Abstract
Objective
To determine the nature of telephone-delivered collaborative care intervention provided patients below and above age 60 experiencing clinically significant depressive symptoms following coronary artery bypass graft (CABG) surgery, and whether patient age is related to response and remission rates and delivery of care at 8-month follow-up.
Design
Exploratory post-hoc analysis of data collected in a randomized controlled trial.
Setting
Seven Pittsburgh-area general hospitals.
Participants
58 depressed post-CABG patients below age 60 and 92 comparable patients age 60 and above randomized to the RCT's intervention arm.
Measurements
Components of collaborative care provided patients over the 8-month study period, and HRS-D scores at 8-month follow-up to determine response and remission status.
Results
There were no differences in the cumulative 8-month rates at which the components of collaborative care were delivered to the two age groups. Similar response and remission rates were also achieved by these groups.
Conclusion
Older and younger patients experiencing clinical depression following CABG surgery can be treated with comparable components of collaborative care and both age groups will achieve clinical outcomes that do not differ significantly from each other.
Keywords: Collaborative care, coronary artery bypass graft surgery, depression
Depressive symptoms are reported by up to one-half of patients following coronary artery bypass graft (CABG) surgery.1 These symptoms are associated with numerous adverse outcomes including poorer health-related quality of life (HRQoL) and worse functional status,2 and higher risk of rehospitalizations.3 Given these adversities, Rollman et al.4, 5 conducted a randomized controlled trial which compared the outcomes of telephone-delivered collaborative care with a physician's usual care in treating depressed post-CABG patients. Patients randomized to the intervention versus usual care reported significantly greater improvements in their HRQoL, physical functioning, and mood symptoms at 8-month follow-up.5
Rollman et al.'s5 findings are consistent with the extensive body of research that has found collaborative care to effectively treat depressive episodes,6, 7 even among the old-old.8 Surprisingly, however, it remains unclear whether collaborative care achieves the same clinical outcomes with depressed mid-life and older patients and, equally critically, whether the two age-groups benefit most from similar or age-specific elements of this multi-component treatment.9 Several cautionary themes related to the interpretation of clinical studies conducted with older persons are emphasized by Scott and Guyatt.10 Of note in this regard is the possibility that depression and medical illness have bidirectional causality with each contributing to the other, a phenomenon possibly more prevalent in older than younger persons.11
The complex interactions between age, depression, and physical illness are of particular concern in treating depressed CABG patients given the “dose-response” relationship between medical comorbidity and treatment outcomes, i.e. more serious physical illnesses are associated with poorer treatment responses for depression.12 Since depressed older patients are more likely to be experiencing such medical disorders as arthritis and circulatory problems which adversely affect the mood disorder's outcome,13 should collaborative care emphasize particular components of customized intensity in relation to the patient's age and medical status? Also pertinent to this concern is the indirect and fluctuating relationship between depressive symptoms and functional impairment.14-17 The latter may be associated with depression but also with other psychiatric and medical illnesses. Indeed, elderly depressed patients who also are medically fragile often suffer functional limitations for reasons substantially unrelated to their depression. One consequence of this indirect relationship is the time lag in response/remission rates for this mood disorder and functional limitations,16 i.e. improved functioning often occurs at a later time point than remission of the core symptoms comprising the depressive episode.
Few studies to date have considered the effectiveness of collaborative care in relation to a patient's age and medical status. Grypma et al.'s18 adaptation of the IMPACT model of collaborative care found this treatment effective for depressed primary care patients both above and below age 60, but the authors provided no information about the severity of medical illnesses experienced by their subjects. This omission limits the generalizability of their findings to depressed post-CABG patients. In a study more directly pertinent to the treatment of depressed CABG patients, Ell et al.19 pooled data from three RCTs that tested collaborative care in oncology clinics, primary care settings, and home health care programs. They found this intervention equally effective for patients older and younger than age 60 in reducing depressive symptoms and improving quality of life. However, their finding requires replication given 6-month retention rates of only 65.5% across the three pooled RCTs.
Given persisting uncertainties about the relationship between a depressed patient's age and the effectiveness of collaborative care's multiple components, Rollman et al.'s5 RCT of depressed CABG patients ranging in age from 35 to 87 provides a unique opportunity for an exploratory post-hoc analysis of this issue even though it was not initially powered for this purpose. The following report, therefore, describes treatments provided patients above and below age 60 (the chronologic dichotomy used by Unutzer et al.20 and Bruce et al.21 in their studies with older depressed primary care patients), age-specific response and remission rates, and functional outcomes at successive points in time for mid-life and older patients.
Methods
The research design for testing the effectiveness of collaborative care interventions for depressive episodes following CABG surgery has been previously detailed.4, 5 The following information, therefore, summarizes the major features of the RCT pertinent to ascertaining whether patient age affects treatment patterns and outcome using a protocol that had been approved by the IRBs of the University of Pittsburgh, each of the participating hospitals, and by the Data Safety Monitoring Board appointed by the NHLBI which funded the study.
