Abstract
Objective: To determine the incidence of major depressive disorder, bipolar disorder, panic disorder, social anxiety disorder, and generalized anxiety disorder and to assess their detection rates in the Canadian primary care setting.
Method: The descriptive, cross-sectional study was conducted in 7 primary care clinics in 3 Canadian provinces, Ontario, British Columbia, and Nova Scotia, from December 6, 2005, to May 5, 2006. Patients in clinic waiting rooms who consented to participate in the study were administered the Mini International Neuropsychiatric Interview (MINI) (N = 840). These patients' medical charts were then reviewed for evidence of previous diagnosis of a mood or anxiety disorder. Misdiagnosis was defined as cases for which a diagnosis was reached on the MINI but not in the patient's chart.
Results: Of the 840 primary care patients assessed, 27.2%, 11.4%, 12.6%, 31.2%, and 16.5% of patients met criteria for major depressive disorder, bipolar disorder, panic disorder, generalized anxiety disorder, and social anxiety disorder, respectively. Misdiagnosis rates reached 65.9% for major depressive disorder, 92.7% for bipolar disorder, 85.8% for panic disorder, 71.0% for generalized anxiety disorder, and 97.8% for social anxiety disorder.
Conclusions: With high prevalence rates and poor detection, there is an obvious need to enhance diagnostic screening in the primary care setting.
Mood and anxiety disorders, including depression (major depressive disorder), dysthymia, bipolar disorder, generalized anxiety disorder, social anxiety disorder, panic disorder, and agoraphobia, are reported to be the most common mental illnesses and affect almost 30% of the US population.1 The functional limitations of mental health disorders translate into significant professional and societal costs, estimated to be $14–$38 billion in Canada.2,3 The latter figure includes cost of physician visits, hospitalizations, morbidity and mortality, and other related costs such as social welfare administration. According to “The Economic Burden of Anxiety Disorders,” a study commissioned by the Anxiety Disorders Association of America, anxiety disorders cost almost one-third of the $148 billion total mental health bill for the United States.4 More than $22.8 billion of these costs are associated with the repeated use of health care services, as those individuals suffering with anxiety disorders often seek relief for symptoms that mimic physical illnesses.4 In the World Health Organization (WHO) study Psychological Problems in General Health Care, researchers found that patients suffering from depression more often presented to their primary care physicians with physical complaints than with psychological ones.5
In fact, it has been reported that people with an anxiety disorder are 3 to 5 times more likely than those without to visit their doctor,6 but their symptoms are often attributed to physical causes. Such is the case with depression, for which core symptoms of the disorder such as fatigue, decreased energy, and a lack of motivation are often misinterpreted by the primary care physician to be the result of physical causes.7 In many cases, the primary care physician may be distracted by the presence of physical complaints or may feel too pressed for time or may not be qualified to probe into mental health problems.8 Therefore, the challenge is to provide accurate early detection and identification of people who are at increased risk for developing mood and anxiety disorders so that they may receive appropriate treatment.
Despite the severity and disabling nature of these disorders, many individuals are often misdiagnosed or undiagnosed by physicians, resulting in self-medication, higher incidence of substance abuse, frequent use of medical services, inappropriate treatment, and social isolation, as well as educational and occupational impairment.9,10 People may suffer from anxiety disorders for years before receiving appropriate treatment, resulting in significant morbidity for those who suffer from these disorders in addition to social and economic costs.
While there is considerable literature suggesting that we are making strides toward facilitating effective treatments for mood and anxiety disorders,11 a variety of studies have suggested that the correct diagnosis of mood and anxiety disorders is lacking in the primary care setting.7,8,12,13 Failure to properly diagnose these disorders is related not only to the insufficient training of clinicians in this area, but also to limited duration of appointments, examinations focused on physical aspects of a patient's condition, and insufficient rapport building.9,14 Furthermore, the diagnostic tools available are often not used by physicians, as they are lengthy and time consuming and must be administered by a trained clinician.9,15
PREVALENCE RATES OF MOOD AND ANXIETY DISORDERS
Various studies have reported high prevalence rates of psychiatric disorders in primary care. The WHO Collaborative Study of Psychological Problems in General Health found that 10.4% of the 26,000 patients screened met criteria for current depression.16,17 In other studies, major depressive disorder has been shown to be one of the most common mental disorders seen in primary care patients, with prevalence rates ranging from 23% to 35%.18–21 It has been estimated that 80% of people with major depressive disorder are treated entirely in the primary care setting, resulting in depression being one of the most prevalent and fastest rising disorders in primary care.22 In comparison, lifetime prevalence rates of bipolar disorders are estimated to range from 1% to 5% in the general population,23 although the prevalence of bipolar spectrum disorders may be as high as 6.5% in adults.23
With respect to panic disorder, the National Comorbidity Survey found the lifetime prevalence in the United States to be 4.7%.24 The prevalence of current (1 month) panic disorder meeting full criteria was between 6.7% and 8.3% in the primary care setting,25 whereas lifetime prevalence rates reached up to 13% in this specific setting.26–29
