Abstract
Topical anesthetics rapidly ease ear pain in distressed children
Practice changer
Use 3 drops of topical 2% lidocaine drops or benzocaine to provide rapid pain relief for children with acute otitis media.1
Strength of recommendation
B: 2 good-quality, randomized controlled trials
Bolt P, Barnett P, Babl FE, Sharwood LN. Topical lignocaine for pain relief in acute otitis media: results of a double-blind placebo-controlled randomised trial. Arch Dis Child. 2008;93:40–44.
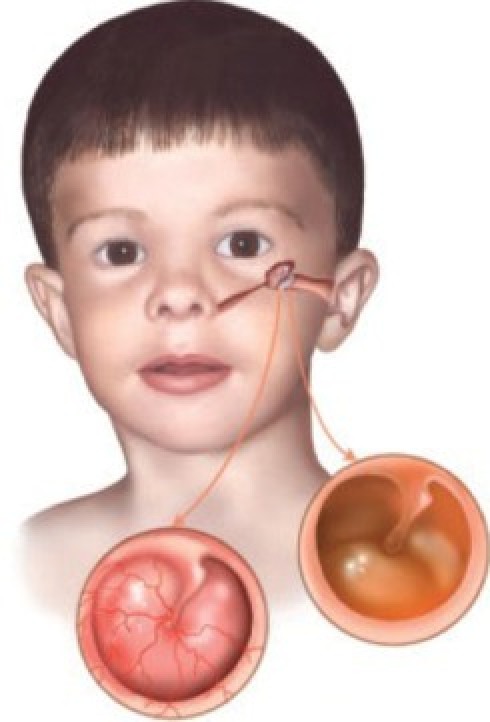
ILLUSTRATIVE CASE
A mother brings her 3-year-old son to your office first thing in the morning. The boy has fever and right ear pain. You see that the tympanic membrane is dull, red, and bulging. The mother has been up most of the night with her child. She implores you to “do something.” She is exhausted and her son is crying and holding his right ear. You know that antibiotics will not provide immediate pain relief and oral analgesics will take a while to help. What can you offer that will help right away?
FAST TRACK
Topical anesthetics are a useful option with acute ear pain whether due to otitis externa or acute otitis media
Until this study, we’ve had only 1 placebo-controlled trial to guide how we manage a big problem. Big in terms of distress to parents and children, and in sheer numbers—acute otitis media (AOM) is extremely common in children.2,3
Routine antibiotics: Woeful lack of evidence
Even when antibiotics are indicated, pain relief is minimal and takes several days.4-8 Despite “a woeful lack of substantial evidence on the question of antibiotic therapy” for AOM, it is the most common reason for the prescription of antibiotics in children.4,6 A Cochrane review showed that antibiotics have no effect on recurrence of AOM or complications, including hearing impairment.5 The same review showed no pain reduction in 24 hours and only 30% pain reduction in 2 to 7 days with antibiotic use.5 Antibiotics clearly have a minimal role in providing pain relief for AOM.
Oral analgesics too slow
Oral analgesic use in AOM has been studied and has shown good results. We calculated the number needed to treat (1.0 divided by the absolute risk reduction) for both ibuprofen (number needed to treat [NNT]=5) and acetaminophen (NNT=6) from data in the 1996 trial by Bertin et al.9
It is a common practice in the United States to treat AOM with oral analgesics. However, the onset of pain relief with oral medications can be slow and the relief is generally not complete, so oral medications are not immediately helpful to meet the needs of our crying 3-year-old patient and his exhausted mother.
Topical anesthetics
To our knowledge, prior evidence on the efficacy of topical anesthetics is limited to 1 placebo-controlled trial. A randomized trial by Hoberman et al,10 with 54 subjects, showed a statistically significant 25% reduction in pain with the analgesic drops Auralgan (containing antipyrine, benzocaine, and glycerine) at 30 minutes when compared with olive oil. A 2006 Cochrane review11 did not include the Bolt et al trial1 described in this PURL, but did include the Hoberman trial10 and 3 trials that compared a topical anesthetic with naturopathic herbal ear drops for AOM pain, and the review concluded that evidence was insufficient.
