Abstract
Background:
Pituitary metastasis as a presenting manifestation of silent systemic malignancy is rare. We describe four such cases.
Materials and Methods:
Four patients (0.7%) of malignancy with pituitary metastasis out of 540 patients of sellar mass within a period of 10 years were analyzed for clinical, hormonal and radiological findings.
Result:
The age range of these patients was 39-60 years with lag time ranging from 2to 5 months. Pituitary pathology was presenting manifestation in all 4 patients including diabetes insipidus, ophthalmoplegia and variable anterior pituitary hormone deficiency. 2 patients had bronchogenic carcinoma and one each had squamous cell and adenocarcinoma with unknown primary. Diagnosis of pituitary metastasis was confirmed in three on pituitary mass histopathology and in one it was based on rapidly appearing mass in a short time.
Conclusion:
Rapidly appearing mass in the sellar region, short lag time,sudden onset of ophthalmoplegia, -symptoms and signs disproportionate to the size of mass, presence of diabetes insipidus and destroyed but normal sized sella should invoke the suspicion of pituitary metastasis.
Keywords: Non-functioning pituitary adenoma, pituitary metastasis, radiological features
INTRODUCTION
Pituitary adenomas are a major cause of sellar mass and constitute up to 15% of all intracranial lesions.[1,2] Therefore, in patients with known systemic malignancy, pituitary adenoma may be found, more often, simultaneously than pituitary mass as a result of metastasis. Pituitary metastasis is rarely encountered in clinical practice. It is usually found at the terminal stage of malignancy, with frequency ranging form 1 to 25% at autopsy.[3] The most common primary malignancies with metastasis to the pituitary are breast and lung carcinoma. Rarely, malignancies arising from gastrointestinal tract, uterus, prostate, urinary bladder and pancreas may metastasize to pituitary.[4] A surgical series of 780 post-transsphenoidal surgery cases revealed only 6 cases with metastatic disease (0.8%).[5] Pituitary metastasis may be mistaken for pituitary adenoma since both have many similar radiological findings.
Here, we describe the clinical and radiological features of four patients with pituitary metastasis who presented with sellar mass mimicking pituitary adenoma and were later on found to have pituitary metastasis.
MATERIALS AND METHODS
We analyzed 10 years of hospital records of mass involving sellar and suprasellar region, between the years 2001 and 2010, of Neuroendocrine Center at Postgraduate Institute of Medical Education and Research, Chandigarh, India. Cases with pituitary metastasis were recorded and analyzed separately. All the cases were confirmed to have pituitary metastasis on histopathological examination, except onewho was having rapidly increasing sellar mass and metastatic adenocarcinoma from unknown primary site. We could retrieve X-ray of sella, computed tomography (CT) with coronal cuts, and 1.5 T magnetic resonance (MR) imaging with 3-mm thick T1- and T2-weighted images before and after gadolinium contrast of all the cases. We analyzed imaging characteristics of these four patients to obtain findings which can help to differentiate pituitary metastasis from pituitary adenoma. We hereby describe the clinical presentation, imaging findings and hormonal profiles of these patients.
RESULTS
Between the years 2001 and 2010, 540 cases of space-occupying lesions in the sellar and suprasellar region were registered at our center. Out of 540 cases, 4 (0.7%) were due to pituitary metastasis.
Pituitary pathology was the presenting manifestation in all four patients and they were diagnosed as having pituitary metastasis retrospectively based on histopathology report in 3 patients and one with circumstantial evidence of rapidly growing sellar mass (case-1). The site and histology of primary malignancy in these patients were: bronchogenic carcinoma in two patients, squamous cell carcinoma with occult primary and adenocarcinoma with multifocal metastasis but unknown primary in one each [Table 1].
Table 1.
