Abstract
Objectives
Hydronephrosis is the most common abnormality found on prenatal ultrasound. The utility of prophylactic antibiotics in the postnatal management of this condition is controversial. No study has assessed practice patterns of general pediatricians in the management of prenatally-detected hydronephrosis.
Methods
An 18 question survey was sent to a random cross-sectional national sample of pediatricians from the American Medical Association Masterfile. Participants answered questions regarding practice location and type, practice experience, frequency of cases seen, familiarity with the literature, use of antibiotics, work-up of hydronephrosis, and specialist referral. Multivariate logistic regression identified factors associated with prescribing antibiotics.
Results
244 of 461 (53%) subjects responded. 56% routinely prescribe antibiotics for prenatally-detected hydronephrosis. 57% perform postnatal work-up themselves. Of these, 98% routinely order ultrasounds while ~40% routinely order voiding cystourethrograms. 94% have specialists readily available, but only 41% always refer to a specialist. On multivariate logistic regression, those who believe prophylactic antibiotics to be beneficial are significantly more likely to prescribe antibiotics compared with those who have not read the literature (OR 6.1, 95%CI 2–15). Those without specialist consultation readily available have an increased odds of starting prophylactic antibiotics compared with those who have consultation available (OR 7.2, 95%CI 1.3–39).
Conclusion
Most pediatricians initiate postnatal management of prenatally-detected hydronephrosis, therefore pediatricians truly are gatekeepers to children with this condition. Knowledge of practice patterns is crucial for the dissemination of evidence-based information to the appropriate providers and enables us to learn more about the utility of antibiotic prophylaxis in future studies.
Keywords: kidney disease, antibiotic prophylaxis, practice variation, survey, prenatal diagnosis
Introduction
Prenatal hydronephrosis is the most common abnormality found on prenatal screening ultrasounds, occurring in ~1% of those screened1. Hydronephrosis can be caused by a number of urologic conditions. Prior to the widespread use of prenatal ultrasound, hydronephrosis was only detected after presentation with symptoms such as pain or infection. Because symptoms were present, surgical treatment was the norm after diagnosis of underlying etiology. In contrast, most cases of prenatally-detected hydronephrosis are asymptomatic and of variable clinical consequence. Most patients will resolve spontaneously, though some patients do require surgery and some even progress to renal failure2. As we do not yet know how to predict the ultimate outcome of an individual patient, the management for prenatal hydronephrosis usually involves serial radiographic imaging and possible antibiotic prophylaxis3.
The role of prophylactic antibiotics is controversial as observational studies have found antibiotics both beneficial and harmful1,4,5. While some research regarding pediatric urologist practice patterns has been done6, no study has looked at the practice pattern of general pediatricians regarding antibiotic use and management of prenatal hydronephrosis. This target population is of interest because pediatricians are the gatekeepers to children with prenatal hydronephrosis.
Materials and Methods
Study Sample
Following approval from the University of California San Francisco (UCSF) internal review board, we randomly selected a cross-sectional sample (n=3,151) from a pool of 24,657 pediatricians throughout the United States drawn from the American Medical Association Masterfile, a comprehensive list of licensed allopathic and osteopathic doctors7. The list was generated and emails were sent through Medical Marketing Services, Inc (Carol Stream, Il). Random selection was restricted to subjects self-designated as “office based”, “medical teaching”, or “hospital staff”. Those who self-designated “administration”, “research”, subspecialty, or resident were excluded. Non-responders to the initial email received a second reminder email two weeks later. Participants were offered a $5.00 gift card from Starbucks® for completion. This incentive was chosen based on evidence supporting small guaranteed dollar amounts versus larger lottery-based amounts in optimizing response rates8.
Survey Instrument
The survey was developed by the authors and pilot-tested with ten members of Department of Pediatrics at UCSF with the specific goal of eliciting feedback on survey design. Two separate clinical research panels, including members experienced in survey administration and pediatric urologists, then reviewed it for further modification. The 18 question survey required fewer than 5 minutes to complete. Participants provided their state, type of practice, years in practice, number of new cases of prenatal hydronephrosis seen per year, and familiarity with the literature on this topic (source of the literature, such as journal reading or conference attendance was left to the interpretation of the respondent). Regarding specialist use, participants provided accessibility of specialists to their patients, factors influencing decisions to refer to a specialist, and preferred role of the specialist. Participants also provided answers to management steps in the postnatal period regarding antibiotics use, postnatal work-up, management of confirmed postnatal hydronephrosis, and factors influencing antibiotic use. The survey was administered electronically in March 2010 and answers were collected through a commercial internet company, Questionpro (Seattle, Washington).
