Abstract
Existing research has shown that anxiety sensitivity (AS) is positively associated with alcohol use and that individuals with high AS use alcohol to avoid or escape negative affect associated with aversive stimuli. The current study investigated the associations between AS and drinking behavior among individuals with comorbid alcohol dependence and posttraumatic stress disorder (PTSD). We assessed baseline PTSD symptoms, AS, and drinking behavior among participants (N = 151) who were enrolled in a randomized clinical trial for alcohol dependence. We hypothesized that AS would moderate the association between PTSD symptoms and drinking behavior, with PTSD symptoms being more strongly associated with drinking behavior among individuals with high AS. Results showed that AS was strongly associated with PTSD (r = .48) and moderately associated with drinking behavior (r = .18). As predicted, the interaction of AS with severity of PTSD symptoms was associated with frequency of drinking; however, contrary to our hypothesis, PTSD symptoms were more strongly associated with drinking behavior among individuals with relatively low AS. The implication of the present results for treatment of both PTSD and alcohol dependence are discussed.
Keywords: Posttraumatic stress disorder, alcohol dependence, anxiety sensitivity
One of the variables that has been found consistently to predict problematic use of alcohol is anxiety sensitivity. Anxiety sensitivity (AS) is defined as the fear of anxiety (or “fear of fear”) and its attendant sensations (e.g., Reiss, Peterson, Gursky, & McNally, 1986); seminal work on the construct revealed that it is somewhat distinct from anxiety itself, capturing instead individual differences in reactions to anxiety. Although different individuals might experience relatively similar levels of anxiety, individuals who are high in AS are more likely to be disturbed by the anxiety and to develop an anxiety disorder; accordingly, AS is a moderator of the association between anxiety and various outcomes. Subsequent research has described AS as an “amplifier” of negative states, including anxiety as well as other aversive experiences such as pain (e.g., Asmundson & Norton, 1995).
Many studies have reported that AS is positively associated with alcohol use (e.g., Stewart, 1995; Stewart, Peterson, & Pihl, 1995; Stewart, Zvolensky, & Eifert, 2001). In a prospective study AS was found to be a risk factor for problematic alcohol use: AS at baseline predicted alcohol use disorders 2 years later (Schmidt, Buckner, & Keough, 2007). AS remains a predictor of alcohol use even after controlling for trait anxiety (Dehaas, Calamari, & Bair, 2002; Dehaas, Calamari, Bair, & Martin, 2001), suggesting that its effect on drinking behavior is not attributable simply to higher levels of anxiety.
Existing research supports the hypothesis that individuals with high AS use alcohol as a means to avoid or escape from negative affective states associated with aversive stimuli (Dehaas et al., 2002; Dehaas et al., 2001; Reyno, Stewart, Brown, Horvath, & Wiens, 2006; Stewart et al., 2001); that is, AS appears to moderate the relationship between negative affect and alcohol use. For example, AS predicts alcohol use in contexts such as interpersonal conflicts or physical discomfort, whereas in more affectively positive settings such as pleasant times with others, AS is unrelated to alcohol use (Dehaas et al., 2002; Dehaas et al., 2001; Reyno et al.). In addition, individuals with high AS report particularly more alcohol use in negative emotion situations than do low AS individuals, in both clinical (Dehaas et al., 2002; Dehaas et al., 2001; Reyno et al.) and nonclinical populations (Samoluk & Stewart, 1998). Individuals with high AS also have higher sensitivity to the fear dampening effects of alcohol than do individuals with low AS (MacDonald, Baker, Stewart, & Skinner, 2000; Stewart & Pihl, 1994; Zack, Poulos, Aramakis, Khamba, & MacLeod, 2007), which likely contributes to the motivation for high-AS individuals to drink alcohol in stressful situations. This effect has been demonstrated in both men and women (MacDonald et al.; Zack et al.).
Several studies have investigated the role of AS in alcohol use disorders among individuals with anxiety disorders. Dehaas et al. (2001) found that AS predicted drinking and drug use in substance users with comorbid anxiety disorders; similarly, Dehaas et al. (2002) reported that among individuals with anxiety disorders, use of depressants like alcohol was more common among high AS individuals when they encountered negative situations. Individuals with high levels of AS who also have posttraumatic stress disorder (PTSD) may be at particular risk for problematic alcohol consumption given the high levels of stress and anxiety that define PTSD. Therefore it is important to identify the specific variables that interact with AS to predict greater alcohol use among individuals with PTSD. Identification of these variables may lead to more targeted treatments that specifically address the use of alcohol to dull fear-related symptoms following a trauma.