The lifetime prevalence of generalized anxiety disorder was found to be 5.1%.30 Generalized anxiety disorder is the most frequent anxiety disorder in primary care, with 5.8% to 22.0% of primary care patients complaining of anxiety problems, which suggests that these patients are high users of primary care resources.31–33 In fact, the prevalence of generalized anxiety disorder in primary care could be twice that in the general population. The estimated prevalence of generalized anxiety disorder in general medical practice was 2.8% to 8.5%,9,32,34,35 while it ranged from 1.6% to 5.0% in the general community.35–37
Finally, in terms of social anxiety disorder, research has revealed a 12-month prevalence rate of 7.9% and a lifetime prevalence rate of 13.3%.38,39 This condition is associated with higher rates of health care use, as well as psychiatric comorbidity, particularly major depressive disorder, alcohol abuse, and suicide attempts.7,40 Social anxiety disorder is the most prevalent of any anxiety disorder and is the third most common psychiatric disorder behind depression and alcohol abuse.40 Social anxiety disorder is also prevalent in the primary care setting, with a lifetime prevalence of 14.4%.5,41
Despite the high prevalence of mood and anxiety disorders, few patients are screened and diagnosed appropriately. Indeed, recent studies suggest that a quarter of psychiatrists and half of primary care physicians often do not use Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for major depressive disorder when diagnosing depression.42 Furthermore, despite the availability of several validated, easy-to-administer scales that can facilitate diagnosis and monitoring of outcomes in patients with mood disorders, they are not routinely used by the majority of clinicians.43 This is despite guideline recommendations supporting the routine use of validated outcome scales such as the 9-item Patient Health Questionnaire (PHQ-9), the Quick Inventory of Depressive Symptomatology Self-Rated (QIDS-SR), the Beck Depression Inventory (BDI), or the Center for Epidemiologic Studies Depression Rating Scale (CES-D) to assess and monitor patients being treated for depression.44,45
Research studies indicate that general practitioners recognize mood disorders at chance levels, and, accordingly, between 50% to 70% of depressive episodes go undetected by physicians.46 The detection rates for bipolar disorder,23 panic disorder,47 generalized anxiety disorder,48 and social anxiety disorder41 range from 0.5% (social anxiety disorder) to 50% (bipolar disorder). The low detection rates for mental health disorders in primary care are mirrored by poor quality of care. For instance, only a third to half of patients with anxiety disorders receive appropriate treatment in primary care.49,50
These findings highlight the need for evidence-based practice guidelines and effective screening tools. Given that mood and anxiety disorders are relatively common and associated with considerable impairment, there is clearly a need to examine how well they are being diagnostically detected in real-world clinical practice. The present study is unique, as it was designed to assess the rates of diagnosis of mental disorders specifically within the Canadian primary care population. It is the authors' hope to facilitate the efforts of primary care physicians, to enhance the diagnosis of these disorders, and, in the long term, to improve treatment of those suffering from these illnesses in primary care in Canada.
METHOD
This multicenter descriptive, cross-sectional study was conducted in 7 primary care practice settings in 3 Canadian provinces, Ontario, British Columbia, and Nova Scotia, from December 6, 2005, to May 5, 2006. These sites were selected by contacting various site clinic directors directly at their primary care practices. Upon interest shown by the clinic director in the study, subsequent meetings were arranged to discuss requirements and the study time commitments required. Requirements for a study site to be enrolled entailed the following: consent to approach all English-speaking patients in their clinic's waiting room to participate in the study, available room to facilitate the diagnostic interview, access to patient charts, and space provided to conduct all relevant chart reviews. This original research was approved by Optimum Ethics Research Board in Oshawa, Ontario, Canada.
Participants
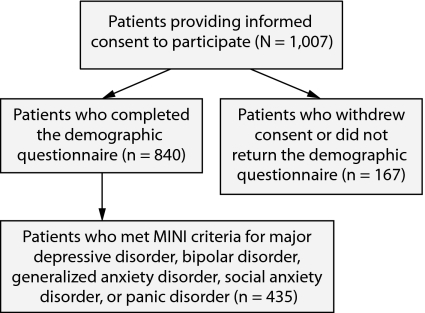
Participants were recruited from physician clinics' waiting rooms over a 6-month period. Intensity of recruitment varied by clinic, and assessors' presence ranged from 2 to 7 days per week. All English-speaking patients over the age of 18 years, who were able to give informed consent, and who had presented to the clinic for an appointment with their primary care physician were eligible and offered an opportunity to participate in this study. A sample of 1,007 eligible subjects indicated interest to participate in the study, gave informed consent, and were asked to submit a demographic questionnaire (Appendix 1). From this recruited, consenting sample, 167 subjects withdrew consent or submitted incomplete demographic information. Reasons for withdrawing consent included subjects having time constraints, being preoccupied with current child care needs, being called in for their appointment by their physician, or feeling ill. Participants' names were recorded on a spreadsheet to avoid duplication of cases. As a result, a sample of 840 subjects underwent phase 1 of the study and were administered the Mini International Neuropsychiatric Interview (MINI).51 From this sample, 435 subjects met criteria on the MINI diagnostic interview for 1 or more of the following diagnoses: major depressive disorder, bipolar disorder, generalized anxiety disorder, social anxiety disorder, or panic disorder (Figure 1). No data are available on participants who declined participation, as they did not provide informed consent.
Figure 1.
Subjects' Participation in Various Phases of Recruitment During the Study
Abbreviation: MINI = Mini International Neuropsychiatric Interview.
