Abstract
Epilepsy has a significant impact on health-related quality of life (HRQOL) of patients and personal coping style is an important determinant. Less is known about home caregivers. This study investigates HRQOL and coping style of both patients and caregivers and their interaction. Epilepsy patients attending the outpatient clinic of the University Medical Centre in Utrecht and their caregivers were sent EQ5D and RAND-36 questionnaires. The Utrecht Coping List was used to chart personal coping styles. HRQOL scores of patients and caregivers were compared to the general Dutch population. The association between patient and caregiver HRQOL scores was calculated. A stepwise backward multivariate linear regression analysis was used to explain variances in caregiver HRQOL. Eighty-six couples (49%) returned all questionnaires. Caregiver HRQOL scores were comparable to the general Dutch population (EQ5D: 0.88–0.88; p = 0.90, RAND-36 MCS: −2 points; p = 0.16), while patients HRQOL scores were lower (EQ5D: 0.79; p < 0.01, RAND-36 MCS −10 points; p < 0.01). However, on several specific domains, associations between patient and caregiver HRQOL scores within couples were found. Passive coping style explained 50% of variation in HRQOL scores of caregivers. As a group, caregivers of epilepsy patients have normal HRQOL, but there are significant associations between patient and caregiver HRQOL scores. Improving caregiver HRQOL through interventions on coping style might benefit patients as well. Recognizing personal coping styles of both patient and caregiver should be part of a patient-oriented approach in treatment.
Keywords: Health-related quality of life, Coping, Caregivers, Epilepsy
Introduction
Epilepsy is one of the most common neurological conditions affecting about six per 1000 people in European countries [1]. Seizures tend to arise suddenly, giving the disease its highly unpredictable character and high psychological impact. Seizures occurring in a public place can lead to embarrassing and sometimes dangerous situations. At work or in a social context, people with epilepsy may also experience lack of understanding and stigma. Epilepsy is known to have a significant impact on quality of life of patients [2–4], but also of people close to and caring for someone with epilepsy [5]. For clinical studies of chronic diseases, including epilepsy, health-related quality of life (HRQOL) is an important outcome parameter. The emphasis usually lies on patients, with less attention given to caregivers. In a previous study exploring HRQOL in caregivers we found a trend of caregivers of patients with therapy resistant epilepsy to have decreased mental component scores of HRQOL. We also found that caregiver HRQOL was not related to objective disease and patient characteristics but seemed related to self-perceived burden of care [6].
Self-reported burden of care probably reflects that person’s natural reaction to the situation he or she is confronted with. This reaction can be described as a coping style. Coping is an individual response to stress in general and will therefore influence mental health in adverse life events [7]. In patients, there is an association between having a passive coping style and lower quality of life [8]. In this study we investigate the relation of coping style to mental domains of HRQOL in caregivers of epilepsy patients and its impact on HRQOL of patients.
Methods
Subjects
We contacted over the phone all epilepsy patients who attended the outpatient clinic of the department of neurology at the University Medical Centre in Utrecht (UMCU), The Netherlands between January 2007 and September 2009. After consent, they were sent questionnaires. The UMCU is a secondary and tertiary referral centre for epilepsy, with epilepsy surgery facilities and a teaching hospital. Inclusion required a diagnosis of partial epilepsy, age between 16 and 80 years, an IQ higher than 80, a normal neurological examination and the ability to complete a Dutch questionnaire. Exclusion criteria were presence of a neurological deficit, e.g. due to stroke or malignancy in the patient. The local medical ethics committee approved this study.
Questionnaires
Two questionnaires were sent to the patients. One was completed by the patient and one by their main caregiver. Patients were asked to give the caregiver questionnaire to the person on whom they at times need to rely because of their epilepsy. If there was no such person, patients were asked to state this as well.