Statistical Analysis
Responses are reported as proportions of total respondents with means and medians as appropriate. Demographics of respondents, non-respondents, non-contacts, and total population were compared using chi squared and ANOVA. The primary outcome was the proportion of subjects prescribing prophylactic antibiotics. Multivariate logistic regression for the primary outcome was performed with the following a priori predictor variables: years in practice, geographic region, practice type, number of yearly cases, self-perceived knowledge of literature in this subject, and availability of specialist consultation. All of these predictors were kept in the multivariate model for face validity, even if non-significant on univariate analysis. Categorical predictor variables were collapsed to binary variables after verifying that there was no statistical difference between the categories and their association with the outcome. States were categorized into four regions according to the United States Census Bureau9. Thirteen states had no responders to the survey. These were all rural states below the United States population density average. A sensitivity analysis was performed by refitting the regression model including only those states with population densities below average or not a part of the continental United States. A 0.05 two-sided level of significance was set for all measures of association. All analyses were performed using Stata 11.0 (College Station, TX).
Results
3151 invitations were sent via email. Of these, 176 emails were undeliverable (bounced). 2514 did not open the email therefore delivery could not be confirmed. As they did not view the invitation to participate nor the survey content, these subjects were excluded from analysis. These bounced and delivery unconfirmed groups will henceforth be referred to as “non-contact.” 461 (14.6%) were confirmed to have received the email. Of these who opened the email, 244 responded by completing the survey and 217 did not complete the survey (53% response rate). Overall, 8.2% (244/2975) of the total emails sent completed the survey. Using a 95% confidence interval, this response rate results in a 6% margin of error in estimating the practices of the more than 24,000 practicing pediatricians in the United States. Gender, practice location, and practice type did not differ between the respondents, non-respondents, non-contacts, and total population. Age did differ between these populations (p=.005) (Table 1).
Table 1.
Demographics of Survey Recipients from AMA Masterfile Data.
| Respondents | Non- Respondents |
Non- Contacts |
Total Population |
|
|---|---|---|---|---|
| No. subjects | 254a | 207a | 2690 | 3151 |
| Median age (IQR)b | 45(38–53) | 48(40–58) | 48(40–57) | 48(40–57) |
| % Male | 40 | 46 | 43 | 43 |
| Geographic region, n(%) | ||||
| Northeast | 68(27) | 49(24) | 644(24) | 761(24) |
| Midwest | 43(17) | 35(17) | 501(19) | 579(18) |
| South | 73(29) | 65(31) | 943(35) | 1081(34) |
| West | 70(28) | 58(28) | 602(22) | 730(23) |
| Practice type, n(%) | ||||
| Office based | 221(87) | 181(88) | 2319(86) | 2721(86) |
| Hospital staff | 32(13) | 23(11) | 307(11) | 362(12) |
| Medial teaching | 1(.4) | 2(1) | 64(2) | 67(2) |
10 subjects in this table listed as “respondents” are mis-classified and treated as “non-respondents” in the remainder of the paper. This misclassification is due to 10 subjects clicking the link to open the survey, but not starting the survey. Respondent n=244 and non-respondent n=217 have been used for response rate calculation and for all other calculations presented in this study.
Median age was significantly different between the groups (p=.005). The groups were similar with respect to sex, geographic region, and practice type.
Demographic categories in Table 1 are determined according to pre-set AMA Masterfile categories derived from MMS electronic data tracking. This tracking assesses the number of email invitations opened and the number of survey links clicked. Clicked links are considered responses by the data tracking system. This tracking resulted in 254 respondents clicking the survey link; however the true response rate via actual completed survey results was 244. MMS detected 10 survey links opened that did not result in survey completion. A sensitivity analysis was performed comparing self-reported geographic location with MMS derived geographic location. These results did not differ (p=.83), therefore we do not believe the misclassification of the 10 subjects was substantive. N=244 was used in all further calculations of response rate and responses to the survey.
