current approaches to conceptualizing eating disorders (Westen & Harnden-Fischer, 2001). Moreover, this study extends the literature on personality subtypes in eating disorders by documenting that this approach has utility in predicting longitudinal, as well as cross-sectional, outcomes. Finally, subtypes similar to those identified in this sample have been described in other psychiatric groups (e.g., Miller, Kaloupek, Dillon, & Keane, 2004), and a trait-based approach to conceptualizing personality psychopathology is consistent with proposed revisions to the classification of personality disorders in DSM-5 (Personality and Personality Disorders Work Group, 2010). Thus, subtyping individuals based on comorbid personality psychopathology may have utility across diagnostic categories as a means of identifying clinically relevant subgroups.
The present findings also have implications for the treatment of AN. Although a standard behavioral intervention emphasizing group therapy and meal support was reasonably effective for the overcontrolled and low psychopathology subtypes, outcomes were demonstrably poorer for patients with undercontrolled AN. There is substantial evidence that personality disorder comorbidity is associated with attenuated treatment response and increased treatment seeking among individuals with Axis I disorders, but most studies have failed to identify specific patterns of personality psychopathology that predict poor outcomes (for review, see Reich, 2003; also see, Keel et al., 2002). Some data have suggested that impulsivity is associated with a poor response to psychotherapeutic interventions for BN (Wonderlich et al., 2007); however, few studies have examined impulsive personality traits in relation to treatment response in AN. This may be due, in part, to concerns about the validity of assessing personality traits in underweight individuals (Cassin & von Ranson, 2005). Although starvation may exacerbate some personality features, the results of this study suggest that within-group differences in the manifestation of personality psychopathology in patients with AN have important implications for treatment response. In particular, the current data suggest that a presentation characterized by emotion dysregulation, aggression, and impulsivity is associated with a poor response to intensive treatment for AN and high rates of readmission during short-term follow-up.
Future work is needed to identify mechanisms that explain poor short-term outcomes in individuals with undercontrolled AN. For example, there is evidence that a diminished ability to tolerate distress is associated with early drop-out among individuals receiving residential treatment for substance use (Daughters et al., 2005). Likewise, negative urgency, a form of impulsivity defined as the tendency to act rashly when experiencing negative mood, has been associated with disordered eating (Fischer, Smith, & Cyders, 2008). AN treatment is distressing for many patients. The goals of weight gain and decreasing aberrant eating behaviors set by treatment providers often are inconsistent with patient goals of thinness and self-control (Vitousek, Watson, & Wilson, 1998). If individuals with undercontrolled AN have poorer distress tolerance skills or are more likely to act rashly in the presence of negative mood, these characteristics might place them at greater risk for treatment drop-out and negative clinical outcomes. Moreover, the structured environment of an inpatient or day hospital setting may be particularly provocative for undercontrolled AN patients given the expectations that they will follow a prescribed meal plan, participate in supportive meal sessions and therapy groups, and interact effectively with other patients and staff in the milieu (Treat et al., 2008). Ironically, impaired distress tolerance and impulsivity also may make it more difficult for undercontrolled patients to manage stressors outside of an intensive setting, leading to increased reliance on acute care as a form of crisis intervention.
Future studies are needed to evaluate whether distress tolerance and impulsivity mediate response to intensive treatment in individuals with undercontrolled AN, as this may suggest targets for individualized interventions. Although our intensive treatment program includes therapy groups that focus on distress tolerance skills, they may not be sufficient to address the needs of undercontrolled AN patients. An alternative model might be to develop a specific DBT track for undercontrolled AN patients that emphasizes distress tolerance, emotion regulation, and impulse control skills. Several small case series reports have described the use of DBT programs for individuals with eating disorders and comorbid borderline personality disorder, with mixed results (Chen, Matthews, Allen, Kuo, & Linehan, 2008; Kröger et al., 2010; Palmer et al., 2003). However, no study has focused specifically on DBT for AN. Thus, this may be a promising direction for future research.
