Abstract
Context/objective
To describe preinjury alcohol and drug use and opportunities for secondary prevention among persons with recent spinal cord injury (SCI).
Design
Survey.
Setting
Acute inpatient rehabilitation program.
Participants
Participants were 118 (84.8%) of 139 consecutive admissions who met inclusion criteria and were screened for preinjury alcohol and drug use.
Interventions
None.
Outcome measures
Alcohol and drug use, toxicology results, alcohol problems, readiness to change, and treatment preferences.
Results
Participants were on average 37 years old, 84% were men, and 85% were white. Fifty-one percent of the sample was considered ‘at-risk’ drinkers. Significant lifetime alcohol-related problems were reported by 38% of the total sample. Thirty-three percent reported recent illicit drug use and 44% of the 82 cases with toxicology results were positive for illicit drugs. Seventy-one percent of at-risk drinkers reported either considering changes in alcohol use or already taking action. Forty-one percent reported interest in trying substance abuse treatment or Alcoholics Anonymous (AA). Motivation to change alcohol use was significantly and positively associated with self-reported indicators of alcohol problem severity.
Conclusion
Preinjury alcohol and drug abuse are common among persons with recent SCI. Substance abuse screening is feasible and detects not only salient clinical problems but also significant motivation to change and interest in AA or treatment, all of which represent an important window of opportunity for appropriate brief interventions and referrals. In contrast with the idea that alcoholism is a ‘disease of denial’, the majority of at-risk drinkers with new onset SCI indicate they are considering making changes.
Keywords: Alcohol, Drug, Substance-related disorders, Spinal cord injuries, Rehabilitation, Paraplegia, Tetraplegia, Toxicology screening
Alcohol and drug abuse or dependence is a common comorbid condition among newly injured persons with spinal cord injury (SCI). Preinjury alcohol use and abuse has been shown to be higher among individuals who sustain SCI compared to the general population, with approximately one-third of newly injured persons with SCI reporting a history of alcohol-related problems.1 A significant proportion of persons with SCI report that preinjury alcohol or drug use contributed to their injury,1 while estimates of intoxication at the time of injury range from 17 to 62%.2–4
Preinjury alcohol or drug use among persons with SCI has been associated with adverse medical and rehabilitation outcomes. Preinjury alcohol problems have been related to less functional independence at rehabilitation admission and discharge as well as slower progress during inpatient rehabilitation.5 Persons with SCI who have a history of problem drinking also report spending less time in productive activities (including rehabilitation therapies) during inpatient rehabilitation.6 History of preinjury alcohol and drug use predicts poorer health status and psychological adjustment following discharge. Use of alcohol and illicit substances prior to injury appears to be a risk factor for post-injury medical complications such as cardiovascular disease, kidney and liver disorders, urinary tract infections, and development of pressure ulcers.7,8 This is significant as evidence suggests that having one complication doubles the length of stay, increases mortality by fivefold, and adds more than $50 000 of hospital expenses among post-surgical patients with SCI.9 Additionally, preinjury alcohol and drug use are associated with increased risk of bankruptcy following injury.10
Rates of post-injury alcohol abuse among persons with SCI also appear to be quite high. Although many persons with SCI remain abstinent from alcohol and drugs following injury, others use alcohol or drugs post-injury at a rate exceeding that of the general population. Kolakowsky–Hayner found that about half of individuals with SCI who used alcohol prior to injury reported using alcohol at 12 months following injury.2 Of these, 41% were classified as moderate-to-heavy drinkers and approximately 20% reported using illicit drugs. Other studies have found that up to three-quarters of persons with SCI who used alcohol or drugs prior to injury returned to drinking within 7–18 months post-injury. High rates of illicit substance use are also reported.11,12 Additionally, Banerjea et al.12 found that among individuals with SCI accessing outpatient Veterans Health Administration or Medicare providers over a 2-year period, 9% had diagnosable alcohol use disorders, and 8% had other substance abuse problems identified in their medical chart with ICD-9CM codes. Post-injury alcohol use has been shown to be a leading cause of mortality among persons with SCI.13,14 It has also been associated with poorer rehabilitation and medical outcomes9,15 and with high rates of mental illness.12
Patterns of preinjury alcohol and drug use among persons with SCI have been increasingly well documented. However, much of the literature has methodological shortcomings that limit validity. Many studies of preinjury alcohol and drug use among persons with SCI are based exclusively on questionnaire or interview data, which may result in method bias. Also, most studies are based on community samples. Limited data are available on newly injured, consecutive inpatients with SCI. Several studies of preinjury alcohol and drug use have reported data based on admission toxicology screens or serum alcohol levels, with positive blood alcohol levels (BALs) ranging from 40 to 44% and positive drug toxicology screens ranging from 27 to 35%.1,3,16,17 However, many estimates of drug use based on toxicology screens may have limited validity because they screen for presence of opiates or benzodiazepines. These drugs are often administered in emergency medical treatment and may represent a possible confound. Also, some reports include results of drug toxicity screens that did not test for the presence of cannabinoids.3 Only one study has compared self-report data on drug and alcohol use with results of toxicity screens. Heinemann et al.16 found that 40% of patients seen in an acute SCI facility had positive BALs at admission, with 63% of these patients having BALs greater than the common legal limit of 100 mg/dL. Drug toxicity screens were positive for 35% of patients. Agreement was 78% between self-reported alcohol use and BALs, but only 58% between self-reported drug use and the results of urine toxicology screens.
Although preinjury alcohol and drug use appears to be an important factor in rehabilitation of newly injured persons with SCI, relatively few rehabilitation centers have incorporated systematic screening, assessment, or treatment protocols into their programs. It has been suggested that rehabilitation may present a critical ‘window of opportunity’ to address drug and alcohol problems in rehabilitation populations.1,2 Such interventions may have important implications for progress during rehabilitation as well as adjustment following discharge.
This study was designed with several goals in mind: (1) to replicate and extend prior research on the prevalence of alcohol and drug-related problems in people undergoing inpatient rehabilitation for SCI by recruiting a larger representative sample than has been reported in previous studies; (2) to include and compare both subjective and objective measures of illicit drug use, since polydrug abuse may have important implications for treatment planning and prognosis;18 and (3) to facilitate treatment planning by assessing readiness to change substance use and treatment preferences among at-risk drinkers. Based on prior research and clinical experience we hypothesized that: (1) alcohol and drug abuse would be highly prevalent in this population; (2) greater self-reported alcohol-related problems would be positively associated with greater readiness to change alcohol use; and (3) participants would report significant interest in making changes in alcohol use, indicated by interest in attending treatment or Alcoholics Anonymous (AA) as well as changing alcohol use on their own. Such findings would provide support for the importance of identifying and intervening in substance abuse problems during inpatient rehabilitation.
