Abstract
Objective
Toward meeting the need for a measure of individual differences in substance use disorder (SUD) liability that is grounded in the multifactorial model of SUD transmission, this investigation tested to what degree transmissible SUD risk is better measured using the continuous Transmissible Liability Index (TLI) (young adult version) compared to alternative contemporary clinical methods.
Method
Data from 9,535 18- to 30-year-olds in the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions, a U.S. representative sample, were used to compute TLI scores and test hypotheses. Other variables were SUDs of each DSM-IV drug class, clinical predictors of SUD treatment outcomes, treatment seeking and usage, age of onset of SUDs and substance use (SU), and eligibility for SUD clinical trials.
Results
TLI scores account for variation in SUD risk over and above parental lifetime SUD, conduct and antisocial personality disorder criteria and frequency of SU. SUD risk increases two- to four-fold per standard deviation increment in TLI scores. The TLI is associated with SUD treatment seeking and usage, younger age of onset of SU and SUD, and exclusion from traditional clinical trials of SUD treatment.
Conclusions
The TLI can identify persons with high versus low transmissible SUD risk, worse prognosis of SUD recovery and to whom extant SUD clinical trials results may not generalize. Recreating TLI scores in extant datasets facilitates etiology and applied research on the full range of transmissible SUD risk in development, treatment and recovery without obtaining new samples.
Keywords: substance use disorders, transmissible risk, assessment, young adults, treatment outcomes
1. Introduction
Recent literature reviews and individual studies have identified the need for innovative measures of the full scope of SUD liability that (a) quantifies finite individual differences, (b) builds upon the multifactorial nature of SUD etiology, and (c) encompasses liability that is shared among disorders consequent to using a variety of substances (Conway et al., 2010; Ridenour et al., 2009; Shaffer et al., 2004; Vanyukov et al., 2009). Theoretically, behavior genetics research offers the most encompassing models of overall SUD liability. To illustrate, the behavior genetic construct “transmissible risk” includes all genetic and environmental mechanisms underlying parent-child correlation for liability to an illness (Rice et al., 1980).
Attempts to quantify the full range of transmissible risk at the individual level have occurred based on a behavior genetic perspective (Boomsma et al., 1990; Boomsma et al., 1991) but have not led to instruments for widespread use in research or applied settings. Contemporary assessment of an individual’s transmissible risk typically is limited to estimating familial “load” based on number affected parents or other first-degree relatives (Clark et al., 2005; Kirillova et al., 2008; Leggio et al., 2009; Milne et al., 2009; Portier et al., 2004; Rice et al., 1980). However, numerous and complex genetic and environmental risk factors contribute to transmissible risk whereas a count of family members (usually parents) with SUD informs about the average risk of the group of persons having the same count (e.g., having two SUD parents vs. having only one). SUD transmissible risk also is not specific to substances. For instance, number of first-degree relatives with SUD resulting from use of one substance (e.g., alcohol) predicts an individual’s risk for SUDs from using other substances (Compton et al., 2002; Merikangas et al., 2009; Nurnberger et al., 2004). Twin studies document large overlap between heritable and environmental risk for SUDs related to different substances (Kendler, 2003b; Twuang et al., 1998). Furthermore, to a great extent, SUD genetic and environmental risks also contribute to externalizing disorders, personality characteristics such as disinhibition, and to a lesser extent internalizing disorders (Kendler et al., 2003a; King et al., 2004), all of which likely contribute to SUD ontogenies (Kendler, et al., 2003b; Knopik et al., 2004; Kreek et al., 2005; van den Bree et al., 1998).
Stemming from the multifactorial inheritance of SUD liability, a behavior genetic model has been developed for nuclear family data that allows partitioning SUD risk broadly into transmissible (composed of heritable and much of shared environment) and non-transmissible components (correlated and non-correlated between generations, respectively) (Kirisci et al., 2009; Vanyukov et al., 2003a; Vanyukov et al., 2009). A measure of transmissible SUD risk that is comprehensive must implicitly capture manifold paths of risk transmission between generations (Rice et al., 1980; Vanyukov et al., 2003b). This is because transmissible SUD risk encompasses varied sources and mechanisms. Considering genetic influences alone, genes associated with SUD risk are manifold, each singly contributing little to SUD risk variance and each usually associated with multiple forms of SUD (e.g., related to using tobacco as well as illegal drugs) (Bierut et al., 2007; Dick and Foroud, 2003; Kreek et al., 2005; Uhl et al., 2002). Accordingly, to quantify an individual’s transmissible SUD risk on a continuum, a method has been developed to index SUD liability using items that query a breadth of child characteristics which are associated with parental SUD, thus encompassing the various pathways to such outcomes (Kirisci et al., 2009; Vanyukov et al., 2003a; Vanyukov et al., 2009).
A measure of an individual’s overall SUD liability offers several practical benefits. Youth at elevated SUD risk needing targeted prevention could be readily and more accurately detected during routine screening (Leggio et al., 2009; Poirier et al., 2004; Kirisci et al., 2009). Need for long-term treatment or prevention may be better identified because transmissible SUD risk likely is mediated by factors that augment intractability of SUD, including genetic and transmissible environmental mechanisms (e.g., gene environment interactions contained in heritability estimates) translating into neuropsychological deficits or habitual behaviors formed through years of familial interactions (Caspi et al., 1996; Milne et al., 2009; Ridenour et al., 2009). Also, genetic studies which utilize the high-risk design could better identify persons belonging to high- versus low-risk groups.
An instrument that quantifies an individual’s overall transmissible SUD risk must achieve at least three qualities compared to other instruments. First, it must improve upon family history or counting relatives with SUD, which is used in research and applied settings (Milne et al., 2009). Second, in contrast to myriad measures of specific family characteristics that putatively mediate transmission of SUD risk to offspring, quantifying someone’s overall transmissible risk requires capturing risk variance that is due to manifold mediators in a single instrument (e.g., administering manifold measures is generally clinically unfeasible, each measure encompasses unspecified portions of variance in transmissible risk, and how much transmissible risk is contained in an individual’s score is unknown). Third, if in fact the instrument broadly measures overall transmissible risk rather than one of the major contributing factors (cf. conduct disorder, frequency of substance use), it should account for variance in SUD liability above and beyond those contributing factors. The Transmissible Liability Index (TLI) was recently developed to quantify an individual’s overall transmissible SUD risk on a normally distributed scale, specifically achieving the aforementioned qualities (Kirisci et al., 2009; Vanyukov et al., 2009).