Participants
Post-CABG patients were recruited prior to hospital discharge at two university-affiliated and five community-based hospitals in the greater Pittsburgh, PA region between 2004 and 2007. Trained nurse-recruiters were directed to medically-stable post-CABG patients at each study site and obtained their signed informed consent to undergo screening with the two-item version of the Patient Health Questionnaire (PHQ-2).22 An affirmative answer to either the mood or anhedonia question was considered a positive depression screen. Patients were required to score >23 on the Folstein Mini-Mental Status Exam23 as evidence of their mental competence, to not exhibit indicators of severe mental illness or histories thereof, and to be discharged home or to short-term rehabilitation. Patients meeting these and other eligibility criteria4 then signed informed consent statements permitting a research assistant to contact them again following hospital discharge. Since such mood symptoms as fatigue and sleeplessness commonly follow CABG surgery and possibly represent the routine sequellae of this surgery, patients were administered the full PHQ-924 two-weeks following hospital discharge to confirm the earlier positive PHQ-2 depression screen. On this latter occasion, patients remained protocol eligible when scoring ≥ 10 which signifies at least a moderate level of depressive distress.
Assessment and Outcome Measures
The nurse recruiters collected patients' socio-demographic information including their self-reported race, and conducted a detailed chart review of needed medical information. Blinded telephone assessors administered the SF-3625 to determine mental (MCS) and physical (PCS) HRQoL, the 12-item Duke Activity Status Index (DASI)26 to determine disease-specific physical functioning, and the 17-item Hamilton Rating Scale for Depression (HRS-D)27 to track mood symptoms at 2, 4, and 8 months. At baseline, the Perceived Social Support Scale (PSSS)28 was administered to assess social support, and the Life Orientation Test (LOT-R)29 was administered to assess generalized levels of optimism. Patients were mailed a $20 check as reimbursement for time spent in the research protocol following each of the four contacts for a total of $80.
Randomization Procedure
Following completion of the two-week post-discharge assessment and confirmation of protocol-eligibility, 150 patients were randomized to the collaborative care intervention and 152 to the usual care arm of the RCT in a 1:1 ratio in blocks of four at each site, with no stratification by age. Given our interest in whether age affects the delivery and effectiveness of collaborative care, this paper focuses solely on the 150 of 302 protocol-eligible patients randomized to the intervention arm.
Interventions
Initial Telephone Contact
A nurse care manager telephoned patients to review their psychiatric history, provide psychoeducation about depression and its impact on cardiac disease, and to describe treatment options. As was more fully described elsewhere,4 the treatment options included: (1) a workbook to enhance the patient's ability to self-care for depression; (2) antidepressant pharmacotherapy prescribed by the primary care physician; (3) “watchful waiting” for mildly elevated mood symptoms; and (4) referral to a local mental health specialist.
Case Review
Nurse care managers presented clinical information regarding the patient to the Clinical Team consisting of study psychiatrist (CFR), internist (BLR), and psychologist (BHB). This included an overview of the patient's course of illness, medication usage, workbook chapters covered, and additional details to inform clinical decision making. On this basis, the Clinical Team formulated treatment recommendations consistent with the patient's needs, current preferences, and insurance coverage. The care manager then conveyed the Clinical Team's recommendations to the patient and his/her physician.
Antidepressant Pharmacotherapy
Selective serotonin reuptake inhibitors (SSRIs) can be safely prescribed cardiac patients30, 31 and none has superior efficacy in treatment-naïve patients.32, 33 The clinical team, therefore, typically recommended that the primary care physician prescribe citalopram for the patient since it is available in generic form, has limited drug-drug interactions, and requires few dosage adjustments. PCPs had to approve and prescribe all adjustments to their patients' pharmacotherapy.
Mental Health Referral
Referral to a mental health specialist was advised for patients displaying a poor treatment response, severe psychopathology, complex psychosocial problems, and for those expressing this treatment preference. When indicated, the care manager helped facilitate the specialist referral and followed up to confirm that an appointment had been made and kept.
Follow-Up
Care manager telephone contacts of 15-45 minutes were conducted every other week during the acute phase of treatment to: assess treatment response by administering the PHQ-9, review lesson plans, monitor pharmacotherapy where indicated, and discuss new treatment recommendations generated by the weekly case reviews. The acute phase typically lasted two to four months and as the patient improved, telephone contacts with him/her diminished to a less frequent schedule until the 8-month intervention was completed.
Blinded Assessments
Telephone assessors, blinded to the patient's status as an intervention or usual care patient, periodically contacted study subjects to administer the previously described instruments assessing clinical and functional status, and explicitly cautioned patients at the start of each call not to divulge their treatment assignment. Given the nature of collaborative care for depression, neither patients randomized to this intervention nor their physicians were blinded to this treatment assignment.
Statistical Analyses
Baseline comparisons of the two age-groups were performed with parametric t-tests for continuous variables and chi-square tests for categorical ones. Eight-month response and remission outcomes (50% or greater improvement of HRS-D scores and HRS-D scores ≤ 7, respectively) were compared with chi-square test, and Cohen-h effect sizes were computed. Multiple imputation techniques were used to calculate the missing 8-month HRS-D scores that were used to determine remission outcome. Continuous outcome measures were compared across time with repeated measures mixed effects models with time as a categorical variable. Time to first rehospitalization was determined with Kaplan-Meier survival analytic methods and the results were tested for significance of differences with a log-rank chi-square statistic.