In this study, overcontrolled patients responded better to intensive treatment than undercontrolled patients and had the lowest rates of readmission. These findings are consistent with research documenting that obsessive-compulsive personality traits are positively related to treatment acceptance and completion in AN patients (Crane, Roberts, & Treasure, 2007), but contrast with evidence that obsessive-compulsive and avoidant personality psychopathology is associated with a more protracted course of illness in individuals with eating disorders (Steinhausen, 2002; Thompson-Brenner et al., 2008). One possible explanation is that factors that predict initial treatment response may differ from those associated with longer-term outcomes. For example, inhibited and constrained personality traits may enable overcontrolled AN patients to tolerate the structured environment of an intensive treatment setting, facilitating better initial outcomes and a decreased risk of premature discharge relative to undercontrolled patients. A shy and cautious interpersonal style also may decrease the likelihood that overcontrolled patients will seek additional intensive treatment in the short-term. In the longer-term, however, overcontrolled personality traits may make it more difficult for individuals to relinquish eating disorder symptoms, leading to a chronic course of illness (Steinhausen, 2002).
The high rate of readmission among patients in the low psychopathology subtype was an unexpected finding. Although this group had the best clinical outcomes at discharge from intensive treatment, nearly one quarter were readmitted within three months. There are several plausible explanations for this result. For example, some individuals may have been incorrectly classified either because they underreported personality psychopathology or had maladaptive personality traits that were not assessed. Another possibility is that the low psychopathology subtype represents a spurious class identified by the LPA, although this seems unlikely given the number of studies that have documented a low psychopathology group using empirical methodology (Wonderlich et al., 2007). A third explanation is that another variable diminished the predictive validity of personality traits in the low psychopathology subtype. For example, changes in comorbid Axis I disorders or psychosocial functioning following discharge from intensive treatment might have contributed to readmission in this group.
The findings of the current study need to be considered in light of several limitations. First, participants were severely ill individuals seeking intensive treatment at an academic medical center. Based on previous research (Thompson-Brenner & Westen, 2005; Westen & Harnden-Fischer, 2001), we think that distinctions among the personality subtypes would be similar in other samples of AN patients, although rates of the undercontrolled subtype might be lower. However, these hypotheses need to be tested. Second, although the sample is large for a single-site investigation of AN, it is smaller than is recommended for LPA (Leoutsakos et al., 2010). The results of the bootstrapping procedure provide reassurance that the subtypes are reliable, but future research using larger samples of AN patients is needed to replicate the current findings. Third, outcome classifications at discharge were based on expectations for short-term intensive treatment (Treat et al., 2008) and may not apply in settings in which longer-term intensive treatment is available. Moreover, because this study was conducted in the context of a specific intensive treatment program, it is possible that the results may not generalize to other interventions. Finally, this study did not evaluate personality traits prospectively; thus, we do not know whether personality subtypes are stable over time. We also cannot comment on whether maladaptive personality traits preceded or followed onset of eating disorder symptoms.
In conclusion, this study supports the clinical utility of personality subtypes in patients with AN. Future research is needed to identify the mechanisms responsible for differential treatment response among personality subtypes in AN. In addition, the present findings suggest a need for the development of interventions to improve outcomes among individuals with undercontrolled AN. This work could help to increase the number of AN patients who benefit from treatment and decrease the personal and societal costs of this debilitating illness.
Acknowledgments
This research was supported by K01 MH080020 from the National Institute of Mental Health. We would like to thank Paul Pilkonis for input regarding the assessment of personality psychopathology and Courtney Alesandro, Ashley Bright, Juliana Bandi, Joanna Gould, and Katherine Heron for their contributions to data collection.
Footnotes
Psychometric properties of the discharge EDE were consistent with those of the original measure. Internal consistencies of the subscales ranged from α= 0.60 to α= 0.92. Inter-rater reliabilities for the EDE Global score, number of binge-eating episodes, and number of purging episodes at discharge were ρ= 0.98, r = 1.00, and r = 1.00, respectively.
The mean classification agreement rate between the original and bootstrapped samples was 93.6% (SD = 6.7).
