Abstract
Purpose
To examine the performance and properties of the revised Health Care System Distrust scale among surrogates in the intensive care unit.
Materials and Methods
Pilot, prospective cohort study of 50 surrogates of adult, mechanically-ventilated patients surveyed on days 1, 3 and 7 of ICU admission.
Results
Responses on the Health Care System Distrust scale on day 1 ranged from 9 to 34 (possible range 9–45 with higher scores indicating more distrust), with a mean and standard deviation of 20.3 ± 6.9. Factor analysis demonstrated a 2-factor structure, corresponding to the domains of values and competence. Cronbach’s alpha for the overall scale was 0.83, for the competence subscale 0.76 and for the values subscale 0.74. Health care system distrust was inversely correlated with trust in ICU physicians (Pearson coefficient: −0.63). When evaluated over the course of each patient’s ICU stay, health care system distrust ratings decreased by 0.31 per patient-day (95% CI .55-.06; p=.015). Correlation between health care system distrust and trust in ICU physicians decreased slightly over time.
Conclusions
Among surrogates in the ICU, the Health Care System Distrust scale has high internal consistency and convergent validity. There was substantial variability in surrogates’ trust in the health care system.
Keywords: health care system, distrust, critical care, surrogate
Introduction
Trust is increasingly recognized as a measurable and important construct in health care. In sociological terms, trust can be viewed as a measure of social capital – a belief that the trustee will act in the truster’s best interests (1, 2). In the health care setting, trust and its converse, distrust, are thought to be multidimensional, encompassing perceptions that the health care system is capable of doing what is needed (technical competence) and the perception that the health care system aims to do what is needed (value congruence) (3). Much of the early work on trust in medical contexts focused on trust in one’s personal physician—a key component of the doctor-patient relationship that is known to be associated with patient satisfaction (4, 5), adherence to treatment regimens (6, 7), and willingness to remain with a physician (8, 9). More recently, health care system distrust has emerged as a related but conceptually distinct aspect of trust (3, 10, 11). While patients generally report high levels of trust in their own providers, distrust in the U.S. health care system is common and may be more closely associated with overall health status (11). Health care system distrust also differs between races—with African American patients generally reporting more distrust than Caucasian patients—and is a potential mediator of disparities in health care quality and outcomes (12–14), as well as observed underrepresentation of racial/ethnic minorities in medical research. (15)
Health care system distrust may play a particularly important role in the intensive care unit (ICU). Trust is directly tied to one’s sense of vulnerability (1), which is likely heightened by the high risk of morbidity and the number of invasive procedures inherent in critical care. Family members or other surrogates are often asked to make decisions for patients in the ICU who are too ill to communicate for themselves (16, 17). In a handful of studies, less trust in ICU physicians has been associated with physician-surrogate discordance about prognosis (18) and a preference among surrogates for more control over decision making (19). General mistrust has also been cited as a potential source of physician-family conflicts, which arise frequently in the setting of high stakes decision making about end-of-life issues (20, 21). However, surrogates in the ICU often lack an established relationship with the clinicians directing their loved one’s care, and therefore trust in one’s personal physician may be less important in the early stages of an ICU stay. In this context, family members’ trust in the health care system may affect how they relate to and interact with the clinical team. Therefore, the ability to measure health care system distrust may be central to efforts to understand and improve decision making in the ICU.
The Revised Health Care System Distrust Scale is a validated survey instrument for measuring health care system distrust in outpatient populations (3). However, to our knowledge, measurement of health care system distrust has not been validated in a critical care setting. In this paper we examine the performance and properties of the Revised Health Care System Distrust Scale among a diverse group of surrogate decision makers in the ICU, outline a conceptual model for the role of health care system distrust in modulating key ICU outcomes, and propose future directions for evaluating trust and distrust in the ICU.