Method
Participants
The study sample was drawn from 139 consecutive patients with recent SCI admitted to an inpatient rehabilitation unit within a Level 1 Trauma center that serves a four state region. Participants were recruited over approximately 4 years (6/95–7/99). Non-English speakers (n = 5), patients under 18 years of age (n = 1), patients with severe traumatic brain injury (TBI) and not able to reliably answer questions (n = 1), and patients with severe psychiatric disorders (e.g. psychosis; n = 3) were excluded from the study sample. Nine eligible patients could not be screened prior to discharge, and two patients did not complete the alcohol problem measure, resulting in a final sample of 118 participants. Thirty-two participants were diagnosed with SCI and TBI, whereas 86 participants were diagnosed with SCI only. Of participants diagnosed with SCI, 61 (51.7%) had paraplegia and 57 (48.3%) had tetraplegia.
As can be seen in Table 1, participants were on average 37.3 years old (median age = 35 years), approximately 85% were white and 84% were men. Seventy-two percent of participants were single, divorced, or separated, 88% worked full- or part-time and 77% had at least a high school education.
Table 1.
Demographic characteristics for total sample and sub-samples
| Total sample | At-risk drinkers | Not at-risk | ||
|---|---|---|---|---|
| Sample characteristics | n = 118 | n = 60 | n = 58 | P value |
| Age in years (SD) | 37.3 (14.1) | 37.4 (11.9) | 37.1 (16.1) | ns |
| Gender | — | — | — | ns |
| Men | 99 (83.9%) | 53 (53.5%) | 46 (46.5%) | |
| Women | 19 (16.1%) | 7 (36.8%) | 12 (63.2%) | |
| Race* | n = 114 | n = 58 | n = 56 | ns |
| White | 97 (85.1%) | 48 (49.5%) | 49 (50.5%) | |
| African American | 8 (7.0%) | 5 (62.5%) | 3 (37.5%) | |
| Native American | 1 (0.9%) | 1 (100%) | 0 | |
| Hispanic | 3 (2.6%) | 3 (100.0%) | 0 | |
| Asian American | 5 (4.4%) | 1 (20.0%) | 4 (80.0%) | |
| Marital** | n = 116 | n = 59 | n = 57 | .009 |
| Single | 64 (55.2%) | 37 (57.8%) | 27 (42.2%) | |
| Married/cohabiting | 32 (27.6%) | 10 (31.3%) | 22 (68.7%) | |
| Separated/divorced | 17 (14.7%) | 10 (58.8%) | 7 (41.2%) | |
| Employment status | n = 115 | n = 57 | n = 59 | ns |
| Full time | 83 (72.2%) | 47 (56.6%) | 36 (43.4%) | |
| Part time | 5 (4.3%) | 3 (60.0%) | 2 (40.0%) | |
| Unemployed | 9 (7.8%) | 5 (55.6%) | 4 (44.4%) | |
| Education*** | n = 116 | n = 59 | n = 57 | ns |
| Less than high school | 28 (24.1%) | 16 (57.1%) | 12 (42.9%) | |
| High school | 51 (44.0%) | 30 (58.8%) | 21 (41.2%) | |
| More than high school | 37 (31.9%) | 13 (35.1%) | 24 (64.9%) |
Note: *P value for combined variable ‘White versus other’; **P value for combined variable ‘married/cohabiting versus unmarried’; ***P value for combined variable ‘completed high school versus not’.
Procedures
Participants were administered questionnaires by a trained interviewer as a part of standard rehabilitation care. Measures were administered an average of 36.5 days post-SCI (median = 25 days) and 15.6 days after admission to the rehabilitation unit. In order to prevent potential reactivity effects of the alcoholism measure on measures of readiness to change, the readiness to change instrument was always administered first. In addition, there were no systematic attempts to educate participants about or intervene in alcohol-related problems before the study assessment. Relevant medical diagnostic and clinical information was obtained from the patient's chart. Our human subjects institutional review board approved all procedures for this study. In order to enhance participation and subject protection, we obtained a Certificate of Confidentiality from the National Institute on Alcoholism and Alcohol Abuse. This certificate affords investigators the right to refuse disclosure of any alcohol-related research information, even under subpoena, from local, state, or federal authorities.
Measures
Alcohol consumption and drug use
Drinking was assessed by asking the number of times participants drank any alcoholic beverage during the month before their injury and how many drinks they typically consumed on each drinking occasion. Binge drinking was assessed by asking the number of times in the month prior to injury the patient had consumed five or more drinks on a single occasion. Participants were also asked whether they had driven an automobile after having consumed two or more drinks in the month before their injury. Finally, participants were asked about any illicit drugs used during the 3-month period prior to injury.
Physical dependency
Physical dependency upon alcohol was measured by using the 12-item Ph scale from the Brief Drinker Profile.19 The Ph scale includes items such as: ‘Are you always able to stop drinking when you want to?’ and ‘Are you able to drink more now than you used to without feeling the same effect?’ Scores on the Ph scale range from 0 to 20. The following qualitative ranges are suggested by the measure's authors: 1–4 (mild), 5–10 (definite and significant), 11–14 (substantial), and 15–20 (severe).
Lifetime alcohol-related problems
The Short Michigan Alcoholism Screening Test (SMAST) is a 13-item list of common signs and symptoms of alcoholism.20 Respondents indicate whether they have ever experienced each symptom of problem drinking during their lifetime. Examples of items include: ‘Does any member of your family (wife, husband, parents, etc.) ever worry or complain about your drinking?’ and ‘Have you ever gotten into trouble at work because of drinking?’ Items are equally weighted and summed to yield a total score. The SMAST is a relatively brief measure with demonstrated reliability and validity in a number of populations, including patients with SCI and TBI.1,21,22 A cutoff score of 3 or more was used to indicate a clinically significant history of problem drinking (at-risk drinking).20
Readiness to change
The Readiness to Change Questionnaire (RTC) was used to assess readiness to change preinjury drinking patterns.23 The RTC consists of statements reflecting thoughts and behaviors associated with the most common stages of change found among persons in health care settings (i.e. precontemplation, contemplation, and action). Each stage of change is represented by four items. Precontemplation items refer to the denial or non-endorsement of alcohol-related problems. Contemplation items refer to beliefs that alcohol might be a problem and that behavior change is being considered. Action items reflect behavior changes the person is already making to cut down or stop drinking. Participants rate the degree to which they agree or disagree with each item on a five-point Likert-type scale. The RTC was specifically developed for brief opportunistic assessments in medical settings.23,24 It has demonstrated reliability and validity and has been used to assess readiness to change drinking habits in acutely hospitalized patients with TBI and SCI.1,23–25 For the heuristic value of stage assignment and for comparability to other studies, the original 12-item version of this measure was used to categorize each at-risk drinker into a specific stage of change. However, an overall readiness to change score was computed for correlational analyses, consisting of the sum of the contemplation and action scale scores minus the precontemplation scale score.
