Abstract
OBJECTIVES
Identifying predictors of late-life depression that are amenable to change may lead to interventions that result in better and faster remission. Thus, authors investigated the impact of two different strategies for coping with physical illness on depression in older, primary care patients. Health-oriented goal engagement strategies involve the investment of cognitive and behavioral resources to achieve health goals. Conversely, disengagement strategies involve the withdrawal of these resources from obsolete or unattainable health goals, combined with goal restructuring.
METHODS
Participants were 271 adults aged >59 who took part in a two-year randomized clinical trial for treating depression in the elderly (PROSPECT -- Prevention of Suicide in Primary Care Elderly: Collaborative Trial). The use of engagement and disengagement strategies, along with other risk factors for depression, were included in a tree-structured survival analysis to identify subgroups of individuals at risk for not achieving depression remission.
RESULTS
Greater use of disengagement strategies predicted earlier remission of depression, particularly among more severely depressed elderly. Use of engagement strategies did not predict earlier remission.
CONCLUSION
Interventions that encourage disengagement from unattainable health goals may promote remission from depression in older, primary care patients.
Keywords: aging, depression, health, control
INTRODUCTION
Late-life depression is a disabling condition associated with premature deaths from suicide and cardiovascular illness (Bruce et al., 2004). Factors such as anxiety, insomnia, hopelessness, cognitive impairment, lack of social support and physical disability are known to impede remission from depression in old age (Alexopoulos et al., 2005; Dombrovski et al, 2007; Andreescu et al., 2007; Reynolds et al., 2006; Buysse et al., 1996). These factors, however, are often hard to modify. Thus, if the clinical objective is to achieve a better and faster remission from depression in old age, it would be useful to find predictors of remission that are amenable to change.
The use of control strategies aimed at overcoming health problems is a factor potentially associated with late-life depression that may also be modifiable (Gitlin et al., 2006a, 2006b). The lifespan theory of control (Heckhausen and Schulz, 1993, 1995; Schulz and Heckhausen, 1996; Heckhausen et al., 2010) suggests that efforts to actively alter one’s environment and adapt to life changes psychologically are important for successful aging. It identifies two types of control strategies, those that serve goal engagement functions (e.g., investing time and effort in goal pursuit, increasing motivational commitment) and those that serve goal disengagement functions (e.g., downgrading the importance of a goal, enhancing the value of alternative goals), as critical to successful aging.
Engagement strategies are most advantageous when pursuing attainable goals and have been shown to reduce depressive symptomology in older adults (Wrosch et al., 2002; Gitlin et al., 2007). Alternatively, disengagement strategies are important once goals are no longer attainable; these strategies help to maintain subjective well-being by protecting the individual from the negative effects of failure as well as preserving motivational resources of the individual (Wrosch et al., 1999, 2000, 2003).
Clinically, interventions informed by the theory of control have been shown not only to preserve and enhance individuals’ motivation to stay engaged in important and attainable life goals, but also to improve functional outcomes in disabled community-dwelling elderly (Gitlin et al., 2006a, 2006b). While the use of engagement and disengagement strategies has been shown to predict better mood in older adults in general (Wrosch et al., 2002; Gitlin et al., 2007), studies of these strategies in clinical depression are lacking. Thus, the aim of the present study is to investigate the impact of control strategies on late life depression, and specifically, whether the use of control strategies predicts depression remission in this population. If this were true, interventions aimed at enhancing control strategy use could be developed to promote recovery from depression in older adults.
Data from a large randomized controlled trial of depression management in primary care designed to reduce depressive symptoms and suicidal ideation (Bruce et al., 2004) are used to address the study aims. To account for the numerous factors associated with depression while still presenting clinically meaningful findings, the authors utilized tree-structured methods for characterizing baseline depression severity and predicting time to depression remission. The models developed through tree-structured methods can guide intervention development by identifying subgroups of individuals for whom the use of health-oriented control strategies would be particularly beneficial (Kiernan et al., 2001).
METHODS
The PROSPECT Clinical Trial
PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial) was aimed at reducing depressive symptoms and suicidal ideation in older, primary care adults through a depression care manager intervention (Bruce et al., 2004). Two-stage depression screening resulted in a representative sample of primary care participants aged 60 and older from 20 practices in greater New York City, Philadelphia and Pittsburgh regions. Practices were paired by region, affiliation, size and population type. Within these pairs, practices were randomly assigned to either the depression care manager intervention or enhanced usual care.
The final cohort included 599 depressed individuals with either major or minor depression, as defined by the DSM-IV modified by requiring four depressive symptoms, a 24-item Hamilton Rating Scale for Depression (HRSD-24) score of ten or higher and duration of at least four weeks. The detailed flow of participants was reported by Bruce et al.(2004). Participants were observed at baseline, four, eight, 12, 16 and 24 months. The institutional review boards oversaw the study at the respective universities. All participants provided informed consent.