Interviewers, Training Procedure, and Supervision
Interviewers were psychology students with bachelor's, master's, or doctorate (PsyD) degrees. In total, 4 examiners were trained. All underwent an extensive training period of approximately 1 week. During the training, the different disorders were explained, emphasizing DSM-IV52 criteria and differential diagnosis. All MINI51 sections were practiced, and prefield training was completed, which was then followed by the rating of 5 practice interviews before starting fieldwork. All interviewers were supervised weekly. Furthermore, all interviews were audio recorded, and the recordings were sampled randomly for assessment of validity and reliability of the assessment (by M.K. and M.V.). Interviews wherein disagreement existed between the reviewer and the interviewer were discussed, and a consensus diagnosis was given. Data were entered into an SPSS, version 14.0 spreadsheet (IBM Corporation, Somers, New York) and then rechecked for any errors in entry.
Materials
Mini International Neuropsychiatric Interview (MINI).
The MINI is a short, semistructured diagnostic inventory for DSM-IV and ICD-10 psychiatric disorders. The MINI has good reliability and validity as compared to the Composite International Diagnostic Interview and the Structured Clinical Interview for DSM-IV (SCID).51 The MINI has high reliability for all disorders examined in the present study, with an interrater reliability κ of 0.98.51
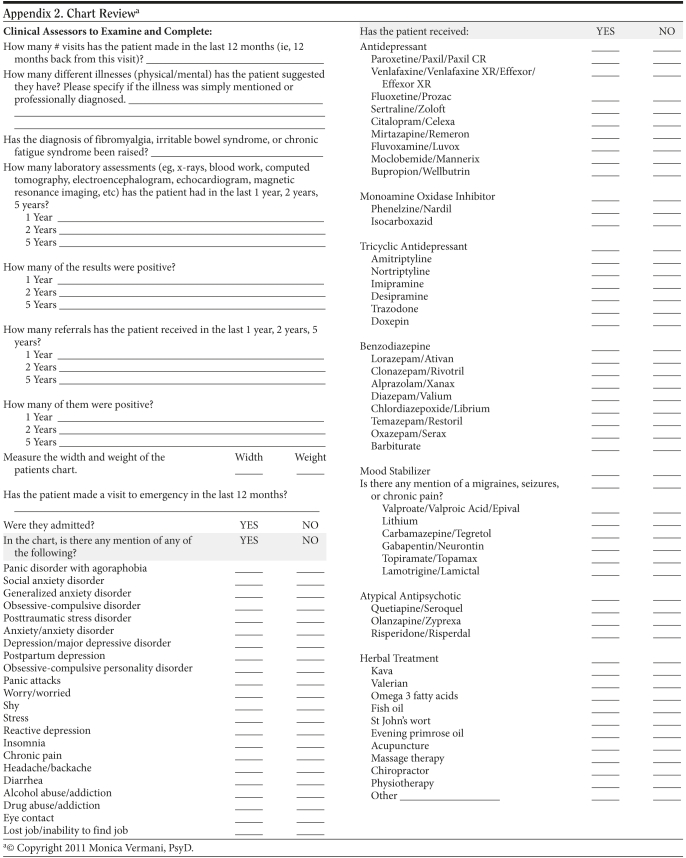
Chart review.
The reviewers were trained to examine the chart of every patient currently meeting criterion for depression, bipolar disorder, panic disorder, generalized anxiety disorder, or social anxiety disorder on the MINI in order to examine the rate of diagnosis detection by primary care physicians. The chart reviewers examined notes from the past 12 months for any mention of a specific diagnosis (Appendix 2). The words that were used to define an accurate diagnosis of each disorder are as follows: (1) depression, major depressive disorder, or major depressive episode; (2) bipolar, mania, hypomania, or bipolar affective disorder; (3) panic disorder, panic attacks, panic disorder with agoraphobia, agoraphobia; (4) anxiety, generalized anxiety disorder; and (5) social phobia, social anxiety disorder. Rates of accurate and inaccurate diagnosis were recorded.
In addition, the presence of keywords in patients' charts was examined and used as indicators that might suggest partial diagnosis by the primary care physicians. This list of words included worry, stress, insomnia, chronic pain, headache, backache, diarrhea, alcohol abuse/addiction, drug abuse/addiction, and eye contact. Prescriptions were not used to make a diagnosis because there are many off-label uses of psychiatric medications.53 However, the use of antidepressants, mood stabilizers, and atypical antipsychotics was included in the list of suggestive words. The complete list is available in Appendix 1.
Research Protocol/Procedures
Trained clinical assessors were randomly sent to physician offices in order to facilitate procedures for the following study until the recruitment of required subjects was completed. Patients who gave informed consent were then administered the MINI51 as a structured clinical interview in order to make an objective diagnosis for current and lifetime diagnoses. Subsequently, the clinical assessors reviewed the physicians' clinical medical charts/file information pertaining to the subjects who had a MINI diagnosis in search of any notes confirming the diagnosis of the chronic disorders of social anxiety disorder, generalized anxiety disorder, panic disorder, bipolar disorder, and major depressive disorder.
Statistical Analysis
SAS software, version 9.1 (SAS Institute, Cary, North Carolina) was used to perform statistical analysis. T tests were used to assess differences between subjects with and without a MINI diagnosis. Selected keywords were tested for association with specific diagnoses. Pearson's goodness-of-fit χ2 statistic or Fisher exact tests (for cells that had less than 5 counts) were calculated on nonmissing values. Statistical significance was accepted at α < .05.