Methods
Study Design, Subjects and Setting
We performed a pilot prospective, cohort study of health care system distrust among surrogate decision makers of critically ill patients. The setting for this study was the medical intensive care unit at the Hospital of the University of Pennsylvania, an 865-bed urban teaching hospital in Philadelphia, Pennsylvania. Because of its location, the hospital provides both primary care for urban, inner-city patients in Philadelphia and tertiary referral care for patients throughout southeastern Pennsylvania, southern New Jersey and northern Delaware. The medical ICU has 24 beds and is staffed by two attending intensivists, each of which manage a team consisting of a nurse practitioner, a clinical pharmacist, and between 3 and 6 physicians-in-training.
Subjects were mechanically-ventilated, adult ICU patients and their primary surrogate decision makers. All weekday and non-holiday admissions from August 19, 2009 to February 3, 2010 were screened for eligibility. We excluded patients with chronic respiratory failure, patients who were likely to die within 24 hours, patients who lacked a surrogate decision maker, and surrogates who were non-English speaking. Recruitment took place within 24 hours of ICU admission. We did not perform specific sample size calculations. Instead, we enrolled a total of 50 patients and 50 surrogates as an initial sample that would allow us to determine the properties of the Revised Health Care System Distrust Scale in a diverse ICU population.
All surrogates provided written informed consent. Human subjects regulatory approval was obtained from the University of Pennsylvania Institutional Review Board.
Measurements
All data were collected by a trained research coordinator. Patient clinical data was obtained from the medical chart. Other data were obtained from in-person interviews with surrogate decision makers. Interviews were performed on days 1, 3 and 7 of ICU admission using standardized survey instruments. All surrogates were interviewed on day 1, and subsequent interviews were performed as long as the patient was still alive and in the ICU. In the event that surrogates were not available for interview on a given study day they were interviewed on the next study day.
Health care system distrust
We measured health care system distrust among surrogates using the 9-item Revised Health Care System Distrust scale (3) (see Table 2 for wording of individual items). This scale was administered on Day 1 for all surrogates and on days 3 and 7 if the patient was still alive and in the ICU at that time. The Revised Health Care System Distrust scale was developed in a multi-phase process involving focus groups with individuals of diverse racial/ethnic backgrounds from the Philadelphia area and interviews with primary care patients (3). Each item is answered using a 5-point scale where 1=strongly disagree and 5=strongly agree. The range of possible scores is 9–45, with higher scores indicating more distrust. The measure includes two subscales corresponding to the concepts of technical competence (4 items, range of possible scores 4–20) and value congruence (5 items, range of possible scores 5–25). Among individuals in the general population the scale has been found to have high internal consistency (Cronbach’s alpha overall 0.83; competence subscale 0.77; values subscale 0.73) and content validity (3).
Table 2.
Rotated factors loadings for the Revised Health Care System Distrust Scale
| Item | Sub-scale | Factor loadings
|
|
|---|---|---|---|
| Competence | Values | ||
| 1. The Health Care System does its best to make patients’ health better | C | 0.661 | −0.391 |
| 2. The Health Care System covers up its mistakes | V | 0.474 | 0.474 |
| 3. Patients receive high quality medical care from the Health Care System | C | 0.733 | −0.494 |
| 4. The Health Care System makes too many mistakes | C | 0.670 | 0.374 |
| 5. The Health Care System puts making money above patients’ needs | V | 0.808 | 0.168 |
| 6. The Health Care System gives excellent medical care | C | 0.751 | −0.449 |
| 7. Patients get the same medical treatment from the Health Care System, no matter what their race or ethnicity | V | 0.642 | −0.459 |
| 8. The Health Care System lies to make money | V | 0.678 | 0.468 |
| 9. The Health Care System experiments on patients without them knowing | V | 0.504 | 0.644 |
Items 1, 2 6 and 7 are reverse scored.
C = competence subscale, V = value subscale
Trust in ICU Physicians
To assess the relationship between health care system distrust and trust in the ICU physicians, we also administered an adapted version of the Trust in Physicians scale (5). (See appendix for adapted version.) This scale was administered on Day 1 for all surrogates and on days 3 and 7 if the patient was still alive and in the ICU at that time. The original 11-item scale showed high internal consistency (Cronbach’s alpha .89), reliability and content validity (5). We omitted a single question from the original scale that was not applicable to the ICU setting. The range of possible scores in the adapted version was 10–50, with higher scores indicating more trust.