The depression care manager intervention focused on two major components of care: physician knowledge and treatment management. For the physician knowledge component, physicians were advised to use a prescribed treatment algorithm that included the recommendation of an SSRI and interpersonal therapy. For the treatment management component, depression care managers collaborated with physicians to help them recognize depression, monitored the patients’ progress and provided interpersonal psychotherapy to patients who refused medication. “Usual care” was enhanced by educating physicians about the treatment guidelines and notifying them when a patient met criteria for a depression diagnosis (Bruce et al., 2004).
Predictor and Outcome Measures
Use of health-oriented engagement and disengagement control strategies was measured with the Optimization in Primary and Secondary Control survey (Schulz and Heckhausen, 1998), shown in Table 1. Given a 5-point scale, participants were asked to indicate to what extent a statement applied to them. Possible answers ranged from 1 (“almost never true”) to 5 (“almost always true”). With respect to health-oriented goals, four engagement items assessed the investment of internal behavioral resources (“I put in more effort to get better”), recruitment of external resources (“I try to get as much advice as I can”) and use of cognitive strategies to maintain motivation (“I avoid things that could distract me”). Four disengagement items assessed the ability to withdraw from unattainable health goals (“I focus on other important things in my life”) and preserve motivational resources when faced with health difficulties, which includes the use of strategic social comparison (“other people are worse off than I am”) and external attributions for failure (“I am not to blame for it”). Total engagement and disengagement scores were prorated for individuals missing one or two items. The Chronbach alphas for the disengagement and engagement subscales in PROSPECT were .51 and .67, respectively.
Table 1.
Health Engagement (E) and Disengagement (D) Strategies Scale
|
Additional covariates were selected based on previously identified relationships with either depression or use of health-oriented control strategies (Bruce et al., 2004; Alexopoulos et al., 2005; Dombrovski et al., 2007; Andreescu et al., 2007; Reynolds et al. 2006; Wrosch et al., 2000, 2002, 2003; Gitlin et al., 2007; Wrosch and Heckhausen, 1999). These covariates were anxiety measured by the Clinical Anxiety Scale (CAS) (Snaith et al., 1982), hopelessness measured by the Beck Hopelessness Scale (BHS) (Beck et al., 1975), cognitive impairment measured by the Mini Mental State Exam (MMSE) (Folstein et al., 1975), burden of physical illness measured by the Charlson Comorbidity Index (CCI) (Charlson et al., 1987), diagnosis of major depressive disorder, intervention assignment and other demographic characteristics. The Kuder-Richardson internal reliability of the BHS has been reported as ranging from .82 to .93 in psychiatric populations (Beck and Steer, 1988). The Chronbach alpha for the CAS has been reported as .94 in a combined psychiatric and non-psychiatric adult population (Westhuis and Thyer, 1989).
Outcome measures were baseline depression severity and time to first depression remission. In the original PROSPECT analyses (Bruce et al., 2004; Alexopoulos et al., 2005), the HRSD-24 measured depression severity, with a cutoff of HRSD-24 < 10 used to detect depression remission. The HRSD-24 intraclass correlation coefficient under a random effects model of assessors across the three PROSPECT sites was 0.97 (Bruce et al., 2004).
In the present analyses, the authors used hopelessness and anxiety as covariates due to earlier studies that suggested they have prognostic value. Although it is recognized that hopelessness and anxiety are part of the depressive syndrome, the HRSD-24 had to be modified to avoid tautology. Thus, two anxiety items and one hopelessness item were removed to create a modified 21-item Hamilton Rating Scale for Depression (HRSD-21m). Depression remission was defined as the first time a participant had an HRSD-21m score lower than eight. The HRSD-21m was prorated for participants missing individual scale items.
Participants
Three hundred and six participants answered at least six of eight questions on the control strategies questionnaire at baseline. This sample of 306 differed from the original PROSPECT sample of 599 with respect to the proportion of individuals from each region (Χ2 = 68.21, df = 2, p < .01) and the proportion of white individuals (Χ2 = 11.896, df = 1, p < .01). Specifically, this study’s sample had a larger proportion of individuals from Pittsburgh, where collecting control strategy data was given greater priority, and a larger proportion of white individuals. The authors excluded 35 individuals with suspected dementia as indicated by a score of MMSE < 24 because they were not able to reliably report on the use of control strategies. Thus, 45.2% (N=271) individuals contributed to the baseline analyses. When modeling time to first depression remission, the authors excluded 37 individuals with either HRSD-21m < 8 at baseline (as a result of a decline in depression severity from screening to baseline) or no HRSD-21m follow-up measurements.
Tree-Structured Methodology
Tree-structured methodology is a statistical technique that identifies a set of homogenous subgroups based on a combination of observed risk factor levels. Several benefits led the authors to select it as the primary method of analysis. First, the final tree model only includes covariates and their interactions that have been empirically identified as important for distinguishing subgroups. Second, the tree model can identify subgroups of at-risk individuals for whom an intervention could be particularly beneficial. Third, the model can be used to easily classify new patients into risk groups, thereby more directly informing clinical management.