Clinico-radiological features and hormonal profiles of four cases with pituitary metastases
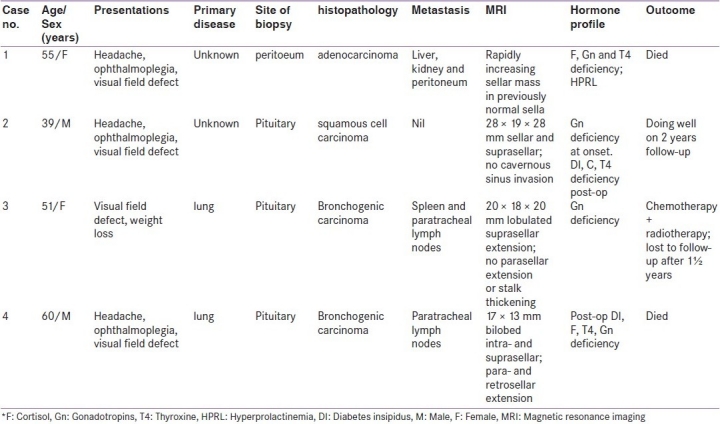
Clinico-radiological features and hormonal profiles of all four cases are summarized in Table 1. In short, the presenting manifestation included the following: mass effect due to pituitary enlargement in three and ophthalmoplegia and diabetes insipidus (DI) in one. The lag period from the onset of symptoms to the diagnosis was between 2 and 5 months. All of them had decreased visual acuity and field of vision.
All four patients had hypopituitarism of variable degree at presentation. One patient had DI at the time of diagnosis, while two patients developed DI after transsphenoidal surgery (TSS). One patient had hyperprolactinemia at presentation. Three patients had secondary hypogonadism. Cortisol deficiency was present in one patient at the time of presentation, while two patients developed it after TSS. Central hypothyroidism was noted in one patient at presentation and one patient developed it after TSS. All patients had normal skull X-ray and coned view of sella except one who had destruction of sella without erosion or double flooring [Figures 1a and b]. On imaging, three patients had both intrasellar and suprasellar metastatic deposits, and one patient had only sellar deposits. In one patient, initial imaging showed primary empty sella; however, repeat imaging, 4 months later, showed sellar and parasellar involvement (case 1) [Figures 2a and b]. Pituitary metastases were iso-intense on T1-weighted image, moderately hypointense on T2-weighted image and showed variable enhancement after contrast administration. These tumors, with sellar and suprasellar components, were dumb-bell shaped with a distinct indentation at diaphragm sella. Though ophthalmoplegia was present in three patients, apparent cavernous sinus involvement on imaging was found in only one patient. One patient had stalk thickening without DI, two patients had DI without stalk thickening, while the fourth patient had neither DI nor stalk thickening.
Figure 1.
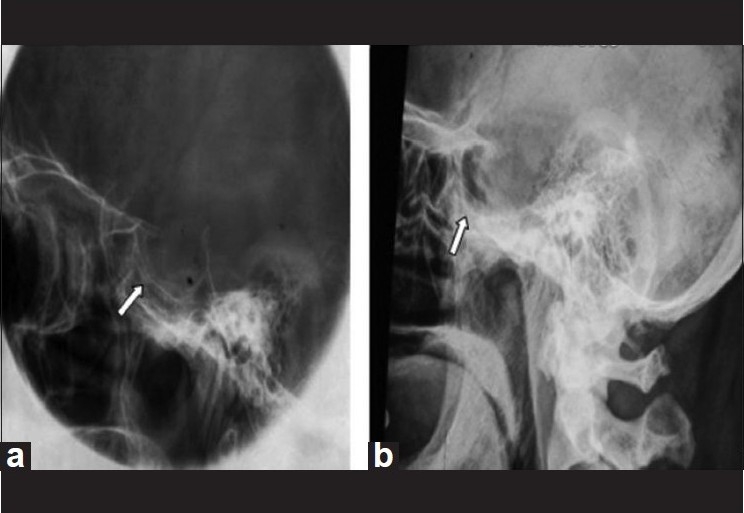
X-ray sella coned view shows double flooring of sella (a), classical of pituitary adenoma, while destruction of sellar floor is suggestive of pituitary metastasis (b)
Figure 2.
