Abstract
Primary hydatid cyst of the pancreas represents a rare clinical entity. The clinical presentation depends on the location of a hydatid cyst in the pancreas. A hydatid cyst located in the head of the pancreas usually manifests as obstructive jaundice due to the extrinsic compression of the common bile duct. A case of a hydatid cyst of the head of the pancreas in a 4-year-old female is reported. She presented with abdominal pain and jaundice. Contrast-enhanced computed tomography scan of the abdomen revealed a cystic mass at the lower end of the common bile duct, which mimicked a choledochal cyst. The diagnosis of hydatid cyst was made intraoperatively, with postoperative findings revealing a hydatid cyst at the head of the pancreas that was compressing the lower end of the common bile duct. After cystectomy, no recurrence was seen in follow-up.
Hydatid disease is a serious health problem in endemic areas. Most human infections are due to Echinococcus granulosa transmitted between synanthropic hosts and livestock, while Echinococcus multilocularous infection is uncommon and appears to be endemic in specific areas such as Siberia, northern Canada and Bararia, India.1 The pancreas is considered a rare, atypical location for a hydatid cyst. Involvement of the pancreas in hydatid disease has an incidence ranging between 0.2% and 2.0%.2 Only a few cases of hydatid cyst in the head of the pancreas have been reported.3 The embryo of a hydatid cyst ends up in the pancreas mainly by hematogenous spread. The clinical presentation of pancreatic hydatid disease depends on the size and anatomic location of the cyst and is usually due to the pressure effect of the cyst on adjacent structures. Abdominal pain, obstructive jaundice and an abdominal mass are the most common presenting symptoms of hydatid cyst of the head of pancreas. Hydatid cysts of the pancreas are generally difficult to diagnose preoperatively and, because of their rarity, may be mistaken for more commonly encountered cystic lesions. Surgery remains the treatment of choice for hydatid cyst of the pancreas.
CASE
A 4-year-old female presented with upper abdominal pain of 4 months duration and yellowish discoloration of the eyes of 2 months duration. There was no history of fever, vomiting or weight loss. On general physical examination, a yellowish discoloration of the sclera was seen. The systemic examination was unremarkable. Abdominal examination revealed a nontender, soft cystic globular swelling filling the epigastrium and right hypochondrium. The complete blood count was normal except for an eosinophilic count of 25% (normal, 0-2%). Liver function tests showed a bilirubin of 8.6 mg/dL (normal, 0-1.5 mg/dL), and alkaline phosphatase was 1843 U/L (normal, 100-320 U/L). X-ray of the abdomen showed a soft tissue shadow in the upper abdomen, and the chest x-ray was normal. Ultrasonography of the abdomen revealed an anechoic lesion measuring 10×15×7 cm with a well-defined thin margin in relation to the distal common bile duct, which was dilated, along with intrahepatic biliary channels. Computerized tomography of the abdomen showed a large uniform cystic density mass with a well-defined wall in relation to the head and body of pancreas with dilatation of the common bile duct and both hepatic ducts (Figure 1). The liver was normal. A diagnosis of choledochal cyst was made. The patient had an exploratory laparotomy; the gall bladder was distended with a dilated cyst and common bile duct. A cystic mass measuring 10×15× 7 cm occupying the lesser sac with a loop of the duodenum stretched over the mass was seen (Figure 2). The operative area was protected by a 0.5% cetremide solution, and the cyst was aspirated and the germinal membrane was extracted (Figure 3). There was no communication between the ectocyst and the pancreatic ducts. A postoperative cholangiography was done to check the patency of the common bile duct. The lower end of the common bile duct traversed the medial wall of the ectocyst, as confirmed during cholangiography. External draining of the cavity was done. Hydatid serology was negative. The patient was discharged on albendazole, with an uneventful follow-up for the next 2 years.
Figure 1.