Preferred change strategies: Participants were asked ‘At the present time are you interested in: Alcohol treatment? Trying AA? Making changes on your own?’ Participants were asked to respond yes or no to each change strategy.
Blood alcohol and toxicology testing
Serum alcohol level (mg/dL) and toxicology screen by urinalysis are routinely obtained as a part of the emergency room assessment of trauma patients in our medical center. In this sample, 89 (75.4%) cases had a BAL included in the medical record. For drug toxicology screens, 82 (69.5%) cases had results reported in the medical record.
Attributions regarding the cause of injury
Participants were asked to indicate the degree to which they thought they were responsible for the cause of their injury. They were also asked to indicate the extent to which they thought alcohol or drug use was a cause of their injury. Ratings for both questions were made on a 0–2 point ordinal scale. Possible responses were: ‘not at all’, ‘somewhat’ and ‘very much’.
Results
Definition of at-risk drinkers
The inclusion criteria for classification of at-risk drinkers were as follows: (1) being a current drinker and scoring in the ‘alcoholic’ range on the SMAST (SMAST score ≥3); (2) BAL at admission to the emergency room in the ‘intoxicated’ range (BAL > 99); or (3) at least once in the month prior to injury, binge drinking (five or more drinks per occasion) or driving an automobile after having had two or more drinks.1
Based on these criteria, 60 persons (50.8%) were classified as at-risk drinkers. Forty-four persons (37.9%) met at-risk criteria based on their SMAST score and status as current drinkers. Twenty-one (35%) participants classified as at-risk were intoxicated at the time of their injury. No participants with SMAST scores in the normal range were intoxicated at the time of their injury. Twenty participants (33.3%) were considered at-risk drinkers based on other risky drinking behaviors in the month preceding injury, such as binge drinking (n = 11) or driving after having two or more drinks (n = 9). Of the 58 persons not considered to be at-risk, four (6.9%) were abstinent alcoholics. That is, they reported a significant history of alcohol problems on the SMAST but reported being abstinent from alcohol for over 1 year at the time of injury.
Demographics and at-risk status
Demographic variables for the total sample, at-risk drinkers, and persons classified as not at-risk are shown in Table 1. Because of the small number of participants in certain cells, categories of some demographic variables were combined to facilitate statistical analysis. These variables included race or ethnicity (white versus non-white), education (high school graduate versus not), marital status (married or cohabiting versus never married, divorced/separated, or widowed) and vocational status (employed full- or part-time versus unemployed). Participants classified as at-risk were significantly more likely to be single than currently married or cohabiting (odds ratio = 3.08). Although at-risk drinkers and not–at-risk drinkers were equally likely to be high school graduates, fewer at-risk drinkers reported post-secondary education. All participants who self-identified as Native American (n = 1) or Hispanic (n = 3) met criteria for inclusion in the at-risk category.
Alcohol use patterns
Of the total sample, 70 participants (59.3%) reported drinking at least once in the month before injury. Twenty participants (16.9%) reported abstaining from alcohol for at least 1 year. Participants drank on average 7.2 (SD, 9.0) times per month and 2.8 (SD, 3.9) drinks per occasion. The average number of drinks per week (6.7) falls at the 70th percentile for American males and the 80th percentile overall. Over one-third of the total sample (35.6%) reported binge drinking, and 17.7% drove an automobile after having two or more drinks in the month prior to SCI. No demographic variables were associated with weekly alcohol consumption.
Preinjury alcohol-related problems
Self-reported alcohol problems were prevalent in this sample of people with SCI. Over 40% of the total sample scored above the cutoff on the SMAST. The most frequently endorsed SMAST items were: having attended one or more AA meetings (37.1%), having gone for help about drinking (20.7%), having been arrested for drunk behavior other than driving while intoxicated (13.8%), and having been arrested for driving while intoxicated (12.1%).
Blood alcohol level
Admission BALs were available for 89 (75.4%) participants (see Table 2). Of these, 28 (31.5%) had a positive BAL and 21 (23.6%) were considered intoxicated (at or above the legal limit of 100 mg/dl). Of those who were intoxicated, 57.1% also scored in the ‘alcoholic’ range on the SMAST, suggesting that they also had a history of alcohol-related problems. Of those who were not intoxicated, 35.4% scored in the ‘alcoholic’ range on the SMAST.
Table 2.