Results
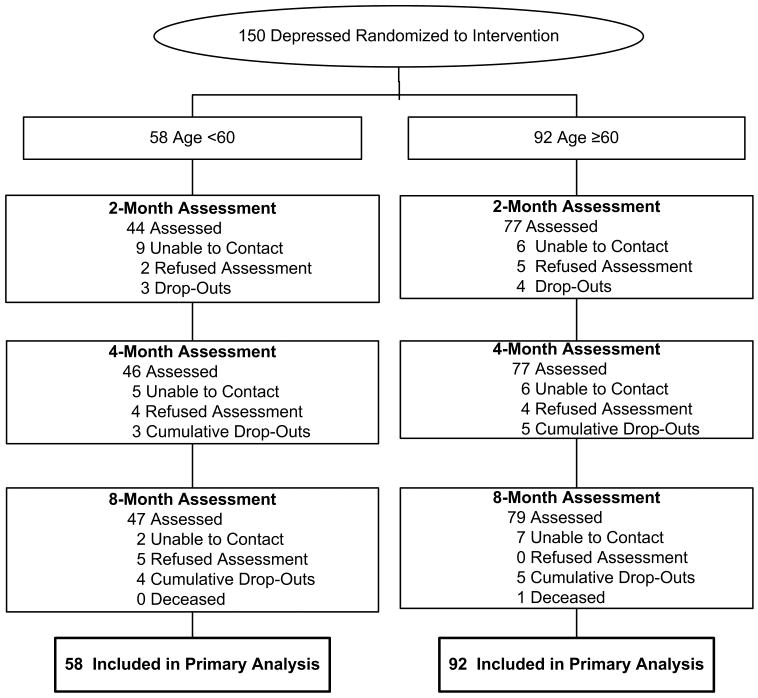
A depiction of the screening and assessment procedures through which patients were recruited for both the RCT's intervention and usual care arms is provided by Rollman et al.5 With regard to the subcohort of protocol-eligible patients subsequently randomized to collaborative care, Figure 1 traces the longitudinal course of the 58 such patients <60 years of age and the 92 such patients who were 60 years and older at baseline. Retention in the follow-up assessments was high for both age groups; 76%, 79%, and 81% of the younger patients participated in the 2, 4, and 8-month follow-ups, respectively. Similarly, 84%, 84%, and 86% of the older patients participated in the 2, 4, and 8-month follow-ups, respectively.
Figure 1.
Age-related randomization and follow-up patterns for intervention patients.
Sample Characteristics
The younger and older patients randomized to collaborative care differed, as would be expected, on the demographic characteristics of age and work status (Table 1). Furthermore, significantly fewer younger than older patients were Caucasian and fewer members of the latter group reported an education beyond high school. With regard to the 30 measures of psychosocial, psychiatric, and medical status assessed at baseline, the two age groups differed on only four of them. Compared to younger patients, older ones had significantly higher SF-36 Mental Component Scores (44.7 vs. 40.9, t-test=-2.00, d.f.=1, p=0.05) and SF-Bodily Pain scores (41.0 vs. 37.2, t-test=-2.40, d.f.=1, p=0.02) Contrary to the concern that older patients experience more medical illnesses that could impede recovery from depressive episodes, this group experienced significantly more such morbidity only with regard to chronic obstructive pulmonary disease (28.3% vs. 10.3%; χ2=6.29, d.f.=1, p=0.01), and congestive heart failure (26.1% vs. 12.1%; χ2=4.08, d.f.=1, p=0.04).
Table 1.
Baseline sociodemographic characteristics by age group
| Demographic | Intervention Age < 60 (N=58) |
Intervention Age ≥ 60 (N=92) |
t-test or χ2 | df | P |
|---|---|---|---|---|---|
| Age, mean (SD) | 52.5 (6.2) | 70.3 (6.6) | 16.54 | 148 | < 0.0001 |
| Male, % (N) | 51.7 (30) | 55.4 (51) | 0.20 | 1 | 0.66 |
| Caucasian, % (N) | 81.0 (47) | 92.4 (85) | 4.34 | 1 | 0.04 |
| >High School education, % (N) | 70.7 (41) | 48.9 (45) | 6.90 | 1 | 0.01 |
| Married, % (N) | 65.5 (38) | 67.4 (62) | 0.06 | 1 | 0.81 |
| Working, part- or full-time, % (N) | 77.6 (45) | 18.5 (17) | 51.25 | 1 | <0.0001 |
Processes of Care
Collaborative care of depression is a multi-component intervention9 and we compared the frequency with which ten of its elements were delivered to younger and older patients. Table 2 indicates that there were no differences between the two age-groups in their cumulative 8-month rates for using nine of the ten elements of collaborative care (all p>0.05). They differed significantly only with regard to their use of the muscle relaxation compact disc offered by the care manager. Almost 1/3 of the younger patients employed this material over the study's time period but only 16% of the older patients did so (χ2=4.50, d.f.=1, p=0.03), reflecting perhaps the former group's greater comfort with this technology.
Table 2.