Topical anesthetic plus oraI analgesia for earache relief
Topical aqueous 2% lidocaine eardrops provide rapid relief for many young children presenting with ear pain attributed to acute otitis media
Simple oral analgesia, used concurrently, is a likely contributor to effective management of this painful childhood condition
Bolt P et al.1
STUDY SUMMARY: Pain measured by visual analogue, Bieri faces scales
This double-blind, randomized, placebo-controlled trial1 compared aqueous lidocaine 2% drops with saline drops in the ear, for reducing pain due to AOM in patients 3 to 17 years of age. The trial was conducted at an Australian children’s hospital emergency room. The study evaluated “lignocaine,” the name for lidocaine in Australia.
Emergency physicians instilled 3 drops of either lidocaine or saline into the affected ear in the 2 groups (n=31 in the study group and n=32 in the placebo group). Patients, parents, treating physicians, and staff administering ear drops and assessing pain were blinded to group assignment. Doctors measured pain at baseline and after 30 minutes and patients measured pain at baseline, 10, 20, and 30 minutes after the drops were instilled, using the Bieri faces pain scale and a visual analogue scale.12
FAST TRACK
The results of this study are consistent with increased uptake of the drug through the inflamed tympanic membrane
Lidocaine reduced pain scores by 50% from baseline at 10 and 30 minutes compared with saline. No serious side effects were noted at 30 minutes, although 3 patients in the lidocaine group complained of mild dizziness the next day. The treating physician prescribed paracetamol (equivalent to acetaminophen) for participants in both the lidocaine and the placebo group at their discretion. The proportion given paracetamol was similar in both groups.
WHAT’S NEW: Pain relief is immediate
Family physicians have used topical anethestics for otitis externa for decades. This RCT adds evidence that topical anesthetics are useful for providing immediate pain relief from AOM, as well. The 2004 guidelines from the American Academy of Pediatrics and the American Academy of Family Physicians indicate that management of AOM should include the assessment and treatment of pain.
We think that topical agents such as lidocaine and benzocaine are useful adjuncts to oral analgesics in providing immediate pain relief, especially in the face of evidence showing that antibiotics do not offer significant pain relief.
Previous studies have shown that aqueous lidocaine is ineffective on uninflamed tympanic membrane.13 The results of this study are consistent with increased uptake of the drug through the inflamed tympanic membrane.
CAVEATS: Children >3 years studied
This trial included only children older than 3 years, so the results may not apply to younger children and infants.
This essentially was a study of ear pain treatment, which, in our view, does not detract from the clinical usefulness of the findings. Topical anesthetics seem to be useful for ear pain in general.
Concurrent analgesics
Some variability existed in the oral analgesics the children received, as these agents were given at the discretion of the parents and treating physicians. We think that this does not detract from the study findings, as it represents a practical, real-world setting, which is desirable in an effectiveness RCT. Moreover, the extent of pain reduction was over and above that conferred by analgesic administration.
CHALLENGES TO IMPLEMENTATION: Lidocaine is not sold in a dropper
Aqueous lidocaine is not sold in a bottle with a dropper: our search on www.drugstore.com and www.drugs.com did not yield an otic preparation with only aqueous lidocaine. However, 2% injectable lidocaine, which is readily available, can be used with a dropper. Aqueous lidocaine can be compounded at a compounding pharmacy and placed in a bottle with a dropper.
Benzocaine might be a suitable substitute
In preparing this PURL, we learned from several colleagues that they always keep a bottle of benzocaine in their pocket and they apply the drops to the ears of their pediatric patients with AOM when they see them in their offices or in the emergency department.