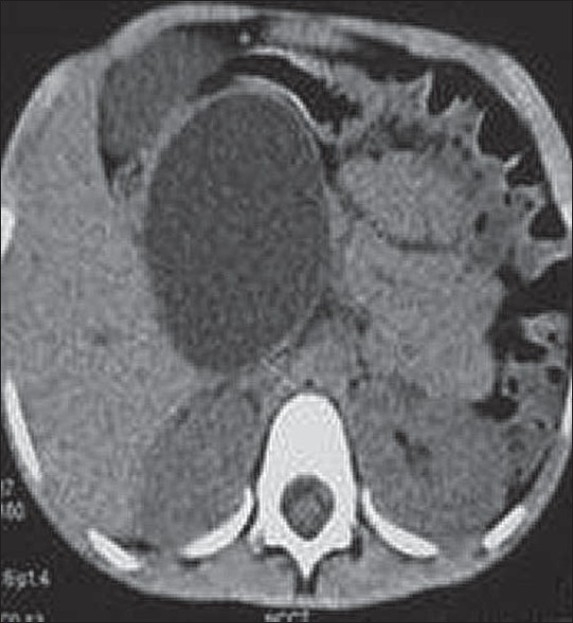
Large uniformly cystic density mass in relation to the head and body of pancreas with dilatation of common bile duct and both hepatic ducts (CT scan).
Figure 2.

Distended gallbladder, cystic duct with a large cystic swelling in relation to the lower end of the common bile duct.
Figure 3.

Germinal layer of hydatid cyst being removed.
DISCUSSION
Pancreas is an uncommon site for a hydatid cyst, even in countries where echinococcal disease is endemic. The most probable route of pancreatic infestation is hematogenous dissemination after passage of the embryo through both liver and lung. Migration of embryos down the bile duct into the pancreatic duct via the lymphatic circulation from the intestinal mucosa to the pancreas or by portal blood into pancreatic veins has also been suggested, these being less likely, but other possible routes.4 Involvement of the pancreas in hydatid disease has the following distribution pattern: in head, 57%; body, 24%; and tail, 19%.5
Clinical presentation is variable and insidious, depending on the location and the size of cyst.2 Epigastric pain, discomfort, vomiting and weight loss are the main symptoms.6 Obstructive jaundice is caused by the extrinsic compression of the common bile duct by cysts located in the head of the pancreas.7 Cholangitis, duodenal stenosis or fistula, acute and chronic pancreatitis, pancreatic abscess and pancreatic fistula due to compression and erosion into the pancreatic ducts are unusual complications of hydatid cysts involving the head of the pancreas. Cysts located in the body or tail of the pancreas are virtually symptomless and may be detected only as the presence of a mass and its subsequent effect. Cysts in the body and tail of the pancreas may be asymptomatic or may present as a palpable mass. Mesenteric vein thrombosis and segmental portal hypertension due to splenic vein thrombosis are uncommon presentations of cysts in the body and tail of pancreas.8–10 Rarely, the cyst ruptures spontaneously into the peritoneal cavity, or gastrointestinal tract and abscess formation occurs.11
Diagnosis is seldom made preoperatively unless hydatid disease is suspected. A high level of clinical suspicion with laboratory and imaging studies sometimes helps in making the diagnosis. Imaging studies used are ultrasound, computed tomography and magnetic resonance imaging (MRI), but these methods have limited sensitivity in making a specific diagnosis because of the considerable overlap of imaging features.12 Identification of a hydatid cyst as a choledochal cyst is based on the presence of intimal contact between the hydatid cyst and the lower end of common bile duct.
The surgical removal of the cyst is a definitive treatment; and to prevent dissemination, the protection of the operative field and sterilization of the cyst with a scolicidal solution are necessary.3 Depending on the site, various methods of surgical treatment have been used. Cysts located in the head of pancreas have been treated by various methods. Pericystectomy with drainage of the residual cavity is the technique of choice.11,13 Pericystectomy can be total or partial. If the cyst is communicating with the main pancreatic duct, then distal pancreatectomy is the procedure of choice, or a cystoenteric anastomosis. Partial pericystectomy is the choice where there is an inadvertent risk to surrounding structures; otherwise, total pericystectomy is preferable. The Whipple resection, or marsupialization, has been done in some cases of hydatid cyst of the pancreatic head. Percutaneous drainage of the cyst is a good alternative to surgery in patients with high surgical risk; and in such cases, it must be combined with medical chemoprophylaxis using albendazole.14 Hydatid cyst in the head of the pancreas is extremely rare, but should be included in the differential diagnosis of cystic lesion of the pancreas.