Drinking and drinking problems in the total sample and at-risk drinkers
| Drinking characteristics | Total sample | At-risk drinkers |
|---|---|---|
| BAL at admission (mg/dl) | n = 89 | n = 51 |
| 0 | 61 (68.5%) | 24 (47.1%) |
| 13–99 | 6 (6.7%) | 5 (9.8%) |
| 100–199 | 15 (16.9%) | 15 (29.43%) |
| 200–299 | 4 (4.5%) | 4 (7.8%) |
| 300–352 | 3 (3.4%) | 3(5.9%) |
| Lifetime alcohol-related problems (SMAST) | n = 116 | n = 85 |
| SMAST positive (>2) | 44 (37.9%) | 40 (47.1%) |
| Have attended AA | 34 (29.3%) | 31 (36.5%) |
| Have gone for help about drinking | 17 (14.7%) | 16 (18.8%) |
| Have been arrested for driving while intoxicated | 14 (12.1%) | 14 (16.5%) |
| Have been arrested for other drunk behavior | 24 (20.7%) | 23 (27.1%) |
| Preinjury alcohol use patterns | n = 113 | n = 60 |
| Number of days per month in which drinking occurred m (SD) | 7.2 (9.0) | 4.4 (7.0) |
| Number of drinks consumed per occasion m (SD) | 2.8 (3.9) | 4.6 (4.7) |
| Average number of drinks per week m (SD) | 6.7 (10.7) | 11.4 (12.5) |
| Drove after having two or more drinks | 20 (17.7%) | 20 (33.3%) |
| Bingeing (>5 drinks per occasion) at least once | 42 (37.2%) | 60 (66.6%) |
| Physical dependency | n = 116 | n = 60 |
| None (0) | 23 (19.8%) | 5 (8.3%) |
| Mild (1–4) | 61 (52.6%) | 24 (40.0%) |
| Significant (5–10) | 24 (20.7%) | 23 (38.3%) |
| Substantial (11–14) | 6 (5.2%) | 6 (10.0%) |
| Severe (15–20) | 2 (1.7%) | 2 (3.3%) |
Alcohol and causal attributions of injury
Nearly one-quarter (24%) of the total sample reported that alcohol was either ‘somewhat’ or ‘very much’ involved in the cause of their injury. For participants classified as at-risk drinkers, the results were even more striking. Of 52 participants classified as not at-risk, only 2 (3.8%) attributed the cause of their injury to alcohol use, whereas 24 of the 56 participants classified as at-risk (42.9%) reported that alcohol had contributed to the cause of their injury (chi square = 22.45, df = 2, P < 0.000). At-risk status was also associated with attributing the cause of injury to oneself. Of participants classified as not at-risk, 21 (41.2%) reported that they were somewhat responsible for the cause of their injury and only 4 (7.8%) reported that they were very much a cause of their own injury. However, 19 (34.5%) of the at-risk drinkers reported that they were somewhat responsible for their injuries and 16 (29.1%) stated that they were very much a cause of their injury (chi square = 7.94, df = 2, P < 0.019).
Drug use
Complete self-report data on drug use were available for 110 (93.2%) participants (see Table 3). Overall, 36 (32.7%) participants admitted using one or more illicit drugs during the 3 months prior to injury, primarily marijuana (28.2%), cocaine (6.4%), and amphetamines (9.1%). At-risk drinkers were significantly more likely to report use of cocaine (P < 0.05) and marijuana (P < 0.01).
Table 3.
Rates of self-reported drug use and admission toxicology results for the total sample and by at-risk drinking
| Source of data | Total sample | At-risk drinkers | Not at-risk drinkers | Pearson χ2 |
|---|---|---|---|---|
| Self-reported drug use | (n = 110) | (n = 54) | (n = 56) | — |
| Cocaine | 7 (6.4%) | 6 (11.1%) | 1 (1.8%) | 4.0* |
| Marijuana | 31 (28.2%) | 22 (40.7%) | 9 (16.1%) | 8.3** |
| Amphetamines | 10 (9.1%) | 7 (13.0%) | 3 (5.4%) | 1.9 |
| Hallucinogens | 2 (1.8%) | 2 (3.7%) | 0 | 2.1 |
| Heroin | 3 (2.7%) | 2 (3.7%) | 1 (1.8%) | 0.4 |
| Other | 1 (0.9%) | 1 (1.9%) | 0 | 1.1 |
| Number of self-reported users | 36 (32.7%) | 23 (42.6%) | 13 (23.2%) | 4.7* |
| Toxicology results available | n = 82 | n = 43 | n = 39 | — |
| Cocaine | 4 (4.9%) | 4 (9.3%) | 0 | 3.7 |
| Marijuana | 20 (24.4%) | 15 (34.9%) | 5 (12.8%) | 5.4* |
| Amphetamine | 6 (7.3%) | 3 (7.0%) | 3 (7.7)% | 0.0 |
| Number with positive screen | 36 (43.9%) | 21 (48.8%) | 15 (38.5%) | 0.9 |
*P < 0.05; **P < 0.01.
Results of toxicology screens were available for 69.5% of the total sample (n = 82). Of these, 23 (28.1%) participants showed at least one positive result for marijuana, cocaine, or amphetamines (see Table 3). Seven participants (8.5%) showed positive toxicology results for two or more of these drugs. Consistent with findings from self-report data, positive toxicology results for marijuana and cocaine were significantly higher among at-risk drinkers (P < 0.05). The toxicology screen also included opiates and benzodiazepines, which were positive in 23.2 and 6.1% of the total sample, respectively. However, because these drugs might have been administered for therapeutic reasons by emergency medical technicians or emergency personnel from other hospitals, it was impossible to discriminate between substances used prior to injury versus those administered therapeutically following injury. Therefore, these data were not analyzed further.
Next, we compared the results of drug use screening by self-report versus toxicology screen. A comparable number of drug users were identified by self-report methods (n = 36) and toxicology screen (n = 36). Participants on whom toxicology data were obtained were more likely than persons on whom self-report data were gathered to screen positive for illicit drug use (43.9 versus 33.6%). However, a higher proportion of the total sample could be screened by self-report methods (95.8%) than by toxicology (69.5%). Of the 76 persons in the total sample for whom combined toxicology and self-report measures were available, 24 (31.6%) reported illicit drug use within the past 3 months and 34 (44.7%) tested positive for some illicit drug.
The overall degree of agreement between these two indicators of drug usage was only moderate (kappa = 0.43, P < 0.001). Of the 76 persons for whom both self-report and toxicology data were available, 15 (19.7%) denied drug use but tested positive for one or more illicit drugs, while 6 persons admitted using drugs during the 3 months prior to injury but tested negative for drugs at the time of injury. Similarly, agreement between toxicology and self-report within specific types of drugs was only fair (kappas = 0.47–0.69). For example, toxicology and self-reported marijuana use indicators were both positive in only 14 cases. In four cases, the patients denied marijuana use but their toxicology screen was positive for this drug. In nine cases patients admitted using marijuana in the past 3 months, but did not test positive for marijuana at the time of injury. Similar results were obtained for cocaine and amphetamines.