Psychometric properties of the age 10–12 TLI include statistical prediction of SUD up to 12 years later (Kirisci et al., 2009; Vanyukov et al., 2009). Prior prospective research has shown that TLI scores at ages 10–12 are superior to paternal SUD diagnosis in predicting offspring’s SUD by early adulthood (Vanyukov et al., 2009). Consistent with the TLI theoretical and methodological underpinnings, its scores are highly heritable (Hicks et al., under review; Vanyukov et al., 2009) and its associations with adolescent SUD and behavioral disinhibition are largely due to heritable factors (Hicks et al., under review). Accomplishing one purpose of the TLI, to facilitate risk assessment for intervention, the young adult version of the TLI detects college youths in need of SUD prevention (Arria et al., 2009). Whereas TLI research to date has included distinct samples such as families with SUD and control parents (Kirisci et al., 2009), college students (Arria et al., 2009) and twins (Vanyukov et al., 2009), the present study evaluated the young adult TLI in a representative sample of the U.S. general population.
The following hypotheses were tested. TLI scores are highly associated with SUD diagnoses, treatment seeking, service utilization and onset as well as age of first substance use (SU). The TLI is more strongly associated with (and provides incremental validity for prediction of) SUD compared to number of parents with SUD as well as respondent symptoms of conduct disorder, symptoms of antisocial personality disorder and frequency of alcohol or illegal drug use. Additional exploratory analyses were based on Blanco et al.’s (2008a) report that sizable proportions of SUD patients meet commonly used exclusion criteria of randomized clinical trials. Systematic exclusion of patients with high transmissible SUD risk may have occurred in clinical trials because SUD risk and severity correlate with several of the exclusion criteria including low education, unstable employment and comorbid medical conditions. Thus, extant treatment literature may not generalize well to patients with high transmissible SUD risk. If so, the TLI could identify patients to whom extant clinical trial results do not generalize and assist with replication of clinical trials among persons with high transmissible liability to SUD.
2. Methods
2.1 Sample
The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) is a nationally-representative sample of adults living in all 50 United States and the District of Columbia. These data were acquired as a public dataset; as such, all IRB reviews and approvals occurred prior to obtaining the dataset. NESARC was conducted by the U.S. Census Bureau and National Institute on Alcohol Abuse and Alcoholism. The NESARC methods have been described previously in detail (Blanco et al., 2008b; Hasin et al., 2007). The sample was drawn from individual households and group residencies including college dormitories, military personnel living off base, boarding or rooming houses, nontransient hotels and motels, shelters, facilities for housing workers and group homes. Young adults (ages 18–24), African-Americans and Hispanics were oversampled. The overall response rate was 81%.
Only 18–30 year olds (mean = 24.1, SD = 3.8, N = 9,535) were included because the present TLI version was developed for young adults. Sample composition was 44.0% male; 71.5% European-American, 19.5% African-American, 4.1% Asian and 3.5% Native American; 27.7% were of Hispanic ethnicity. Personal income of 63.7% of participants was less than $20,000. Twelve or more years of education were completed by 82.7% of participants. Thirty percent were married, 58.6% were never married, 5.9% lived with a partner and 5.4% were divorced or separated.
2.2 Instrumentation
2.2.1 Substance Use Disorders
The Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV (AUDADIS-IV) (Grant et al., 2001) was used for NESARC. Psychometric properties of this structured interview are well-established; reliabilities for lifetime SUDs (used herein), conduct disorder and antisocial personality disorder range from good to excellent (κ > 0.74) (Ruan et al., 2008). In addition to comprehensively characterizing alcohol and drug use, AUDADIS-IV also obtains information about treatment history and parental lifetime SUD (Blanco et al., 2008b; Hasin et al., 2007). Frequencies of using alcohol and each class of illegal drug are queried for the prior 12 months. The illegal drug used most frequently by each participant was analyzed presently. NESARC frequency of use categories were reverse coded such that no use = 0 and daily use = 10.
2.2.2 Eligibility for Randomized Clinical Trials
Blanco et al. (2008b) culled items from the NESARC protocol that are often used to exclude participation in randomized clinical trials of SUD treatment (e.g., comorbid medical condition, low education, unstable employment, marital status). A dichotomous variable reflecting eligibility for clinical trials was derived based on responses to Blanco et al.’s items.
2.2.3 Transmissible SUD Liability
Because discrepant factors impinge on SUD risk at different developmental stages, three TLI versions have been derived: early adolescence (ages 10–12), mid adolescence (ages 14–16) and young adulthood. The same methodology was used to identify and calibrate TLI items, but was conducted separately for different ages of participants enrolled in a prospective study of SUD etiology at the Center for Education and Drug Abuse Research (CEDAR). The CEDAR sample consists of children recruited through proband fathers having either SUD consequent to using illegal drugs (SUD+) or no major adult psychiatric disorder (SUD−) who are being followed through age 30. Based on the multifactorial model of SUD liability and to establish the TLI’s construct validity, items that were tested for inclusion in the TLI were drawn from constructs that previous research demonstrated were associated with SUD risk. Items were further reduced by requiring that they statistically differentiated sons of SUD+ fathers from sons of SUD- fathers, and when subjected to factor and item response theory analyses, loaded onto a single latent construct (Kirisci et al., 2009; Vanyukov et al., 2009). In sum, the young adult TLI consists of 64 items derived from eight self-report assessments1.
One strength of the young adult TLI is it can be replicated in many existing datasets because the items come from widely used instruments. Twenty-four NESARC survey items resembled young adult TLI items (Table 1). Consistent with behavior genetic findings on transmissible risk (Kendler et al., 2003b; Kendler et al., 2003a; King et al., 2004; Knopik et al., 2004; Kreek et al., 2005; van den Bree et al., 1998), these items queried conduct disorder/antisocial personality disorder (12 items) and other illegal or aggressive behavior (2 items), personality traits (6 items), mood (2 items) and anxiety (2 items). Exploratory factor analysis demonstrated that these NESARC items are indicators of a single dimension (e.g., the first three eigenvalues were 10.0, 2.5, and 1.4), replicating results from the CEDAR sample. Methodology studies (e.g., comparisons between scree plot versus eigenvalue ratio test versus Kaiser criterion or eigenvalue>1 rule) suggest only the first factor of the TLI should be considered robust. Factor loadings appear in Table 1.
Table 1.