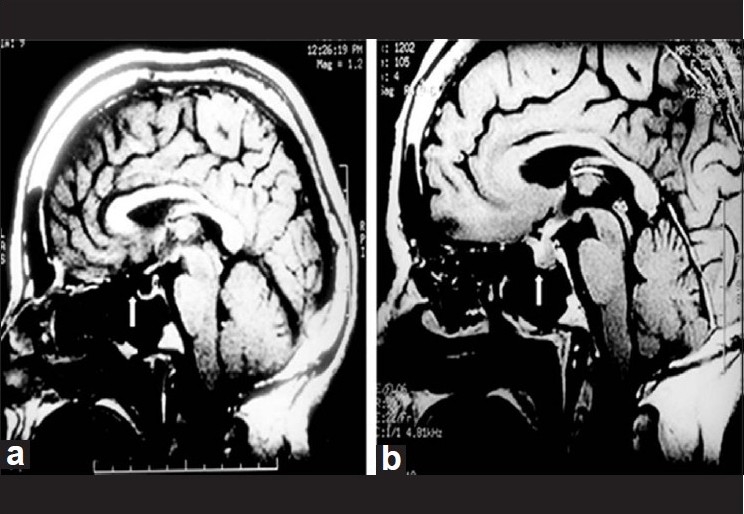
Magnetic resonance imaging shows empty sella (a) which was filled up by rapidly progressive mass in the pituitary region suggestive of pituitary metastasis.(b)
DISCUSSION
Our study shows that pituitary metastasis may be the only presenting manifestation of malignant disease elsewhere. Short lag time between onset of symptoms and presentation, presence of diabetes insipidus, ophthalmoplegia, signs and symptoms disproportionate to tumor size, and rapidly growing sellar mass and destroyed but normal sized sella are some clues to suggest the diagnosis of pituitary metastasis.
Breast carcinoma in women and bronchogenic carcinoma in men are the most common primary tumors with pituitary metastasis.[4] Only 7% of pituitary metastasis found at autopsy are symptomatic for the local pathology in the pituitary.[5,6] Though pituitary metastasis is commonly found in elderly population, one of our patients was young with age at presentation below 40 years. Short lag time between onset of symptoms and clinical presentation is more suggestive of pituitary metastasis than pituitary adenoma. The lag time of 2to 5 months was observed in our study. In majority of cases, the primary malignancy is obvious and widespread by the time pituitary metastasis is present.[6] However, despite the use of whole body CT scan, MRI and 18Fluoro deoxyglucose Position Emission Tomography scan (18FDG-PET), the primary site of malignancy could not be identified in two of our patients.
The most important clinical clue to differentiate pituitary adenoma from metastasis is the presence of DI.[6,7] In our study, one patient had DI at presentation and two developed in the immediate postoperative period. DI is caused by metastatic infiltration, microinfarct, and/or hemorrhage in the stalk and/or hypothalamic nuclei or sometimes in posterior pituitary. Predilection for the tumor to infiltrate the posterior pituitary is due todirect arterial supply to it, therefore, the metastasis first localizes in the capillary bed of posterior pituitary and then reaches the anterior lobe.[8,9]
Visual field defect is a common feature of pituitary adenoma with supra-sellar extension while ophthalmoplegia has much more discriminatory value as compared to visual field defect in patient with pituitary metastasis. In our study, visual acuity and field of vision were compromised in all four patients, and three of them had ophthalmoplegia.. The presence of anterior pituitary hormone insufficiency disproportionate to tumor size and duration of symptoms is more suggestive of pituitary metastasis than adenoma. Hormone excess, other than hyperprolactinemia, is never found in pituitary metastasis. In one of the studies, hypopituitarism was found in 60% of cases with pituitary metastasis and was the presenting feature in 7% of the cases.[8,9] However, in majority of patients, the hormonal insufficiency was purely biochemical, without the presence of clinical manifestations. Hyperprolactinemia, though frequently described in literature, was present in only one of our patients.