RESULTS
Baseline characteristics of participants with and without a MINI diagnosis are reported in Table 1. Participants with a MINI diagnosis were on average younger than those with no MINI diagnosis: 34 and 41 years of age, respectively (P < .01). These subjects were also less likely to have completed some postsecondary education, with 51% reporting having a college education, bachelor's, master's, or higher degree, compared to 69% among those with no MINI diagnosis (P < .01). It was noted that those with 1 or more MINI diagnoses were also less likely to be with a partner (cohabiting or married: 42%) compared to those without a MINI diagnosis (56%, P < .01). Moreover, those with a MINI diagnosis generally had a lower annual income than those without a MINI diagnosis (P < .01). Lastly, there were no significant differences in the status of employment or ethnicity between the 2 groups.
Table 1.
Demographic Characteristics of Participants With and Without a Mini International Neuropsychiatric Interview (MINI) Diagnosis
| Characteristics | All Phase 1 Participants | Subjects With No Diagnoses | Subjects With MINI Diagnosis (Phase 2) |
| Subjects, n | 840 | 406 | 435 |
| Age, mean (SD), ya | 37 (16) | 41 (17) | 34 (14) |
| Female, %a | 72.7 | 69.6 | 75.6 |
| Education, %a | |||
| Elementary/high school/some postsecondary | 40.1 | 31.1 | 48.6 |
| College/bachelor's/master's/PhD/equivalent | 59.9 | 68.9 | 51.4 |
| Marital status, %a | |||
| Single/divorced/separated/widowed | 51.4 | 44.5 | 57.7 |
| Cohabiting/married | 48.6 | 55.5 | 42.3 |
| Annual income, %a | |||
| $10,000–$39,999 | 27.5 | 20.9 | 33.7 |
| $40,000–$80,000 | 35.1 | 35.9 | 34.4 |
| > $80,000 | 37.5 | 43.3 | 32.0 |
| Education/employment, % | |||
| Full-time or part-time out of home/school | 74.1 | 73.5 | 74.8 |
| Home/unemployed/no school/no work/on leave/retired | 25.8 | 26.6 | 25.2 |
| Ethnicity | |||
| European | 51.0 | 51.5 | 50.4 |
| Canadian | 12.5 | 15.8 | 9.5 |
| South Asian | 6.1 | 5.7 | 6.4 |
| East Asian | 5.6 | 6.7 | 4.5 |
| Caribbean | 4.3 | 3.9 | 4.7 |
| Otherb | 20.5 | 16.4 | 24.5 |
Indicates that there were significant differences (P < .01) between the groups with and without a MINI diagnosis.
Includes Latin American, Native American, Filipino, or West Asian, with no individual group representing more than 5% of the sample.
Table 2 reports the rates of diagnosis and detection of mood and anxiety disorders by primary care physicians. Of 840 MINI interviews, 435 patients were diagnosed with at least 1 condition. The most prevalent conditions were generalized anxiety disorder (262/840: 31.2%) and major depressive disorder (229/840: 27.2%). The detection rates by physicians were found to be considerably low. Specifically, from the 229 individuals who met the criteria for major depressive disorder, slightly more than a third (n = 78) had been correctly detected by primary care physicians. With respect to bipolar disorder, panic disorder, generalized anxiety disorder, and social anxiety disorder, a small proportion of patients were detected by physicians. The detection rates for generalized anxiety disorder (n = 262), panic disorder (n = 106), bipolar disorder (n = 96), and social anxiety disorder (n = 139) were 29.0%, 14.2%, 7.3%, and 2.2%, respectively.
Table 2.
Rates of Detection and Misdiagnosis of Anxiety and Mood Disorders by Primary Care Physicians
| Phase 1a | Phase 2b | ||||
| Disorder | Meeting Criteria on MINI, n (%)c | No. With Exact Diagnosis by Physician, n (%)d | Not Exactly Detected by Physicians, % | No. With Any Psychiatric Diagnosis by Physician | Nondetection by Physicians, % |
| Major depressive disorder | 229 (27.2) | 78 (34.1) | 65.9 | 24 | 55.5 |
| Bipolar disorder | 96 (11.4) | 7 (7.3) | 92.7 | 42 | 49.0 |
| Panic disorder | 106 (12.6) | 15 (14.2) | 85.8 | 47 | 41.5 |
| Generalized anxiety disorder | 262 (31.2) | 76 (29.0) | 71.0 | 42 | 55.0 |
| Social anxiety disorder | 139 (16.5) | 3 (2.2) | 97.8 | 23 | 81.3 |
Analysis includes all patients who were administered the MINI.
Analysis includes cases for which any diagnosis of mood and anxiety disorder was made in the chart, but the specific disorder was different than the one diagnosed by the MINI.
Includes patients meeting MINI criteria within this primary care setting.
Includes patients whose diagnosis on the MINI was in concordance with information contained in the patient's chart.
Abbreviation: MINI = Mini International Neuropsychiatric Interview.
It is plausible that primary care physicians recognized patients suffering from mood and anxiety disorders without necessarily reaching the most accurate diagnosis. To account for this possibility, a second phase of analysis included all charts that mentioned any mood or anxiety disorder, whether or not it matched the MINI information. Despite the additional inclusion of these cases, the rate of nonrecognition by primary care physicians remained substantial: 55.5%, 49.0%, 41.5%, 55.0%, and 81.3% for major depressive disorder, bipolar disorder, panic disorder, generalized anxiety disorder, and social anxiety disorder, respectively (Table 2).