Original TLI Items and NESARC Items Used to Recreate the TLI
| CEDAR Item Question (Domain) | NESARC Item | Loading | NESARC Item Question |
|---|---|---|---|
| I always seem to have something pleasant to look forward to.A (mood) | S4AQ2 | 0.56 | In your entire life, have you ever had a time, lasting at least 2 weeks, when you didn’t care about the things that you usually cared about, or when you didn’t enjoy the things you usually enjoyed? |
| I find it very easy to enjoy life. A (mood) | S4CQ1 | 0.57 | Have you ever had a time that lasted for at least 2 years when your mood was low, sad or depressed most of the day, more than half of the time? |
| I often prefer not to have people around me. A (anxiety) | S8Q1A6 | 0.41 | Have you ever had a strong fear or avoidance of being in a crowd or standing in a line? |
| S10Q1A1 | 0.51 | Most of the time throughout your life, regardless of the situation or whom you were with, have you avoided jobs or tasks that dealt with a lot of people? | |
| I know that certain people would enjoy it if I got hurt. A (personality) | S10Q1A26 | 0.65 | Do you often have to keep an eye out to keep people from using you, hurting you or lying to you? |
| When people are friendly they usually want something from me. A (personality) | S10Q1A27 | 0.69 | Do you send a lot of time wondering if you can trust your friends or the people you work with? |
| I know that people have purposely spread false rumors about me. A (personality) | S10Q1A28 | 0.66 | Do you find that it is best not to let other people know much about you because they will use it against you? |
| Did you have a bad temper?B (personality) | S10Q1A32 | 0.53 | Do you often get angry or lash out when someone criticizes or insults you in some way? |
| I have runaway C (CD/ASPD) | S11AQ1A4 | 0.59 | Did you ever run away from home overnight at least twice when you were living at home or run away and stay away for a longer time? |
| I am pretty honest C (CD/ASPD) | S11AQ1A11 | 0.70 | Did you ever have a time in your life when you lied a lot, not counting any times you lied to keep from being hurt? |
| Did you do risky or dangerous things a lot? B (personality) | S11AQ1A14 | 0.54 | Did you ever do things that could have easily hurt you or someone else - like speeding or driving after having too much to drink? |
| S11AQ1A15 | 0.38 | Did you ever get more than 3 traffic tickets for reckless or careless driving, speeding, or causing an accident? | |
| I destroy things belonging to others. D (CD/ASPD) | S11AQ1A17 | 0.75 | Did you ever destroy, break, or vandalize someone else’s property - like their car, home or other personal belongings? |
| I fail to pay debts or meet other financial responsibilities.D (CD/ASPD) | S11AQ1A19 | 0.57 | Did you ever fail to pay off your debts - like moving to avoid paying rent, not making payments on a loan or mortgage, failing to make alimony or child support payments or filing for bankruptcy? |
| I have stolen.C (CD/ASPD) | S11AQ1A20 | 0.77 | Did you ever steal anything from someone or someplace when no one was around? |
| S11AQ1A22 | 0.74 | Did you ever shoplift? | |
| I steal.D (CD/ASPD) | S11AQ1A23 | 0.73 | Did you ever rob or mug someone or snatch a purse? |
| Have you made money doing something that was against the law? B (illegal/aggressive) | S11AQ1A24 | 0.76 | Did you ever make money illegally like selling stolen property or selling drugs? |
| I have committed assault.D (CD/ASPD) | S11AQ1A27 | 0.73 | Did you ever get into a lot of fights that you started? |
| Have you gotten into physical fights?B (CD/ASPD) | S11AQ1A28 | 0.60 | Did you ever get into a fight that came to swapping blows with someone like a husband, wife, girlfriend or boyfriend? |
| Assault with a deadly weapon.C (illegal/aggressive) | S11AQ1A29 | 0.76 | Did you ever use a weapon like a stick, knife, or gun in a fight? |
| I physically attack people.D (CD/ASPD) | S11AQ1A30 | 0.70 | Did you ever hit someone so hard that you injured them or they had to see a doctor? |
| S11AQ1A32 | 0.67 | Did you ever physically hurt another person in any other way on purpose? | |
| Did you threaten to hurt people?B (CD/ASPD) | S11AQ1A31 | 0.74 | Did you ever harass, threaten or blackmail someone? |
Note: TLI=Transmissible Liability Index. CEDAR=Center for Education and Drug Abuse Research. NESARC=National Epidemiologic Survey on Alcohol and Related Conditions. Loading=standardized factor loading on the single TLI factor using NESARC data.
Multidimensional Personality Questionnaire (Tellegen 1982).
Dysregulation Inventory (Mezzich et al., 2001).
Andrew Scale of Severity and History of Violence (Andrew, 1974).
Young Adult Self-Report (Achenbach, 1997). CD/ASPD=conduct disorder / antisocial personality disorder.
To confirm that the NESARC-based TLI measures the same construct as the CEDAR-derived TLI, two parallel index scores were created. One index was derived using item parameters (difficulty and discrimination) calibrated from the NESARC sample. The other index utilized item parameters calibrated from the CEDAR sample. As expected, the nearly perfect correlation between these two indexes in the total sample (0.937), males (0.935) and females (0.938) demonstrated they measure the same construct. For the present investigation, TLI scores were derived using the CEDAR item calibration parameters.
2.2.4. Statistical Analyses
Statistical analyses consisted of logistic regression, Kendall’s τ, Spearman’s ρ, Pearson correlation, ANOVA and receiver operating characteristic curves. Effect size of mean differences was evaluated using Cohen’s d, which for two groups corresponds to the number of standard deviations separating them on average (Cohen, 1988). Because analyses utilized 11 different DSM-IV SUD categories, interpretation of results was based on effect sizes rather than p-value adjustment (e.g., Bonferroni correction).
3. Results
3.1 Relationship between TLI and Parent SUD
The TLI is significantly associated with paternal and maternal SUD (Table 2). Odds ratios for predicting a mother/father with an SUD are virtually equal for males and females. The magnitude of these associations also is equivalent to this association in the CEDAR sample, using parent reports of their own SUDs (τ = 0.24; p<0.001; Vanyukov, personal communication). In participants with zero parents having SUD, TLI scores ranged from −0.9 to 4.5 (mean=−0.2, SD=0.88) and predicted participant SUD resulting from alcohol or illegal drug use with odds ratio (OR) = 2.7 (95% C.I.=2.5–2.9). Among participants with two SUD parents, TLI scores ranged from -0.9 to 4.1 (mean=0.9, SD=1.17) and predicted SUD with OR=2.8 (95% C.I.=2.2–3.4).
Table 2.