Process measures of collaborative care: cumulative rates as of 8-month
| All (N=150) |
Age < 60 (N=58) |
Age ≥ 60 (N=92) |
χ2 (df=1) |
P | |
|---|---|---|---|---|---|
| Care manager contacts, median (range) | 10 (0-28) | 9 (0-28) | 10 (0-23) | 1.85 | 0.17 |
| ≥ 3 Calls %, (N) | 87% (130) | 86% (50) | 87% (80) | 0.02 | 0.90 |
| ≥ 3 Mentions of workbook use by care manager, % (N) | 85% (128) | 84% (49) | 86% (79) | 0.0 | 0.82 |
| Workbook Completed, % (N) | 45% (68) | 43% (25) | 47% (43) | 0.19 | 0.66 |
| Use of muscle-relaxation compact disc % (N) | 22% (33) | 31% (18) | 16% (15) | 4.50 | 0.03 |
| Instructed about sleep hygiene, % (N) | 73% (108) | 68% (39) | 77% (69) | 1.06 | 0.27 |
| Mental health specialist recommended by care manager | 17% (26) | 19% (11) | 16% (15) | 0.18 | 0.68 |
| Antidepressant medications, % (N)† | 51% (76) | 59% (34) | 46% (42) | 2.39 | 0.12 |
| Antidepressant medication change, % (N)† | 9% (14) | 12% (4) | 24% (10) | 1.18 | 0.18 |
| Perceived treatment barriers, % (N) | 65% (97) | 75% (43) | 60% (54) | 3.71 | 0.06 |
Antidepressant pharmacotherapy includes selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), bupropion, and mirtazapine.
Outcomes
The 8-month outcomes resulting from collaborative care of post-CABG depression in relation to age were assessed on the psychiatric indices of response and remission14 as well as related clinical and functional measures. With regard to the index of response, no significant difference was found between the two age-groups (Table 3). After eight months of collaborative care, a 50% or greater improvement of their mood symptoms was achieved by 56.5% and 43.1% of the older and younger age-groups, respectively (χ2=2.56, d.f.=1, p=0.11). Remission rate was also similar for the two age groups; 53.3% and 41.4% of the older and younger patients, respectively, scored ≤ 7 on the HRS-D at the 8-month follow-up assessment (χ2=2.01, d.f.=1, p=0.16). Cohen-h effect sizes of 0.27 for response rate and 0.24 for remission were obtained for the two age groups (Table 3). The number needed to treat (NNT) with collaborative care in contrast to usual care to achieve one additional response at 8-months was 4.3 (95% CI 2.5-14.6) for patients below age 60 and 4.6 (95% CI 2.8-13.0) for those age 60 and above.
Table 3.
8-month response and remission outcomes
| Age <60 (N=58) |
Age ≥ 60 (N=92) |
Cohen h Effect Size (95% CI) |
χ2 (df=1) |
P | |
|---|---|---|---|---|---|
| ≥ 50% decline from baseline HRS-D score | 43.1% (25/58) | 56.5% (52/92) | 0.27 (-006-0.60) | 2.56 | 0.11 |
| HRS-D score ≤ 7 at 8-month | 41.4% (24/58) | 53.3% (49/92) | 0.24 (-0.09-0.57) | 2.01 | 0.16 |
Abbreviation:
HRS-D: Hamilton Rating Scale for Depression
Since factors associated with recovery at 8-months could differ among the study's younger and older patients, we analyzed the 14 baseline age-specific socio-demographic, psychosocial, and psychiatric variables for each age group that could possibly distinguish those who did/did not score ≤ 7 on the HRS-D at the 8-month follow-up assessment (Table 4). Among the younger patients, those who recovered and those who did not differed only on the SF-36 PCS, with the latter group scoring significantly lower. On the other hand, older non-remitters differed significantly from older remitters in not being married, scoring lower on the SF-36 MCS, scoring lower on the LOT-R measure of optimism, and experiencing more depressive symptoms as assessed on the HRS-D.
Table 4.
Baseline sociodemographic and clinical characteristics and 8-month recovery status.