Non-significant univariate predictors of poor outcome at discharge included EDE Global score at baseline and court-ordered treatment (p’s > .10). Non-significant univariate predictors of discharge against medical advice included age, BMI at admission to intensive treatment, EDE Global score at baseline, current major depressive episode, duration of AN symptoms, and court-ordered treatment (p’s > .10). Level of care was not included as a covariate because it was strongly associated with days in intensive treatment, F (2, 151) = 31.70, p < .001.
Although there were no differences among the personality subtypes in completion of follow-up assessments, we reran the Cox regression using the full sample assuming that none of the participants lost to follow-up had been readmitted within three months of discharge. The pattern of results was the same (data available upon request).
Non-significant univariate predictors of readmission included age, BMI at discharge, discharge against medical advice, rate of weight gain during intensive treatment, lifetime anxiety disorder, psychotherapy during follow-up, and pharmacotherapy during follow-up (p’s > .07).
Results were the same when models were fit predicting risk of readmission to intensive treatment for eating disorder, hospitalization for eating disorder, and any hospitalization for eating-related or other psychiatric disorder (data available upon request).
Portions of this manuscript were presented at the 16th annual meeting of the Eating Disorders Research Society; October 8, 2010; Cambridge, MA.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Jennifer E. Wildes, Department of Psychiatry, University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center
Marsha D. Marcus, Department of Psychiatry, University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center
Ross D. Crosby, Neuropsychiatric Research Institute, Fargo, ND
Rebecca M. Ringham, Department of Psychiatry, University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center
Marcela Marin Dapelo, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center.
Jill A. Gaskill, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center
Kelsie T. Forbush, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center
References
- Agras WS, Brandt HA, Bulik CM, Dolan-Sewell R, Fairburn CG, Halmi KA, …Wilfley DE. Report of the National Institutes of Health workshop on overcoming barriers to treatment research in anorexia nervosa. International Journal of Eating Disorders. 2004;35:509–521. doi: 10.1002/eat.10261. [DOI] [PubMed] [Google Scholar]
- Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of eating disorder NOS compared with full eating disorder syndromes. International Journal of Eating Disorders. 2009;42:565–570. doi: 10.1002/eat.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Angst J, Cassano G. The mood spectrum: Improving the diagnosis of bipolar disorder. Bipolar Disorders. 2005;7(Suppl 4):4–12. doi: 10.1111/j.1399-5618.2005.00210.x. [DOI] [PubMed] [Google Scholar]
- Attia E. Anorexia nervosa: Current status and future directions. Annual Review of Medicine. 2010;61:7, 1–7.11. doi: 10.1146/annurev.med.050208.200745. [DOI] [PubMed] [Google Scholar]
- Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? International Journal of Eating Disorders. 2009;42:581–589. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- Attia E, Walsh BT. Anorexia nervosa. American Journal of Psychiatry. 2007;164:1805–1810. doi: 10.1176/appi.ajp.2007.07071151. [DOI] [PubMed] [Google Scholar]
- Becker AE, Thomas JJ, Pike KM. Should non-fat-phobic anorexia nervosa be included in DSM-V? International Journal of Eating Disorders. 2009;42:620–635. doi: 10.1002/eat.20727. [DOI] [PubMed] [Google Scholar]
- Birmingham C, Su J, Hlynsky J, Goldner EM, Gao M. The mortality rate from anorexia nervosa. International Journal of Eating Disorders. 2005;38:143–146. doi: 10.1002/eat.20164. [DOI] [PubMed] [Google Scholar]
- Bozdogan H. Model selection and Akaike’s information criteria (AIC): The general theory and its analytic extensions. Psychometrika. 1987;52:345–370. [Google Scholar]