FAST TRACK
Oil suspensions cannot be given if the eardrum is ruptured
Benzocaine is available in various brand names (eg, Auralgan, Americaine, A/B otic drops, among others). These are oil suspensions and not an aqueous solution as used in this study, so it would be important not to use these preparations in the presence of a ruptured tympanic membrane because the oil suspension may not be absorbed. The aqueous solution will be absorbed so it can be used even if a ruptured tympanic membrane is suspected.
In most situations rupture of the tympanic membrane gives immediate pain relief. However, in some, the pain persists and it may be difficult to tell if the tympanic membrane has ruptured or the debris and pus is from otitis externa. In those situations, the aqueous lidocaine solution might be preferred.
Should parents give drops at home?
This study does not address home use of these drops. However, benzocaine preparations have been used safely for many years for otitis externa at home, and we cannot think of any reason why drops could not be prescribed for home use in acute otitis media.
PURLs methodology This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Contributor Information
Shailendra Prasad, Department of Family Medicine and Community Health, University of Minnesota, Minneapolis.
Bernard Ewigman, Department of Family Medicine, The University of Chicago.
John Hickner, Department of Family Medicine, The University of Chicago.
References
- 1.Bolt P, Barnett P, Babl FE, Sharwood LN. Topical lignocaine for pain relief in acute otitis media: results of a double-blind placebo-controlled randomised trial. Arch Dis Child. 2008;93:40–44.. doi: 10.1136/adc.2006.110429. [DOI] [PubMed] [Google Scholar]
- 2.Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989;160:83–94.. doi: 10.1093/infdis/160.1.83. [DOI] [PubMed] [Google Scholar]
- 3.Arnold J. Otitis media and its complications. In: Nelson W, Behrman R, Kliegman R, Arvin A, eds. Nelson Textbook of Pediatrics. 15th ed. Philadelphia: Saunders; 1996:1814-1824. [Google Scholar]
- 4.Chan LS, Takata GS, Shekelle P, Morton SC, Mason W, Marcy SM. Evidence assessment of management of acute otitis media: II. Research gaps and priorities for future research. Pediatrics. 2001;108:248–254.. doi: 10.1542/peds.108.2.248. [DOI] [PubMed] [Google Scholar]
- 5.Glasziou PP, Del Mar CB, Sanders SL, Hayem M. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219.. doi: 10.1002/14651858.CD000219.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Hendley JO. Clinical practice. Otitis media. N Engl J Med. 2002;347:1169–1174.. doi: 10.1056/NEJMcp010944. [DOI] [PubMed] [Google Scholar]
- 7.Rovers MM, Glasziou P, Appelman CL, et al. Antibiotics for acute otitis media: a meta-analysis with individual patient data. Lancet. 2006;368:1429–1435.. doi: 10.1016/S0140-6736(06)69606-2. [DOI] [PubMed] [Google Scholar]
- 8.Gasper K, St Anna L, Montgomery L. Clinical inquiries. Are antibiotics effective for otitis media with effusion? J Fam Pract. 2003;52:321–323.. [PubMed] [Google Scholar]
- 9.Bertin L, Pons G, d’Athis P, et al. A randomized, double-blind, multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam Clin Pharmacol. 1996;10:387–392.. doi: 10.1111/j.1472-8206.1996.tb00590.x. [DOI] [PubMed] [Google Scholar]
- 10.Hoberman A, Paradise JL, Reynolds EA, Urkin J. Efficacy of Auralgan for treating ear pain in children with acute otitis media. Arch Pediatr Adolesc Med. 1997;151:675–678.. doi: 10.1001/archpedi.1997.02170440037006. [DOI] [PubMed] [Google Scholar]
- 11.Cochrane Database Syst Rev. doi: 10.1002/14651858.CD005657.pub2. 2006 Jul 19;3: CD005657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain. 2001;93:173–183.. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 13.Moller A, Grontved A. Topical anaesthesia of the normal tympanic membrane: a controlled clinical trial of different suspensions of lidocaine. ORL J Otorhinolaryngol Relat Spec. 1990;52:168–173.. doi: 10.1159/000276128. [DOI] [PubMed] [Google Scholar]