Data on age, gender, marital status, employment, seizure frequency, seizure type and side effects of treatment were obtained from the patient. From the caregiver, data were obtained on gender, relationship to the patient, whether he or she lives with the patient, number of hours per week given to patient care and if he or she received professional help in patient care. The HRQOL questionnaires of patients and caregivers consisted of two generic, validated questionnaires: the RAND-36 [9] and the EQ5D [10]. The RAND-36 consists of 36 questions providing HRQOL scores on the eight domains mental health, social functioning, vitality, role emotional, bodily pain, general health, physical functioning and role physical (minimum 0, optimum 100). These domains are expressed in two summary scores (range 0–100), reflecting the mental (MCS) and physical component scores of HRQOL. The EQ5D consists of two items: five questions giving a utility score (minimum 0, optimum 1) and a VAS score to express QOL on a range of 0–100%.
Coping style was measured using the Utrecht Coping List (UCL) [11], providing coping style profiles. This is a validated questionnaire that measures coping style for problems and unpleasant events in daily life. Subscores describe an individual tendency to seven coping strategies: passive reaction pattern, active confronting, palliative reaction, seeking social support, avoidance, expressing emotions and reassuring thoughts. The UCL is based on the premise that coping strategies are not exclusive and may be present in various combinations [11].
Analysis
Statistical analyses were performed using SPSSv15.0 (SPSS Inc., Chicago, USA). A retrospective powercalculation was done to assess the number of participants needed to reach power of 0.80 to find a statistically significant difference in mental component score of 4 or more, which is considered a minimal important difference in epilepsy patients [12]. A minimum of 35 participants would be needed for this power level.
Summary scores on the eight RAND-36 domains, the MCS (mental component score) and physical component score, were calculated [13]. The scores of both patients and caregivers were compared to the general Dutch population scores using a two-tailed independent sample t test [9]. EQ5D utility scores were calculated (British MVH A1 guidelines). Patient and caregiver scores were compared to scores from the Dutch population using a two-tailed independent sample t test [10]. Scores on the various coping styles were calculated and compared to the general Dutch population [11]. All population scores were matched according to age and sex.
The association of scores on RAND-36 domains, MCS, physical component score and coping style of patients to those of their caregivers was investigated using Pearson’s correlation co-efficient.
The Pearson correlation coefficient was used to investigate the association between coping styles of caregivers and their RAND-36 MCS and physical component scores. The coping style having the strongest association with MCS was studied in a multivariate regression analysis.
First, the association between MCS/PCS and caregiver characteristics (age, gender, relationship to patient, co-habiting, hours of care given to patient and receiving professional help in patient care) and epilepsy characteristics of the patient [duration of epilepsy, seizure frequency, number of anti-epileptic drugs (AED) and experiencing adverse side-effects], was studied by univariate regression analysis, selecting characteristics associated with a p value less than 0.20. To study independent effects of coping style and caregiver and epilepsy characteristics on HRQOL, all selected parameters, including the coping style with the strongest association to MCS were entered in a stepwise backwards multivariate linear regression analysis, with caregivers’ MCS/PCS as the dependent variable.
Results
Out of 177 couples of patients and caregivers, 105 patients returned their questionnaires (59%), 86 couples (49%) returned all questionnaires. There were no significant differences in age or sex between responders and non-responders. Demographic and epilepsy characteristics of patients and caregivers are presented in Table 1.
Table 1.
Clinical and demographic characteristics of patients and caregivers
| Caregivers | Patients | |
|---|---|---|
| (N = 86) | (N = 86) | |
| Epilepsy characteristics | ||
| Mean duration of epilepsy in years | 13 (range: 1–62) | |
| Seizure frequency last 2 years | ||
| Median (per month) | 0 (range: 0–250) | |
| Seizure free (%) | 20 | |
| <1/month (%) | 35.4 | |
| 1 or more/month (%) | 44.6 | |
| of which daily (%) | 15 | |
| Using >1 anti-epileptic drug (%) | 36 | |
| Experiencing adverse side-effects of AED (%) | 59.3 | |
| Demographic characteristics | ||
| Mean age in years | 52 (range: 21–78) | 43 (range: 17–78) |
| Female (%) | 54 | 58 |
| Paid employment (%) | 45 | |
| Relationship to patient | ||
| Partner (%) | 65 | |
| Parent (%) | 33 | |
| Other (%) | 2 | |
| Cohabiting (%) | 87 | |
| Hours of care given per week (median) | 1 (range: 0–168) | |
Quality of life
Average EQ5D utility score of caregivers was 0.88 (SD 0.17), which is comparable to the Dutch population (0.88, SD 0.19, p = 0.90), and of patients 0.79 (SD 0.25), 0.09 points lower than the average Dutch population (p < 0.01) (10).