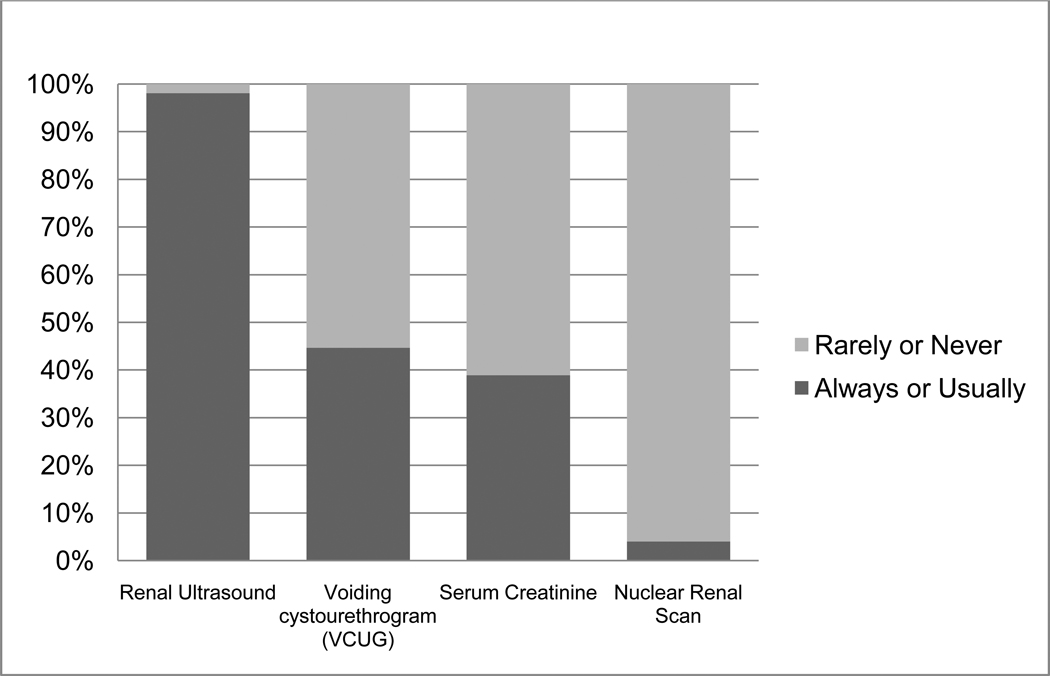
Responses to factors influencing the use of prophylactic antibiotics and specialty referral are listed in Table 2. Almost half of pediatricians refer to a specialist as a part of the initial management of prenatally detected hydronephrosis. 86% of pediatricians always or sometimes initiate work-up of prenatally-detected hydronephrosis through their own office. Those who do initiate work-up almost always order a renal ultrasound (98%). Voiding cystourethrogram (VCUG) and serum creatinine are less frequently obtained (Figure 1).
Table 2.
Practice patterns and factors influencing use of prophylactic antibiotics and referral to specialists. Question and answer wording replicate the administered survey.
| How frequently do you treat new cases of prenatal hydronephrosis? | No. of subjects(%)a |
|---|---|
| Monthly (>12 per year) | 24(10.1) |
| Every other month (6–11 per year) | 34(14.4) |
| Once in a while (2–5 per year) | 128(54.0) |
| Less than once a year | 51(21.5) |
| Do you initiate work-up or management of prenatal hydronephrosis by ordering tests through your office after the baby is born? | |
| Yes | 136(56.7) |
| Depends | 69(28.8) |
| No, I prefer the specialists to order their own studies | 32(13.2) |
| No, I neither order my own studies nor refer to a specialist | 3(1.24) |
| When an infant known to have PRENATAL hydronephrosis is born, what is/are your initial management step(s)? (check all that apply) | |
| Order investigational studies | 177(73.4) |
| Refer to urologist | 75(31.1) |
| Start antibiotics | 38(15.8) |
| Refer to nephrologist | 28(11.6) |
| Other | 27(11.2) |
| Do nothing if the child is otherwise doing well | 15(6.2) |
| In infants confirmed to have persistent hydronephrosis on postnatal ultrasound and has not yet seen a specialist, do you prescribe prophylactic antibiotics? | |
| Always | 70(29.3) |
| Usually | 65(27.2) |
| Rarely | 58(24.3) |
| Never | 46(19.3) |
| In those who answered “never”: | |
| Reasons FOR NOT prescribing prophylactic antibiotics. (check all that apply) | |
| I prefer a specialist to make that decision | 26(56.5) |
| I do not think it is indicated based on studies | 20(43.5) |
| I was not aware that antibiotics are indicated or a topic of debate | 14(30.4) |
| I am worried about the development of antibiotic resistance | 12(26.1) |
| Other | 7(15.2) |
| In those who answered “Always”, “Usually”, “Rarely”: | |
| Reasons FOR prescribing prophylactic antibiotics. (check all that apply) | |
| Prevent urinary tract infection | 141(73.1) |
| Awaiting more extensive work-up or specialist consultation | 109(56.5) |
| This is the way I was trained | 57(29.5) |
| Standard of care in my community | 49(25.4) |
| Young infants are more likely to have infections | 28(14.5) |
| Medico-legal protection | 23(11.9) |
| Other | 17(8.8) |
| Reassures parents | 7(3.6) |
| In those who answered “Usually”, “Rarely” or “Never”: | |
| Which of the following clinical situations might cause you to prescribe prophylactic antibiotics? (check all that apply) | |