| Age <60 | Age ≥ 60 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable, mean (SD) | Recovered (n=24) |
Non-Recovered (n=34) |
t-test or χ2 | df | P | Recovered (n=49) |
Non-Recovered (n=43) |
t-test or χ2 | df | P |
| Age, years | 53.5 (4.5) | 51.9 (7.1) | 1.06 | 55.4 | 0.29 | 71.0 (6.5) | 69.6 (6.7) | 1.07 | 90 | 0.29 |
| Male, % | 58 | 47 | 0.71 | 1 | 0.40 | 63 | 47 | 2.60 | 1 | 0.11 |
| Caucasian, % | 83 | 79 | 0.14 | 1 | 0.71 | 92 | 93 | 0.05 | 1 | .083 |
| >High School education, % | 67 | 74 | 0.32 | 1 | 0.57 | 47 | 51 | 0.16 | 1 | 0.69 |
| Married, % | 75 | 59 | 1.63 | 1 | 0.20 | 78 | 56 | 4.92 | 1 | 0.03 |
| Working, part- or full-time, % | 83 | 74 | 0.78 | 1 | 0.38 | 18 | 19 | 0.001 | 1 | 0.98 |
| SF-36 MCS‡ | 42.1 (9.3) | 40.1 (12.7) | 0.66 | 56 | 0.51 | 47.1 (11.1) | 41.9 (10.2) | 2.31 | 90 | 0.02 |
| SF-36 PCS‡ | 33.5 (5.0) | 30.4 (6.1) | 2.05 | 56 | 0.04 | 32.3 (7.7) | 29.4 (7.5) | 1.83 | 90 | 0.07 |
| DASI | 8.8 (6.6) | 7.3 (6.2) | 0.87 | 56 | 0.39 | 7.6 (5.2) | 5.5 (5.3) | 1.90 | 90 | 0.06 |
| PSSS | 69.2 (8.2) | 69.0 (12.9) | 0.05 | 55.5 | 0.96 | 74.0 (6.8) | 66.6 (12.1) | 3.56 | 64 | 0.001 |
| LOT-R | 15.0 (4.2) | 13.1 (4.8) | 1.51 | 51 | 0.14 | 16.0 (3.8) | 14.0 (5.1) | 2.06 | 83 | 0.04 |
| SF-36 Bodily Pain | 37.1 (8.2) | 37.2 (9.7) | 0.08 | 56 | 0.94 | 42.7 (9.0) | 39.2 (10.9) | 1.67 | 90 | 0.10 |
| PHQ-9§ | 13.4 (3.0) | 13.9 (3.8) | 0.56 | 56 | 0.58 | 12.9 (2.4) | 13.9 (3.4) | 1.58 | 75.4 | 0.11 |
| HRS-D§ | 17.8 (6.8) | 17.7 (6.8) | 0.05 | 56 | 0.96 | 13.7 (6.5) | 18.2 (7.5) | 3.07 | 90 | 0.003 |
Abbreviations:
SF-36 MCS: Medical Outcomes Study Short Form Health Survey Mental Component Scale
SF-36 PCS: Medical Outcomes Study Short Form Health Survey Physical Component Scale
DASI: Duke Activity Status Index
PSSS: Perceived Social Support Scale
LOT-R: Life Orientation Test Revised Optimism Score
HRS-D: Hamilton Rating Scale for Depression
Higher scores indicate better health-related quality of life
Higher scores indicate more severe symptoms
We additionally examined age-related outcome measures over time using repeated measures mixed effect models on each of four measures assessing domains of functioning (Table 5). As expected, an improvement in patient status is noted for all of these measures with a significant time effect. A significant age-group effect is also noted for the variables assessed by the HRS-D, SF-36 MCS, and DASI. Older subjects reported lower depressive distress on the HRS-D, better mental functioning on the SF-36 MCS, and better disease-specific physical functioning on the DASI throughout the 8-month assessment period. However, a significant age-group by time interaction was found only on the DASI. Scores rose from 7.9 to 29.9 during the 8-month follow-up period for younger patients but only from 6.6 to 23.1 (increments of 22.0 vs. 16.5 points; F=3.03, d.f.=3,379, p=0.03) among older patients on this measure of disease-specific physical functioning.
Table 5.
Mixed-effect results on intervention group.
| Age Group effect | Time effect | Age Group × Time Interaction | |
|---|---|---|---|
| HRS-D | F=13.33 df=1,142 <0.001 |
F=57.29 df=3.371 <0.001 |
F=1.48 df=3,371 0.21 |
| SF-36 MCS | F=13.21 df=1,143 <0.001 |
F=19.52 df=3,371 <0.001 |
F=1.98 df=3,371 0.13 |
| SF-36 PCS | F=0.83 df=1,151 0.37 |
F=125.89 df=3,377 <0.001 |
F=0.24 df=3,377 0.87 |
| DASI | F=11.14 df=1,149 0.001 |
F=125.89 df=3,377 <0.001 |
F=3.03 df=3,379 0.03 |
Abbreviations:
HRS-D: Hamilton Rating Scale for Depression
SF-36 MCS: Medical Outcomes Study Short Form Health Survey Mental Component Scale
SF-36 PCS: Medical Outcomes Study Short Form Health Survey Physical Component Scale
DASI: Duke Activity Status Index
Finally, with regard to the critical outcome measure of time to initial rehospitalization for cardiac reasons, the Kaplan-Meier survival curves revealed no significant differences between the younger and older patients (LR chi-square = 0.01, d.f.=1, p=0.99). The cumulative rehospitalization rate over eight months was virtually identical for patients younger and older than 60 years of age, 14.5% and 14.8%, respectively.
Discussion
Collaborative care's effectiveness in managing depressive disorders is now well established.6, 7 Investigators and clinicians, therefore, are now considering whether and how this intervention can be delivered to patients of differing socio-demographic and clinical characteristics. The variables of patient age and health status are particularly significant in this regard since they profoundly influence the setting and manner in which depressed patients are treated. This paper, then, is the first to our knowledge to find no significant age-related difference in the manner in which collaborative care is delivered and the outcomes which it attains for patients who are clinically depressed following CABG surgery. Thus, despite growing attention to the manner in which age distinctively affects the diagnosis of depression and should be considered in revisions of DSM-V,34 developmental factors may not necessarily affect treatment processes and clinical outcomes across the age spectrum.