The average EQ5D VAS score of HRQOL was 81% in caregivers and 72% in patients. Dutch population averages of the VAS score were not available for comparison.
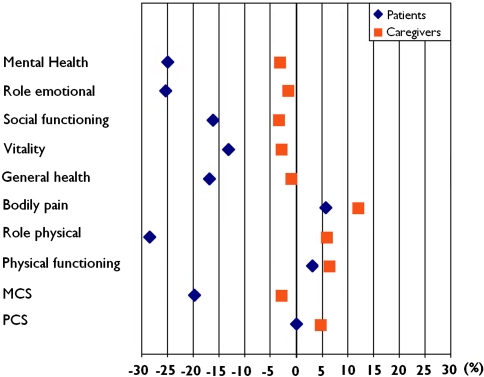
Figure 1 shows the proportional difference of scores of caregivers and patients compared to the average Dutch population on the eight domains and summary scores of the RAND-36. RAND-36 scores of caregivers tended to be marginally lower in MCS (−2 points, p = 0.16), while PCS scores (+2) and scores on the domains physical functioning (+5.3) and bodily pain (+9) were above average (p < 0.05) (Fig. 1).
Fig. 1.
Proportional difference of RAND-36 scores of patients and caregivers compared to the Dutch population average which is presented as zero (the y-axis). Patient HRQOL scores are decreased on most domains. Caregiver scores are similar to the general Dutch population, although they score significantly higher on bodily pain
RAND-36 scores of patients were significantly reduced (p < 0.01) on the MCS (−10 points) and the individual mental domains: social functioning (−14 points), mental health (−19 points), vitality (−11 points) and general health (−12 points) and the physical domain: role physical (−22 points). This last domain describes experienced physical restrictions in reaching goals in life.
Interactions between caregivers and patients
Low-to-medium positive correlations between patients and caregivers were found for the RAND-36 domains physical functioning, social functioning, mental health, bodily pain, general health, physical component score and MCS (Table 2). There was a correlation of passive coping style of patients and caregivers (Pearson R = 0.25, R 2 = 0.06, p = 0.03). Other coping styles did not show statistically significant correlations.
Table 2.
Relation between caregiver and patient RAND-36 scores
| Pearson’s correlation (R) | p value | |
|---|---|---|
| Physical functioning | 0.44 | <0.01 |
| Social functioning | 0.53 | <0.01 |
| Role physical | 0.05 | 0.65 |
| Role emotional | 0.17 | 0.13 |
| Mental health | 0.30 | 0.01 |
| Vitality | 0.16 | 0.15 |
| Bodily pain | 0.24 | 0.03 |
| General health | 0.28 | 0.01 |
| PCS | 0.35 | <0.01 |
| MCS | 0.32 | <0.01 |
| EQ5D | 0.19 | 0.09 |
The relations were established calculating Pearson correlation co-efficient. A positive correlation indicates that when the patient scores high on a certain domain his or her caregiver tends to score high on this domain as well. PCS and MCS stand for physical and mental component score
No significant correlations between coping style of caregivers and patient physical component score or MCS was found (Table 3).
Table 3.