| Specialist recommends it | 133(78.7) |
| History of UTI | 116(68.6) |
| Severe hydronephrosis | 97(57.4) |
| Solitary kidney with hydronephrosis | 68(40.2) |
| Bilateral hydronephrosis | 44(26.0) |
| Elevated baseline creatinine | 27(16.0) |
| Uncircumcised boy | 16(9.5) |
| Vesicoureteral reflux | 9 (7.8) |
| Other | 2(1.2) |
| Which of the following would influence your decision to refer to a specialist? (check all that apply) | |
| Severe hydronephrosis | 162(69.5) |
| Solitary kidney | 147(63.1) |
| Vesicoureteral reflux diagnosis | 134(57.5) |
| Elevated creatinine | 132(56.7) |
| I always refer to a specialist | 96(41.2) |
| Other | 18(7.7) |
Total n may sum to greater than 244 as questions instructing “check all that apply” permitted more than one response. Total n in all other questions may not sum to 244 as all subjects did not answer all questions.
Figure 1.
Frequency of investigational studies obtained by general pediatricians performing postnatal work-up of prenatally-detected hydronephrosis.
The use of prophylactic antibiotics is almost evenly split. If an infant is confirmed to have postnatal hydronephrosis on ultrasound, 56% of respondents always or usually prescribe antibiotics while 44% rarely or never do. Of those who do not prescribe antibiotics, the most common reasons cited are preferring a specialist to make this decision (57%), and not believing antibiotics are indicated (44%). Of those who do prescribe antibiotics, the most common reasoning is preventing UTI (73%). Those who would not ordinarily prescribe antibiotics would be swayed to do so by specialist recommendation (79%) or a history of UTI (69%). Interestingly, factors such as vesicoureteral reflux (VUR), renal insufficiency, and circumcision status have little influence on this decision (Table 2).
Forty-one percent of pediatricians always refer to a specialist for confirmed postnatal hydronephrosis, though complicated disease states such as severe hydronephrosis or a solitary kidney do have some influence (Table 2). Once a patient has been referred, 78% of pediatricians would prefer the specialist to perform future management rather than performing the follow-up themselves. The vast majority of pediatricians have specialist consultation readily available to their patients (94%).
On multivariate logistic regression, beliefs from reading literature and the availability of specialists are associated with the use of prophylactic antibiotics (Table 3). Those who believe antibiotics are beneficial or inconclusive have a 3–6 fold greater odds of prescribing antibiotics compared with those who have not read the literature(p<.001). Those who do not have specialist consultation readily available to their population have 7 fold higher odds of prescribing antibiotics compared with those who do have specialists readily available (p=.02). Geographic region, practice type, frequency the condition is seen, and years in practice are not associated with the use of prophylactic antibiotics.
Table 3.