A small number of studies have examined the relationship between AS and alcohol use in individuals with comorbid PTSD. Simpson, Jakupcak, and Luterek (2006) found no significant relationship between AS and either alcohol use or alcohol craving among patients with PTSD; however, AS was significantly correlated with PTSD symptom clusters, alexithymia, and difficulty controlling negative thoughts. Baseline AS also accounted for a substantial proportion of the variance in predicting both baseline and follow-up PTSD scores across all symptom clusters, including re-experiencing (e.g., nightmares, flashbacks), avoidance (e.g., trying not to think about the trauma, feelings of detachment from others), and hyperarousal (e.g., difficulty sleeping, jumpiness). Veterans with chronic hepatitis C also have been found to have positive correlations among PTSD symptoms, AS, and alcohol use (Lehman & Cheung, 2002), although this study did not examine the variables that might interact with AS to lead to alcohol abuse or dependence.
In sum, there is strong evidence that AS is associated with drinking behavior, as well as evidence that individuals with anxiety disorders like PTSD may be particularly vulnerable to using alcohol as a means to dampen anxiety. Only a small number of studies have assessed the associations among AS, alcohol use, and PTSD. Thus while existing research has begun to elucidate how AS affects drinking behavior among individuals with PTSD, additional work is necessary to determine the variables that interact with AS to predict problematic alcohol use.
The purpose of the current study was to examine whether AS moderates the association between trauma symptoms and alcohol consumption, using a large sample (N = 151) of individuals with comorbid PTSD and alcohol dependence. We hypothesized that severity of trauma symptoms would interact with AS to predict greater alcohol consumption. Specifically, we predicted that for high AS individuals, more severe trauma-related symptoms would be associated with a greater degree of drinking, whereas for low AS individuals, more severe trauma symptoms would not affect the degree of drinking. This prediction was based on previous research showing greater sensitivity to anxiety symptoms associated with high AS, and the greater subsequent motivation to dampen these symptoms through the use of alcohol (e.g., Dehaas et al., 2002).
Method
Participants
Participants (N = 151) were adults with alcohol dependence (AD) and posttraumatic stress disorder (PTSD), as defined by the DSM-IV, who participated in the National Institute on Alcohol Abuse and Alcoholism- (NIAAA) funded randomized, placebo-controlled, double-blinded clinical trial, “Naltrexone and CBT for Patients with Alcoholism and PTSD” (PI: Edna B. Foa, Ph.D.). The majority of participants were male (70.0%), were on average 42.8 years of age (SD = 9.8), and 64.2% had an average income of $30,000 or less. The majority of patients were black (64.2%), and the remainder identified as white (29.8%), Hispanic (4.0%), or other (2.0%). Most participants were recruited through public advertisements (e.g., free city newspapers). Potential participants were screened during an initial phone interview.
Procedure
Data were collected at nine different assessment time points over the course of 1 year (at weeks 0, 4, 8, 12, 16, 20, 24, 38, and 52). At each assessment, the Anxiety Sensitivity Index (ASI) was completed by the patient as part of a larger packet of questionnaires, and the PTSD Symptom Scale Interview (PSS-I) was administered by a trained masters or doctoral level clinician. The Timeline Follow-Back (TLFB) was administered weekly by a trained research assistant.
Measures
The Anxiety Sensitivity Index (ASI; Reiss et al., 1986) is a 16-item self-report questionnaire that measures the extent to which individuals are sensitive to emotional or physical sensations that they may experience. Participants are asked to respond based on the extent to which they agree with each statement (e.g., “It scares me when I feel faint”; “It scares me when I feel ‘shaky’”). Responses are rated on a Likert-type scale that ranges from 0 (very little) to 4 (very much). Earlier studies have shown that the ASI has adequate test/retest reliability (r =.71) and good internal consistency (Reiss et al., 1986); internal consistency for the ASI in the current study was excellent (Cronbach’s α = .92).