Associations between TLI and Parental SUD
| Total Sample | Males | Females | |
|---|---|---|---|
| Father AUD (ORs) | 1.8 (1.7–1.8) | 1.9 (1.7–2.0) | 1.7 (1.6–1.8) |
| Mother AUD (ORs) | 2.0 (1.8–2.1) | 2.1 (1.8–2.3) | 2.0 (1.8–2.2) |
| Father SUD (ORs) | 2.2 (2.0–2.3) | 2.3 (2.1–2.6) | 2.1 (1.9–2.3) |
| Mother SUD (ORs) | 2.2 (2.0–2.4) | 2.3 (2.0–2.7) | 2.2 (2.0–2.5) |
| Number of Parents with AUD (τ) | 0.22 | 0.23 | 0.22 |
| Number of Parents with SUD (τ) | 0.21 | 0.21 | 0.22 |
Note: All results reached p<.001. OR=odds ratio per TLI standard deviation increment. τ=Kendall’s tau correlation. Participants reporting they did not know whether a parent had problems related to substance use were omitted. TLI=Transmissible Liability Index. SUD=substance use disorder due to using an illegal drug. AUD=alcohol use disorder.
3.2 Gender, Race/Ethnicity Differences
The mean TLI difference between males (n=4,137) and females (n=5,249) is statistically significant (F = 21.83, p<0.0001), consistent with gender differences in SUD prevalence, although its size is trivial: males mean=0.05 (SD=1.04) and females mean=0.04 (SD=0.97). In contrast, Asians (n=395, mean TLI=−0.28, SD=0.8) and Hispanics (n=2,462, mean TLI=−0.13, SD=1.0) differed significantly from all other race/ethnicity groups (European-Americans (n=4,524) mean TLI=0.07, SD=1.0. African-Americans (n=1,898) mean TLI=0.04, SD=1.0). Compared to Asians, the mean difference is small to medium versus European-Americans (d=0.39) and African-Americans (d=0.36) and small versus Hispanics (d=0.17). Compared to Hispanics, the mean difference is small versus other European-Americans (d=0.20) and African-Americans (d=0.17).
3.3 TLI and SUDs
For each of the 11 DSM-IV classes of drugs, a standard deviation increment in TLI score corresponds to a 2- to 4-fold increase in odds of SUD for men and women (Table 3). This association is greater for SUDs related to illegal drugs than for SUDs resulting from alcohol or tobacco use. Specifically, each TLI standard deviation increment is associated with about 250% increased odds for SUD consequent to using legal drugs (alcohol and tobacco), but a 300% to 400% increased odds for SUD resulting from illegal drug use. To further illustrate the size of this association, participants in the highest TLI quartile had an OR for illicit drug use disorder of 18.3 (95% CI=14.9–22.5) compared to participants in the lowest TLI quartile; the corresponding OR for any SUD (except from tobacco use) was 10.6 (95% CI=9.3–12.0).
Table 3.
Increase in SUD Risk per TLI Standard Deviation Increment
| SUD from use of: | Total Sample | Men | Women | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Alcohol | 2.5 | 2.4 – 2.7 | 2.5 | 2.3–2.7 | 2.6 | 2.4–2.8 |
| Tobacco | 2.3 | 2.2 – 2.5 | 2.2 | 2.1–2.4 | 2.4 | 2.2–2.6 |
|
| ||||||
| Cannabis | 3.0 | 2.8 – 3.2 | 3.0 | 2.7–3.3 | 2.9 | 2.7–3.2 |
| Hallucinogens | 3.4 | 3.0 – 3.8 | 3.2 | 2.7–3.8 | 3.5 | 2.9–4.2 |
| Cocaine | 3.5 | 3.1 – 4.0 | 3.3 | 2.8–3.9 | 3.7 | 3.1–4.5 |
| Inhalants | 3.6 | 2.8 – 4.7 | 3.6 | 2.6–4.9 | 3.6 | 2.4–5.4 |
| Tranquilizers | 3.6 | 3.0 – 4.3 | 3.4 | 2.6–4.0 | 4.1 | 3.0–5.5 |
| Heroin | 4.0 | 2.7 – 6.0 | 3.7 | 2.2–6.0 | 4.6 | 2.3–9.2 |
| Other Opioids | 3.7 | 3.2 – 4.3 | 3.7 | 3.1–4.6 | 3.7 | 2.9–4.6 |
| Stimulants | 3.7 | 3.2 – 4.2 | 3.7 | 3.0–4.5 | 3.7 | 3.1–4.4 |
| Sedatives | 3.8 | 3.1 – 4.6 | 3.2 | 2.5–4.1 | 4.8 | 3.5–6.5 |
Note: N was 4,137 for men and 5,249 for women. The dotted line partitions legal (above) from illegal (below) substances. TLI=Transmissible Liability Index.
SUD=substance use disorder. OR=odds ratio. CI=confidence interval.
3.4 Incremental Validity
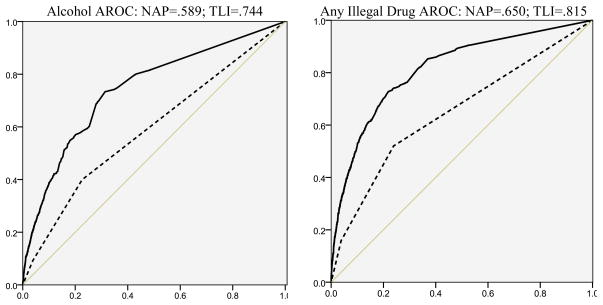
Because so many TLI items in NESARC consist of conduct and antisocial personality disorder criteria (Spearman’s ρ=.76, p<.001 between them and TLI, consistent with past behavior genetic studies; Kendler et al., 2003b; van den Bree et al., 1998), as well as alternative clinical diagnostic measures (e.g., parents with SUD), the incremental validity of the TLI over and above these measures was tested. Compared to number of parents with SUD, TLI scores account for 16% and 17% more of the area under the ROC curve predicting alcohol use disorder and illegal drug use disorder, respectively (Figure 1).
Figure 1.
Receiver Operating Characteristic Curves: TLI vs. Number of Parents with SUD.
Note: AROC = area under the receiver operating characteristic curve. NAP = number of affected parents (with lifetime SUD). TLI = Transmissible Liability Index. SUD=substance use disorder.