Appendix.
Adapted Version of the Trust in Physicians Scale
| Full scale | Rate on scale of 1–5, 1 = strongly disagree and 5 = strongly agree | ||||
|---|---|---|---|---|---|
| 1. I doubt that ___________________’s doctors really care about him/her as a person | 1 | 2 | 3 | 4 | 5 |
| 2. ___________________’s doctors are usually considerate of his/her needs and puts them first | 1 | 2 | 3 | 4 | 5 |
| 3. If ___________________’s doctors tell me something is so, then it must be true | 1 | 2 | 3 | 4 | 5 |
| 4. I sometimes distrust ___________________’s doctors’ opinions and would like a second one | 1 | 2 | 3 | 4 | 5 |
| 5. I trust ___________________’s doctors’ judgments about his/her medical care | 1 | 2 | 3 | 4 | 5 |
| 6. I feel ___________________’s doctors do not do everything they should about his/her medical care | 1 | 2 | 3 | 4 | 5 |
| 7. I trust ___________________’s doctors to put his/her medical needs above all other considerations when treating his/her medical problems | 1 | 2 | 3 | 4 | 5 |
| 8. ___________________’s doctors are well qualified to manage (diagnose and treat or make an appropriate referral) medical problems like his/hers | 1 | 2 | 3 | 4 | 5 |
| 9. I trust ___________________’s doctors to tell me if a mistake was made about his/her treatment | 1 | 2 | 3 | 4 | 5 |
| 10. I sometimes worry that ___________________’s doctors may not keep the information we discuss totally private | 1 | 2 | 3 | 4 | 5 |
Surrogate and Patient Characteristics
Age, gender, race, surrogate-patient relationship, religion, household income, employment status and previous hospital experience for patients and surrogates were measured by questionnaire. Surrogates were asked to answer each of these questions for their loved one. For example, a question about prior hospitalization was worded: “To the best of your knowledge, has ____ been hospitalized in the past?” Religiosity was assessed by asking surrogates “How important is religion in your everyday life?,” with responses categorized as “not at all important,” “not too important,” “fairly important,” or “very important.”
Analysis
Patient and surrogate characteristics are presented as means and standard deviations, medians and interquartile ranges, or frequencies and percents, as appropriate. We used summary statistics and histograms to examine the distribution of item responses among surrogates for the overall Health Care System Distrust Scale and for the competence and values subscales. We then used exploratory factor analyses with the varimax orthogonal rotation to determine the factor structure of the scale among ICU surrogates (22). To determine the number of factors to extract we visually inspected a scree plot of eigenvalues. This process determined whether the scale loaded onto two factors and discriminated between the concepts of competence and values, as observed in the outpatient setting. Since factor analysis requires complete data, we first imputed missing values using single median imputation—values were missing for less than 2% of responses. Prior to factor analysis we reverse coded negatively worded items. We calculated Cronbach’s alpha to evaluate internal consistency for the overall scale and for each subscale.
To assess construct validity, we evaluated the association between health care system distrust and trust in ICU physicians by calculating Pearson correlation coefficients. We further explored changes in trust over the course of each patient’s ICU staying using linear regression with generalized estimating equations, in which the health care system distrust scale was the dependent variable and interview day was the independent variable (23). This approach allowed us to assess changes over time even though surrogates contributed different amounts of data and were not always interviewed on the same study day. We specified an exchangeable correlation matrix and robust Huber-White confidence intervals. All data analyses were performed using Stata 11.1 (College Station, TX). A p-value of ≤0.05 was considered significant.
Results
A total of 580 patients were screened for eligibility during the enrollment period. Of these, 493 were not eligible (412 not mechanically ventilated, 28 no surrogate available, 26 ventilator-dependent, 19 expired or death imminent, 8 other reasons). Of the 87 patients who met eligibility criteria, 5 were deemed inappropriate by their physicians and 32 had a surrogate who declined to participate, leaving a total of 50 patients and their surrogates enrolled.