The PTSD Symptom Scale Interview (PSS-I; Foa, Riggs, Dancu, & Rothbaum, 1993), a 17-item clinical interview, was used to assess the severity of DSM-IV PTSD symptoms. Participants are asked about the nature and frequency of PTSD symptoms they have experienced in the past 2 weeks. Responses are coded using a four-point scale that ranges from 0 (“not at all”) to 3 (“5 or more times per week/very much”). The PSS-I yields a total sum score of the 17 items (range = 0 – 51), and three subscales: Re-experiencing (5 items, range = 0 – 15), Avoidance (7 items, range = 0 – 21), and Hyperarousal (5 items, range = 0 – 15). Foa et al. (1993) found the PSS-I to have excellent internal consistency (Cronbach’s α = .85); symptom cluster subscales alpha coefficients were Re-experiencing .69, Avoidance .65, and Hyperarousal .71. Foa et al. also found the PSS-I also to have good test/retest reliability (r = .80) and excellent convergent validity (94% accuracy, compared to the Structured Clinical Interview for DSM-III-R; Spitzer, Williams, & Gibbon, 1989). The total score in the present study was found to have good internal consistency (Cronbach’s α = .75), and each subscale was found to have acceptable to good internal consistency: Re-experiencing (Cronbach’s α = .62), Avoidance (α = .59), and Hyperarousal (α = .52).
The Timeline Follow-Back Interview (TLFB; Sobell & Sobell, 1995), a calendar-based measure, was used to assess baseline alcohol consumption on a daily basis for the time since the previous assessment. In the current study, internal consistency was found to be good (Cronbach’s α = .71). For the purpose of the present study, we used percent days drinking (PDD) as the outcome measure since it was the primary alcohol behavior outcome measure in the parent study.
Data Analysis
Because data were collected in the context of a treatment study, all patients at baseline had relatively high levels of PTSD symptoms and drinking frequency. For this reason, data were selected cross-sectionally from the nine assessment points (weeks 0–52) in order to avoid a restriction of range on the variables of interest. For each assessment point we selected approximately 17% of the cases that had data for that point; the raw number of selected cases varied somewhat at each assessment point depending on the number of cases that had data at that point. A total of 151 cases were represented in the sample of selected cases, ranging from 16.3% (14/86) of cases selected at week 8 to 19.2% (25/130) of cases taken from week 0.
Data were normally distributed, thus general linear regressions were conducted to examine ASI as a moderator of the association between PTSD symptom severity and alcohol consumption. Assessment time point was entered as a covariate (as weeks completed), to control for the possible symptom reduction as a result of treatment at time points > 0.
Results
Patients on average reported drinking 25.9% (SD = 34.5) of the days prior to the assessment time point. The mean age at which the index trauma was experienced was 20.7 (SD = 13.2), and participants on average had moderately severe PTSD as assessed by the PSS-I (M = 19.3, SD = 11.5).
Correlational Analyses
We hypothesized that AS would moderate the association between PTSD severity and percentage of drinking days. For individuals high in AS, we predicted that higher PSS-I scores would be associated with a greater drinking frequency (PDD), whereas for individuals low in AS, higher PSS-I scores would not affect the degree of drinking. Bivariate correlations were conducted to examine the variables that may moderate the association between AS and drinking behavior (see Table 1). The total PSS-I score and PDD were positively and significantly correlated with ASI. Further, the subscales of the PSS-I were examined individually, and were found to be significantly correlated with ASI. We then examined the interactions between ASI and PTSD symptoms on drinking behavior.
Table 1.
Bivariate associations among PDD, anxiety sensitivity, and PTSD symptoms
| Variable | Mean (SD) | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. PDD | 25.1 (34.5) | .18† | .29* | .27* | .29* | .27* |
| 2. ASI | 21.4(15.7) | - | .48** | .44** | .40** | .40** |
| 3. PSS-I: Total | 19.3(11.5) | - | .91** | .77** | .85** | |
| 4. Re-experiencing | 8.2 (5.6) | - | .62** | .68** | ||
| 5. Avoidance | 4.1 (3.5) | - | .54** | |||
| 6. Hyperarousal | 7.2 (4.5) | - |
p < .05,
p < .01,
p < .001
Note: PDD = percent days drinking; ASI = Anxiety Sensitivity Index; PSS-I = PTSD Symptom Scale Interview
Moderators of the Effect of PTSD Symptoms on PDD
A series of multiple regressions was conducted to assess whether anxiety sensitivity (measured by ASI) interacted with the PSS-I and its subscales to predict variance in PDD. Following recommendations by Aiken and West (1991), all predictors were mean-centered before being entered into the regression, in order to correct for collinearity. Post hoc variance inflation factor (VIF) values were examined and found to be low (< 2), and tolerance values found to be high (> 0.7).