Using logistic regression (Table 4), TLI was the largest unconditional predictor of lifetime SUD compared to parental SUD, previous-year SU, and a count of criteria for conduct and antisocial personality disorders. Changes in ORs from unconditional to multivariate logistic regressions demonstrated overlap between TLI scores with parental SUD, conduct disorder/antisocial personality disorder and SU (as expected). Specifically regarding incremental validity, the TLI accounts for significantly more cases of SUD over and above the other predictors and provides the largest conditional OR among all the predictors. Similar results, including ORs, occur when these analyses are repeated using alcohol use disorder or illegal drug SUD in place of any SUD.
Table 4.
Incremental Validity of the TLI, Predicting Lifetime SUD
| Unconditional OR | Model I Conditional OR | Model II: TLI Added Conditional OR | |
|---|---|---|---|
| Paternal SUD | 2.3 (2.12–2.58) | 1.3 (1.14–1.51) | 1.2 (1.09–1.45) |
| Maternal SUD | 3.1 (2.67–3.57) | 1.2 (1.00–1.55) | 1.2 (1.00–1.50) |
| Sum of ASPD and CD Criteria | 1.4 (1.35–1.40) | 1.3 (1.30–1.35) | 1.2 (1.17–1.24) |
| Frequency of Alcohol Use During Prior 12 Months | 1.5 (1.44–1.50) | 1.4 (1.41–1.47) | 1.4 (1.42–1.48) |
| Frequency of Drug Use During Prior 12 Months | 1.6 (1.51–1.61) | 1.3 (1.25–1.35) | 1.3 (1.25–1.35) |
| Transmissible Liability Index | 2.8 (2.64–2.93) | - - | 1.5 (1.37–1.68) |
|
| |||
| −2 Log Likelihood Fit | 6,930.501 | 6,866.628 | |
| Likelihood Ratio χ2 | N / A | 63.873, 1df, p<0.001 | |
| Cox & Snell R2 | 0.357 | 0.362 | |
| Nagelkerke R2 | 0.502 | 0.509 | |
Note: TLI=Transmissible Liability Index. OR=odds ratio. Conditional=controlling statistically for all other predictors in the model. CI=confidence interval. SUD=substance use disorder resulting from use of alcohol, inhalants or an illegal drug, but not tobacco. ASPD=antisocial personality disorder. CD=conduct disorder. Parenthetical values are 95% confidence intervals.
R2 statistics for logistic regression are not interpreted as proportion of variance accounted for, but rather as relative indicators of fit to the data (larger coefficients represent better fit).
Compared to Model I (omission of TLI as a predictor), when the TLI is added (thereby parsing out the effect of TLI items which are conduct and antisocial personality criteria), the conditional ORs decrease for paternal SUD (NS) and sum of criteria for conduct and antisocial personality disorders (p<.05), but not for frequency of SU in the past 12 months, indicating that significant variance in the former three predictors are due to (a) paternal transmissible factors as well as (b) other factors. This finding is further born out by the significantly decreased TLI OR from the bivariate association to the conditional model.
3.5 Age of Onset
The original TLI (ages 10–12) was derived to measure transmissible SUD risk prior to SU initiation. Young adult TLI scores also correlate with both younger SU initiation as well as SUD onset for all substances (Table 5). In effect, greater transmissible SUD liability correlates with earlier age of SU onset.
Table 5.
Pearson Correlations between TLI and Age of First SU or First SUD
| Alcohol | Nicotine | Cannabis | Sedative | Opioid | Tranquilizer | Amphetamine | Cocaine | Hallucinogen | Inhalant | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age of First SU | −.25 | −.25 | −.28 | −.28 | −.15 | −.18 | −.28 | −.26 | −.19 | −.29* |
| Age of First SUD | −.20 | −.23 | −.16 | −.21* | −.15 | −.21 | −.16 | −.17 | −.20 | −.25 |
Note: All p-values < .01 unless otherwise noted.
p<.10 due to small number of participants (n) providing the variable. TLI = Transmissible Liability Index. SUD = substance use disorder. N for age of heroin use was too small to obtain correlations.
3.6 Results within Clinical Populations
Table 6 presents associations between the TLI and treatment for SUD among those with a lifetime SUD. Each TLI standard deviation increment corresponds to a 2- to 4-fold increase in the odds of receiving SUD treatment as well as 60% reduced probability of attempting SUD recovery without treatment. TLI scores are more strongly related to treatment utilization to recover from an illegal drug SUD than an alcohol SUD.
Table 6.
Associations between TLI Standard Deviation Increment and Services Used Because of SUD
| Treatment Service | Alcohol | Illegal Drugs | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Any Intervention | 1.7 | 1.5–1.9 | 2.2 | 1.9–2.6 |
| 12 Step Program* | - - | - - | 1.8 | 1.6–2.1 |
| Family or Social Service Agency | 1.9 | 1.5–2.4 | 2.2 | 1.6–3.0 |
| Detoxification | 2.0 | 1.6–2.5 | 2.4 | 1.9–3.1 |
| Inpatient Ward | 3.3 | 2.5–4.2 | 2.3 | 1.8–3.0 |
| Outpatient Clinic | 2.2 | 1.8–2.7 | 2.5 | 2.0–3.2 |
| Rehabilitation | 1.9 | 1.6–2.3 | 2.5 | 2.0–3.1 |
| Emergency Room | 2.8 | 2.2–3.5 | 2.1 | 1.6–2.9 |
| Halfway House | 2.0 | 1.3–3.1 | 2.4 | 1.4–4.0 |
| Crisis Center | 2.2 | 1.3–3.8 | 2.1 | 1.1–4.1 |
| Clergy, Priest or Rabbi | 2.3 | 1.7–3.0 | 2.1 | 1.5–3.0 |
| Private Professional | 2.5 | 2.0–3.0 | 2.1 | 1.7–2.5 |
| Try to Quit on Own | 0.4 | 0.3–0.5 | 0.4 | 0.3–0.5 |
Note: All results reached p<.001. n = 2,967; persons qualifying for any SUD resulting from use of alcohol or an illegal drug. TLI = Transmissible Liability Index. SUD = substance use disorder. OR=odds ratio. CI=confidence interval.
12 Step program was not queried separately for alcohol vs. illegal drugs.
Persons meeting traditional exclusion criteria for randomized clinical trials had greater TLI scores (mean=0.37, SD=1.19) than eligible persons (mean=−0.12, SD=0.9) (F=440.14, p<0.0001). This difference is medium sized (d=0.47), suggesting that persons with greater transmissible SUD risk are systematically excluded from clinical trials of SUD treatments.