Characteristics of surrogates and patients are shown in Table 1. Of the 50 surrogates, the majority were female and their ages ranged from 25 to 88. Of the 50 patients, the majority were male and ages ranged from 22 to 88. Most commonly, surrogates were the patient’s spouse/partner or child. Just over one third of patients and surrogates were African American. Surrogates and patients were predominantly Christian, Catholic or Protestant, and 88% of surrogates reported that religion was fairly or very important in their everyday life. Household incomes ranged widely. Over half of surrogates worked full or part time outside the home, while the majority of patients were either unemployed or retired. The vast majority of surrogates and patients had previously been hospitalized, and many had prior experiences in the ICU.
Table 1.
Surrogate and patient characteristics
| Variable | Surrogate (n = 50) | Patient (n = 50) |
|---|---|---|
| Age, years, mean ± SD | 53.8 ± 12.7 | 58.1 ± 15.2 |
| Female | 35 (70.0) | 18 (36.0) |
| Race | ||
| White | 29 (58.0) | 31 (62.0) |
| Black | 17 (34.0) | 17 (34.0) |
| Other | 4 (8.0) | 2 (4.0) |
| Relationship to patient | ||
| Spouse/partner | 21 (42) | |
| Parent | 6 (12) | |
| Sibling | 8 (16) | |
| Child | 11 (22) | |
| Friend | 2 (4) | |
| Other relative | 2 (4) | |
| Religion | ||
| Christian | 13 (26.0) | 9 (18.0) |
| Catholic | 14 (28.0) | 16 (32.0) |
| Protestant | 13 (26.0) | 14 (28.0) |
| Jewish | 4 (8.0) | 4 (8.0) |
| No religious affiliation | 2 (4.0) | 3 (6.0) |
| Other | 4 (8.0) | 4 (8.0) |
| Household income | ||
| < $50,000 | 19 (38.0) | 19 (38.0) |
| $50,000 – $100,000 | 10 (20.0) | 9 (18.0) |
| $100,000 + | 18 (36.0) | 13 (26.0) |
| Decline to answer | 3 (6.0) | 8 (16.0) |
| Unknown | 0 (0) | 1 (2.0) |
| Employment status | ||
| Full or part time out of home | 31 (62.0) | 16 (32.0) |
| In home/homemaker | 7 (14.0) | 1 (2.0) |
| Unemployed | 5 (10.0) | 14 (28.0) |
| Retired | 7 (14.0) | 19 (38.0) |
| Previous hospital experience | ||
| Prior hospitalization | 45 (90.0) | 40 (80.0) |
| Prior ICU admission | 13 (26.0) | 28 (56.0) |
| Prior episode of MV | 4 (8.0) | 15 (30.0) |
Values are N (percent) except where indicated otherwise.
Abbreviations: SD = standard deviation; ICU = intensive care unit; MV = mechanical ventilation
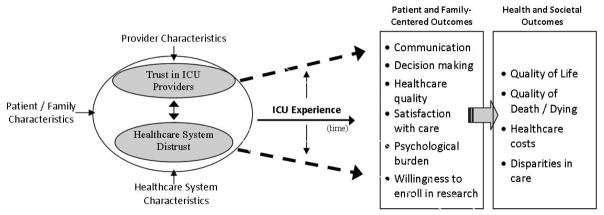
Distribution of surrogates’ responses to the Health Care System Distrust Scale on Day 1 are shown in Figure 1. For the overall scale, responses ranged from 9 to 34, with a mean and standard deviation of 20.3 ± 6.9. For the original competence subscale, responses ranged from 4 to 17, with a mean and standard deviation of 8.3 ± 3.2. For the original values subscale, responses ranged from 5 to 22, with a mean and standard deviation of 12.0 ± 4.4.
Figure 1.
Distribution of the Health Care System Distrust Scale in surrogate decision makers of intensive care patients: overall scale (Panel A), competence sub-scale (Panel B), and value sub scale (Panel C).*
*The Competence and Value subscales include the questions originally assigned to each subscale in the work by Shea et al. (3)
In factor analysis, the overall scale loaded onto two factors. Factor loadings for the two subscales are shown in Table 2. Cronbach’s alpha for the overall scale was 0.83, for the original competence subscale 0.76 and for the original values subscale 0.74.