Combined alcohol and drug use categories
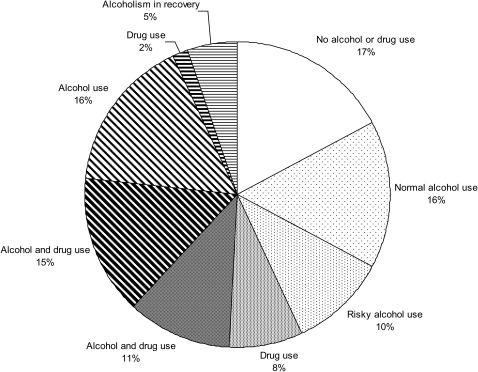
In Fig. 1 we summarize concurrent alcohol and drug use for the entire sample. Only 33% of the sample exhibits either ‘normal’ alcohol use or no alcohol or drug use. Among those who use alcohol, only 38% do not have a history of significant alcohol-related problems or co-occurring drug use. Isolated drug use is rare, accounting for 10% of the sample. In a majority of cases, drug use is complicated by alcohol use and a history of alcohol-related problems. A small fraction of those with a history of alcohol problems is in recovery (abstinent from alcohol and drug use) at the time of injury.
Figure 1.
Drinking and drug use for those with or without lifetime alcohol-related problems as categorized by the SMAST (n = 116).
Note: White or speckled areas represent persons without significant lifetime alcohol-related problems (SMAST ≤ 3). Striped areas represent persons with significant lifetime alcohol-related impairments (SMAST ≥ 3).
Within the white or speckled areas: No alcohol or drug use, no alcohol use within past year, no drug use; Normal alcohol use, alcohol use without repeated binge drinking, drinking and driving or drug use; Risky alcohol use, self-reported binge drinking (two or more) or driving after drinking, but no drug use; Drug use, drug use with no alcohol use in at least one year; Alcohol and drug, current alcohol and drug use.
Within the striped areas: Alcohol and drug, current alcohol and drug use; Alcohol use, current alcohol use without current drug use; Drug use, no alcohol use within past year, but current drug use; Alcoholism in recovery, no alcohol use within past year and no drug use.
Motivation to change alcohol use
Based on RTC responses, we categorized all 58 at-risk drinkers into one of three mutually exclusive stages of change. Seventeen (29.3%) were in the precontemplation phase, 15 (25.9%) were in the contemplation phase, and 26 (44.8%) were in the action phase (see Table 4). The mean readiness to change score was 3.5 (SD, 8.8).
Table 4.
Stage of change and interest in common change strategies among at-risk drinkers (n = 58)
| n (%) | |
|---|---|
| Proportion in each (highest) stage of change | |
| Precontemplation | 17 (29.3%) |
| Contemplation | 15 (25.9%) |
| Action | 26 (44.8%) |
| Preferred change strategies | |
| Want treatment | 22 (37.9%) |
| Wanting to try AA | 16 (27.6%) |
| Wanting to make changes on their own | 46 (79.3%) |
To examine whether alcohol problem severity was related to readiness to change, Pearson correlations were performed between readiness to change scores and alcohol problem indicators for at-risk drinkers. Greater readiness to change was significantly and positively associated with higher SMAST scores (r = 0.37, P < 0.01) and higher levels of physical dependency (r = 0.28, P < 0.05), but not with admission BAL (r = 0.12, ns) or total number of drinks per week (r = 0.11, ns).
Next, we examined the potential relationship between alcohol as a cause of injury, self as a cause of injury, and subsequent readiness to change. Participants were asked to rate the extent to which they thought alcohol or drugs were a cause of their injury as well as the degree to which they thought they were responsible for their injury. These ratings were correlated with readiness to change scores for at-risk drinkers. Attributing the cause of injury to alcohol or drugs was positively and significantly associated with readiness to change (Spearman's rho = 0.34, P < 0.02). There was a trend for attributing the cause of injury to oneself to be associated with greater readiness to change (Spearman's rho = 0.36, P = 0.05).
Preferred change strategies
Finally, we examined change strategies preferred by at-risk drinkers. Data concerning treatment preferences were available on 58 (96.7%) of the at-risk drinkers. Of these, 22 persons (37.9%) reported wanting alcohol treatment, 16 (27.6%) wanted to attend AA, and 46 (79.3%) reported wanting to change alcohol use on their own. Thirteen persons (22.4%) were interested in all three options and 24 (41.4%) were interested in either treatment or AA. Forty-seven (81.0%) at-risk drinkers expressed interest in at least one of the three change strategies, whereas 11 (19.0%) were uninterested in any strategy. Those who wanted to try AA or wanted treatment reported significantly more lifetime alcohol-related problems as reflected by SMAST scores (rho = 0.41 and 0.34, respectively, both P < 0.001). There was a trend for persons wanting to change on their own to have higher SMAST scores (rho = 0.24, P < 0.07). Preferred change strategies were unrelated to physical dependency scores, but wanting to change on one's own was associated positively with greater readiness to change (rho = 0.48, P < 0.01). Chi-square analyses indicated that persons classified as at-risk drinkers, who had a history of alcohol treatment, were significantly more likely to report wanting treatment or express interest in attending AA (P < 0.05). However, this group was no more likely to report wanting to change on their own than persons who had no history of alcohol treatment. Persons who self-identified as white were more likely than non-whites to prefer to change on their own. Preferred change strategies were unrelated to gender, age, education, vocational status, marital status, weekly alcohol consumption, or BAL.
Discussion
Alcohol use
Results of the current study are consistent with previous findings indicating widespread history of substance use among newly admitted patients with SCI. Nearly 40% of our total sample of inpatients reported a history of significant alcohol-related problems as measured by the SMAST. This rate of problem drinking is comparable to those of other studies of trauma patients assessed with the SMAST at our institution, including patients with TBI25 and general trauma.26 The results of this study are also consistent with other studies assessing alcohol problems among consecutive inpatients with SCI.1,3,16,17 Interestingly, rates of significant alcohol problems based on self-reports of consecutive inpatients appear much higher than estimates based on community surveys. Young et al.4 surveyed 123 community residents with SCI and found that 21% of respondents reported significant alcohol-related problems based on their SMAST scores. This rate was only slightly higher than the 16% found in a large community survey of the general population.27 These data likely indicate that there is a significant reduction in alcohol-related problems in the period following SCI. Severe medical problems, such as SCI, would be expected to trigger significant spontaneous reductions in rates of alcohol-related problems.28
Nearly one-third (31.5%) of the total sample was found to have a positive BAL at admission, a rate consistent with that reported by other studies assessing consecutive inpatients with SCI and TBI.1,3,29 The majority of patients with positive BALs (78.6%) were considered intoxicated at admission, a rate comparable to the 75% reported by McKinley's group.3 Seven participants showed admission BALs that were two to three times greater than the legal limit. Although BALs may appear to be a reliable and objective means of assessing problem drinking, increasing evidence suggests that this measure fails to identify many problem drinkers.26 In the current study, nearly half of persons classified as at-risk drinkers had admission BALs of zero. An additional 10% showed positive BALs that were below the legal limit of intoxication. Ideally, problem drinking should be assessed by both BAL and self-report measures to ensure that false negatives are minimized.