Utrecht Coping List scores of male and female caregivers and Dutch population (mean and standard deviation) and correlation of coping scores to caregiver and patient mental and physical component score (MCS and PCS)
| Coping style | Scores Utrecht coping list | Pearson correlation of Utrecht coping list scores to MCS and PCS | ||||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | |||||||
| Caregivers | Dutch population | Caregivers | Dutch population | |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | MCS caregiver | PCS caregiver | MCS patient | PCS patient | |
| Active confronting | 20 (3.8) | 18.3 (3.5) | 19 (2.8) | 19.3 (5.1) | 0.16 | 0.05 | −0.10 | −0.03 |
| Palliative reaction | 15 (3) | 15.5 (3.6) | 17 (3.2) | 17.3 (6.1) | −0.41** | −0.30** | 0.03 | −0.13 |
| Avoidance | 15 (3) | 14.8 (3.3) | 15 (2.7) | 15.2 (6.0) | −0.16* | −0.22* | −0.16 | −0.19 |
| Seeking social support | 12 (2.8) | 11.3 (3.0) | 14 (3.6) | 14.5 (4,9) | −0.07 | −0.02 | −0.01 | −0.01 |
| Passive reaction pattern | 10 (2.4) | 10.7 (2.9) | 11 (2.5) | 10.9 (5.4) | −0.71** | −0.10 | −0.18 | 0.02 |
| Expressing emotions | 6 (1.5) | 6.2 (1.7) | 6 (1.4) | 6.4 (2.3) | −0.26 | −0.08 | −0.12 | 0.02 |
| Reassuring thoughts | 12 (2.4) | 11.6 (2.5) | 13 (2.5) | 12.1 (3.8) | −0.07 | −0.07 | −0.12 | −0.11 |
** p < 0.01, * p < 0.05
Coping and quality of life
The distribution of coping styles of caregivers was comparable to the general Dutch population (Table 3).
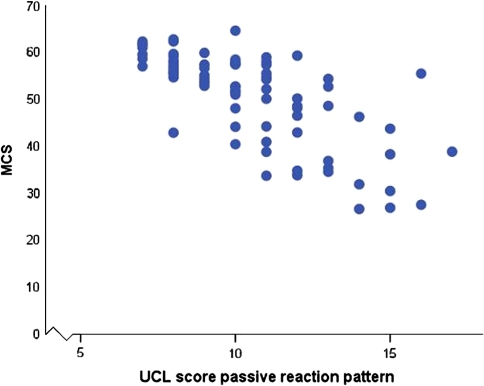
Passive coping style had the strongest association to the MCS in caregivers (Table 3, Fig. 2): passive coping style explained 50% of the variance in MCS (R 2 = 0.50), using univariate analysis. The gender of the caregiver and whether the patient experienced side effects of anti-epileptic drugs were also related to the caregiver MCS in the univariate analysis (p < 0.20, Table 3). The multivariate model with passive coping style and gender of the caregiver, and side effects in the patient explained 55% of variance in MCS (R 2 = 0.55), suggesting that these last two parameters explained only an additional variation of about 5% compared to passive coping style of the MCS (Table 4).
Fig. 2.
Scatter plot relating caregivers’ mental component score and score on passive coping style. High scores on passive coping style seem related to low scores on the mental component of HRQOL as measured by RAND-36
Table 4.
Results of uni- and multivariate analysis calculating the correlation of caregiver and patient characteristics and passive coping style to caregiver mental and physical component scores (MCS, PCS)
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| R | P | R2 | R | P | R2 whole model | |
| Mental component scale | ||||||
| Age | −0.09 | 0.43 | ||||
| Sex | −0.28 | 0.01 | 0.08 | −0.16 | 0.052 | |
| Relationship to patient | −0.02 | 0.84 | ||||
| Cohabiting | −0.08 | 0.49 | ||||
| Hours of care given to patient | 0.04 | 0.76 | ||||
| Professional help in patient care | −0.11 | 0.32 | ||||
| Employment status | ||||||
| patient | −0.04 | 0.74 | ||||
| Duration epilepsy | −0.08 | 0.51 | ||||
| Seizure freguency (per month) | −0.09 | 0.42 | ||||
| Numberof AED’s | −0.05 | 0.67 | ||||
| Adverse side-effects | −0.16 | 0.15 | 0.03 | −0.16 | 0.04 | |
| Coping: passive reaction pattern | −0.71 | 0 | 0.5 | −0.67 | 0 | 0.55 |
| Physical component scale | ||||||
| Age | −0.39 | 0.01 | 0.15 | −0.28 | 0.01 | |
| Sex | 0.01 | 0.94 | ||||
| Relationship to patient | 0.11 | 0.35 | ||||
| Cohabiting | 0.17 | 0.12 | 0.03 | 0.19 | 0.07 | |
| Hours of care given to patient | −0.4 | 0.01 | 0.16 | −0.36 | 0 | |
| Professional help in patient care | −0.03 | 0.79 | ||||
| Employment status patient | 0.06 | 0.63 | ||||
| Duration epilepsy | −0.1 | 0.45 | ||||
| Seizure frequency (per month) | 0.01 | 0.92 | ||||
| Number of AEDs | 0.02 | 0.83 | ||||
| Adverse side-effects | 0 | 0.98 | −0.12 | 0.25 | ||
| Coping: passive reaction pattern | −0.1 | 0 | 0.01 | 0.54 | 0 | 0.29 |
ÇVariables associated to MCS and PCS with a p value < 0.20 were included in multivariate analysis. R 2 is given for these variables and for the whole model. R 2 indicates the proportion of variance explained by these individual variables or the whole model
The coping style palliative reaction had the strongest correlation to physical component score in caregivers (Table 3). Univariate analysis showed age, cohabiting and hours of care given to epilepsy patient to be related to caregiver physical component score. A multivariate model including these factors and passive coping style (as a comparison to MCS) explained 29% (R 2 = 0.29) of variance in physical component score with passive coping style contributing only 1% (Table 4).