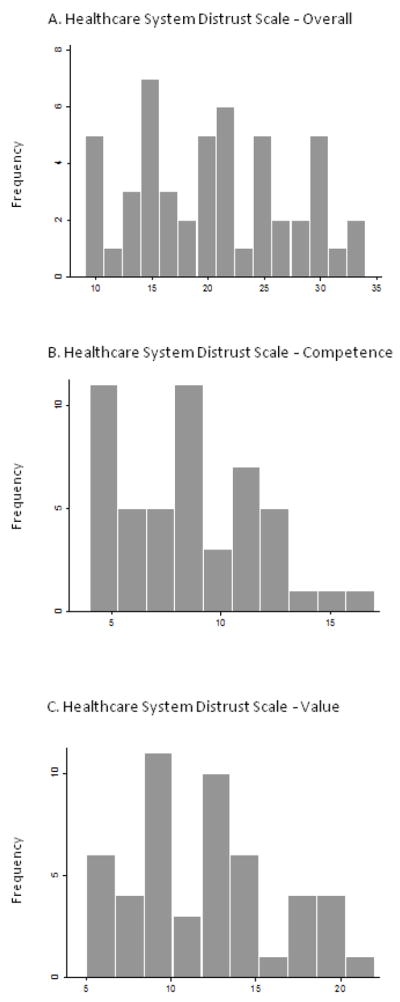
The association between health care system distrust and trust in physicians on day 1 is shown in Figure 2. As health care system distrust increased trust in physicians decreased, with substantial correlation between the two variables (Pearson correlation coefficient: −0.63). When evaluated over the course of each patient’s ICU stay, health care system distrust ratings decreased by 0.31 per patient-day (95% CI .55-.06; p=.015). In contrast, trust in physicians remained unchanged (change in trust for each day = 0.12, 95% CI: −0.15 to 0.39, p=0.39). Correlation between heath care system distrust and trust in physicians slightly decreased over time (day 3 Pearson correlation coefficient: −0.61, n=39; day 7 Pearson correlation coefficient: −0.54, n=15).
Figure 2.
Correlation between the Health Care System Distrust Scale and trust in physicians.
Discussion
We demonstrate that health care system distrust is a measurable construct among surrogate decision makers in the ICU, with wide variation in the diverse population we studied and no obvious floor or ceiling effects. Consistent with findings in non-critical care settings (3, 10), the measure also had high internal consistency and discriminated between the concepts of values and competence. Its convergent validity is supported by the inverse correlation with trust in ICU physicians, and the diminution of the correlation between health care system distrust and trust in physicians over the course of a patient’s ICU stay may support the instrument’s divergent validity.
The erosion of public trust in physicians and the health care enterprise has received significant attention in recent years (2, 24, 25), leading to a proliferation of research on how to measure patient trust and its significance on both intrinsic grounds and as a predictor of health outcomes (1, 26, 27). The majority of this research has focused on trust between a patient and his or her personal physician (5, 27, 28). Less attention has been paid to measures of trust or distrust in medical systems, or to the importance of these concepts outside the primary care physician’s office. To our knowledge, ours is the first study to measure health care system distrust among surrogates in the ICU, and our findings support the feasibility of future research aimed at understanding the role of health care system distrust in critical care settings.
Understanding health care system distrust among surrogates is important for several reasons. First, increased vulnerability associated with serious illness, invasive procedures, and patients’ loss of decision making capacity increase the need for trust in the ICU. Second, previous studies in different settings have demonstrated divergent validity between broader measures of trust in the medical system or physicians in general and interpersonal physician trust (11, 29). Hall et al hypothesized that early in a treatment relationship, interpersonal trust is likely to be based primarily on trust in general systems, but that as a relationship progresses, a divergence between general and interpersonal trust is more likely (29). The absence of long-standing relationships with ICU physicians, coupled with extensive previous exposure to the health care system, may elevate the importance of health care system distrust among surrogates, which in turn may influence trust in personal physicians. As suggested by our preliminary finding of decreased correlation between health care system distrust and trust in ICU physicians over the course of a patient’s stay, these concepts may diverge based on time and experiences in the ICU. Though of note, the trust in physicians scale we used was not developed specifically for ICU physicians, and it is possible that aspects of interpersonal trust in critical care settings remain unmeasured. And finally, trust may relate to key outcomes in the ICU, including family satisfaction, the quality of physician-family communication, the quality of death or dying, and the high psychological burden experienced by surrogates.