Univariate and multivariate analysis of characteristics associated with the prescription of prophylactic antibiotics for prenatally-detected hydronephrosis.
| N(%)a | Univariate OR (95% CI) |
Multivariate OR (95% CI) |
P Valueb |
|
|---|---|---|---|---|
| Years in practice | ||||
| 0–15 | 126(52.5) | Referentc | Referent | |
| >15 | 114(47.5) | 1.17 (0.7–2.0) | 1.37 (0.8–2.5) | 0.3 |
| No. of cases encountered per year | ||||
| 0–5 | 179(75.5) | Referent | Referent | |
| ≥6 | 58(24.5) | 1.50 (0.8–2.8) | 1.29 (0.6–2.6) | 0.7 |
| Geographic region | ||||
| Northeast | 59(25.7) | Referent | Referent | |
| Midwest | 36(15.1) | 1.31 (0.6–3.1) | 1.67 (0.6–4.4) | 0.3 |
| South | 72(30.1) | 0.87 (0.4–1.8) | 1.06 (0.5–2.3) | 0.9 |
| West | 72(30.1) | 0.54 (0.3–1.1) | 0.54 (0.2–1.2) | 0.1 |
| Practice type | ||||
| Non-academicd | 219(90.1) | Referent | Referent | |
| Academic | 22(9.1) | 2.23 (0.8–5.9) | 1.78 (0.6–5.5) | 0.3 |
| Belief from literature of antibiotic effect | ||||
| Not up-to-date | 92(40.0) | Referent | Referent | |
| Equal benefit and harm | 86(37.4) | 3.04 (1.6–5.6) | 3.33 (1.7–6.6) | 0.001 |
| Beneficial | 40(17.4) | 6.51 (2.7–15.7) | 6.06 (2.4–15.4) | <.0005 |
| Harmful | 12(5.2) | 1.63 (0.5–5.4) | 3.23 (0.8–12.4) | 0.09 |
| Specialist consultation readily available | ||||
| Yes | 215(94.9) | Referent | Referent | |
| No | 14(6.1) | 5.03 (1.1–23.0) | 7.24 (1.3–38.9) | 0.02 |
Total n may not always sum to 244 as all respondents did not answer all questions
P values refer to the multivariate analysis results. All p values <.05 on multivariate analysis were also found to be <.05 on univariate analysis
”Referent” indicates reference group to which other groups are compared in calculating odds ratios
Non-academic includes private practice, community clinic, hospital-based, managed care, and other
This survey lacked respondents from thirteen states, all with low population densities (Alaska, Arizona, Idaho, Iowa, Minnesota, Montana, New Hampshire, North Dakota, Rhode Island, South Dakota, Vermont, West Virginia, Wyoming). A sensitivity analysis refitting the multivariate logistic regression to include only low population or geographically distant states (Colorado, Maine, Mississippi, Nebraska, Nevada, New Mexico, Oregon, Utah, Wisconsin, Hawaii) resulted in similar point estimates for the significant predictors compared with the original model including all states.
Comment
The use of prophylactic antibiotics for prenatal hydronephrosis shares similar theoretical risks and benefits with other urologic conditions, such as VUR. Advocates of antibiotics operate under the assumption that antibiotics prevent renal damage and scarring from recurrent pyelonephritis. Detractors are concerned for the development of antibiotic resistance, unnecessary health care costs, and the exposure of a large number of children to the unlikely, but serious risks of antibiotics, such as Stevens-Johnson syndrome.
We document for the first time general pediatricians’ practice patterns in the management of prenatal hydronephrosis. Pediatricians are divided on the use of prophylactic antibiotics in prenatally detected hydronephrosis with 56% routinely using and 44% not routinely using antibiotics. These findings show there is no predominant consensus; therefore future studies are paramount in order to guide therapy.
This survey shows the literature to be an important influence on pediatricians who incorporate this knowledge into practice. Those who believe that antibiotics are beneficial have a 6 fold greater odds of prescribing antibiotics compared with those who have not read the literature. One might wonder why those who find the literature ambiguous are still more likely to prescribe antibiotics. This finding highlights the multi-factorial nature of medical decision making. These physicians may prefer to err on the side of caution, especially as no definitive evidence yet exists to justify or refute the use antibiotics. Alternatively, they may prescribe them due to other factors such as community standards and medico-legal protection. We show that a variety of issues contribute to such decisions.
More than half of pediatricians always order investigational studies through their office. It is clear that those who choose to do so are appropriate and efficient with their management algorithm. 98% routinely order ultrasounds, which are relatively inexpensive and non-invasive. In contrast, 40% of subjects routinely order VCUGs, which is considered a more invasive test. Finally, only 4% order renal nuclear scans, invasive, expensive tests with very specific indications. This step-wise progression of radiographic imaging is generally consistent with management of prenatal hydronephrosis from the urologic viewpoint where all patients are screened with a renal ultrasound, some patients undergo a VCUG for concerning hydroureteronephrosis or abnormal bladder changes, and few patients undergo a renal scan to assess for obstruction, renal scarring, or differential renal function3.