Drug use
High rates of concurrent alcohol and drug use were indicated by both self-report data and results of toxicity screens. Nearly one-third of the total sample reported using an illicit drug within the past 3 months. Marijuana was the most commonly reported drug (28.2%), followed by amphetamines (9.1%) and cocaine (6.4%). At-risk drinkers were significantly more likely to report using one or more drugs in the 3 months prior to injury. This is significant as other studies found the use of alcohol and illicit substances prior to injury may be a risk factor for post-injury medical complications such as cardiovascular disease, kidney and liver disorders, urinary tract infections, and development of pressure ulcers.7,8 Marijuana use has also been associated with higher rates of depressive symptoms and stress among community-dwelling individuals with SCI.4
Results of toxicology screens indicated that over one-quarter of the total sample tested positive for the presence of cocaine, amphetamines, or marijuana at admission, and one-third of these participants tested positive for two or more drugs. At-risk participants accounted for 100% of persons who tested positive for cocaine, 80% of persons who tested positive for marijuana, and 50% of persons who tested positive for amphetamines. In the only other study comparing self-report data on drug and alcohol use with results of toxicity screens, Heinemann et al.16 reported 58% agreement between self-reported drug use and the results of urine toxicology screens. We also found only moderate agreement between self-report of drug use and toxicology results. In the case of individuals who reported no drug use but had positive toxicology results, it is possible that the discrepancy may be due to unwillingness to report use of illicit drugs, comorbid TBI and associated amnesia, or false positive toxicology results. For individuals who reported drug use but showed negative toxicology results, the imperfect agreement between measures may be because toxicology results are valid only for a brief period and may not indicate non-recent drug use, whereas questionnaire items ask about drug use within the past 3 months. While imperfect, assessing illicit drug use by self-report appears to be a reasonable and efficient strategy. Questionnaire data were available for 95.8% of the sample, whereas toxicology results were available for only 69.7% of the sample. Although some patients may be unwilling or unable to report drug use, questionnaire data may also identify users that toxicology screens do not.
Overall, little is known about the medical and psychosocial impact of drug use among individuals with SCI and further investigation is certainly warranted. This is particularly true for marijuana use, as it is the most commonly used substance in this sample and is frequently used for pain and spasticity relief post-SCI.30
Treatment implications
As predicted, greater readiness to change preinjury patterns of alcohol use was associated significantly and positively with greater number of alcohol-related problems, as well as with attributing the cause of injury to alcohol use. A positive relationship between self-reported severity of alcohol-related problems and readiness to change has been reported in the primary care literature.31 These data seem to indicate appropriate problem recognition and concern about the need to change among those with greater self-reported alcohol-related problems. This contradicts the common belief that alcoholism is a disease of denial, requiring skepticism and confrontation on the part of the clinician. These data suggest instead a ‘teachable moment’, in which the crisis of severe injury may trigger self-reflection and openness to change drinking behavior. If the substantial interest in formal alcohol treatment and attending AA reported by our participants is replicated in other studies, this could provide the basis for strategic referrals. For patients who indicate interest in treatment, clinicians should be able to refer patients to an accessible treatment setting. Unfortunately, evidence suggests that many rehabilitation medicine physicians do not routinely ask about substance abuse. Of those who do, as many as 40% who diagnose individuals with substance use disorders do not refer for treatment.32 To aid in this process, the federal Substance Abuse and Mental Health Services Administration maintains a website for locating substance abuse treatment services throughout the country (http://dasis3.samhsa.gov/). For patients wishing to attend AA, clinicians could assist the patient in finding convenient and appropriate meetings following discharge or even during rehabilitation, if available. Parallel counseling may also help facilitate the person's effective use of AA.33 A detailed therapy manual has been written for this purpose and is available through the National Institute on Alcohol Abuse and Alcoholism web page: (http://pubs.niaaa.nih.gov/publications/match.htm). Persons interested in self-change may be receptive to and benefit from brief interventions to bolster motivation to change or education regarding relapse prevention skills. Recent research regarding unassisted recovery from alcoholism indicates that self-change may be an effective strategy for some patients. Many patients may benefit from self-help guides.34,35
Several evidence-based approaches to reducing substance abuse in medical settings may be appropriate in rehabilitation settings. For example, a recent Cochrane review of 28 controlled trials indicates that brief interventions characterized mainly by feedback and advice delivered by primary care physicians or other health care workers is associated with significant reductions in drinking lasting 1 year.36 The National Institute on Alcohol Abuse and Alcoholism has developed a useful resource for primary care physicians who wish to advise patients about problem drinking. It can be obtained from the NIAA at http://www.niaaa.nih.gov/Publications/EducationTrainingMaterials/default.htm.
Motivational interviewing has been tested as a health behavior change approach in over 70 randomized controlled trials and produces an average between-groups effect size of 0.26 SD in alcohol-related outcomes.37 Motivational interviewing can be successful regardless of the person's initial stage of change and is thought to be more effective among people with characteristics suggesting greater initial anger or resistance.38 Although no randomized clinical trials of motivational interviewing have been conducted with patients in acute rehabilitation, motivational interviewing has been used successfully in both emergency medical39 and acute inpatient medical settings.40 Consequently, motivational interviewing appears to be a promising approach to reducing the rate of alcohol abuse following SCI rehabilitation and should be studied in randomized controlled trials with SCI rehabilitation populations.
At-risk substance use in this population occurs at a very high frequency, has a significant negative impact on psychosocial and medical outcomes,6–9,11 and presents an opportunity for change in the form of hospitalization for SCI; as such, it would behoove providers regularly working with SCI rehabilitation populations to be aware of available resources and obtain adequate training on working with individuals with substance abuse problems. Of additional note, individuals with a new SCI who regularly use alcohol and drugs face one of the most challenging events of their lives in inpatient rehabilitation without a frequently used coping mechanism, however ineffective it may be. Balancing lifestyle change with the trials of rehabilitation can be a process that may be aided by additional support in the form of rehabilitation psychology or social work.
Limitations
Several limitations of this study should be noted. First, this study was conducted within a single rehabilitation unit of an urban level 1 Trauma center in the Pacific Northwest. For example, 70% of the subjects were men who described themselves as white. These results may not generalize to other racial or ethnic groups, women, types of rehabilitation centers, or geographic areas.