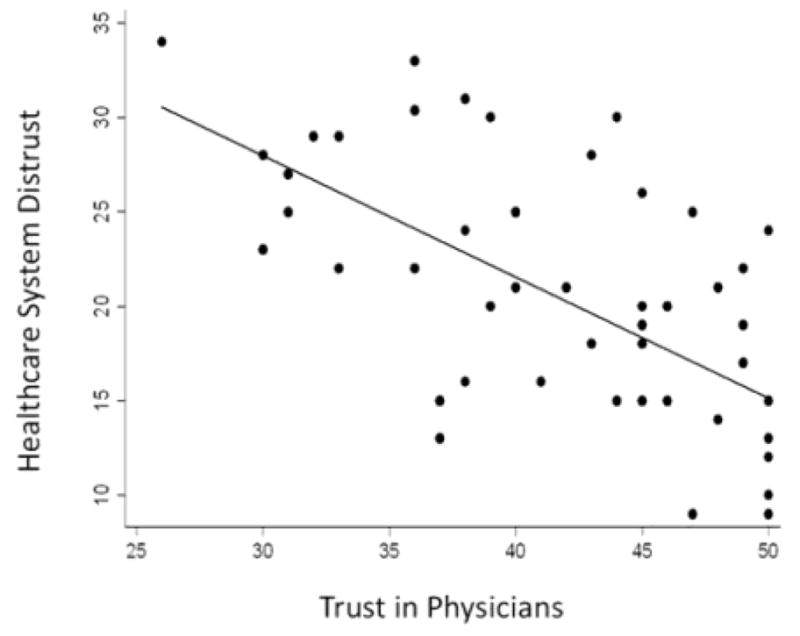
The role of health care system distrust among surrogates in the ICU is likely to be complex. We have developed a preliminary conceptual model to guide future research aimed at understanding predictors and outcomes of the general construct of trust in critical care settings (Figure 3). In this model the broad concept of trust comprises health care system distrust and trust in providers, and may be affected by provider factors (demographics, professional characteristics, personality, communication style, interpersonal skills), patient and family factors (socio-demographic characteristics, personality, familial relationships, cultural background, prior experiences with illness and/or the healthcare system), and health care system factors (medical errors, cultural sensitivity, and costs). While trust in physicians is the most studied, we refer broadly to trust in ICU providers in this model because other types of providers (such as nurse practitioners, nurses, or social workers) may also play an important role in this arena. Our model hypothesizes that health care system distrust is a separate construct from trust in providers, although they are tightly linked. The degree to which they are correlated may change over time and in relationship to one’s experiences in the ICU. In addition, we propose several potential effects of trust or distrust in the ICU, categorized as patient and family-centered outcomes (communication, decision-making, health care quality, satisfaction with care, psychological burden, willingness to enroll in research) and health and societal outcomes (quality of life, quality of death, healthcare costs and disparities in care). Future work should empirically test the components of this model, especially whether health care system distrust and trust in providers are truly distinct entities in the ICU setting, or if they are merely different ways to measure a single, greater concept of general trust.
Figure 3. Conceptual Model of Trust in the ICU (adapted from Armstrong, 2006).
This model illustrates that provider, patient/family, and healthcare system characteristics may influence trust in the ICU. Trust in providers and healthcare system distrust are related and likely to change over the duration of an ICU stay. Potential outcomes of trust in the ICU are listed.
Several additional questions merit particular attention in future studies. First, building on previous work examining racial differences in health care-related distrust and the potential role of distrust as a contributor to racial disparities in critical care (13, 30), we need additional research to understand how patterns of health care system distrust in the ICU differ among diverse racial/ethnic groups. Racial differences in the use of intensive care services at the end of life are well described, with black patients receiving more intensive treatments and less palliative and hospice care before death than white patients, but such differences remain incompletely understood (31, 32). Issues of trust in the health care system may play a role in these racial differences, and data is needed to support or refute such hypotheses.