Only 41% of pediatricians routinely refer to a specialist despite availability of specialists to virtually all communities, which suggests that pediatricians are comfortable initiating the workup and management of less severe cases of hydronephrosis. Once they do refer, 78% of pediatricians prefer the specialist to perform future management. This highlights a positive working relationship between specialties in a condition that can require both operative and non-operative management.
Despite the high incidence of prenatal hydronephrosis, studies on antibiotic use in this population are still nascent compared with other pediatric urinary conditions, such as VUR. No randomized trial exists regarding the use of antibiotics in children with prenatal hydronephrosis. Of the existing retrospective studies, Lee, et al10 found a 19% incidence of infection in one year. In contrast, Roth, et al4, performed a similar study with a 4.3% incidence of UTI over 27 months.
Extrapolation of data from randomized studies in other UTI-related fields11–13 is difficult as these studies find both benefit and no benefit. These studies are also limited by small sample sizes, a lack of placebo, and other methodological limitations. These limitations underscore the need for pediatricians, nephrologists, and urologists to begin collaborative planning of adequately powered and appropriately focused studies on prenatal hydronephrosis.
We believe the data from this study will help direct future clinical trials. We show that current antibiotic use has no predominant practice. This variability suggests that future studies would be more feasible compared to a situation where, for example, 95% of physicians already prescribe antibiotics and may be more reluctant to change current practice. Another major obstacle to trial recruitment is physician “buy-in” or acceptance of the importance of the study question and equipoise of the trial arms. If study protocols require physicians to radically deviate from their management style, physicians may be reluctant to enroll their patients. This study elucidates factors influencing physician management which will enable future trials to avoid pitfalls by effectively tailoring their study protocols. Characterizing the distribution of patients seen by pediatricians versus specialists will also aid organization of future recruitment sites.
Our study is limited by the 53% response rate. This potentially creates a selection and response bias; however studies have shown that reliance on response rate as the sole indicator of validity is not the correct approach to survey data14,15. Instead, the focus should be placed on whether response bias exists. Age and gender are examples of parameters proven to be associated with response bias15. We show that the respondents, non-respondents, non-contacts, and the overall population of this study have similar genders, geographic locations, and practice types, so we believe this is not the case. The only parameter in which the respondents differ from the other populations was in age (median age 45 vs. 48), however we believe that this is statistically significant due to the large “n” of the study, but not clinically significant. Furthermore, we have used the same mailing source and obtained a similar response rate to other recently published surveys7,16,17. The strength in this mailing source lies in the fact that it is a nationally representative sample. A local sample (such as polling doctors within one hospital) might result in a higher response rate but would lower generalizability as compared to a national sample.
Another source of bias is a lack of response from the thirteen states mentioned in the results section. All of these states are below average in United States population density and therefore could be classified as rural. As a sensitivity analysis, we re-fitted our multivariate logistic regression using 9 states also under the population density average for which we had responses. Hawaii was included to approximate the geographic isolation experienced by Alaska. This refitted model resulted in similar point estimates for significant predictors as the full model including all states; therefore we do not believe these thirteen rural states are a likely source of bias.
Conclusion
We report the current state of practice regarding prenatal hydronephrosis for general pediatricians across the United States, the first-line physicians in this condition. Pediatricians vary considerably in their use of prophylactic antibiotics, their indications to do so, and their incorporation of specialty care. The results of this study will optimize future study design by providing the insight required to maximize feasibility and subject recruitment.