REFERENCES
- 1.Safioleas MC, Moulakakis KG, Manti C, Kostakis A. Clinical considerations of primary hydatid disease of the pancreas. Pancreatology. 2005;5:457–61. doi: 10.1159/000086548. [DOI] [PubMed] [Google Scholar]
- 2.Rausch RL. Cystic echinococcosis in the Arctic and Sub-Arctic. Parasitology. 2003;127:S73–85. doi: 10.1017/s0031182003003664. [DOI] [PubMed] [Google Scholar]
- 3.Jai SR, El Hattabi K, Bensardi F, Chehab F, Khaiz D, Bouzidi A. Primary hydatid cyst of the pancreas causing obstructive jaundice. Saudi J Gastroenterol. 2007;13:191–3. doi: 10.4103/1319-3767.36752. [DOI] [PubMed] [Google Scholar]
- 4.Krige J, Mirza K, Bornman P, Beningfield S. Primary hydatid cysts of the pancreas. S Afr J Surg. 2005;43:37–40. [PubMed] [Google Scholar]
- 5.Gayral F, Bourree P, Jourdanne PH, Millat Kyste hydatique du pancreas: Une observation. Presse Med. 1998;10:3787–8. [PubMed] [Google Scholar]
- 6.Moosavi S, Khajouei H. Epigastric mass due to a hydatid cyst of the pancreas.A case report and review of the literature. JOP. 2007;8:232–4. [PubMed] [Google Scholar]
- 7.Ozmen M, Moran M, Karakahya M, Coskun F. Recurrent acute pancreatitis due to a hyudatid cyst of the pancreatic head.A case report and review of the literature. JOP. 2005;6:354–8. [PubMed] [Google Scholar]
- 8.Wong S, Braghirolli-Neto O, Min Zu, Buckels J, Mirza D. Hydatid liver disease as a cause of recurrent pancreatitis. J R Coll Surg Edin. 1999;44:407–9. [PubMed] [Google Scholar]
- 9.Coskun T, Kama NA, Dener C, Gözalan U. Primary hydatid disease of the pancreas. Am J Gastroenterol. 1997;92:899–900. [PubMed] [Google Scholar]
- 10.Barrera MC, Villanua J, Barrena JF, Nogues A. Pancreatic Hydatid disease. Pediatr Radiol. 1995;25:169–70. [PubMed] [Google Scholar]
- 11.Arikkan A, Sayan V, Eriki S. Hydatid cyst of the pancreas: a case report with 5 - years follow - up. Pediatr Surg Int. 1999;15:579–81. doi: 10.1007/s003830050677. [DOI] [PubMed] [Google Scholar]
- 12.Missas S, Gouliamos A, Kourias E, Kalovidouris A. Primary hydatid disease of the pancreas. Gastrointest Radiol. 1987;12:37–8. doi: 10.1007/BF01885099. [DOI] [PubMed] [Google Scholar]
- 13.Faucompret S, Farthouat P, Sainton T, Breda Y. Complicated hydatid cyst of the pancreas after needle biopsy. Ann Chir. 2001;126:491–2. doi: 10.1016/s0003-3944(01)00536-3. [DOI] [PubMed] [Google Scholar]
- 14.Yattoo N, Khuroo S, Zargar S, Bhat F, Sofi B. Percutaneous drainage of the pancreatic head Hydatid cyst with obstructive jaundice. J Gastroenterol Hepatol. 1999;14:931–4. doi: 10.1046/j.1440-1746.1999.01967.x. [DOI] [PubMed] [Google Scholar]