Discussion
Caregivers for chronic epilepsy patients report similar HRQOL compared to the general Dutch population. However, there is a significant correlation between passive coping style and lower mental component HRQOL scores in caregivers of epilepsy patients. Caregivers show relatively high scores, i.e. feel better than average, on physical aspects of HRQOL such as bodily pain and physical functioning. Within couples of caregivers and patients, associations on several domains of the HRQOL scores are found. Passive coping style explains 50% of variation in HRQOL scores of caregivers. Caregivers of patients with a passive coping style, often also have a passive coping style themselves.
This study yields two interesting correlations. Firstly, coping style explains a high percentage of variation in mental component of HRQOL in caregivers. We found the same between coping and HRQOL in epilepsy patients [8]. Other studies on coping of caregivers of patients with chronic disease show comparable results. Objective disease (seizure related) measures seem to matter less, again as in other diseases. For HRQOL of caregivers of patients with Huntington’s disease a positive correlation was found between positive appraisal of caregiving and general life satisfaction. Caregivers’ individual interpretation of their situation had a more significant impact on well-being than objective disease characteristics [14]. Visser-Meily et al. [15] found that 15–27% of variance in psychological functioning of spouses of stroke patients could be explained by coping strategies.
Secondly, we found that scores on several domains of caregiver HRQOL are significantly associated to scores on these same domains of the patient they are close to. Similar results have been found in patients with heart failure and their spouses. Patients with spouses scoring high on depression had lower HRQOL scores [16]. This brings up the thought that patient HRQOL can be improved by improving caregiver HRQOL. Because we found coping to be such an important factor in HRQOL in caregivers, an intervention on coping of caregivers could lead to better HRQOL of caregivers and patients. Results from other studies indicate this might be the case. Interventions for caregivers of patients with dementia led to benefits in psychological distress of caregivers and in patient mood. Also, patients were able to stay at home cared for by their spouses for a longer period of time [17]. In pain management in end-stage cancer patients, a partner-guided pain management training protocol improved caregiver satisfaction for being able to help the patient control pain [18]. Currently, a large trial with COPD patients and caregivers studies the influence of an intervention through training coping skills of patients as well as caregivers [19].
In a previous study on QOL of caregivers of epilepsy patients we found a trend for lower MCS of caregivers [6]. This study was executed in a small group of patients with severe, intractable forms of epilepsy. Our present study does not show a significantly decreased MCS in caregivers of focal epilepsy patients. This difference can probably be explained by the fact that the epilepsy patients in the present group have less severe forms of epilepsy.
The response rate of 49% for couples of patients and caregivers was relatively low. It is conceivable that a more assertive group of patients and caregivers has responded yielding relatively high HRQOL scores.
Other studies on caregiver QOL report a tendency towards slightly reduced QOL in caregivers of patients with chronic disease. For example, a HRQOL study in multiple sclerosis (MS) showed a 3.4 point lower MCS in caregivers [20]. Another study in caregivers of MS patients showed lower SF-36 scores on the domains mental health, general health and vitality [21]. It is difficult to compare epilepsy to more chronically progressive diseases. Focal epilepsy is a paroxysmal recurrent disease and the majority of patients are physically normal between seizures, in contrast to MS. In more severe and intractable epilepsy a lower QOL in caregivers would be expected (as we found earlier). On the other hand, several studies have shown that objective disease characteristics do not explain variation in HRQOL in epilepsy patients because even in patients with a single or few seizures the unpredictability of the disease has a high psychological impact [4].