- Bulik CM, Berkman ND, Brownley KA, Sedway JA, Lohr KN. Anorexia nervosa treatment: A systematic review of randomized controlled trials. International Journal of Eating Disorders. 2007;40:310–320. doi: 10.1002/eat.20367. [DOI] [PubMed] [Google Scholar]
- Carter JC, Blackmore E, Sutandar-Pinnock K, Woodside DB. Relapse in anorexia nervosa: A survival analysis. Psychological Medicine. 2004;34:671–679. doi: 10.1017/S0033291703001168. [DOI] [PubMed] [Google Scholar]
- Cassin SE, von Ranson KM. Personality and eating disorders: A decade in review. Clinical Psychology Review. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Chen EY, Matthews L, Allen C, Kuo JR, Linehan MM. Dialectical behavior therapy for clients with binge-eating disorder or bulimia nervosa and borderline personality disorder. International Journal of Eating Disorders. 2008;41:505–512. doi: 10.1002/eat.20522. [DOI] [PubMed] [Google Scholar]
- Clark LA, Simms LJ, Wu KD, Casillas A. Manual for the Schedule for Nonadaptive and Adaptive Personality. Minneapolis: University of Minnesota Press; (in press) [Google Scholar]
- Couturier J, Lock J. What is remission in adolescent anorexia nervosa? A review of various conceptualizations and quantitative analysis. International Journal of Eating Disorders. 2006;39:175–183. doi: 10.1002/eat.20224. [DOI] [PubMed] [Google Scholar]
- Crane AM, Roberts ME, Treasure J. Are obsessive-compulsive personality traits associated with a poor outcome in anorexia nervosa? A systematic review of randomized controlled trials and naturalistic outcome studies. International Journal of Eating Disorders. 2007;40:581–588. doi: 10.1002/eat.20419. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, Brown RA. Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. Journal of Abnormal Psychology. 2005;114:729–734. doi: 10.1037/0021-843X.114.4.729. [DOI] [PubMed] [Google Scholar]
- Eating Disorders Work Group. Eating disorders. 2011 May 9; Retrieved from http://www.dsm5.org/proposedrevisions/pages/eatingdisorders.aspx.
- Eddy KT, Keel PK, Dorer DJ, Delinsky SS, Franko DL, Herzog DB. Longitudinal comparison of anorexia nervosa subtypes. International Journal of Eating Disorders. 2002;31:191–201. doi: 10.1002/eat.10016. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York: The Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Cooper Z, O’Connor ME. Eating Disorder Examination. In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. 16.0D. New York: The Guilford Press; 2008. pp. 265–308. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. User’s Guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders - Research Version - (SCID-I for DSM-IV-TR, November 2002 Revision) 2002. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders - Patient Edition (With Psychotic Screen) (SCID-I/P (W/PSYCHOTIC SCREEN) 2007. revision. [Google Scholar]
- Fischer S, Smith GT, Cyders MA. Another look at impulsivity: A meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clinical Psychology Review. 2008;28:1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek H, van Hoeken D. Review of the prevelance and incidence of eating disorders. International Journal of Eating Disorders. 2003;34:383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- Holliday J, Landau S, Collier D, Treasure J. Do illness characteristics and familial risk differ between women with anorexia nervosa grouped on the basis of personality pathology? Psychological Medicine. 2005;36:529–538. doi: 10.1017/S0033291705006641. [DOI] [PubMed] [Google Scholar]
- Keel PK, Dorer DJ, Eddy KT, Delinsky SS, Franko DL, Blais MA, Herzog DB. Predictors of treatment utilization among women with anorexia and bulimia nervosa. American Journal of Psychiatry. 2002;159(1):140–142. doi: 10.1176/appi.ajp.159.1.140. [DOI] [PubMed] [Google Scholar]