Finally, charts were evaluated for keywords describing those patients who had received a MINI diagnosis, but who had not been recognized by their primary care physician as suffering from an anxiety or mood disorder. Table 3 highlights that, although primary care physicians may have been cautious to make a diagnosis, some symptoms were recognized. In all nondiagnosis cases (n = 188), 21.8% had a mention of headache/backache in their charts. Similarly, stress, diarrhea/constipation, and insomnia were recognized in 18.1%, 15.4%, and 12.8% of charts, respectively. Similar trends were noticeable when looking at specific disorders (Table 3).
Table 3.
Frequency of Recognition of Symptoms Associated With Mood and Anxiety Disorders in Patients Who Received a MINI Diagnosis But Whose Charts Did Not Mention Any Mood or Anxiety Disordeab
| Symptom | Social Anxiety Disorder/Social Phobia (n = 67) | Generalized Anxiety Disorder (n = 111) | Panic Disorder (n = 29) | Major Depressive Disorder (n = 69) | Bipolar Disorder (n = 38) | All Nondiagnoses (n = 188) |
| Worry | 6 (9) | 8 (7) | 2 (7) | 4 (6) | 1 (3) | 12 (6) |
| Shy | 0 | 0 | 0 | 0 | 0 | 0 |
| Stress | 9 (13) | 26 (23) | 8 (28) | 13 (19) | 7 (18) | 34 (18) |
| Insomnia | 10 (15) | 13 (12) | 4 (14 | 11 (16) | 6 (16) | 24 (13) |
| Chronic pain | 4 (6) | 13 (12) | 8 (28) | 11 (16) | 5 (13) | 21 (11) |
| Headache/backache | 14 (21) | 23 (21) | 11 (38) | 16 (23) | 15 (40) | 40 (22) |
| Diarrhea/constipation | 10 (15) | 18 (16) | 5 (17) | 13 (19) | 7 (18) | 29 (15) |
| Alcohol use/addiction | 3 (5) | 7 (6) | 3 (10) | 6 (9) | 2 (5) | 8 (4) |
| Drug use/addiction | 0 | 1 (1) | 0 | 1 (2) | 0 | 1 (1) |
| Eye contact | 0 | 1 (1) | 0 | 0 | 0 | 1 (1) |
| Lost job/inability to find a job | 1 (2) | 1 (1) | 0 | 1 (2) | 0 | 1 (1) |
| Other stressor | 8 (12) | 12 (11) | 3 (11) | 0 | 5 (13) | 19 (10) |
| Use antidepressant medication | 5 (8) | 6 (5) | 0 | 1 (2) | 1 (3) | 8 (4) |
| Use mood stabilizer | 2 (3) | 0 | 0 | 8 (12) | 1 (3) | 2 (1) |
| Use atypical antipsychotic | 1 (2) | 2 (2) | 1 (4) | 2 (3) | 2 (5) | Not applicable |
Data are represented as number (%) of cases.
The number of all nondiagnoses (n = 188) represents the number of patients that were diagnosed with 1 or more disorders on the MINI. In contrast, the number associated with each specific condition represents the number of cases. Because some patients were diagnosed with > 1 disorder, the sum of the cases for each condition does not add up to the number of nondiagnoses.
Abbreviation: MINI = Mini International Neuropsychiatric Interview.
Among all chart reviews of patients with a MINI diagnosis (n = 435), correlations were found between social phobia diagnosis on the MINI and the mention of lost job/inability to find job in the patient's chart (P < .05). Similarly, generalized anxiety disorder was correlated with mention of worry, stress, alcohol abuse/addiction, and lost job/inability to find job (P < .05). A diagnosis of panic disorder was linked with mentions of worry, stress, insomnia, chronic pain, diarrhea/constipation, and drug abuse/addiction (P < .05). Finally, insomnia (major depressive disorder only), drug abuse/addiction, and lost job/inability to find job were significantly associated with both major depressive disorder and bipolar disorder (P < .05).
DISCUSSION
The purpose of this investigation was to determine the rate of detection of several mood and anxiety disorders in a sample of patients visiting their primary care physician. First, according to results on the MINI, high percentages of patients (n = 435, 51.7%) were found to meet criteria for major depressive disorder, bipolar disorder, panic disorder, social anxiety disorder, or generalized anxiety disorder. Significant differences were noted in terms of education, marital status, and annual income between those who met the criteria for 1 of the assessed diagnoses and those who did not.
More importantly, the percentage of people in physicians' medical clinics who were found to meet criteria on the MINI for major depressive disorder, bipolar disorder, panic disorder, social anxiety disorder, or generalized anxiety disorder and who were not detected by physicians by virtue of the chart review process was also high and therefore worrisome. Nondetection rates by primary care physicians (as measured by the chart review) were as follows: 65.9% of patients with major depressive disorder, 92.7% of patients with bipolar disorder, 85.8% of patients with panic disorder, 71.0% of patients with generalized anxiety disorder, and an outstanding 97.8% of individuals with social anxiety disorder. Even when taking into account cases for which chart review revealed a mood and anxiety diagnosis that was different than the MINI diagnosis, the rates of detection remained low, ranging from 41.5% for panic disorder to 81.3% for social anxiety disorder. These results are comparable to findings in the National Comorbidity Survey and in other smaller studies in primary care, which reported that general practitioners fail to diagnose up to half of cases of depression or anxiety.12,13,54–56
Finally, in a number of cases that were not fully diagnosed, primary care physicians had recorded symptoms associated with the disorder, most often headache/backache (21.8%), diarrhea/constipation (15.4%), and insomnia (12.8%). This is consistent with literature reporting that patients with mental health disorders often visit medical clinics for physical symptoms.48 Overall, the present study noted that the detection by primary care physicians was poor, and there were high incidences of misdiagnosis/underdiagnosis of mood and anxiety disorders in primary care clinics.