Table 7 results serve two purposes. First, they test the TLI validity within persons eligible for treatment (i.e., those with an alcohol or illegal drug SUD) (first two columns), providing validity estimates specifically for clinical populations. Second, they test whether TLI validity differs by eligibility for clinical trials (last four columns). Even among those with SUD, the TLI is highly associated with SUDs, except alcohol use disorder. Moreover, these associations generalize across eligibility for SUD clinical trials, suggesting the TLI quantifies SUD liability even among subgroups of persons with an SUD.
Table 7.
SUD Risk per TLI Standard Deviation Increment Among Persons Needing SUD Treatment
| SUD resulting from use of: | Total Subsample (n=2,967) | Eligible for RCT (n=1,891) | Ineligible for RCT (n=1,076) | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Alcohol | 1.0 | 0.9–1.1 | 0.8 | 0.7–1.0 | 1.1 | 0.9–1.3 |
| Tobacco | 1.7 | 1.6–1.9 | 1.6 | 1.4–1.8 | 1.8 | 1.6–2.0 |
| Cannabis | 1.8 | 1.7–2.0 | 1.7 | 1.5–1.9 | 1.9 | 1.7–2.2 |
| Hallucinogens | 2.3 | 2.0–2.6 | 2.3 | 1.9–2.8 | 2.0 | 1.7–2.4 |
| Cocaine | 2.4 | 2.1–2.7 | 2.1 | 1.7–2.6 | 2.3 | 1.9–2.8 |
| Inhalants | 2.6 | 2.0–3.4 | 3.1 | 1.8–5.3 | 2.0 | 1.5–2.8 |
| Tranquilizers | 2.5 | 2.1–3.0 | 2.6 | 2.0–3.8 | 2.1 | 1.6–2.7 |
| Other Opioids | 2.6 | 2.2–3.1 | 2.4 | 1.9–3.2 | 2.4 | 1.9–3.0 |
| Stimulants | 2.5 | 2.1–3.0 | 2.1 | 1.7–2.7 | 2.5 | 2.0–3.1 |
| Sedatives | 2.7 | 2.2–3.3 | 3.3 | 2.1–5.0 | 2.1 | 1.6–2.6 |
| Heroin | 2.9 | 1.9–4.5 | 2.2 | 1.1–4.3 | 3.9 | 2.0–7.8 |
Note: Sample consists of persons qualifying for any SUD from using alcohol or an illegal drug. SUD=substance use disorder. RCT=randomized clinical trial. TLI=Transmissible Liability Index. OR=odds ratio. CI=confidence interval.
4. Discussion
This investigation elucidated associations between transmissible SUD risk and SUD diagnoses, treatment and independent recovery attempts in a sample representative of the U.S. general population. TLI scores accounted for greater variation in SUD risk compared to number of parents with lifetime SUD. Odds for each SUD increased 2- to 4-fold per standard deviation increment in TLI scores. TLI scores provided the largest unique prediction of SUD when included in the same logistic model as parental SUD, SU and psychiatric antisocial symptoms. TLI scores also were highly associated with younger-age initiation of SU and onset of SUD, suggesting the TLI may be useful for identifying a high-risk group in need of prevention. If, in applied settings the TLI could identify youth at high risk for SUD, perhaps an effective tailored prevention for such youth could sizably reduce SUD (Ridenour et al., 2009; Yoon et al., 2002) and lead to substantial cost savings to society due to reductions in criminal behavior, incarceration and SUD treatment (Spoth et al., 2002).
The size of TLI association with SUD is smaller for disorders consequent to using alcohol/tobacco than illegal drugs, demonstrating that the TLI measures not only risk shared by all substances but also transmissible risk that is specific to SUD consequent to using illegal drugs. This result is consistent with the theory and methods of TLI derivation as a measure of transmissible SUD risk related to using illegal drugs, which shares substantial genetic and environmental variance with risk for addiction to legal drugs (Kendler et al., 2007). These results also confirm prior findings in the CEDAR sample (Kirisci et al., 2009; Vanyukov et al., 2009).
4.1 TLI Uses
One use for the TLI is improved selection of participants for SUD etiology research, including genetic studies (Conway et al., 2010). Not only could youth and young adults be selected from families with numerous relatives who have an SUD, but levels of transmissible risk among siblings could be differentiated. A second use for the TLI is improved identification of homogenous subgroups of SUD patients for clinical trials. Evidence suggests that SUD patients with high transmissible risk differ from others in ontogeny, prognosis and treatment needs (Clark et al., 2005; Leggio et al., 2009) as well as treatment responsivity (Milne et al., 2009; Blanco et al., 2008; Yoon et al., 2002). Use of the TLI in SUD clinical trials could expand the research and applied implications drawn from such studies. For example, the TLI identifies persons who are systematically excluded from SUD clinical trials and is associated with using services for SUD treatment. It could therefore improve translation of SUD clinical trial results (and identify gaps in such studies) for clinical settings. Moreover, inasmuch as transmissible risk delineates SUD patient typologies (Clark et al., 2005; Leggio et al., 2009), finer quantification of the full range of transmissible risk may improve such subtyping. As demonstrated herein, such TLI research can utilize secondary analysis of extant data.
The TLI also could be used to screen for high risk youth (starting at ages 10–12) in need of targeted prevention (Arria et al., 2009; Kirisci et al., 2009; Vanyukov et al., 2009; Ridenour et al., 2009). Again, datasets exist to test the TLI’s utility for prevention contexts. Yoon et al. (2002) specify several practical ways in which a measure of transmissible risk could enhance prevention and public health interventions, including identification of homogenous subgroups for tailoring interventions.
4.2 Study Limitations
One study limitation is that number of parents with an SUD was based on offspring report. More rigorous measurement would utilize parent reports of their own SUDs (although similar results were found with parent self-reports as noted earlier). Using cross-sectional data also is a limitation (e.g., relying on retrospective recall); although prospective data such as results from other TLI studies (Arria et al., 2009; Kirisci et al., 2009; Vanyukov et al., 2009) demonstrate the implied directionality in associations.
Because racial/ethnic groups and genders statistically differed on mean TLI scores, these differences should be clarified and, if measurement biases are found, accounted for in TLI scoring algorithms. Further research on clinical SUD samples or youth at-risk for SUD could better specify applied uses for the TLI. The TLI accounts for paternal transmissible SUD risk; the corresponding contribution of maternal transmissible risk (and overlap between the two sources) remains unknown. Finally, results from these cross-sectional, partially retrospective recall data need to be replicated using young adult’s TLI scores to longitudinally predict SUD outcomes.