In each model, gender and assessment point (week) were entered in the first block as covariates. Next, PSS-I (total or subscale score) was entered, followed by the putative moderator variable (ASI) in order to assess for main effects. The interaction term was entered last, thus five variables were entered into each model. Total PSS-I score was investigated first. See Table 2 for regression results.
Table 2.
Regression models for gender, week, ASI, PSS-I, and ASI×PSS-I on percent days drinking
| Outcome | Predictor | R2 | Adj R2 |
R2 Chg. |
B | SE | β |
|---|---|---|---|---|---|---|---|
| Percent Days Drinking | Gender | .20 | .17 | .01 | 1.27 | 5.92 | .02 |
| Week | .15 | −.71 | .21 | −.29** | |||
| PSS-I total score | .03 | .57 | .29 | .19* | |||
| ASI | .01 | .16 | .21 | .07 | |||
| ASI × PSS-I total score | .02 | −.03 | .02 | −.15† | |||
| Gender | .20 | .17 | .01 | .87 | 5.92 | .01 | |
| Week | .15 | −.73 | .21 | −.30* | |||
| PSS-I Re-experiencing | .03 | 1.05 | .58 | .17† | |||
| ASI | .01 | .19 | .20 | .08 | |||
| ASI × PSS-I Re-experiencing | .02 | −.06 | .03 | −.15† | |||
| Gender | .22 | .18 | .01 | 3.09 | 5.95 | .04 | |
| Week | .15 | −.72 | .21 | −.30** | |||
| PSS-I Avoidance | .04 | 2.38 | .96 | .23* | |||
| ASI | .01 | .11 | .20 | .05 | |||
| ASI × PSS-I Avoidance | .03 | −.11 | .05 | −.17* | |||
| Gender | .19 | .15 | .01 | .54 | 5.99 | .01 | |
| Week | .15 | −.79 | .21 | −.32* | |||
| PSS-I Hyperarousal | .03 | 1.26 | .72 | .16† | |||
| ASI | .01 | .18 | .20 | .08 | |||
| ASI × PSS-I Hyperarousal | .01 | −.03 | .04 | −.06 |
Note. ASI = Anxiety Sensitivity Index; PSS-I = Posttraumatic Symptom Scale – Interview;
p < .10,
p < .05,
p < .01
The combination of ASI, PSS-I total score, and their interaction significantly predicted PDD, accounting for 17.2% of variance in drinking, F(5, 126) = 6.40, p < .0001. We then examined the three subscales of the PSS-I in order to understand which clusters of symptoms drove this interaction. The combination of ASI, PSS-I re-experiencing subscale, and their interaction accounted for 17.0% of the total variance in PDD, F(5, 126) = 6.35, p < .0001. The regression result was driven by an interaction between ASI and re-experiencing, which approached significance (p = .07). The model of ASI, PSS-I avoidance subscale, and their interaction significantly predicted 18.4% of variation in PDD, F(5, 126) = 6.91, p < .0001. In particular, the model revealed a significant interaction between ASI and avoidance (p = .04). The overall model of ASI by hyperarousal subscale predicted significant variance in PDD, F(5, 126) = 5.71, p < .0001. However, the variance was accounted for by the main effect of the PSS-I hyperarousal subscale; the interaction with ASI was not significant (p = .51).
In order to determine the direction of the interactions between ASI and the PSS-I subscales of re-experiencing and avoidance, guidelines recommended by Aiken and West (1991, p. 19) were utilized (see also Holmbeck, 2002, for a detailed example). Two conditional moderating variables (low and high ASI) were calculated as the respective ASI value +/− 1 SD: Low ASI (ASI + 15.65) and High ASI (ASI − 15.65). Interaction terms were created to include the new conditional moderating variables (Low/High ASI) by multiplying each variable by PTSD severity scores (PSS-I total score and subscales). Post-hoc regression analyses were conducted to include PTSD (main effects), the conditional moderating variable (Low/High ASI), and their interaction. These analyses yielded regression coefficients, or slopes, that defined the strength of the association between PTSD symptom severity and PDD for high and low ASI scores.