Plain radiograph of the sella, though frequently ignored due to availability of modern imaging techniques, is of immense help. Pituitary adenoma, because of its relatively slow growth and benign course, may clinically remain silent for a long time thereby producing slow sellar enlargement,double flooring and destruction of clinoid process. The absence of such findings is characteristic of metastatic disease, even with tumor of similar size[4,5,10] [Figure 1]. Suddenly appearing or a rapidly growing mass on imaging is another clue to suspect pituitary metastasis, as was seen in one of our patients. Stalk thickening, though uncommon, is characteristic of metastasis as opposed to nonfunctioning pituitary adenoma.[10]
Though figure of “8” appearance is common in pituitary adenomas and the waist is usually broad while dumb-bell shaped mass with narrow waist at the level of diaphragma sella is characteristic of pituitary metastasis. Slowly growing adenoma expand and destroys the diaphragma, where asmetastasis seems to respect the diaphragma sellae.[6,7,9,10]
In patients with a clinical suspicion of pituitary metastasis, a transsphenoidal biopsy is recommended to confirm the diagnosis.[11] However, one needs to be more cautious while performing biopsy as the metastatic pituitary deposits may bleed more profusely compared to pituitary adenoma. Nevertheless, this complication was not encountered in our patients.
In conclusion, pituitary metastasis may be the presenting manifestation of a malignant disease elsewhere. Short lagtime,a rapidly appearing mass in sellar region, DI at onset, sudden onset of ophthalmoplegia and a destroyed but normal sized sella favours a diagnosis of pituitary metastasis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brain tumor registry of Japan. Neurol Med Chir (Tokyo) 1992;32:381–547. [PubMed] [Google Scholar]
- 2.Melmed S. Mechanisms for pituitary tumorigenesis: The plastic pituitary. J Clin Invest. 2003;112:1603–18. doi: 10.1172/JCI20401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kovacs K. Metastatic cancer of the pituitary gland. Oncology. 1973;27:533–42. doi: 10.1159/000224763. [DOI] [PubMed] [Google Scholar]
- 4.Roessmann U, Kaufman B, Friede RL. Metastatic lesions of sella tercica and pituitary gland. Cancer. 1970;25:478–80. doi: 10.1002/1097-0142(197002)25:2<478::aid-cncr2820250227>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 5.Teears R, Silverman EM. Clinicopathological review of 88 cases of carcinoma metastatic to pituitary gland. Cancer. 1975;36:216–20. doi: 10.1002/1097-0142(197507)36:1<216::aid-cncr2820360123>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 6.Max MB, Deck MD, Rottenberg DA. Pituitary metastasis: Incidence on cancer patients and clinical differentiation from pituitary adenoma. Neurology. 1981;31:998–1002. doi: 10.1212/wnl.31.8.998. [DOI] [PubMed] [Google Scholar]
- 7.Branch CL, Laws ER. Metastatic tumors of the sella turcica masquerading as primary pituitary tumors. J Clin Endocrinol Metab. 1987;65:469–74. doi: 10.1210/jcem-65-3-469. [DOI] [PubMed] [Google Scholar]
- 8.Rajput R, Bhansali A, Dutta P, Gupta SK, Rachana BD, Bhadada SK. Pituitary metastasis masquerading as pituitary adenoma in a women with adenocarcinoma lung. Pituitary. 2006;9:155–7. doi: 10.1007/s11102-006-8326-0. [DOI] [PubMed] [Google Scholar]
- 9.Morita A, Meyer FB, Laws ER., Jr Symptomatic pituitary metastasis. J Neurosurg. 1998;89:67–73. doi: 10.3171/jns.1998.89.1.0069. [DOI] [PubMed] [Google Scholar]
- 10.Schubiger O, Haller D. Metastasis to pituitary-hypothalamic axis.An MR study of 7 symptomatic patients. Neuroradiology. 1992;34:131–4. doi: 10.1007/BF00588159. [DOI] [PubMed] [Google Scholar]
- 11.Liu H, Yamaki T, Oka S, Koyanagi I, Houkin K. Metastatic renal cell carcinoma mimicking pituitary adenoma: A case report. Neurol Med Chir (Tokyo) 2005;45:418–22. doi: 10.2176/nmc.45.418. [DOI] [PubMed] [Google Scholar]