4.3 Future Steps
An important next step for TLI development involves preparation for clinical use. A beta version of a computer adaptive test for the age 10–12 TLI shortens administration time to 5.0 minutes on average. The preliminary correlation between this computer adaptive version and the full TLI is 0.88 (Kirisci, personal communication). In addition to psychometrics, it will be important to document its acceptability to clinicians and persons completing the TLI. The TLI’s longitudinal prediction of SUD has been determined in etiological data (Arria et al., 2009; Kirisci et al., 2009; Vanyukov et al., 2009). Even so, it will be critical to learn how well baseline TLI scores forecast outcomes of SUD medication, psychosocial treatment and preventive intervention to clarify its optimal clinical uses.
For instance, the primary purpose for derivation of SUD typologies is to improve matching of SUD patients to a treatment that is most likely to be effective (Leggio et al., 2009). In nearly every typology derived to date, subgroups are distinguished partly by familial load whereas the present data demonstrate that familial risk is not categorical but continuous. Accordingly, typologies which include familial risk are likely to more effectively differentiate subgroups of SUD patients using thresholds on a continuum of transmissible risk which are associated with clinical outcomes. It also will be important to detail overlapping and unique characteristics that are useful for subtyping compared to the TLI (e.g., conduct and antisocial personality disorders criteria).
Explication of the lower mean TLI scores among Asians and Hispanics on average compared to the other races/ethnicities is needed. In separate studies of samples not drawn from the general population, TLI scores in 10–12 year old African-Americans did not predict their future SUDs and were on average greater than in European-Americans (TLI scores did predict SUDs by early adulthood in the latter group) (Arria et al., 2009; Vanyukov et al., 2009). Although a mean TLI difference is not synonymous with differential functioning between groups, confirmation that TLI psychometrics generalize to races and ethnicities other than European-Americans is required. If the only race/ethnic difference is the average level of transmissible SUD risk (e.g., rather than TLI validity), learning how familial aggregation of SUD differs in Asians and Hispanics compared to European Americans might unveil moderators of transmissible SUD risk, which in turn may provide clues for improving prevention in other racial/ethnic groups.
To summarize, the TLI was more informative of transmissible SUD risk than the traditional count of parents with a lifetime SUD as well as externalizing disorder symptoms. Greater TLI scores were associated with (a) early signs of problematic SU, specifically younger-age SU initiation and onset of SUD, (b) use of professional services to treat SUDs and (c) greater likelihood of exclusion from clinical trials for SUD treatments. Regardless of how clinical relevance of TLI scores was tested, large associations were observed. The TLI could be used with extant datasets, to join multiple datasets for consequent gain in both analytic power and potential sophistication of research questions, for research on differential responsivity of subgroups to SUD treatment, to identify youth at high SUD risk in need of prevention, for clinical uses such as intervention prognosis as well as in etiology (particularly genetic) research.
Supplementary Material
Footnotes
Supplementary material for this article can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
The self-report items can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM. Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. Department of Psychiatry, University of Vermont; Burlington, VT: 1997. [Google Scholar]
- Andrew JM. Violent crime inclines among community-retained delinquents. Crimin Justice Behav. 1974;1:123–130. [Google Scholar]
- Arria AM, Vincent KB, Caldeira KM. Measuring liability for substance use disorder among college students: implications for screening and early intervention. Am J Drug Alcohol Abuse. 2009;35:233–241. doi: 10.1080/00952990903005957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierut LJ, Madden PA, Breslau N, Johnson EO, Hatsukami D, Pomerleau OF, Swan GE, Rutter J, Bertelsen S, Fox L, Fugman D, Goate AM, Hinrichs AL, Konvicka K, Martin NG, Montgomery GW, Saccone NL, Saccone SF, Wang JC, Chase GA, Rice JP, Ballinger DG. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum Mol Genet. 2007;16:24–35. doi: 10.1093/hmg/ddl441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Olfson M, Okuda M, Nunes EV, Liu SM, Hasin DS. Generalizability of clinical trials for alcohol dependence to community samples. Drug Alcohol Depend. 2008a;98:123–128. doi: 10.1016/j.drugalcdep.2008.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, Olfson M. Mental health of college students and their non-college-attending peers. Arch Gen Psychiatry. 2008b;65:1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boomsma DI, Molenaar PC, Orlebeke JF. Estimation of individual genetic and environmental factor scores. Genet Epidemiol. 1990;7:83–91. doi: 10.1002/gepi.1370070115. [DOI] [PubMed] [Google Scholar]
- Boomsma DI, Molenaar PC, Dolan CV. Estimation of individual genetic and environmental profiles in longitudinal designs. Behav Genet. 1991;21:243–55. doi: 10.1007/BF01065818. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Arch Gen Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Clark DB, Cornelius JR, Kirisci L, Tarter RE. Childhood risk categories for adolescent substance involvement: a general liability typology. Drug Alcohol Depend. 2005;77:13–21. doi: 10.1016/j.drugalcdep.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Lawrence Erlbaum; Hillsdale, NJ: 1998. [Google Scholar]
- Compton WM, Cottler LB, Ridenour TA, Ben-Abdallah A, Spitznagel EL. The specificity of family history of alcohol and drug abuse in cocaine abusers. Am J Addict. 2002;11:85–94. doi: 10.1080/10550490290087866. [DOI] [PubMed] [Google Scholar]