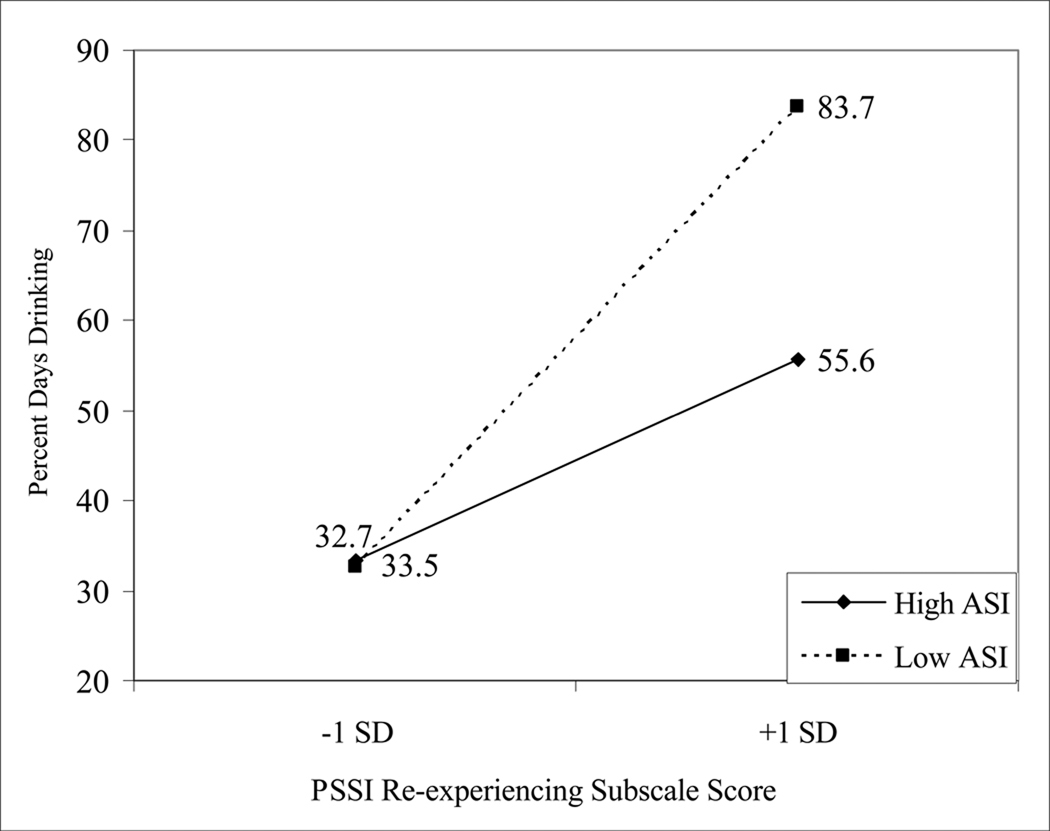
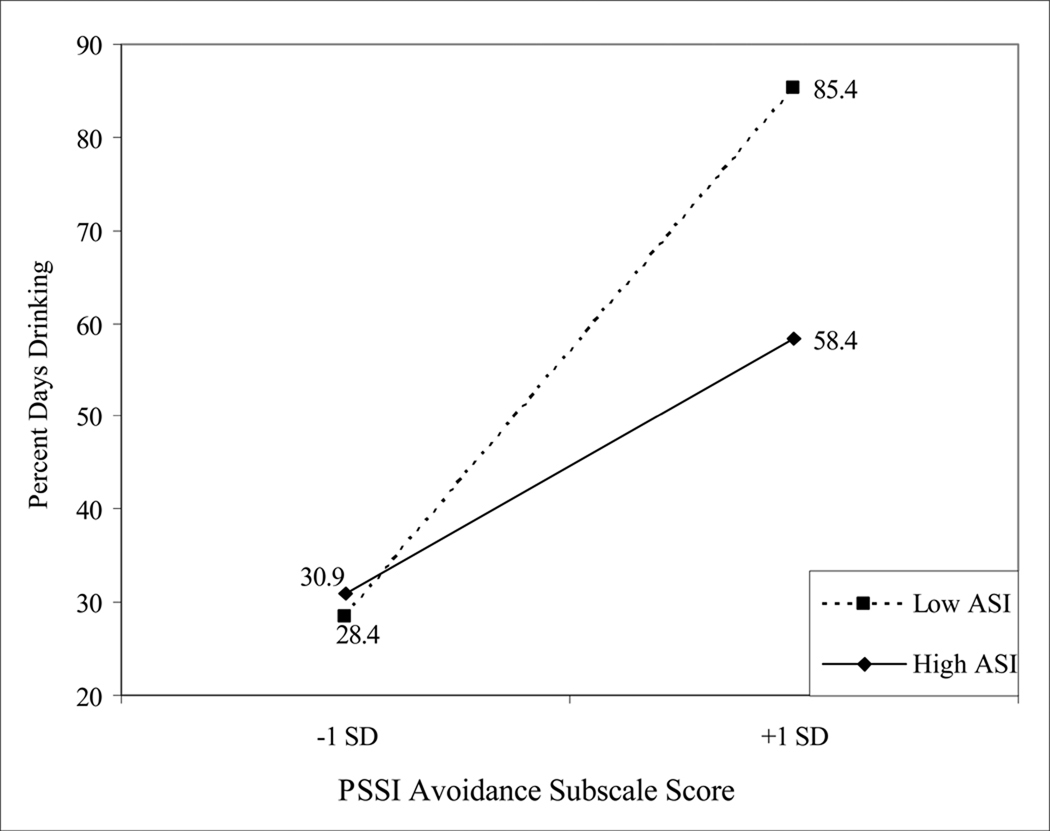
Figure 1 presents a plot of the moderating effect of ASI (low and high) on the association between PSS-I re-experiencing scores and PDD. As can be seen in the figure, individuals with lower ASI scores showed a more positive association between PTSD symptoms and PDD, as indicated by the steeper slope for this group. ASI similarly moderated the effect of PTSD avoidance symptoms on PDD (Figure 2); again, lower scores on ASI were associated with a stronger association between PTSD scores and drinking behavior.
Figure 1.
Interaction of ASI and PSS-I Re-experiencing subscale on PDD.
Figure 2.
Interaction of ASI and PSS-I Avoidance subscale on PDD.
Discussion
In the current study we found a significant interaction between AS and PTSD symptoms on frequency of drinking behavior; however, the direction of the interaction was contrary to our hypothesis. We predicted that AS would moderate the association between severity of PTSD symptoms and drinking behavior such that there would be a more positive association between PTSD symptoms and alcohol consumption among individuals with higher AS; thus the greatest percentage of drinking days was predicted to be among individuals high in AS and with high PTSD symptoms. In contrast to our hypothesis, it was the low AS group whose drinking behavior was more strongly associated with PTSD symptom levels, both for re-experiencing and avoidance symptoms; low levels of PTSD symptoms in this group were associated with relatively fewer days drinking, whereas high levels of PTSD symptoms were associated with more frequent drinking. It should be noted that the reported effects emerged after controlling for week of treatment, which (as would be expected) was strongly associated with drinking behavior.