Second, trust is commonly understood as a state, not a trait, meaning it is susceptible to change over time and may be amenable to intervention (33). In our pilot study, for example, healthcare system distrust lessened over the course of a patient’s ICU stay. Caution should be exercised in drawing conclusions from this finding, given our small sample size. However, larger studies and/or the addition of qualitative data may elucidate experiences in the ICU, such as information sharing with families, interactions with staff, and the provision of culturally sensitive care, that may decrease health care system distrust among surrogates, thereby helping to define appropriate targets for future intervention.
Third, family members of critically ill patients in the ICU experience significant burdens as surrogate decision makers (34, 35). Current international guidelines recommend a shared decision-making model, in which surrogate decision makers and physicians share the responsibility of making decisions on behalf of incapacitated ICU patients (35). However, such a model may be undermined by a lack of trust on the part of surrogates. Recent studies have explored the association between trust in the ICU physician and surrogate understanding of prognosis or preference for control over life support decisions (18, 19). Additional work is needed to evaluate how distrust in the health care system, separate from the nascent relationship between family and intensivist, may impact the process and outcomes of surrogate decision making.
Finally, low rates of enrollment in clinical research, particularly among underrepresented minorities, is a major barrier to ICU research (36). Health care system distrust may influence decisions about research participation. That is, surrogates with more health care system distrust may be unwilling to accept the additional risk of research participation. A better understanding of the role of trust in clinical research participation may inform novel strategies to increase enrollment rates and minimize racial/ethnic disparities in clinical research participation.
Our study had several limitations. As a pilot evaluation, we were not powered to evaluate factors associated with health care system distrust. We anticipate conducting follow-up studies in larger groups to explore the important issues we have described. Additionally, although our sample was fairly diverse, this study was conducted in a single medical ICU. Patterns of trust and distrust vary by county, or even geographic locations within counties (37). Our sample also had considerable experience with hospitalization and the ICU, which may influence trust. Multi-site studies are needed to replicate these findings. Finally, measures of trust may be biased by selection for surrogates willing to participate in a clinical study. In this study 42.5% of eligible subjects did not participate. The direction of the bias is likely selection toward more trusting individuals. However, future work is needed to define the relationship between trust and willingness to participate in clinical research.
In summary, health care system distrust is a measurable and conceptually important construct among surrogate decision makers in the ICU. Understanding its complex role in critical care settings has implications for patients, families, and society.
Acknowledgments
Dr. Schenker was supported by a Junior Faculty Career Development Award from the National Palliative Care Research Center. Dr. White is supported by a Greenwall Foundation Faculty Scholars Award and a Paul Beeson Award in Aging Research from the National Institutes of Health (AG032875). Dr. Kahn is supported by a career development award from the National Institutes of Health (HL082650).