- Conway KP, Levy J, Vanyukov M, Chandler R, Rutter J, Swan GE, Neale M. Measuring addiction propensity and severity: the need for a new instrument. Drug Alcohol Depend. 2010;111:4–12. doi: 10.1016/j.drugalcdep.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Foroud T. Candidate genes for alcohol dependence: a review of genetic evidence from human studies. Alcohol Clin Exp Res. 2003;27:868–879. doi: 10.1097/01.ALC.0000065436.24221.63. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Arch Gen Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Iacono WG, McGue M. Index of the transmissible common liability to addiction: heritability and prospective associations with substance abuse and related outcomes. Addiction. doi: 10.1016/j.drugalcdep.2011.12.017. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. Am J Psychiatry. 2003a;160:687–695. doi: 10.1176/appi.ajp.160.4.687. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Myers J, Prescott CA. Specificity of genetic and environmental risk factors for symptoms of cannabis, cocaine, alcohol, caffeine, and nicotine dependence. Arch Gen Psychiatry. 2007;64:1313–1320. doi: 10.1001/archpsyc.64.11.1313. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003b;60:929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kirillova GP, Vanyukov MM, Kirisci L, Reynolds M. Physical maturation, peer environment, and the ontogenesis of substance use disorders. Psychiatr Res. 2008;158:43–53. doi: 10.1016/j.psychres.2007.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirisci L, Tarter R, Mezzich A, Ridenour T, Reynolds M, Vanyukov M. Prediction of cannabis use disorder between boyhood and young adulthood: clarifying the phenotype and environtype. Am J Addict. 2009;18:36–47. doi: 10.1080/10550490802408829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knopik VS, Heath AC, Madden PAF, Bucholz KK, Slutske WS, Nelson EC, Statham D, Whitfield JB, Martin NG. Genetic effects on alcohol dependence risk: re-evaluating the importance of psychiatric and other heritable risk factors. Psychol Med. 2004;34:1519–1530. doi: 10.1017/s0033291704002922. [DOI] [PubMed] [Google Scholar]
- Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- Leggio L, Kenna GA, Fenton M, Bonenfant E, Swift RM. Typologies of alcohol dependence. From Jellinek to genetics and beyond. Neuropsychol Rev. 2009;19:115–129. doi: 10.1007/s11065-008-9080-z. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Li JJ, Stipelman B, Yu K, Fucito L, Swendsen J, Zhang H. The familial aggregation of cannabis use disorders. Addiction. 2009;104:622–629. doi: 10.1111/j.1360-0443.2008.02468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezzich AC, Tarter RE, Giancola PR, Kirisci L. The Dysregulation Inventory: a new scale to assess the risk for substance use disorder. J Child Adolesc Subst Abuse. 2001;10:35–43. [Google Scholar]
- Milne BJ, Caspi A, Harrington H, Poulton R, Rutter M, Moffitt TE. Predictive value of family history on severity of illness: the case for depression, anxiety, alcohol dependence, and drug dependence. Arch Gen Psychiatry. 2009;66:738–47. doi: 10.1001/archgenpsychiatry.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurnberger JI, Jr, Wiegand R, Bucholz K, O’Connor S, Meyer ET, Reich T, Rice J, Schuckit M, King L, Petti T, Bierut L, Hinrichs AL, Kuperman S, Hesselbrock V, Porjesz B. A family study of alcohol dependence: coaggregation of multiple disorders in relatives of alcohol-dependent probands. Arch Gen Psychiatry. 2004;61:1246–1256. doi: 10.1001/archpsyc.61.12.1246. [DOI] [PubMed] [Google Scholar]
- Poirier MF, Laqueille X, Jalfre V, Willard D, Bourdel MC, Fermanian J, Olié JP. Clinical profile of responders to buprenorphine as a substitution treatment in heroin addicts: results of a multicenter study of 73 patients. Prog Neuropsychopharmacol Biol Psychiatr. 2004;28:267–72. doi: 10.1016/j.pnpbp.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Rice JP, Cloninger CR, Reich T. General causal models for sex differences in the familial transmission of multifactorial traits: an application to human spatial visualizing ability. Soc Biol. 1980;26:36–47. doi: 10.1080/19485565.1980.9988401. [DOI] [PubMed] [Google Scholar]
- Ridenour TA, Clark DB, Cottler LB. The illustration-based Assessment of Liability and Exposure to Substance use and Antisocial behavior© for children. Am J Drug Alcohol Abuse. 2009;35:242–252. doi: 10.1080/00952990902998715. [DOI] [PubMed] [Google Scholar]
- Ridenour TA, Stormshak EA. Introduction and rationale for individualized substance abuse prevention from an ontogenetic perspective. Am J Drug Alcohol Abuse. 2009;35:206–208. doi: 10.1080/00952990903005924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA, Tarter RE, Reynolds MD, Mezzich A, Kirisci L, Vanyukov MM. Neurobehavior disinhibition, parental substance use disorder and neighborhood quality on development of cannabis use disorder in boys. Drug Alcohol Depend. 2009;102:71–77. doi: 10.1016/j.drugalcdep.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huan B, Stinson RS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer HJ, LaPlante DA, LaBrie RA, Kidman RC, Donato AN, Stanton MV. Toward a syndrome model of addiction: multiple expressions, common etiology. Harv Rev Psychiatry. 2004;12:367–374. doi: 10.1080/10673220490905705. [DOI] [PubMed] [Google Scholar]
- Spoth RL, Guyll M, Day SX. Cost-effectiveness and cost-benefit analyses of two interventions. J Stud Alcohol. 2002;63:219–228. doi: 10.15288/jsa.2002.63.219. [DOI] [PubMed] [Google Scholar]
- Tellegen A. A manual for the Differential Personality Questionnaire. Unpublished manuscript 1982 [Google Scholar]
- Tsuang MT, Lyons MJ, Meyer JM, Doyle T, Eisen SA, Goldberg J, True W, Lin N, Toomey R, Eaves L. Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities. Arch Gen Psychiatry. 1998;55:967–972. doi: 10.1001/archpsyc.55.11.967. [DOI] [PubMed] [Google Scholar]
- Uhl GR, Liu QR, Naiman D. Substance abuse vulnerability loci: converging genome scanning data. Trends Genet. 2002;18:420–425. doi: 10.1016/s0168-9525(02)02719-1. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Kirisci K, Moss L, Tarter RE, Reynolds MD, Maher BS, Kirillova GP, Ridenour TA, Clark DB. Measurement of the risk for substance use disorders: phenotypic and genetic analysis of an index of common liability. Behav Genet. 2009;39:233–244. doi: 10.1007/s10519-009-9269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Bree MBM, Svikis DS, Pickens RW. Genetic influences in antisocial personality and drug use disorders. Drug Alcohol Depend. 1998;49:177–187. doi: 10.1016/s0376-8716(98)00012-x. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Kirisci L, Tarter RE, Simkevitz HF, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 2. a measurement approach. Neurosci Biobehav Rev. 2003a;27:517–526. doi: 10.1016/j.neubiorev.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Vanyukov M, Moss H, Tarter R. Research designs in family studies. In: Sloboda Z, Bukowski WJ, editors. Handbook of Drug Abuse Prevention: Theory, Science and Practice. Kluwer Academic/Plenum Publishers; New York: 2003b. pp. 497–519. [Google Scholar]
- Vanyukov MM, Tarter RE, Kirisci L, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 1. common mechanisms and manifestations. Neurosci Biobehav Rev. 2003;27:507–515. doi: 10.1016/j.neubiorev.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Yoon PW, Scheuner MT, Peterson-Oehike KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med. 2002;4:304–310. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.