These results are somewhat surprising in light of existing findings reported in the literature on AS and alcohol use among individuals with anxiety disorders. For example, previous reports with clinical samples found that individuals with high AS report more alcohol use in negative emotion situations than do low AS individuals (e.g., Dehaas et al., 2002; Dehaas et al., 2001). It is possible that methodological differences account for the discrepant findings; for example, both of the studies by Dehaas and colleagues operationalized drinking outcomes as responses to a self-report questionnaire (Inventory of Drug Taking Situations; Annis & Martin, 1985), whereas in the present study degree of drinking was ascertained via patients’ reports about daily drinking behavior based on the Timeline Follow-Back. Nevertheless, the reported results run counter to theoretical expectations, and thus require replication.
Several possible explanations may account for the counterintuitive finding that the highest level of drinking was found among individuals with low AS and high PTSD symptoms. One possibility is that these individuals use alcohol for different reasons than do those with high AS. For example, low AS individuals with high PTSD avoidance symptoms may be “repressors” who deny that high anxiety (PTSD symptoms) is distressing to them (we thank an anonymous reviewer for this interpretation). Thus low AS/high PTSD avoidance individuals may use alcohol in an effort to reduce awareness of their PTSD symptoms. This explanation points to the need for additional research to specify the pathways through which AS moderates the effect of PTSD symptoms on drinking behavior.