- Kröger C, Schweiger U, Sipos V, Kliem S, Arnold R, Schunert T, Reinecker H. Dialectical behaviour therapy and an added cognitive behavioural treatment module for eating disorders in women with anorexia nervosa or bulimia nervosa who failed to respond to previous treatments. An open trial with 15-month follow-up. Journal of Behavior Therapy and Experiental Psychiatry. 2010;41:381–388. doi: 10.1016/j.jbtep.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR. Personality traits and the classification of mental disorders: Towards a more complete integration in DSM-5 and an empirical model of psychopathology. Personality Disorders: Theory, Research, and Treatment. 2010;1:97–118. doi: 10.1037/a0018990. [DOI] [PubMed] [Google Scholar]
- Leoutsakos JM, Zandi PP, Bandeen-Roche K, Lyketsos CG. Searching for valid psychiatric phenotypes: Discrete latent variable models. International Journal of Methods in Psychiatric Research. 2010;19:63–73. doi: 10.1002/mpr.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson J, Vermunt JK. Latent class models for clustering: A comparison with K-means. Canadian Journal of Marketing Research. 2002;20:37–44. [Google Scholar]
- Miller MW, Kaloupek DG, Dillon AL, Keane TM. Externalizing and internalizing subtypes of combat-related PTSD: A replication and extension using the PSY-5 scales. Journal of Abnormal Psychology. 2004;113:636–645. doi: 10.1037/0021-843X.113.4.636. [DOI] [PubMed] [Google Scholar]
- Morgan HG, Russell GF. Value of family background and clinical features as predictors of long-term outcome in anorexia nervosa: Four-year follow-up study of 41 patients. Psychological Medicine. 1975;5:355–371. doi: 10.1017/s0033291700056981. [DOI] [PubMed] [Google Scholar]
- National Institite of Mental Health. National Institute of Mental Health strategic plan. NIH Publication No. 08-6368. 2008 Retrieved from: http://www.nimh.nih.gov/about/strategic-planning-reports/nimh-strategic-plan-2008.pdf.
- O’Brien KM, Vincent NK. Psychiatric comorbidity in anorexia and bulimia nervosa: Nature, prevalence, and causal relationships. Clinical Psychology Review. 2003;23(1):57–74. doi: 10.1016/s0272-7358(02)00201-5. [DOI] [PubMed] [Google Scholar]
- Palmer RL, Birchall H, Damani S, Gatward N, McGrain L, Parker L. A dialectical behavior therapy program for people with an eating disorder and borderline personality disorder: Description and outcome. International Journal of Eating Disorders. 2003;33:281–286. doi: 10.1002/eat.10141. [DOI] [PubMed] [Google Scholar]
- Paul T, Schroeter K, Dahme B, Nutzinger DO. Self-injurious behavior in women with eating disorders. American Journal of Psychiatry. 2002;159(3):408–411. doi: 10.1176/appi.ajp.159.3.408. [DOI] [PubMed] [Google Scholar]
- Peat C, Mitchell JE, Hoek HW, Wonderlich SA. Validity and utility of subtyping anorexia nervosa. International Journal of Eating Disorders. 2009;42:590–594. doi: 10.1002/eat.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Personality and Personality Disorders Work Group. Personality and personality disorders. 2010 December 15; Retrieved from http://www.dsm5.org/PROPOSEDREVISIONS/Pages/PersonalityandPersonalityDisorders.aspx.
- Reich J. The effect of Axis II disorders on the outcome of treatment of anxiety and unipolar depressive disorders: A review. Journal of Personality Disorders. 2003;17(5):387–405. doi: 10.1521/pedi.17.5.387.22972. [DOI] [PubMed] [Google Scholar]
- Root TL, Pisetsky EM, Thornton L, Lichtenstein P, Pedersen NL, Bulik CM. Patterns of co-morbidity of eating disorders and substance use in Swedish females. Psychological Medicine. 2010;40:105–115. doi: 10.1017/S0033291709005662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology. 2006;45:343–366. doi: 10.1348/014466505X53902. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sharp CW, Freeman CP. The medical complications of anorexia nervosa. British Journal of Psychiatry. 1993;162:452–462. doi: 10.1192/bjp.162.4.452. [DOI] [PubMed] [Google Scholar]
- Steiger H, Richardson J, Schmitz N, Israel M, Bruce KR, Gauvin L. Trait-defined eating-disorder subtypes and history of childhood abuse. International Journal of Eating Disorders. 2010;43:428–432. doi: 10.1002/eat.20711. [DOI] [PubMed] [Google Scholar]