Tree-structured methodology creates a set of homogenous subgroups by recursively splitting a sample into distinct subsamples, two at a time. For any given subsample, or node, each observed value on every possible covariate is a potential binary split. A statistic is selected to measure the reduction in deviance (i.e., unexplained error) resulting from a potential split. The authors used a measure of least squares deviance for modeling baseline depression and a measure of full exponential likelihood deviance for modeling time to depression remission. Splits that reduce larger amounts of unexplained error will create more distinct subgroups. Thus, the split that results in the largest reduction in error is the one that divides the parent node into two child nodes. This iterative detection and initiation of binary splits continues until either a pre-specified node size has been reached or all the observations in a node are equivalent.
Because the resulting tree model can often be quite large, it is typically pruned it to a more parsimonious and clinically meaningful size. Pruning a tree model requires one to select a pre-specified complexity parameter, which is used as a penalty for adding more splits to the tree. After pruning, any nodes that are not split are called terminal nodes and are considered to be the final subgroups with respect to the outcome of interest. Further details regarding the creation and pruning of tree-structured regression and survival trees are presented elsewhere (Breiman et al., 1984; LeBlanc and Crowley, 1992).
Analysis Plan
To verify that the effects of engagement and disengagement strategies were not confounded with other known predictors, including hopelessness and anxiety, the authors calculated Pearson partial correlations adjusting for baseline depression severity. Univariate regression analyses were used to identify possible correlates of baseline depression severity. Sensitivity analyses omitting a valid yet outlying data point and using a log transformation of the dependent variable to improve residual plots in some models resulted in no changes in inference. Thus, results from the analyses including the entire cohort were reported.
To explore multivariate associations at baseline, the use of engagement and disengagement strategies, age, gender, education, race, living status, anxiety, hopelessness, burden of physical illness and mental functioning were used as possible covariates in the tree-structured regression model for baseline depression severity.
For the primary outcome of interest (time to first depression remission), univariate Cox proportional hazards models were first used to identify possible correlates of time to depression remission. To explore multivariate associations with time to depression remission, the covariates used in the baseline analysis, as well as intervention assignment, diagnosis of major depressive disorder and baseline depression severity, were included as possible predictors in the tree-structured survival model. The authors required at least 30 observations in each child node and used a complexity parameter of .018 to prune the tree in an effort to avoid overfitting and to keep the model as clinically meaningful as possible. To accommodate eight missing covariate values for the BHS and two individuals with missing major or minor depression diagnoses, the authors incorporated surrogate splitting, discussed by Therneau, et al. (1997). Finally, multivariate Cox proportional hazards models were used to further evaluate the relationships between use of control strategies and time to depression remission after controlling for age, gender, intervention assignment, and level of physical illness.
The statistical program R version 2.9 (R Foundation for Statistical Computing, Vienna, Austria) with the rpart package (Therneau et al., 2008) was used to fit the tree-structured models. SAS version 9.2 (SAS Institute, Inc., Cary, NC) was used for all other analyses.
RESULTS
Baseline Characteristics
Participant characteristics at baseline are displayed in Table 2. Pearson partial correlations adjusting for baseline depression severity showed that engagement was not related to either anxiety (r = −.03, p = .59) or hopelessness (r = −.11, p = .07). Similarly, disengagement was unrelated to either anxiety (r = −.04, p = .44) or hopelessness (r = −.08, p = .18).
Table 2.
Baseline characteristics of N=271 participants.
| Variable | Value |
|---|---|
| Hamilton Rating Scale for Depression, 24 items, median (IQR*) | 17 (13 – 22) |
| Modified Hamilton Rating Scale for Depression, 21 items, median (IQR) | 14 (11 – 17) |
| Disengagement Strategy Use, median (IQR) | 14 (12 – 17) |
| Engagement Strategy Use, median (IQR) | 16 (14 – 19) |
| Age, years, median (IQR) | 69.63 (64.56 – 76.82) |
| Education, years, median (IQR) | 12 (12 – 15) |
| Beck Hopelessness Inventory (N=263), median (IQR) | 7 (4 – 11) |
| Clinical Anxiety Scale, median (IQR) | 3 (1 – 6) |
| Mini Mental State Exam, median (IQR) | 28 (27 – 29) |
| Charlson Comorbidity Index, median (IQR) | 2 (1 – 4) |
| Assigned Intervention, % (n) | 56.83 (154) |
| Female, % (n) | 73.80 (200) |
| White, % (n) | 79.70 (216) |
| Major Depressive Disorder Diagnosis (N=269), % (n) | 75.09 (202) |
| Living with Someone, % (n) | 60.89 (165) |
IQR = Interquartile Range
Correlates of baseline depression severity identified by univariate linear regression models are displayed in Table 3. Decreased engagement was associated with higher baseline depression severity (β = −0.20, p = .02). Other correlates of higher depression severity included younger age, greater hopelessness and greater anxiety.