Furthermore, it is important to examine drinking motives and other cognitive variables that moderate the association between PTSD symptoms and use of alcohol. Such investigations have been conducted in research on the relationship between social anxiety and alcohol use. For example, Bruch, Rivet, Heimberg, and Levin (1997) found that social anxiety (shyness) was negatively associated with alcohol use; however, shy individuals who expect alcohol to be helpful in social interactions tend to consume more alcohol. Future research can examine, for example, the effects of alcohol expectancies on the association between PTSD symptoms and alcohol use.
Although the overall pattern of results reported here is the opposite of what we predicted, certain findings were in line with our hypotheses. Table 1 reveals that, as expected, high AS is associated with greater drinking behavior on average (collapsing across low and high PTSD symptoms; see also Table 2). The most surprising finding is the sharp increase in drinking behavior associated with greater PTSD symptoms among individuals with low AS. Additional research is necessary to determine whether this finding is reliable, if it extends to other outcomes besides drinking behavior, and what accounts for it. Although this finding was not predicted in the present study, at least one previous study reported similar effects associated with low AS; Zvolensky, Kotov, Antipova, Leen-Feldner, and Schmidt (2005) found that individuals with relatively low AS were more likely to use alcohol under conditions of high stress, whereas for high AS individuals high stress was associated with less drinking.
Interestingly, of the three PTSD symptom clusters (re-experiencing, avoidance/numbing, hyperarousal), AS interacted significantly only with avoidance symptoms and marginally significantly with re-experiencing symptoms to predict drinking behavior; this finding is particularly striking in light of the strong correlations among the symptom clusters (see Table 1). While it is possible that these symptom clusters assess the kinds of experiences that tend to provoke greater consumption of alcohol among low AS individuals, additional work is necessary to determine whether the moderating effect of AS is specific to these particular PTSD symptom clusters.
The present results have potential implications for the treatment of individuals with comorbid alcohol use disorders and PTSD. They point to the importance of assessing patients’ levels of AS in order to identify the extent to which their PTSD symptoms and drinking behavior are likely to be associated. Based on the current results, alcohol dependent individuals with low AS are particularly likely to benefit from a reduction in PTSD symptoms in terms of being able to reduce their drinking behavior, whereas individuals with high AS may continue to have problematic levels of drinking even as their PTSD abates. Additional interventions including exposure to interoceptive cues, such as those used to treat panic disorder (e.g., having patients breathe through a straw to induce sensations of suffocation) may complement the standard treatments for PTSD among individuals high in AS, given their overall greater drinking levels.
Strengths of the present study include the large, demographically diverse sample and the use of a clinician-administered PTSD severity measure that makes it unlikely that the results were driven by participants’ response bias. Additionally, the use of a validated measure of drinks consumed (TLFB) rather than more general self-reports about “typical” drinking behavior may more precisely capture participants’ drinking patterns (see Babor, Stephens, & Marlatt, 1997). The present study has several limitations. First, the cross-sectional design precludes conclusion of the causal relationship among AS, PTSD, and drinking. Thus, while it is plausible that individuals with both low AS and high re-experiencing symptoms feel compelled to drink more often, other relationships among these variables are possible. For instance, individuals who drink more and have low levels of AS may be more likely to try to avoid thinking about the trauma memory, thus perpetuating their PTSD symptoms. Longitudinal studies may allow us to determine the direction of these effects, although existing longitudinal research is consistent with the causal role of AS in subsequent self-medication with alcohol (Schmidt et al., 2007).
Additionally, although the present sample was diverse in terms of participant race and ethnicity, 70% of participants were male, which likely is a function of the epidemiology of alcohol dependence (e.g., Anthony, Warner, & Kessler, 1994); however, the majority of patients with PTSD are female (Breslau, 2009). Thus it may be beneficial to attempt to replicate the current findings in samples that are more gender balanced. However, it is important to note that there were no significant gender effects in the regression models. It also cannot be known from the current results whether these findings extend to other groups that were underrepresented in the present sample, including individuals of Hispanic ethnicity and races other than African Americans and individuals of European descent. Finally, subsequent studies from the present clinical trial (once all outcome data are collected) will address the effects that AS may have on treatment outcome for individuals with comorbid alcohol dependence and PTSD.