The low detection rates of mood and anxiety disorders highlight the difficulties that exist in primary care. Problems in detection and diagnosis by primary care physicians must be addressed to ensure that patients are appropriately treated and impairment to their quality of life is minimized. In primary care settings, not only diagnosis, but also treatment of mood and anxiety disorders, has been reported to be inadequate.50 In addition, the prognosis for individuals with undetected major depressive disorder is considerably worse than their counterparts who have been accurately diagnosed.57 With detection and treatment being so closely linked, the authors believe that improving the quality of detection by primary care physicians is the first necessary step toward an improved quality of care for these patients.
There were limitations to this research study. For instance, there is no record of the number of refusals to participate in the study. Consequently, there may be some differences between the persons willing to participate in this research study versus those who declined. It is possible that people more inclined were those who assumed they were suffering from a mood or anxiety disorder. Also, recruiting in medical waiting rooms may have biased the sample toward patients with more severe illnesses or symptoms. Patients visiting their primary care physician, and those who attended the clinic frequently, were more likely to be recruited into the study. However, this approach was deemed to be the most appropriate, due to time and money constraints, and has been used in similar investigations.58,59
In addition, and perhaps more importantly, the prevalence of mood and anxiety disorders58–60 and the rate of detection/treatment by primary care physicians54–56,61 were similar to previous reports. Therefore, we are confident that the nature of the present sample did not lead to underestimation or overestimation of the misdiagnosis rate. The present study did not collect information on whether or not subjects had received psychiatric or psychological care, nor if they had been previously diagnosed with a psychiatric condition. A further study limitation is that interrater reliability was not assessed in this study.
Inaccurate rating or diagnosis based on chart review could have influenced our findings. However, the specificity of assessment (ie, the list of terms as indicators) provided clear and standardized guidelines for clinical assessors. Furthermore, all clinical raters were extensively trained and supervised to ensure the quality and uniformity of diagnosis across the different clinics. Finally, an expert reviewer randomly assessed several cases to maintain accurate diagnosis.
It is important to note that while this study was sponsored by a drug company, and, as such, there is a risk for potential bias toward overdiagnosis, our results are in keeping with the findings of several other studies,12,13,16,54–56,61 suggesting that a major funding-induced bias was unlikely.
The large sample size of the present study and the use of the MINI as an objective and well-validated scale provided a unique Canadian perspective of assessment of primary care patients from a variety of sites across the country. The study provides demographic information on common psychiatric diagnoses within the primary care population. It highlights the importance of primary care physicians as first-line agents in the recognition of mood and anxiety disorders. Further to this point, we believe that this information will facilitate communication between the primary care referral source and the psychiatrist to allow for a better understanding and follow-up of patients from the primary care referral site.
CONCLUSION
The present study documents that a substantially high percentage of patients with mood and anxiety disorders is not being detected or diagnosed in primary care practices across Canada despite the recognition and documentation of several symptoms characteristic of the disorder in individual patient charts. These findings support other studies suggesting that underdiagnosis and misdiagnosis of common psychiatric conditions are prevalent in the primary care setting.54–56,61 This situation results in fewer people being treated appropriately, exacerbating the burden of these conditions.
Given that the majority of the population with mental health disorders is likely to visit their primary care physician62 and that there are various factors deterring primary care physicians from using diagnostic scales,9,14,61 the need for a short, simple, self-administered diagnostic instrument is evident.59 Furthermore, understanding the psychology associated with the process of disclosure and detection will no doubt play an important role in increasing the rates of detection and disclosure of psychological problems within the primary care setting. Future research in this area is warranted to facilitate access to treatment for patients presenting with mental health problems to primary care physicians. On the basis of the present data, improvement in diagnosis rates could reduce suffering in the population whose mood and anxiety disorders remain undetected and prevent the resulting economic loss.
Potential conflicts of interest: None reported.
Funding/support: Research was funded by Wyeth Pharmaceuticals, Markham, Ontario, Canada (grant no. 101977).
Acknowledgments
The authors would like to thank Christina Iorio, MA, Department of Psychology, Lakehead University, Thunder Bay, and START Clinic for Mood and Anxiety Disorders, Toronto, Ontario, Canada, and Dina Tsirgielis, BSc, START Clinic for Mood and Anxiety Disorders, Toronto, Ontario, Canada, for their diligent work in the preparation of this article for submission. The authors would like to thank Christina Clark, MSc, for her editorial support. All editorial support was funded by the START Clinic directly. None of the acknowledged individuals have any financial or other affiliations related to the subject of this article.