Footnotes
The authors have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79:613–39. v. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilson L. Trust and the development of health care as a social institution. Soc Sci Med. 2003;56:1453–68. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- 3.Shea JA, Micco E, Dean LT, McMurphy S, Schwartz JS, Armstrong K. Development of a revised Health Care System Distrust scale. J Gen Intern Med. 2008;23:727–32. doi: 10.1007/s11606-008-0575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Pract. 2002;19:476–83. doi: 10.1093/fampra/19.5.476. [DOI] [PubMed] [Google Scholar]
- 5.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study. Physicians Med Care. 1999;37:510–7. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Piette JD, Heisler M, Krein S, Kerr EA. The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749–55. doi: 10.1001/archinte.165.15.1749. [DOI] [PubMed] [Google Scholar]
- 7.Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–20. [PubMed] [Google Scholar]
- 8.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician’s practice. J Fam Pract. 2001;50:130–6. [PubMed] [Google Scholar]
- 9.Tarrant C, Dixon-Woods M, Colman AM, Stokes T. Continuity and trust in primary care: a qualitative study informed by game theory. Ann Fam Med. 8:440–6. doi: 10.1370/afm.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rose A, Peters N, Shea JA, Armstrong K. Development and testing of the health care system distrust scale. J Gen Intern Med. 2004;19:57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. J Gen Intern Med. 2006;21:292–7. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008;56:1953–8. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Armstrong K, McMurphy S, Dean LT, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med. 2008;23:827–33. doi: 10.1007/s11606-008-0561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halbert CH, Armstrong K, Gandy OH, Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 15.Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14:537–46. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White DB, Curtis JR. Care near the end-of-life in critically ill patients: a North American perspective. Curr Opin Crit Care. 2005;11:610–5. doi: 10.1097/01.ccx.0000184301.76007.70. [DOI] [PubMed] [Google Scholar]
- 17.Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35:605–22. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 18.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 182:905–9. doi: 10.1164/rccm.201002-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson SK, Bautista CA, Hong SY, Weissfeld L, White DB. An Empirical Study of Surrogates’ Preferred Level of Control over Value-Laden Life Support Decisions in Intensive Care Units. Am J Respir Crit Care Med. 2010 Oct 29; doi: 10.1164/rccm.201008-1214OC. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Azoulay E, Timsit JF, Sprung CL, et al. Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med. 2009;180:853–60. doi: 10.1164/rccm.200810-1614OC. [DOI] [PubMed] [Google Scholar]
- 21.Fassier T, Azoulay E. Conflicts and communication gaps in the intensive care unit. Curr Opin Crit Care. 2010 Oct 27; doi: 10.1097/MCC.0b013e32834044f0. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Gorsuch RL. Factor Analysis. 2. Hillsdale, N. J: L Erlbaum Associates; 1983. [Google Scholar]
- 23.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 24.Shore DA, editor. The Trust Crisis in Healthcare. Oxford: Oxford University Press; 2007. [Google Scholar]
- 25.Rowe R, Calnan M. Trust relations in health care: developing a theoretical framework for the “new” NHS. J Health Organ Manag. 2006;20:376–96. doi: 10.1108/14777260610701777. [DOI] [PubMed] [Google Scholar]
- 26.Goudge J, Gilson L. How can trust be investigated? Drawing lessons from past experience. Soc Sci Med. 2005;61:1439–51. doi: 10.1016/j.socscimed.2004.11.071. [DOI] [PubMed] [Google Scholar]
- 27.Thom DH, Hall MA, Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care. Health Aff (Millwood) 2004;23:124–32. doi: 10.1377/hlthaff.23.4.124. [DOI] [PubMed] [Google Scholar]
- 28.Hall MA. Researching medical trust in the United States. J Health Organ Manag. 2006;20:456–67. doi: 10.1108/14777260610701812. [DOI] [PubMed] [Google Scholar]
- 29.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37:1419–39. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crawley L, Payne R, Bolden J, et al. Palliative and end-of-life care in the African American community. JAMA. 2000;284:2518–21. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 31.Barnato AE, Berhane Z, Weissfeld LA, Chang CC, Linde-Zwirble WT, Angus DC. Racial variation in end-of-life intensive care use: a race or hospital effect? Health Serv Res. 2006;41:2219–37. doi: 10.1111/j.1475-6773.2006.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169:493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKinstry B, Ashcroft RE, Car J, Freeman GK, Sheikh A. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2006;3:CD004134. doi: 10.1002/14651858.CD004134.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Pochard F, Darmon M, Fassier T, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005;20:90–6. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Carlet J, Thijs LG, Antonelli M, et al. Challenges in end-of-life care in the ICU. Intensive Care Med; Statement of the 5th International Consensus Conference in Critical Care; Brussels, Belgium. April 2003; 2004. pp. 770–84. [DOI] [PubMed] [Google Scholar]
- 36.Cooke CR, Erickson SE, Watkins TR, Matthay MA, Hudson LD, Rubenfeld GD. Age-, sex-, and race-based differences among patients enrolled versus not enrolled in acute lung injury clinical trials. Crit Care Med. 38:1450–7. doi: 10.1097/CCM.0b013e3181de451b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–9. doi: 10.2105/AJPH.2005.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]