Acknowledgements
The authors thank Stanley Guzowski for assistance with data entry and Joseph Giardino for performing a literature search. This work was supported by grants to EBF from the National Institute on Alcohol Abuse and Alcoholism (R01 AA012428) and the National Institute on Drug Abuse (R01 DA023507).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- Annis HM, Martin G. Inventory of Drug-Taking Situations. Toronto, Canada: Addiction Research Foundation; 1985. [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology. 1994;2:244–268. [Google Scholar]
- Asmundson GJ, Norton GR. Anxiety sensitivity in patients with physically unexplained chronic back pain: A preliminary report. Behaviour Research and Therapy. 1995;33:771–777. doi: 10.1016/0005-7967(95)00012-m. [DOI] [PubMed] [Google Scholar]
- Babor TE, Stephens RS, Marlatt GA. Verbal report methods in clinical research on alcoholism: Response bias and its minimization. Journal of Studies on Alcohol. 1987;48:410–424. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- Breslau N. The epidemiology of trauma, PTSD and other posttrauma disorders. Trauma, Violence, and Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- DeHaas RAB, Calamari JE, Bair JP. Anxiety sensitivity and the situational antecedents to drug and alcohol use: An evaluation of anxiety patients with substance use disorders. Cognitive Therapy and Research. 2002;26:335–353. [Google Scholar]
- Bruch MA, Rivet KM, Heimberg RG, Levin MA. Shyness, alcohol expectancies, and drinking behavior: Replication and extension of a suppressor effect. Personality and Individual Differences. 1997;22:193–200. [Google Scholar]
- DeHaas RA, Calamari JE, Bair JP, Martin ED. Anxiety sensitivity and drug or alcohol use in individuals with anxiety and substance use disorders. Addictive Behaviors. 2001;26:787–801. doi: 10.1016/s0306-4603(01)00237-4. [DOI] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and meditational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Lehman CL, Cheung RC. Depression, anxiety, post-traumatic stress, and alcohol-related problems among veterans with chronic hepatitis C. American Journal of Gastroenterology. 2002;97:2640–2646. doi: 10.1111/j.1572-0241.2002.06042.x. [DOI] [PubMed] [Google Scholar]
- MacDonald AB, Baker JM, Stewart SH, Skinner M. Effects of alcohol on the response to hyperventilation of participants high and low in anxiety sensitivity. Alcoholism: Clinical and Experimental Research. 2000;24:1656–1665. [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Reyno SM, Stewart SH, Brown CG, Horvath P, Wiens J. Anxiety sensitivity and situation-specific drinking in women with alcohol problems. Brief Treatment and Crisis Intervention. 2006;6:268–282. [Google Scholar]
- Samoluk SB, Stewart SH. Anxiety sensitivity and situation-specific drinking. Journal of Anxiety Disorders. 1998;12:407–419. doi: 10.1016/s0887-6185(98)00025-5. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Buckner JD, Keough ME. Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behavior Modification. 2007;31:202–219. doi: 10.1177/0145445506297019. [DOI] [PubMed] [Google Scholar]
- Simpson T, Jakupcak M, Luterek JA. Fear and avoidance of internal experience among patients with substance use disorders and PTSD: The centrality of anxiety sensitivity. Journal of Traumatic Stress. 2006;19:481–491. doi: 10.1002/jts.20128. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-III-R (SCID) New York: Biometrics Research Department, New York State Psychiatric Hospital; 1987. [Google Scholar]
- Stewart S. Anxiety sensitivity and alcohol use motives. Journal of Anxiety Disorders. 1995;9:229–240. [Google Scholar]
- Stewart SH, Peterson JB, Pihl RO. Anxiety sensitivity and self-reported alcohol consumption rates in university women. Journal of Anxiety Disorders. 1995;9:283–292. [Google Scholar]
- Stewart SH, Pihl RO. The effects of alcohol administration on psychopsyiological and subjective-emotional responses to aversive stimulation in anxiety sensitive women. Psychology of Addictive Behaviors. 1994;8:29–42. [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. [Google Scholar]
- Zack M, Poulos CX, Aramakis VB, Khamba BK, MacLeod CM. Effects of drink-stress sequence and gender on alcohol stress response dampening in high and low anxiety sensitive drinkers. Alcoholism: Clinical and Experimental Research. 2007;31:411–422. doi: 10.1111/j.1530-0277.2006.00322.x. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Leen-Feldner EW, Schmidt NB. Evaluating anxiety sensitivity, exposure to aversive life conditions, and problematic drinking in Russia: A test using an epidemiological sample. Addictive Behaviors. 2005;30:567–570. doi: 10.1016/j.addbeh.2004.05.025. [DOI] [PubMed] [Google Scholar]