Table 3.
Univariate regression and Cox proportional hazards models.
| Baseline Depression Severity (N=271) |
Time to Depression Remission (N=234) |
|||||
|---|---|---|---|---|---|---|
| Covariate* | Beta | 95% CI | p-value | Hazard Ratio |
95% CI | p- value |
| Age | −0.09 | (−0.15, −0.01) | 0.02 | 1.01 | (0.98, 1.03) | 0.63 |
| Education | −0.16 | (−0.36, 0.03) | 0.10 | 1.05 | (0.99, 1.10) | 0.11 |
| Female | −0.72 | (−1.96, 0.51) | 0.25 | 0.89 | (0.63, 1.26) | 0.50 |
| White | 0.56 | (−0.78, 1.91) | 0.41 | 1.12 | (0.76, 1.65) | 0.56 |
| Living with Someone | 1.08 | (−0.03, 2.19) | .06 | .89 | (0.66, 1.22) | 0.48 |
| Engagement | −0.20 | (−0.36, −0.03) | 0.02 | 1.03 | (0.98, 1.07) | 0.28 |
| Disengagement | −0.11 | (−0.28, 0.05) | 0.17 | 1.05 | (1.00, 1.10) | 0.04 |
| BHS | 0.30 | (0.19, 0.42) | <0.01 | 0.96 | (0.93, 1.00) | 0.03 |
| CAS | 0.38 | (0.26, 0.50) | <0.01 | 0.96 | (0.93, 1.00) | 0.07 |
| MMSE | −0.10 | (−0.47, 0.26) | 0.58 | 0.99 | (0.90, 1.10) | 0.85 |
| CCI | 0.20 | (−0.02, 0.42) | 0.07 | 0.99 | (0.93, 1.06) | 0.77 |
| Intervention | -- | -- | -- | 1.47 | (1.07, 2.01) | 0.02 |
| Baseline HRSD-21m | -- | -- | -- | 0.94 | (0.91, .98) | < 0.01 |
| MDD | -- | -- | -- | 0.88 | (0.61, 1.27) | 0.47 |
HRSD-21m =21-item Hamilton Rating Scale for Depression; BHI = Beck Hopelessness Inventory; CAS = Clinical Anxiety Scale; MMSE = Mini Mental State Exam; CCI = Charlson Comorbidity Index; MDD = Major Depressive Disorder
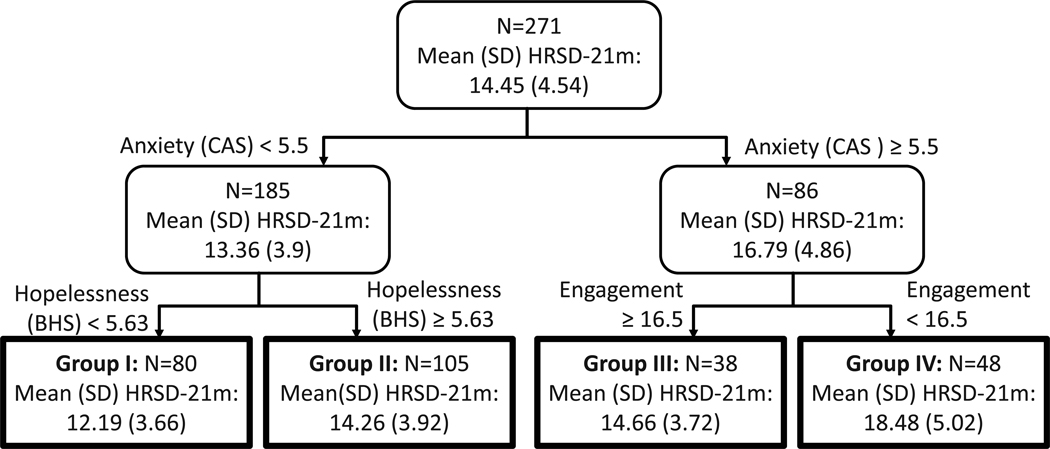
The regression tree in Figure 1 largely confirmed the results of the baseline univariate models, showing that anxiety, hopelessness and engagement were useful in distinguishing between various levels of baseline depression severity. For participants with higher anxiety, engagement was associated with lower depression severity. For participants with lower anxiety, lower hopelessness was associated with lower depression severity. The split on engagement provided the largest relative improvement in the model’s ability to distinguish classification groups; successive splits on subgroups reduced unexplained error by 12.42% (anxiety), 6.22% (hopelessness), and 15.42% (engagement). In contrast, replacing the split on engagement with a competing split on disengagement would have resulted in only a 2.05% reduction in unexplained error.
Figure 1.
Depression Remission
Univariate Cox proportional hazards results for modeling time to depression remission are displayed in Table 3. Greater disengagement at baseline predicted earlier time to remission (exp(β) = 1.05, p = .04). Lower baseline hopelessness, lower depression severity and intervention assignment also predicted earlier time to depression remission.