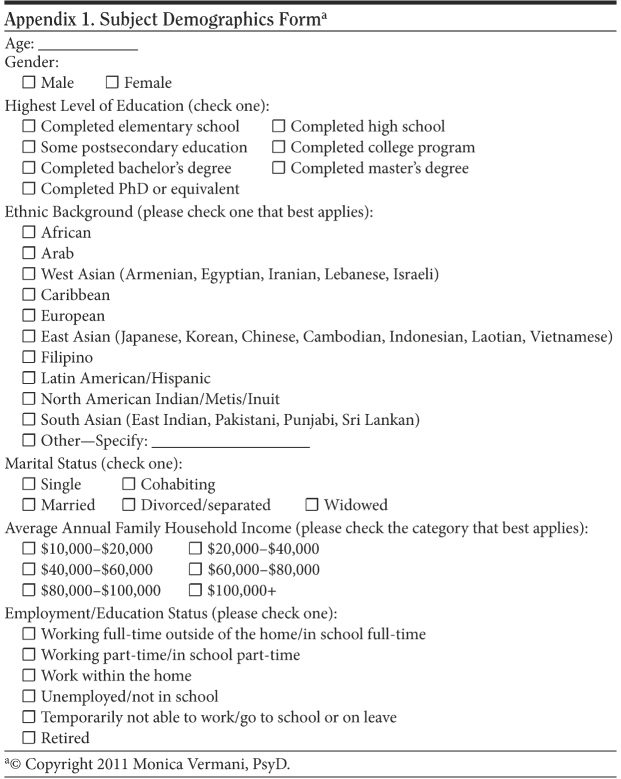
Appendix 1.
Subject Demographics Forma
Appendix 2.
Chart Reviewa
REFERENCES
- 1.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stephens T, Joubert N. The economic burden of mental health problems in Canada. Chronic Dis Can. 2001;22(1):18–23. [PubMed] [Google Scholar]
- 3.Statistics Canada. The daily Canadian community health survey: mental health and well-being (Canada Catalogue no. 11-001-XIE) http://www.statcan.ca/Daily/English/030903/d030903.pdf. Accessed October 19, 2006.
- 4.Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry. 1999;60(7):427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- 5.Weiller E, Bisserbe JC, Boyer P, et al. Social phobia in general health care: an unrecognised undertreated disabling disorder. Br J Psychiatry. 1996;168(2):169–174. doi: 10.1192/bjp.168.2.169. [DOI] [PubMed] [Google Scholar]
- 6.DuPont RL, DuPont CM, Rice DP. Economic costs of anxiety disorders. In: Stein DJ, Hollander E, editors. Textbook of Anxiety Disorders. Washington, DC: American Psychiatric Publishing; 2002. pp. 475–483. [Google Scholar]
- 7.Lecrubier Y. Comorbidity in social anxiety disorder: impact on disease burden and management. J Clin Psychiatry. 1998;59(suppl 17):33–38. [PubMed] [Google Scholar]
- 8.Van Os TW.D.P, Van den Brink RHS, Van der Meer K, et al. The care provided by general practitioners for persistent depression. Eur Psychiatry. 2006;21(2):87–92. doi: 10.1016/j.eurpsy.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Leon AC, Olfson M, Broadhead WE, et al. Prevalence of mental disorders in primary care: implications for screening. Arch Fam Med. 1995;4(10):857–861. doi: 10.1001/archfami.4.10.857. [DOI] [PubMed] [Google Scholar]
- 10.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg D, Huxley P. Common Mental Disorders: A Bio-Social Model. New York, NY: Travistock/Routledge; 1992. [Google Scholar]
- 13.Katon W, von Korff M, Lin E, et al. Adequacy and duration of antidepressant treatment in primary care. Med Care. 1992;30(1):67–76. doi: 10.1097/00005650-199201000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33(2):80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 15.Lecrubier Y, Sheehan D, Weiller E, et al. The Mini International Neuropsychiatric Interview (MINI): a short diagnostic structured interview: reliability and validity according to the CIDI. Eur Psychiatry. 1997;12(5):224–231. [Google Scholar]
- 16.Lecrubier Y. Improved ability to identify symptoms of major depressive disorder (MDD) in general practice. Int J Psychiatry Clin Pract. 2001;5(suppl):3–10. doi: 10.1080/13651500152048397. [DOI] [PubMed] [Google Scholar]
- 17.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 18.Zung WW. The role of rating scales in the identification and management of the depressed patient in the primary care setting. J Clin Psychiatry. 1990;51(suppl):72–76. [PubMed] [Google Scholar]
- 19.Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 20.Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16(4):267–276. doi: 10.1016/0163-8343(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 21.Arnau RC, Meagher MW, Norris MP, et al. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20(2):112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 22.Statistics Canada. Canadian community health survey: mental health and well-being (Canada Catalogue no. 82-617-XIE) http://www.statcan.gc.ca/pub/82-617-x/index-eng.htm. Accessed November 1, 2006.