The generalizability of our study findings is limited given their derivation from a post hoc exploratory analysis of data produced by a randomized controlled trial.5 Furthermore, the RCT's initial statistical power was reduced in this post hoc analysis which focused solely on patients randomized to the larger study's intervention arm. Our findings regarding the lack of differences in the collaborative care provided and the clinical outcomes achieved by the two age groups, thus, potentially are of the false negative type. Nevertheless, pending future evidence to the contrary, the present study is consistent with earlier findings that older depressed patients can be treated with interventions comparable to those provided depressed younger adults and that both age groups will achieve clinical outcomes that do not significantly differ from each other.
Our finding complements the recent report by Ell et al.19 that collaborative care is effective across the full age range in depressed patients experiencing non-cardiac medical illnesses. Additionally, despite earlier findings that CABG survival rates are poorer for older than younger patients,35 collaborative care of depression produces benefits across the full age spectrum as is evidenced by our findings about response/remission rates (Table 3) and risk of rehospitalization for cardiac reasons.
Thus, while the OPTIMIZE-HF36 registry and performance-improvement program found persons 75+ experiencing heart failure to receive poorer quality of care than younger peers, age per se should not determine whether collaborative care is provided persons experiencing post-CABG depression. Coryell et al.37 emphasize that depressive morbidity levels are influenced by age of onset rather than current age or the ageing process itself. We would also note that even when the patient's mood disorder results from vascular disease, collaborative care remains appropriate since this disease is strongly correlated with level of disability rather than a specific depressive symptom pattern.38
This study's finding that older depressed post-CABG patients achieve outcomes that do not significantly differ from those achieved by younger such patients (Table 3) extends earlier reports by Alexopoulos et al.,39 and Reynolds et al.40 which challenged the view that geriatric depression has a poor outcome. Indeed, the older post-CABG patients treated in Rollman et al.'s5 RCT achieved even better remission rates than the less medically ill depressed primary care patients provided collaborative care in the IMPACT20 and PROSPECT21 clinical trials. Depressed post-CABG patients 60 years and older in the present study had 8-month remission rates of 53.3% (Table 3) compared to the 6-month remission rate of 30.1% in the IMPACT trial and the 8-month remission rate of 36.8% in the PROSPECT trial.
These salutary outcomes surely are commendable. We also acknowledge, however, that despite collaborative care's multi-pronged approach to treating the depressive episode, approximately half of patients so treated in Rollman et al.'s5 trial failed to remit when assessed at the 8-month follow-up and so remained at high risk for relapse and recurrence.14 Carney and Freedland41 emphasize that treatment-resistant depression may also be associated with a high risk of mortality or cardiac morbidity and that better pharmacologic and psychotherapeutic interventions are needed to treat more severe manifestations of the mood disorder. A complementary approach for minimizing poor outcomes is to identify patients at high risk for post-CABG depression and to initiate preventive strategies with them even before the surgery is performed. We identified five risk factors associated with non-recovery among patients 60 years and older but, strikingly, only one such factor for patients younger than 60 (Table 4).
The search for risk-factors for incident depression, such as those identified by Lyness et al,42 opens the controversial question of whether routinely to screen all CABG candidates for this mood disorder. The American Heart Association's science advisory43 recommends that patients with coronary heart disease be screened for depression so as not to miss the opportunity to administer effective treatments. The U.S. Preventive Services Task Force, however, recently reiterated its recommendation that such screening occur only when staff-assisted depression care supports are available.44 An even more restrictive approach is proposed by Thombs et al.45 who note that we still lack adequate evidence that routine screening plus collaborative care improves cardiovascular outcomes. Whether and how often to screen patients with vascular disease for depression, thus, remains an open question requiring further evidence beyond that generated by Rollman et al.'s5 RCT.
Since the present study found patient age not significantly related to 8-month response/remission rates, cardiac-related rehospitalization rates, and NNT, did collaborative care achieve these outcomes by expending similar or differing levels of effort in treating younger and older patients? Table 2 indicates that the median number of depression care manager contacts and the other components of collaborative care provided patients were virtually the same across the age spectrum over the study's 8-month duration.
Given this pattern, it is of interest that Grypma et al.18 found younger patients more likely than older ones to terminate collaborative care before attaining their protocol's 10-week minimum. The younger patients' outcomes nevertheless resembled those of older patients participating in the study's more extended follow-ups. The authors speculated that younger patients respond more quickly to collaborative care and, thus, required fewer care manager contacts. It remains to be determined, however, whether caregiving patterns pertinent to depressed primary care patients are equally applicable to more medically-ill patients experiencing post-CABG depression.
While this study found younger and older depressed patients to receive similar elements of collaborative care, the present data set does not permit us to replicate Oxman et al.'s46 finding that the intensity of collaborative care is positively related to clinical outcome. However, Butler et al.'s7 meta-analysis of earlier collaborative care research found no correlation between the number of caregiving components provided patients and various clinical outcomes. They, therefore, caution against “premature orthodoxy” in designating particular collaborative care programs as the gold standard for resolving depressive episodes.