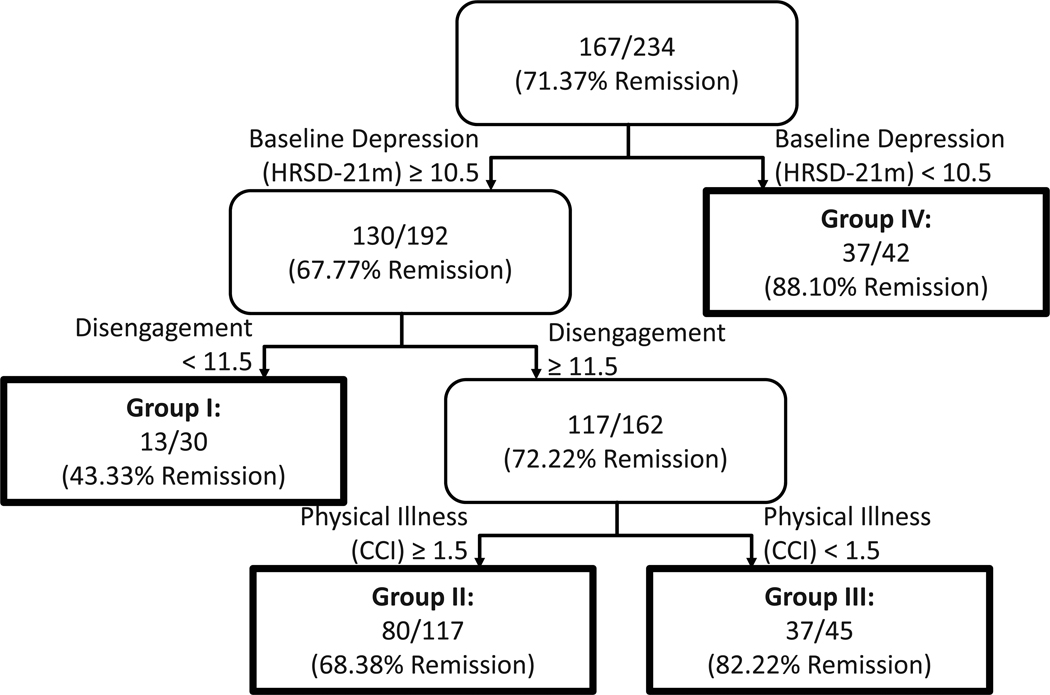
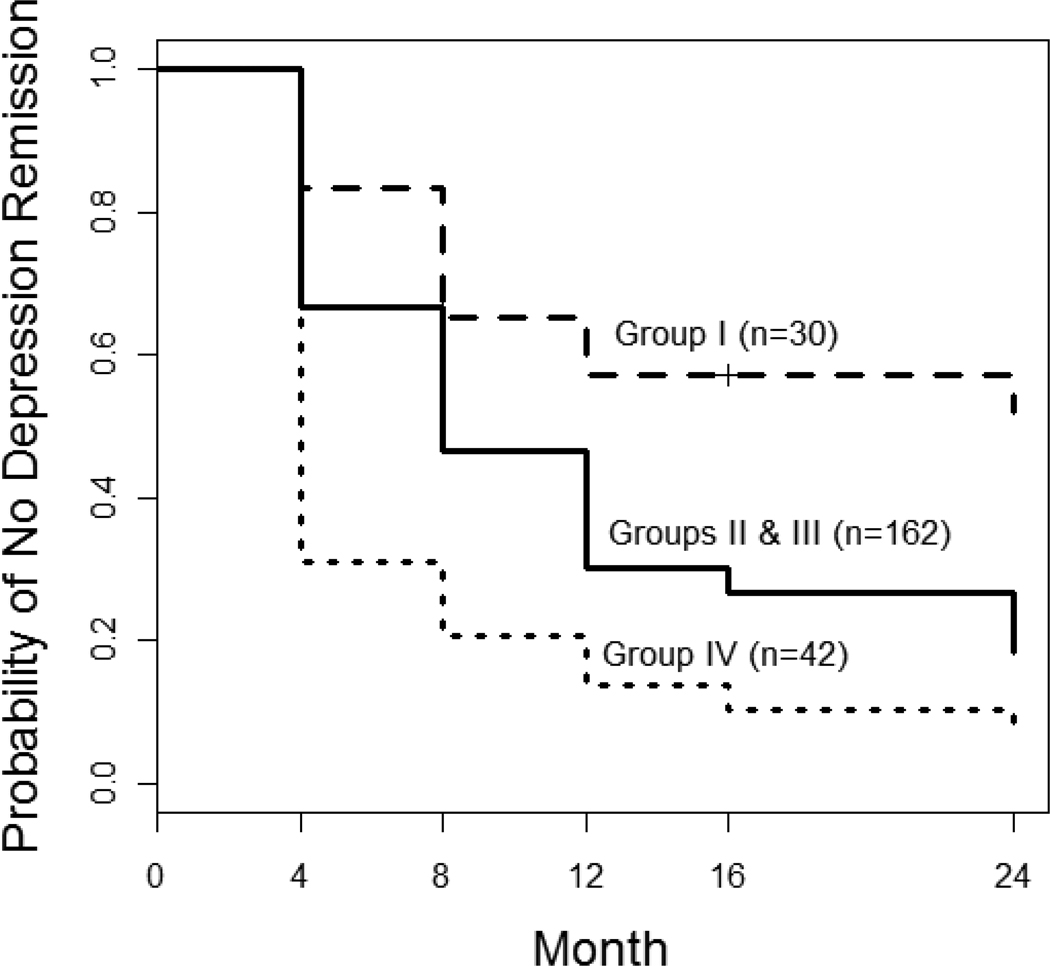
As illustrated in Figure 2, the tree-structured survival model indicated four risk groups for time to depression remission; associated Kaplan Meier distributions are displayed in Figure 3. Predictors that distinguished the four subgroups were baseline depression severity, disengagement, and burden of physical illness. Of the participants with moderate-to-high levels of depression severity, greater disengagement was associated with earlier remission. Burden of physical illness further distinguished time to remission in those with greater disengagement, such that those with a lower burden of illness had earlier remission than those with a higher burden of illness. Nonetheless, older adults with a higher burden of illness and greater disengagement had earlier remission than older adults with lower disengagement.
Figure 2.
Figure 3.
The split on baseline depression severity provided the largest relative improvement in the model’s ability to distinguish risk groups; successive splits on subgroups reduced unexplained error by 4.86% (baseline depression severity), 3.78% (disengagement) and 2.25% (physical illness). Replacing the split on disengagement with a competing split on engagement would have resulted in a relative improvement of only 1.66%.
Two multivariate Cox proportional hazard models were fit to further assess the impact of the use engagement and disengagement strategies on time to depression remission (Table 4). After controlling for gender, age, baseline depression and physical illness, disengagement was a significant predictor of time to remission (HR = 1.06, p=.03). Engagement was not significant (HR=1.01, p=.64) after controlling for these same factors.
Table 4.
Multivariate Cox proportional hazards models for the impact of the use of engagement and disengagement strategies on time to depression remission.
| Covariate | Hazard Ratio |
95% CI | p-value | Hazard Ratio |
95% CI | p-value |
|---|---|---|---|---|---|---|
| Age | 1.00 | (.97, 1.02) | 0.66 | 1.00 | (.98, 1.02) | 0.91 |
| Gender (Female) | 0.75 | (.52, 1.07) | 0.11 | 0.79 | (.55, 1.13) | 0.19 |
| Baseline HRSD-21* | 0.93 | (.90, .97) | < 0.01 | 0.93 | (.89, .97) | < .01 |
| Intervention | 1.53 | (1.12, 2.11) | 0.01 | 1.56 | (1.14, 2.15) | 0.01 |
| Physical Illness | 0.98 | (.91, 1.05) | 0.55 | 0.99 | (.92, 1.06) | 0.70 |
| Use of Disengagement Strategies | 1.06 | (1.01, 1.11) | 0.03 | -- | -- | -- |