Another limitation of this study is that several key variables, including at-risk drinking, were assessed by self-report. Self-reports are subject to numerous biases; social desirability can be especially problematic among substance users. However, studies among both rehabilitation patients and the general population suggest that persons with alcohol and other drug problems provide reliable and valid reports if interviewed in clinical settings, when they are alcohol free, and when they are given reassurances of confidentiality.41,42 Each of these conditions was met in the present study. To increase validity, future studies of preinjury alcohol and drug use among SCI patients might include collateral reports of significant others or caregivers.
This study is also limited by the lack of a standardized diagnostic measure for alcohol abuse or dependence. The SMAST is a brief screening measure that appears useful for indicating problem drinking. However, it is not a diagnostic measure and cannot be used to determine whether cases meet criteria for DSM-IV diagnosis. Future studies might address this issue by including a formal diagnostic measure for alcohol abuse or dependence such as a structured interview based on the DSM-IV. Also, researchers might consider including other screening measures such as the Alcohol Use Disorders Screening Test.43 Developed by the World Health Organization for use in primary care and other medical settings, this 10-item measure provides a single risk score assessing alcohol use, alcohol-related problems, and symptoms of alcohol dependence.
Conclusion
Acute rehabilitation for SCI represents an important opportunity to identify and intervene with persons who have a history of substance abuse. The results of this study confirm that high rates of alcohol and drug problems are common among inpatients with recent SCI. We recommend that routine screening for substance abuse be included in comprehensive rehabilitation care, since as needed screening is likely to be biased.44 Identification of drug and alcohol problems in this population may help identify patients who are at-risk for poorer rehabilitation progress and lower discharge functional independence5 as well as those at-risk for decubitus ulcers and urinary tract infections.7,8 Moreover, brief opportunistic interventions and strategic referrals may help reduce relapse. Rational guidelines already exist for tailoring types and levels of treatment to patient variables.22 At a minimum, at-risk patients with SCI should be educated about the effects of alcohol and other drug use after neurologic injury.45 They may also benefit from physician advice to abstain from alcohol and other drugs. Optimally, at-risk persons should receive brief interventions by psychology or social work staff to attempt to reduce the risk of post-injury complications associated with substance abuse. The current data suggest the majority of persons with SCI and a history of alcohol problems are already thinking about changing their drinking behavior and are open to at least contemplating abstinence or moderation. Depending on patient preferences, brief interventions can function as stand-alone treatments for those who want to change on their own or as a way to promote referral to formal substance abuse treatment or AA. Controlled research is needed to establish an evidence base for substance abuse intervention approaches within SCI rehabilitation and to help SCI programs and clinical staff recognize this important opportunity for secondary prevention of substance abuse problems.
Acknowledgements
This research was supported by the Northwest Regional Spinal Cord Injury System grant and funded by the National Institute on Disability and Rehabilitation Research (H133N50025; H133N060033). The contents of this paper are solely the responsibility of the authors and do not represent the official views of the granting agency. No commercial party having a direct financial interest in the results of the research has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
References
- 1.Bombardier CH, Rimmele C. Alcohol use and readiness to change after spinal cord injury. Arch Phys Med Rehabil 1998;79(9):1110–5 [DOI] [PubMed] [Google Scholar]
- 2.Kolakowsky-Hayner SA, Gourley EV, III, Kreutzer JS, Marwitz JH, Meade MA, Cifu DX. Post-injury substance abuse among persons with brain injury and persons with spinal cord injury. Brain Inj 2002;16(7):583–92 [DOI] [PubMed] [Google Scholar]
- 3.McKinley WO, Kolakowsky SA, Kreutzer JS. Substance abuse, violence, and outcome after traumatic spinal cord injury. Am J Phys Med Rehabil 1999;78(4):306–12 [DOI] [PubMed] [Google Scholar]
- 4.Young M, Rintala D, Rossi C, Hart K, Fuhrer M. Alcohol and marijuana use in a community-based sample with spinal cord injury. Arch Phys Med Rehabil 1995;76(6):525–32 [DOI] [PubMed] [Google Scholar]
- 5.Bombardier CH, Stroud M, Esselman P, Rimmele CT. Do preinjury alcohol problems predict poorer rehabilitation progress in persons with spinal cord injury? Arch Phys Med Rehabil 2004;85(9):1488–92 [DOI] [PubMed] [Google Scholar]
- 6.Heinemann A, Goranson N, Ginsberg K, Schnoll S. Alcohol use and activity patterns following spinal cord injury. Rehabil Psychol 1989;34(10):191–206 [Google Scholar]
- 7.Elliott TR, Kurylo M, Chen Y, Hicken B. Alcohol abuse history and adjustment following spinal cord injury. Rehabil Psychol 2002;47(3):278–90 [Google Scholar]
- 8.Heinemann A, Hawkins D. Substance abuse and medical complications following spinal cord injury. Rehabil Psychol 1995;40(2):125–41 [Google Scholar]
- 9.Boakye M, Patil CG, Santarelli J, Ho C, Tian W, Lad SP. Laminectomy and fusion after spinal cord injury: National inpatient complications and outcomes. J Neurotrauma 2008;25(3):173–83 [DOI] [PubMed] [Google Scholar]
- 10.Hollingworth W, Relyea-Chew A, Comstock BA, Overstreet JKA, Jarvik JG. The risk of bankruptcy before and after brain or spinal cord injury: a glimpse of the iceberg's tip. Med Care 2007;45(8):702–11 [DOI] [PubMed] [Google Scholar]
- 11.Heinemann A, Doll MD, Armstrong KJ, Schnoll S, Yarkony GM. Substance use and receipt of treatment by persons with long-term spinal cord injuries. Arch Phys Med Rehabil 1991;72(7):482–7 [PubMed] [Google Scholar]