Acknowledgments
This work was supported by NIH Grant P30 MH085943, G. Alexopoulos, PI (Schulberg); NIH Grant R01 HL70000 (Rollman); NIH Grant P30 MH71944 (Reynolds); and by the UPMC Endowed Chair in Geriatric Psychiatry (Reynolds).
References
- 1.Pignay-Demaria V, Lesperance F, Demaria R, Frasure-Smith N, Perrault L. Depression and anxiety and outcomes of coronary artery bypass surgery. Ann Thorac Surg. 2003;75:314–321. doi: 10.1016/s0003-4975(02)04391-6. [DOI] [PubMed] [Google Scholar]
- 2.Goyal T, Idler E, Krause T, Contrada R. Quality of life following cardiac surgery: impact of the severity and course of depressive symptoms. Psychosom Med. 2005;67:759–765. doi: 10.1097/01.psy.0000174046.40566.80. [DOI] [PubMed] [Google Scholar]
- 3.Oxlad M, Stubberfield J, Stuklis R, Edwards J, Wade T. Psychological risk factors for cardiac-related hospital readmission within 6 months of coronary artery bypass graft surgery. J Psychosom Res. 2006;61:775–781. doi: 10.1016/j.jpsychores.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 4.Rollman B, Herbeck Belnap B, LeMenager M, et al. The Bypassing the Blues treatment protocol: Stepped collaborative care for treating post-CABG depression. Psychosom Med. 2009;71:217–230. doi: 10.1097/PSY.0b013e3181970c1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rollman B, Herbeck Belnap B, LeMenager M, et al. Telephone-delivered collaborative care for treating post-CABG depression: A randomized controlled trial. JAMA. 2009;302:2095–2103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilbody S, Bower P, Fletcher J, Richards D, Sutton A. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 7.Butler M, Kane R, McAlpine D, et al. Integration of Mental Health/Substance Abuse and Primary Care. AHRQ Publication No. 09-E003. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 8.Williams E, Unutzer J, Lee S, Noel P. Collaborative depression care for the old-old: Findings from the IMPACT trial. Am J Geriatr Psychiatry. 2009;17:1040–1049. doi: 10.1097/JGP.0b013e3181b4bf08. [DOI] [PubMed] [Google Scholar]
- 9.Herbeck Belnap B, Kuebler J, Upshur C, et al. Challenges of implementing depression care management in the primary care setting. Adm Policy Ment Health. 2006;33:71–81. doi: 10.1007/s10488-005-4237-z. [DOI] [PubMed] [Google Scholar]
- 10.Scott I, Guyatt G. Cautioanry tales in the interpretation of clinical studies involving older persons. Arch Int Med. 2010;170:587–595. doi: 10.1001/archinternmed.2010.18. [DOI] [PubMed] [Google Scholar]
- 11.Lu B, Ahmed I. The mind-body conundrum: The somatopsychic perspective in geriatric depression. Am J Geriatr Psychiatry. 2010;18:378–381. doi: 10.1097/jgp.0b013e3181d749c2. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell A, Subramaniam H. Prognosis of depression in old age compared to middle age: a systematic review of comparative studies. Am J Psychiatry. 2005;162:1588–1601. doi: 10.1176/appi.ajp.162.9.1588. [DOI] [PubMed] [Google Scholar]
- 13.Oslin D, Datto C, Kallan M, Katz I, et al. Association between medical comorbidity and treatment outcomes in late-life depression. JAGS. 2002;50:823–828. doi: 10.1046/j.1532-5415.2002.50206.x. [DOI] [PubMed] [Google Scholar]
- 14.Rush A, Kraemer H, Sackeim H, et al. Report by the ACNP Task Force on response and remission in major depressive disorder. Neuropsychopharm. 2006;31:1841–1853. doi: 10.1038/sj.npp.1301131. [DOI] [PubMed] [Google Scholar]
- 15.Papakostas G. Major depressive disorder: psychosocial impairment and key considerations in functional improvement. Amer J Managed Care. 2009;15:S316–S321. [PubMed] [Google Scholar]
- 16.Mintz J, Mintz L, Arruda M, Hwang S. Treatments of depression and the functional capacity to work. Arch Gen Psychiatry. 1992;49:761–768. doi: 10.1001/archpsyc.1992.01820100005001. [DOI] [PubMed] [Google Scholar]
- 17.Weinberger M, Raue P, Meyers B, Bruce M. Predictors of new onset depression in medically ill, disabled older adults at 1 year follow-up. Am J Geriatr Psychiatry. 2009;17:802–809. doi: 10.1097/JGP.0b013e3181b0481a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grypma L, Haverkamp R, Little S, et al. Taking an evidence-based model of depression care from research to practice: Making lemonade out of depression. Gen Hosp Psychiatry. 2006;28:101–107. doi: 10.1016/j.genhosppsych.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Ell K, Aranda M, Xie B, et al. Collaborative depression treatment in older and younger adults with physical illness: Pooled comparative analysis of three randomized clinical trials. Am J Geriat Psychiatry. 2010;18:520–530. doi: 10.1097/JGP.0b013e3181cc0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unutzer J, Katon W, Callahan C, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 21.Bruce M, Ten Have T, Reynolds CR, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer R, Williams J. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 23.Folstein M, Folstein S, McHugh P. “Mini mental state.” A preactical method for grading the cognitive state of patients for the clinican. J Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer R, Williams J. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware J, Kosinski M, Keller S. SF-36 physical and mental health summary scales: A user's manual. 2'nd. Boston: New England Medical Center; 1994. [Google Scholar]