| Use of Engagement Strategies | -- | -- | -- | 1.01 | (.97, 1.06) | 0.64 |
HRSD-21m =21-item Hamilton Rating Scale for Depression
DISCUSSION
In this study of health-oriented control strategies in older, depressed, primary care patients, the use of disengagement strategies predicted earlier remission, particularly in the subgroup of individuals with greater severity of baseline depression. Both univariate and tree-structured baseline regression analyses confirmed earlier findings of Wrosch et al. (2002) and Gitlin et al. (2007) that the use of engagement strategies was related to less severe depressive symptoms in older community-dwelling adults. However, in the present study, the use of engagement strategies did not predict remission, raising the question of whether the finding of cross-sectional association can be explained by the effects of depressed mood on either the reporting of or use of engagement strategies.
Goal Disengagement and Depression Remission
The use of disengagement strategies, such as avoiding self-blame for unmet health goals and shifting focus to other more important domains, was associated with earlier depression remission. The diathesis-stress model and attributional style may explain this link between the use of disengagement strategies and depression remission in the context of chronic health conditions. Specifically, Abramson and colleagues (1989) found that attributing negative events and outcomes to personal failures and subsequently linking them to one’s permanent character can contribute to the onset and maintenance of depression. The use of disengagement strategies for chronic health stresses may counter these negative attributions by prompting elders to avoid self-blame (“I am not to blame for it”), make strategic social comparisons (“other people are worse off than I am”) and shift focus to more realistic goals (“I focus on other important things in my life”). In a similar way, cognitive therapy alleviates depression by challenging feelings of worthlessness and guilt that emerge from the experience of chronic illness and disability and engages the patient in rewarding activities (Sensky, 1989; Beck, 1995). Finally, disengagement strategies can also be viewed as an optimistic way of allocating one’s effort. In agreement with prior findings that a pessimistic explanatory style hampers recovery from depression (Peterson and Seligman, 1984), disengagement may be a constructive response in the face of health stressors and depression.