Another notable result of this study was that caregiver HRQOL scores were relatively high (positive) on physical domains, especially on bodily pain. In the previously mentioned study on caregivers of MS patients a 6 points higher score on bodily pain was found [21], but other studies do not show higher physical component scores for caregivers [22, 23]. An explanation could be that caregivers compare their own physical functioning to that of the patient they live with and not to healthy persons in their environment. This effect could vary in several studies because of the different characteristics of the chronic diseases of patients. It is still difficult to explain this effect in caregivers of epilepsy patients because epilepsy does not lead to more bodily pain in patients.
Though most research on coping style and HRQOL cannot prove causality, in general it is believed that certain coping styles enhance the ability of patients with chronic disease to positively adjust to their situation [24].
Our findings do not indicate caregivers of epilepsy patients studied have significantly decreased quality of life. We find that variance in caregiver HRQOL is largely explained by coping style, as we have previously seen in patients [8], and that coping styles of patients and caregivers are related. To us these findings illustrate that regarding patient care, doctors are not only dealing with a disease but also with the way a person and their environment cope with this disease. We believe interventions in coping style of caregivers as well as patients with chronic disease could have a significant positive impact on HRQOL of both parties. However, research investigating a causal relation between coping style and HRQOL in epilepsy patients is needed to support this conclusion. We advise treating physicians of epilepsy patients to consider well-being of caregivers as well as patients, especially because they tend to have similar coping strategies. Caregivers should be included in the treatment of epilepsy patients and how patients and caregivers are coping with the disease should be considered. When problems in coping are detected, psychological help for epilepsy patients and their caregivers might be indicated and could lead to a significant increase in HRQOL in caregivers as well as patients.
Acknowledgments
We thank all patients and caregivers who participated in this study. We also thank Chad Gundy and Neil Aaronson from The Netherlands Cancer Institute for providing us with extensive data of Dutch population scores on the RAND-36. The study was financially supported by the Netherlands Organization for Scientific Research (NWO), Grant No. 945-05-039.
Conflicts of interest
None of the authors has any conflict of interest to disclose. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Forsgren L, Beghi E, Õun A, Sillanpää M. The epidemiology of epilepsy in Europe. Eur J Neurol. 2005;12:245–253. doi: 10.1111/j.1468-1331.2004.00992.x. [DOI] [PubMed] [Google Scholar]
- 2.Baker GA, Jacoby A, Buck D, Stalgis C, Monnet D. Quality of life of people with epilepsy: a European study. Epilepsia. 1997;38(3):353–362. doi: 10.1111/j.1528-1157.1997.tb01128.x. [DOI] [PubMed] [Google Scholar]
- 3.Jacoby A, Baker GA, Steen N, Potts P, Chadwick DW. The clinical course of epilepsy and its psychosocial correlates: findings from a UK community study. Epilepsia. 1996;37:148–161. doi: 10.1111/j.1528-1157.1996.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 4.Jacoby A, Snape D, Baker GA. Determinants of quality of life in people with epilepsy. Neurol Clin. 2009;27(4):843–863. doi: 10.1016/j.ncl.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Thompson PJ, Upton D. The impact of chronic epilepsy on the family. Seizure. 1992;1:43–48. doi: 10.1016/1059-1311(92)90054-5. [DOI] [PubMed] [Google Scholar]
- 6.Van Andel J, Zijlmans M, Fischer K, Leijten FSS. Quality of life of caregivers of patients with intractable epilepsy. Epilepsia. 2009;50(5):1294–1296. doi: 10.1111/j.1528-1167.2009.02032.x. [DOI] [PubMed] [Google Scholar]