Acknowledgments
Funding Source: NIH UCSF KURe Career Development Program
Abbreviations
- VCUG
voiding cystourethrogram
- UTI
urinary tract infection
- VUR
vesicoureteral reflux
- CI
confidence interval
- OR
odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Internal Review Board Approval: yes
Disclosures: none
References
- 1.Lee R, Cendren M, Kinnamon D, Nguyen H. Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics. 2006;118:586–593. doi: 10.1542/peds.2006-0120. [DOI] [PubMed] [Google Scholar]
- 2.Cordero L, Nankervis C, Oshaughnessy R, Koff S, Giannone P. Postnatal follow-up of antenatal hydronephrosis: a health-care challenge. Journal of Perinatology. 2009;29:382–387. doi: 10.1038/jp.2008.239. [DOI] [PubMed] [Google Scholar]
- 3.Yiee J, Wilcox D. Management of fetal hydronephrosis. Pediatric Nephrology. 2008;23:347–353. doi: 10.1007/s00467-007-0542-y. [DOI] [PubMed] [Google Scholar]
- 4.Roth C, Hubanks J, Bright B, Heinlen J, Donovan B, Kropp B, Frimberger D. Occurrence of urinary tract infection in children with significant upper urinary tract obstruction. Urology. 2009;73:74–78. doi: 10.1016/j.urology.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Conway P, Cnaan A, Zaoutis T, Henry B, Grundmeier R, Karen R. Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. Journal of the American Medical Association. 2007;298:179–186. doi: 10.1001/jama.298.2.179. [DOI] [PubMed] [Google Scholar]
- 6.Merguerian PA, Herz D, McQuiston L, Bibber MV. Variation Among Pediatric Urologists and Across 2 Continents in Antibiotic Prophylaxis and Evaluation for Prenatally Detected Hydronephrosis: A Survey of American and European Pediatric Urologists. Journal of Urology. 2010;184:1710–1715. doi: 10.1016/j.juro.2010.03.115. [DOI] [PubMed] [Google Scholar]
- 7.Golnik A, Ireland M, Borowsky I. Medical homes for children with autism: a physician survey. Pediatrics. 2009;123:966–971. doi: 10.1542/peds.2008-1321. [DOI] [PubMed] [Google Scholar]
- 8.Ulrich C, Danis M, Koziol D, Garrett-Mayer E, R RH, Grady C. Does it pay to pay? A randomized trial of prepaid financial incentives and lottery incentives in surveys of non-physician health care professionals. Nursing Research. 2005;54:2–6. doi: 10.1097/00006199-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Census Regions and Divisions of the United States. Census Regions and Divisions of the United States [Google Scholar]
- 10.Lee J, Choi H, Kim J, Won H, Kim K, Moon D, Cho K, Park Y. Nonrefluxing neonatal hydronephrosis. Journal of Urology. 2008;179:1524–1528. doi: 10.1016/j.juro.2007.11.090. [DOI] [PubMed] [Google Scholar]
- 11.Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, McTaggart SJ, Hodson EM, Carapetis JR, Cranswick NE, Smith G, et al. Antibiotic Prophylaxis and Recurrent Urinary Tract Infection in Children. New England Journal of Medicine. 2009;361:748–759. doi: 10.1056/NEJMoa0902295. [DOI] [PubMed] [Google Scholar]
- 12.Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, Ceccin D, Pavanello L, Molinari P, Maschio F, et al. Prophylaxis after first febrile urinary tract infection in children? a multicenter, randomized, controlled, noninferiority trial. Pediatrics. 2008;122:1064–1071. doi: 10.1542/peds.2007-3770. [DOI] [PubMed] [Google Scholar]
- 13.Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, Minisini S, Ventura A. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? a randomized, controlled trial. Pediatrics. 2008;121:e1489–e1494. doi: 10.1542/peds.2007-2652. [DOI] [PubMed] [Google Scholar]
- 14.Asch D, Jedrziewski M, Christakis N. Response rates to mail surveys published in medical journals. Journal of Clinical Epidemiology. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 15.Cull W, O'Connor K, Sharp S, Tang S. Response rates and response bias for 50 surveys of pediatricians. Health Services Research. 2005;40:213–226. doi: 10.1111/j.1475-6773.2005.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sneed R, May W, Stenccel C. Policy versus practice: comparison of prescribing therapy and durable medical equipment in medical and educational settings. Pediatrics. 2004;116:e612–e625. doi: 10.1542/peds.2004-1063. [DOI] [PubMed] [Google Scholar]
- 17.Groom H, Bhatt A, Washington M, Santoli J. Temporary vaccine recommendations and provider compliance: a survey of pediatric practices during the 2003 2004 pneumococcal conjugate vaccine shortage. Pediatrics. 2008;122:e835–e840. doi: 10.1542/peds.2008-1092. [DOI] [PubMed] [Google Scholar]