Strengths, Limitations and Future Directions
The representativeness of the primary care sample, the longitudinal design, the two-year observation, and the detailed clinical characterization add confidence in the findings. Furthermore, the tree-structured models provide clinically relevant predictions by using risk factors to identify a series of prognostic groups. Such models are arguably more useful for informing interventions than the traditional regression approach because they can identify subgroups of individuals for whom a change in a modifiable risk factor, such as the use of disengagement strategies, would be particularly beneficial. However, tree models do have limitations to consider. Because small changes in the sample can result in different tree structures (Strobl et al., 2009), it is important to utilize independent samples for validation (Kiernan et al., 2001). Overfitting may also be a concern (Strobl et al., 2009), although tree models in this manuscript were fit with a relatively large splitting penalty to avoid this problem as much as possible.
Limitations to this study included the lack of follow-up data on the use of control strategies, a difficulty identifying the time and/or occurrence of depression remission due to measurement of depression severity at intervals of four months or greater, missing baseline control strategy use data on a large proportion of the PROSPECT sample, and the limited ability of the CCI to capture the full extent and functional impact of physical illness. Additionally, the control strategy scales had relatively low reliability and were based on self-report. While the patients’ perception of how they cope with health stressors appears to be important for their well-being, self-report questionnaires cannot fully capture their day-to-day use of these cognitive and behavioral strategies.
This study found that depressed older adults who use disengagement strategies may experience earlier remission. This finding gives rise to the hypothesis that one can help depressed older adults recover from depression by teaching them to use disengagement strategies. In order to test this hypothesis, it will be necessary to show 1) that depressed elders can learn to use disengagement strategies and 2) that increased use of disengagement strategies results in increased recovery rates. To this end, the authors note that disengagement strategies are indeed similar to the strategies that cognitive therapists teach their patients (Beck, 1995), yet many depressed elderly in this sample used these strategies on their own. This adds credence to the hypothesis that depressed elderly could learn to use disengagement strategies through an intervention. Disengagement strategies may be also incorporated into multi-component interventions for depression in primary care, following the approach Gitlin and colleagues used to reduce mortality in functionally impaired older adults (Gitlin et al., 2006a; Gitlin et al., 2006b).
Acknowledgments
Funding Source: NIH 5 T32 MH016804, R01 MH59366, P30 MH68638, R01 MH59380, P30 MH52129, R01 MH59381, P30 MH5224
Role of Sponsor: None
Footnotes
DECLARATION
Conflict of Interest:
Dr. Frank serves as a member of an advisor board for Servier and receives royalties from Guilford press. Dr. Alexopoulos has a research grant from Forest, is a stockholder for Johnson & Johnson, and is a member of the speakers’ bureau for Forest, Lilly, Bristol Meyers Squibb, Astra Zeneca and Merck. Dr. Wallace, Dr. Dombrovski, Dr. Morse, Ms. Houck, Dr. Reynolds, and Dr. Schulz do not have any conflicts of interest.
REFERENCES
- 1.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 2.Alexopoulis GS, Katz II, Bruce ML, et al. Remission in depressed geriatric primary care patients: A report from the PROSPECT study. Am J Psychiatry. 2005;162:718–724. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dombrovski AY, Mulsant BH, Houck PR, et al. Residual symptoms and recurrence during maintenance treatment of late-life depression. J Affect Disord. 2007;103:77–82. doi: 10.1016/j.jad.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andreescu C, Lenze EJ, Dew MA, Begley AE. Effects of comorbid anxiety on treatment response and relapse risk in late-life depression: controlled study. Br J Psychiatry. 2007;190 doi: 10.1192/bjp.bp.106.027169. 344-249. [DOI] [PubMed] [Google Scholar]
- 5.Reynolds CF, Dew MA, Pollock BG, et al. Maintenance treatment of major depression in old age. N Engl J Med. 2006;354:1130–1138. doi: 10.1056/NEJMoa052619. [DOI] [PubMed] [Google Scholar]
- 6.Buysse DJ, Reynolds CFI, Hoch CC, et al. Longitudinal Effects of Nortriptyline on EEG Sleep and the Likelihood of Recurrence in Elderly Depressed Patients. Neuropsychopharmacology. 1996;14:243–252. doi: 10.1016/0893-133X(95)00114-S. [DOI] [PubMed] [Google Scholar]