- 12.Banerjea R, Findley PA, Smith B, Findley T, Sambamoorthi U. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord 2009;47(11):789–95 [DOI] [PubMed] [Google Scholar]
- 13.Krause JS, Carter RE, Pickelsimer E. Behavioral risk factors of mortality after spinal cord injury. Arch Phys Med Rehabil 2009;90(1):95–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Go BK, DeVivo MJ, Richards JS. The epidemiology of spinal cord injury. In: Stover S, DeLisa JA, Whiteneck GG. (eds.) Spinal cord injury: clinical outcomes from the model systems. Gaithersburg, MD: Aspen; 1995. p. 21–55 [Google Scholar]
- 15.Tate DG. Alcohol use among spinal cord injured patients. Am J Phys Med Rehabil 1993;72(4):192–5 [DOI] [PubMed] [Google Scholar]
- 16.Heinemann A, Schnoll S, Brandt M, Maltz R, Keen M. Toxicology screening in acute spinal cord injury. Alcoholism: Clin Exp Res 1988;12(6):815–9 [DOI] [PubMed] [Google Scholar]
- 17.Rothstein JL, Levy E, Fecher R, Gordon SK, Bauman WA. Drug use and abuse in an urban veteran spinal cord injured population. J Am Paraplegia Soc 1992;15(4):217–20 [DOI] [PubMed] [Google Scholar]
- 18.McKay JR. Studies of factors in relapse to alcohol, drug and nicotine use: a critical review of methodologies and findings. J Stud Alcohol 1999;60(4):566–76 [DOI] [PubMed] [Google Scholar]
- 19.Miller WR, Marlatt GA. The brief drinker profile. Odessa, FL: Psychological Assessment Resources; 1987 [Google Scholar]
- 20.Selzer M, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST). J Studies Alcohol 1975;36(1):127–32 [DOI] [PubMed] [Google Scholar]
- 21.Dikmen SS, Donovan D, Loberg T, Machamer J, Temkin NR. Alcohol use and its effects on neuropsychological outcome in head injury. Neuropsychology 1993;7(3):296–305 [Google Scholar]
- 22.Turner AP, Bombardier CH, Rimmele CT. A typology of alcohol use patterns among persons with recent TBI or SCI: Implications for treatment matching. Arch Phys Med Rehabil 2003;84(3):358–64 [DOI] [PubMed] [Google Scholar]
- 23.Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict Alcohol Other Drugs 1992;87(5):743–54 [DOI] [PubMed] [Google Scholar]
- 24.Heather N, Rollnick S, Bell A. Predictive validity of the readiness to change questionnaire. Addiction 1993;88(12):1667–77 [DOI] [PubMed] [Google Scholar]
- 25.Bombardier CH, Ehde D, Kilmer J. Readiness to change alcohol drinking habits after traumatic brain injury. Arch Phys Med Rehabil 1997;78(6):592–6 [DOI] [PubMed] [Google Scholar]
- 26.Rivara FP, Jurkovich GJ, Gurney JG, Seguin D, Fligner CL, Ries R, et al. The magnitude of acute and chronic alcohol abuse in trauma patients. Arch Surg 1993;128(8):907–12 [DOI] [PubMed] [Google Scholar]
- 27.Harburg E, Gunn R, Gleibermann L, Roeper P, DiFrancisco W, Caplan R. Using the Michigan Alcoholism Screening Test to study social drinkers: Tecumseh, Michigan. J Stud Alcohol 1988;49(6):522–31 [DOI] [PubMed] [Google Scholar]
- 28.Tucker JA, Vuchinich RE, Gladsjo JA. Environmental events surrounding natural recovery from alcohol-related problems. J Stud Alcohol 1994;55(4):401–11 [DOI] [PubMed] [Google Scholar]
- 29.Bombardier CH, Rimmele CT, Zintel H. The magnitude and correlates of alcohol and drug use before traumatic brain injury. Arch Phys Med Rehabil 2002;83(12):1765–73 [DOI] [PubMed] [Google Scholar]
- 30.Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med 2006;29(2):109–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams EC, Kivlahan DR, Saitz R, Merrill JO, Achtmeyer CE, McCormick KA, et al. readiness to change in primary care patients who screened positive for alcohol misuse. Ann Family Med 2006;4(3):213–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.West SL, Luck RS, Capps CF, Cifu DX, Graham CW, Hurley JE. Alcohol/other drug problems screening and intervention by rehabilitation physicians. Alcoholism Treatment Q 2009;27(3):280–93 [Google Scholar]
- 33.Project MATCH Research Group Matching alcoholism to client heterogeneity: Project MATCH post-treatment drinking outcomes. J Stud Alcohol 1997;58(1):7–29 [PubMed] [Google Scholar]
- 34.Kishline A. Moderate drinking the moderation management guide for people who want to reduce their drinking. New York: Crown Trade Paperbacks; 1994 [Google Scholar]
- 35.Miller WR, Munoz RF. How to control your drinking. Revised edition Albuquerque: University of New Mexico Press; 1990 [Google Scholar]
- 36.Kaner Eileen FS, Dickinson Heather O, Beyer Fiona R, Campbell F, Schlesinger C, Heather N, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev [serial on the Internet]. 2007;(2): Available from: http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD004148/frame.html [DOI] [PubMed] [Google Scholar]
- 37.Hettema J, Steele J, Miller WR. Motivational Interviewing. Annu Rev Clin Psychol 2005;1:91–111 [DOI] [PubMed] [Google Scholar]
- 38.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 2nd ed. New York, NY: The Guilford Press; 2002 [Google Scholar]
- 39.Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol 1999;67(6):989–94 [DOI] [PubMed] [Google Scholar]
- 40.Gentilello L, Rivara F, Donovan D, Jurkovich G, Daranciang E, Dunn C, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surgery 1999;230(4):473–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Babor TF, Brown J, Del Boca FK. Validity of self-reports in applied research on addictive behaviors: fact or fiction? Addict Behav 1990;12(1):5–32 [Google Scholar]
- 42.Sander A, Witol A, Kreutzer J. Concordance of patients’ and caregivers’ reports of alcohol use after traumatic brain injury. Arch Phys Med Rehabil 1997;78(11):138–42 [DOI] [PubMed] [Google Scholar]
- 43.Allen J, Litten R, Fertig J, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcoholism: Clin Exp Res 1997;21(4):613–9 [PubMed] [Google Scholar]
- 44.Gentilello L, Villaveces A, Ries RR, Nason KS, Daranciang E, Donovan DM, et al. Detection of acute alcohol intoxication and chronic alcohol dependence by trauma center staff. J Trauma 1999;47(6):1131–9 [DOI] [PubMed] [Google Scholar]
- 45.Bombardier CH. Management of substance abuse after trauma. In: Robinson LR. (ed.), Trauma Rehabilitation Philadelphia, PA: Lippincott, Williams & Wilkins; 2005. 225–244 [Google Scholar]