- 26.Hlatky M, Boineau R, Higginbotham M, et al. A brief self-administered questionnaire to determine functional capacity (The Duke Activity Status Index) Am J Cardiology. 1989;64:651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 27.Freedland K, Skala J, Carney R, et al. The Depression Interview and Structured Hamilton (DISH): Rationale, Development, Characteristics, and Clinical Validity. Psychosom Med. 2002;64:897–905. doi: 10.1097/01.psy.0000028826.64279.29. [DOI] [PubMed] [Google Scholar]
- 28.Blumenthal JA, Burg MM, Barefoot J, et al. Social support, type A behavior, and coronary artery disease. Psychosom Med. 1987;49:331–340. doi: 10.1097/00006842-198707000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Scheier M, Matthews K, Owens J, et al. Optimism and rehospitalization after coronary artery bypass graft surgery. Arch Intern Med. 1999;159:829–835. doi: 10.1001/archinte.159.8.829. [DOI] [PubMed] [Google Scholar]
- 30.Glassman A, O'Connor C, Califf R, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 31.Mulsant B, Alexopoulos G, Reynolds CR, et al. Pharmacological treatment of depression in older primary care patients: The PROSPECT algorithm. Int'l J Geriatric Psychiatry. 2001;16:585–592. doi: 10.1002/gps.465. [DOI] [PubMed] [Google Scholar]
- 32.Whooley M, Simon G. Managing depression in medical outpatients. N Engl J Med. 2000;343:1942–1950. doi: 10.1056/NEJM200012283432607. [DOI] [PubMed] [Google Scholar]
- 33.Hansen R, Gartlehner G, Lohr K, et al. Efficacy and safety of second-generation antidepressants in the treatment of major depressive disorder. Ann Intern Med. 2005;143:415–426. doi: 10.7326/0003-4819-143-6-200509200-00006. [DOI] [PubMed] [Google Scholar]
- 34.Kupfer D, Kuhl E, Regier D. Research for improving diagnostic systems: consideration of factors related to later life development. Am J Geriatr Psychiatry. 2009;17:355–358. doi: 10.1097/JGP.0b013e31819e2c40. [DOI] [PubMed] [Google Scholar]
- 35.Alexander K, Peterson E. Coronary artery bypass grafting in the elderly. Am Heart J. 1997;134:856–864. doi: 10.1016/s0002-8703(97)80008-7. [DOI] [PubMed] [Google Scholar]
- 36.Fonarow G, Abraham W, Albert N, et al. Age- and gender-related differences in quality of care and outcomes of patients hospitalized with heart failure (from OPTIMIZE-HF) Am J Cardiol. 2009;104:107–115. doi: 10.1016/j.amjcard.2009.02.057. [DOI] [PubMed] [Google Scholar]
- 37.Coryell W, Solomon D, Leon A, et al. Does major depressive disorder change with age? Psychol Med. 2009;39:1689–1695. doi: 10.1017/S0033291709005364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Licht-Strunk E, Bremmer M, van Marwijk H, et al. Depression in older persons with versus without vascular disease in the open population: similar depressive symptom patterns, more disability. J Affect Disord. 2004;83:155–160. doi: 10.1016/j.jad.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 39.Alexopoulos GS, Vrontou C, Kakuma T, et al. Disability in geriatric depression. American Journal of Psychiatry. 1996;153:877–885. doi: 10.1176/ajp.153.7.877. [DOI] [PubMed] [Google Scholar]
- 40.Reynolds CR, Frank E, Perel J, et al. Nortriptylene and interpersonal psychotherapy as maintenance therapies for recurrent major depression: A randomized controlled trial in patients older than 59 years. JAMA. 1999;281:39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- 41.Carney R, Freedland K. Treatment-resistant depression and mortality after acute coronary syndrome. Am J Psychiatry. 2009;166:410–417. doi: 10.1176/appi.ajp.2008.08081239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lyness J, Yu Q, Tang W, et al. Risks for depression onset in primary care elderly patients: potential targets for preventive interventions. Am J Psychiatry. 2009;166(12):1375–1383. doi: 10.1176/appi.ajp.2009.08101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lichtman J, Bigger JJ, Blumenthal J, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: A science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118:1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 44.U.S. Preventive Services Task Force Screening for depression in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:784–792. doi: 10.7326/0003-4819-151-11-200912010-00006. [DOI] [PubMed] [Google Scholar]
- 45.Thombs B, de Jonge P, Coyne J, et al. Depression screening and patient outcomes in cardiovascular care: A systematic review. JAMA. 2008;300:2161–2171. doi: 10.1001/jama.2008.667. [DOI] [PubMed] [Google Scholar]
- 46.Oxman T, Schulberg H, Greenberg R, et al. A fidelity measure for integrated management of depression in primary care. Med Care. 2006;44:1030–1037. doi: 10.1097/01.mlr.0000233683.82254.63. [DOI] [PubMed] [Google Scholar]