- 7.Gitlin LN, Hauck WW, Winter L, Dennis MP, Schulz R. Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. J Am Geriatr Soc. 2006;54:950–955. doi: 10.1111/j.1532-5415.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- 8.Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, Hauck WW. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 9.Heckhausen J, Schulz R. Optimisation in primary and secondary control. Int J Behav Dev. 1993;16:287–303. [Google Scholar]
- 10.Heckhausen J, Schulz R. A life-span theory of control. Psychol Rev. 1995;102:284–304. doi: 10.1037/0033-295x.102.2.284. [DOI] [PubMed] [Google Scholar]
- 11.Schulz R, Heckhausen J. A life-span model of successful aging. Am Psychol. 1996;51:702–714. doi: 10.1037//0003-066x.51.7.702. [DOI] [PubMed] [Google Scholar]
- 12.Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychol Rev. 2010;117:32–60. doi: 10.1037/a0017668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wrosch C, Schulz R, Heckhausen J. Health stresses and depressive symptomology in the elderly: the importance of health engagement control strategies. Health Psychol. 2002;21:340–348. doi: 10.1037//0278-6133.21.4.340. [DOI] [PubMed] [Google Scholar]
- 14.Gitlin LN, Hauck WW, Dennis MP, Schulz R. Depressive symptoms in older African-american and white adults with functional disabilities: The role of control strategies. J Am Geriatr Soc. 2007;55:1023–1030. doi: 10.1111/j.1532-5415.2007.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wrosch C, Heckhausen J, Lachman ME. Primary and secondary control strategies for managing health and financial stress across adulthood. Psychol Aging. 2000;15:387–399. doi: 10.1037//0882-7974.15.3.387. [DOI] [PubMed] [Google Scholar]
- 16.Wrosch C, Heckhausen J. Control processes before and after passing a developmental deadline: Activation and deactivation of intimate relationship goals. J Pers Soc Psychol. 1999;77:415–427. [Google Scholar]
- 17.Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: Goal disengagement, goal reengagement, and subjective well-being. Pers Soc Psychol Bull. 2003;29:1494–1508. doi: 10.1177/0146167203256921. [DOI] [PubMed] [Google Scholar]
- 18.Kiernan M, Kraemer HC, Winkleby MA, King AC, Taylor CB. Do Logistic Regression and Signal Detection Identify Different Subgroups at Risk? Implications for the Design of Tailored Interventions. Psychol Methods. 2001;6(1):35–48. doi: 10.1037/1082-989x.6.1.35. [DOI] [PubMed] [Google Scholar]
- 19.Schulz R, Heckhausen J. Health-specific optimization in primary and secondary control scales. Pittsburgh, PA: University of Pittsburgh; 1998. [Google Scholar]
- 20.Snaith RP, Baugh SJ, Clayden D, Husain A, Sipple MA. The clinical anxiety scale: An instrument derived from the Hamilton anxiety scale. Br J Psychiatry. 1982;141:518–523. doi: 10.1192/bjp.141.5.518. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Kovacs M, Weissman A. Hopelessness and suicidal behavior: An overview. JAMA. 1975;234:1146–1149. [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clnician. J Psych Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA. Beck Hopelessness Scale Manual. New York, NY: The Psychological Corporation; 1988. [Google Scholar]
- 25.Westhuis D, Thyer BA. Development and Validation of the Clinical Anxiety Scale: A Rapid Assessment Instrument for Empirical Practice. Educational and Psychological Measurement. 1989;49:153–163. [Google Scholar]
- 26.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and Regression Trees. Belmont, CA: Wadsworth International Group; 1984. [Google Scholar]
- 27.LeBlanc M, Crowley J. Relative risk trees for censored survival data. Biometrics. 1992;48:411–425. [PubMed] [Google Scholar]
- 28.Therneau TM, Atkinson EJ, Foundation M. An introduction to recursive partitioning using the RPART routines. Rochester, MN: Section of Biostatistics, Mayo Clinic; 1997. [Google Scholar]
- 29.Therneau TM, Atkinson EJ, Ripley B. Recursive Partitioning: R package. 3.1–4.1 edn. Rochester, MN: 2008. [Google Scholar]
- 30.Abramson LY, Metalsky FI, Alloy LB. Hopeless depression: A theory based subtype of depression. Psychol Rev. 1989;96:358–372. [Google Scholar]
- 31.Sensky T. Cognitive Therapy with Patients with Chronic Physical Illness. Psychother Psychosom. 1989;52:26–32. doi: 10.1159/000288262. [DOI] [PubMed] [Google Scholar]
- 32.Beck JS. Cognitive Therapy: Basics and Beyond. New York: Guilford; 1995. [Google Scholar]
- 33.Peterson C, Seligman MEP. Causal explanations as a risk factor for depression: Theory and evidence. Psychol Review. 1984;91:347–374. [PubMed] [Google Scholar]
- 34.Strobl C, Malley J, Tutz G. An Introduction to Recursive Partitioning: Rationale, Application and Characteristics of Classification and Regression Trees, Bagging and Random Forests. Psychol Methods. 2009;14(4):323–348. doi: 10.1037/a0016973. [DOI] [PMC free article] [PubMed] [Google Scholar]