- Steinhausen H-C. The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry. 2002;159(8):1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Grigoroiu-Serbanescu M, Boyadjieva S, Neumarker KJ, Winkler Metzke C. Course and predictors of rehospitalization in adolescent anorexia nervosa in a multisite study. International Journal of Eating Disorders. 2008;41:29–36. doi: 10.1002/eat.20414. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA. One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: evidence from a national database of health insurance claims. International Journal of Eating Disorders. 2000;27(4):381–389. doi: 10.1002/(sici)1098-108x(200005)27:4<381::aid-eat2>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Strober M. An empirically derived typology of anorexia nervosa. In: Darby PL, Garfinkel PE, Garner DM, Corscina DV, editors. Anorexia nervosa: Recent developments in research. New York: Alan R. Liss, Inc; 1983. pp. 185–196. [Google Scholar]
- Strober M. Pathologic fear conditioning and anorexia nervosa: On the search for novel paradigms. International Journal of Eating Disorders. 2004;35:504–508. doi: 10.1002/eat.20029. [DOI] [PubMed] [Google Scholar]
- Sullivan PF. Mortality in anorexia nervosa. American Journal of Psychiatry. 1995;152:1073–1074. doi: 10.1176/ajp.152.7.1073. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, Eddy KT, Franko DL, Dorer DJ, Vashchenko M, Kass AE, Herzog DB. A personality classification system for eating disorders: a longitudinal study. Comprehensive Psychiatry. 2008;49:551–560. doi: 10.1016/jcomppsych.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, Westen D. Personality subtypes in eating disorders: validation of a classification in a naturalistic sample. British Journal of Psychiatry. 2005;186(6):516–524. doi: 10.1192/bjp.186.6.516. [DOI] [PubMed] [Google Scholar]
- Treat TA, McCabe EB, Gaskill JA, Marcus MD. Treatment of anorexia nervosa in a specialty care continuum. International Journal of Eating Disorders. 2008;41:564–572. doi: 10.1002/eat.20571. [DOI] [PubMed] [Google Scholar]
- Vermut JK, Magidson J. Latent GOLD 4.0 User’s Guide. Belmont, MA: Statistical Innovations, Inc; 2005. [Google Scholar]
- Vitousek K, Watson S, Wilson GT. Enhancing motivation for change in treatment resistant eating disorders. Clinical Psychology Review. 1998;18(4):391–420. doi: 10.1016/s0272-7358(98)00012-9. [DOI] [PubMed] [Google Scholar]
- Wagner A, Barbarich-Marsteller NC, Frank GK, Bailer UF, Wonderlich SA, Crosby RD, …Kaye WH. Personality traits after recovery from eating disorders: Do subtypes differ? International Journal of Eating Disorders. 2006;39:276–284. doi: 10.1002/eat.20244. [DOI] [PubMed] [Google Scholar]
- Westen D, Harnden-Fischer J. Personality profiles in eating disorders: Rethinking the distinction between Axis I and Axis II. American Journal of Psychiatry. 2001;158(4):547–562. doi: 10.1176/appi.ajp.158.4.547. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Livesley WJ, Clark LA. An integrative dimensional classification of personality disorder. Psychological Assessment. 2009;21:243–255. doi: 10.1037/a0016606. [DOI] [PubMed] [Google Scholar]
- Wiseman CV, Sunday SR, Klapper F, Harris WA, Halmi KA. Changing patterns of hospitalization in eating disorder patients. International Journal of Eating Disorders. 2001;30(1):69–74. doi: 10.1002/eat.1055. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Crosby RD, Joiner T, Peterson CB, Bardone-Cone A, Klein M, …Vrshek S. Personality subtyping and bulimia nervosa: Psychopathological and genetic correlates. Psychological Medicine. 2005;35:649–657. doi: 10.1017/S0033291704004234. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Joiner TE, Jr, Keel PK, Williamson DA, Crosby RD. Eating disorder diagnoses: empirical approaches to classification. American Psychologist. 2007;62:167–180. doi: 10.1037/0003-066X.62.3.167. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Lilenfeld LR, Riso LP, Engel S, Mitchell JE. Personality and anorexia nervosa. International Journal of Eating Disorders. 2005;37:S68–S71. doi: 10.1002/eat.20120. [DOI] [PubMed] [Google Scholar]