- 7.Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. 2003;129(2):216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- 8.Westerhuis W, Zijlmans M, Fischer K, van Andel J, Leijten F (2010) Coping style and quality of life in patients with epilepsy: a cross-sectional study. J Neurol (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 9.Aaronson NK, Muller M, Cohoen PD, Essink-Bot M-L, Fekkes M, Sanderman R, Sprangers MAG, Velde te A, Verrips E. Translation, validation and norming of the Dutch language version of the RAND-36 health survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–1068. doi: 10.1016/S0895-4356(98)00097-3. [DOI] [PubMed] [Google Scholar]
- 10.Hoeymans N, van Lindert H, Westert GP. The health status of the Dutch population as assessed by the EQ-6D. Qual Life Res. 2005;14:655–663. doi: 10.1007/s11136-004-1214-z. [DOI] [PubMed] [Google Scholar]
- 11.Schreurs PJG, van de Willige G, Tellegen B, Brosschot JF. Handleiding Utrechtse Coping Lijst: UCL. Lisse: Swets en Zeitlinger; 1988. [Google Scholar]
- 12.Wiebe S, Matijevic S, Elisaziw M, Derry PA. Clinically important change in quality of life in epilepsy. J Neurol Neurosurg Psychiatry. 2002;73:116–120. doi: 10.1136/jnnp.73.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ware JE, Kosinski M. The RAND-36 physical and mental health summary scales: a manual for users version 1. 2. Lincoln: Qualimetric; 2001. [Google Scholar]
- 14.Roscoe LA, Corsentino E, Watkins S, McCal M, Sanchez-Ramos J. Well-being of family caregivers of persons with late-stage Huntington’s disease: lessons in stress and coping. Health Commun. 2009;24:239–248. doi: 10.1080/10410230902804133. [DOI] [PubMed] [Google Scholar]
- 15.Visser-Meily A, Post M, Port vd I, Maas C, Forstberg-Wärleby G, Lindeman E. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke, course and relations with coping strategies. Stroke. 2009;40:1399–1404. doi: 10.1161/STROKEAHA.108.516682. [DOI] [PubMed] [Google Scholar]
- 16.Chung ML, Moser DK, Lennie TA, Rayens MK. The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: testing dyadic dynamics using Actor-Partner Interdependence Model. J Psychosom Res. 2009;67(1):29–35. doi: 10.1016/j.jpsychores.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51:657–664. doi: 10.1034/j.1600-0579.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 18.Keefe FJ, Ahles TA, Sutton L. Partner-guided cancer pain management at the end of life: a preliminary study. J Pain Symptom Mange. 2005;29:263–272. doi: 10.1016/j.jpainsymman.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Blumenthal JA, Keefe JF, Babyak MA, Fenwick CV, Johnson JM, Stott K, Funk RK, McAdams MJ, Palmer S, Martinu T, Baucom D, Diaz PT, Emery CF. Caregiver-assisted coping skills training for patients with COPD: background, design, and methodological issues for the INSPIRE-II study. Clinical Trials. 2009;6:172–184. doi: 10.1177/1740774509102565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patti F, Amato MP, Battaglia MA, Pitaro M, Russo P, Solaro C, Trojano M. Caregiver quality of life in multiple sclerosis: a multicentre Italian study. Mult Scler. 2007;13(3):412–419. doi: 10.1177/1352458506070707. [DOI] [PubMed] [Google Scholar]
- 21.Forbes A, While A, Mathes L. Informal carer activities, carer burden and health status in multiple sclerosis. Clin rehabil. 2007;21(6):563–575. doi: 10.1177/0269215507075035. [DOI] [PubMed] [Google Scholar]
- 22.Wagner CD, Bigatti SM, Stornolio AM. Quality of life of husbands of women with breast cancer. Psychooncology. 2006;15(2):109–120. doi: 10.1002/pon.928. [DOI] [PubMed] [Google Scholar]
- 23.Alvarez-Ude F, Valdés C, Estébanez C, Rebollo P. Health-related quality of life of family caregivers of dialysis patients. J Nephrol. 2004;17(6):841–850. [PubMed] [Google Scholar]
- 24.De Ridder D, Geenen R, Kuijer R, Van Middendorp H. Psychological adjustment to chronic disease. Lancet. 2008;372:246–255. doi: 10.1016/S0140-6736(08)61078-8. [DOI] [PubMed] [Google Scholar]