- 23.Bauer M, Pfennig A. Epidemiology of bipolar disorders. Epilepsia. 2005;46(suppl 4):8–13. doi: 10.1111/j.1528-1167.2005.463003.x. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Chiu WT, Jin R, et al. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63(4):415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barsky AJ, Delamater BA, Orav JE. Panic disorder patients and their medical care. Psychosomatics. 1999;40(1):50–56. doi: 10.1016/S0033-3182(99)71271-5. [DOI] [PubMed] [Google Scholar]
- 26.Fifer SK, Mathias SD, Patrick DL, et al. Untreated anxiety among adult primary care patients in a Health Maintenance Organization. Arch Gen Psychiatry. 1994;51(9):740–750. doi: 10.1001/archpsyc.1994.03950090072010. [DOI] [PubMed] [Google Scholar]
- 27.Roy-Byrne PP, Katon W, Broadhead WE, et al. Subsyndromal ("mixed") anxiety–depression in primary care. J Gen Intern Med. 1994;9(9):507–512. doi: 10.1007/BF02599221. [DOI] [PubMed] [Google Scholar]
- 28.Stein MB, Kirk P, Prabhu V, et al. Mixed anxiety-depression in a primary-care clinic. J Affect Disord. 1995;34(2):79–84. doi: 10.1016/0165-0327(95)00002-5. [DOI] [PubMed] [Google Scholar]
- 29.Sherbourne CD, Jackson CA, Meredith LS, et al. Prevalence of comorbid anxiety disorders in primary care outpatients. Arch Fam Med. 1996;5(1):27–34. doi: 10.1001/archfami.5.1.27. discussion 35. [DOI] [PubMed] [Google Scholar]
- 30.Lépine JP. The epidemiology of anxiety disorders: prevalence and societal costs. J Clin Psychiatry. 2002;63(suppl 14):4–8. [PubMed] [Google Scholar]
- 31.Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. 2002;16(4):162–171. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- 32.Roy-Byrne PP, Wagner A. Primary care perspectives on generalized anxiety disorder. J Clin Psychiatry. 2004;65(suppl 13):20–26. [PubMed] [Google Scholar]
- 33.Shear K, Belnap BH, Mazumdar S, et al. Generalized Anxiety Disorder Severity Scale (GADSS): a preliminary validation study. Depress Anxiety. 2006;23(2):77–82. doi: 10.1002/da.20149. [DOI] [PubMed] [Google Scholar]
- 34.Olfson M, Fireman B, Weissman MM, et al. Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry. 1997;154(12):1734–1740. doi: 10.1176/ajp.154.12.1734. [DOI] [PubMed] [Google Scholar]
- 35.Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 36.Wittchen HU, Zhao S, Kessler RC, et al. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(5):355–364. doi: 10.1001/archpsyc.1994.03950050015002. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Brandenburg N, Lane M, et al. Rethinking the duration requirement for generalized anxiety disorder: evidence from the National Comorbidity Survey Replication. Psychol Med. 2005;35(7):1073–1082. doi: 10.1017/s0033291705004538. [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 39.Connor KM, Kobak KA, Churchill LE, et al. Mini-SPIN: a brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14(2):137–140. doi: 10.1002/da.1055. [DOI] [PubMed] [Google Scholar]
- 40.Davidson JRT, Hughes DL, George LK, et al. The epidemiology of social phobia: findings from the Duke Epidemiological Catchment Area Study. Psychol Med. 1993;23(3):709–718. doi: 10.1017/s0033291700025484. [DOI] [PubMed] [Google Scholar]
- 41.Katzelnick DJ, Kobak KA, DeLeire T, et al. Impact of generalized social anxiety disorder in managed care. Am J Psychiatry. 2001;158(12):1999–2007. doi: 10.1176/appi.ajp.158.12.1999. [DOI] [PubMed] [Google Scholar]
- 42.Zimmerman M, Galione J. Psychiatrists' and nonpsychiatrist physicians' reported use of the DSM-IV criteria for major depressive disorder. J Clin Psychiatry. 2010;71(3):235–238. doi: 10.4088/JCP.08m04940blu. [DOI] [PubMed] [Google Scholar]
- 43.Zimmerman M, McGlinchey JB. Why don't psychiatrists use scales to measure outcome when treating depressed patients? J Clin Psychiatry. 2008;69(12):1916–1919. doi: 10.4088/jcp.v69n1209. [DOI] [PubMed] [Google Scholar]
- 44.Patten SB, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. I: classification, burden and principles of management. J Affect Disord. 2009;117(suppl 1):S5–S14. doi: 10.1016/j.jad.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 45.Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III: pharmacotherapy. J Affect Disord. 2009;117(suppl 1):S26–S43. doi: 10.1016/j.jad.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 46.McQuaid JR, Stein MB, McCahill M, et al. Use of brief psychiatric screening measures in a primary care sample. Depress Anxiety. 2000;12(1):21–29. doi: 10.1002/1520-6394(2000)12:1<21::AID-DA3>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 47.Craske MG, Edlund MJ, Sullivan G, et al. Perceived unmet need for mental health treatment and barriers to care among patients with panic disorder. Psychiatr Serv. 2005;56(8):988–994. doi: 10.1176/appi.ps.56.8.988. [DOI] [PubMed] [Google Scholar]
- 48.Allgulander C. Generalized anxiety disorder: what are we missing? Eur Neuropsychopharmacol. 2006;16(suppl 2):S101–S108. doi: 10.1016/j.euroneuro.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Stein MB, Sherbourne CD, Craske MG, et al. Quality of care for primary care patients with anxiety disorders. Am J Psychiatry. 2004;161(12):2230–2237. doi: 10.1176/appi.ajp.161.12.2230. [DOI] [PubMed] [Google Scholar]
- 50.Weisberg RB, Dyck I, Culpepper L, et al. Psychiatric treatment in primary care patients with anxiety disorders: a comparison of care received from primary care providers and psychiatrists. Am J Psychiatry. 2007;164(2):276–282. doi: 10.1176/appi.ajp.164.2.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sheehan DA, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- 52.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 53.Chouinard G. The search for new off-label indications for antidepressant, antianxiety, antipsychotic and anticonvulsant drugs. J Psychiatry Neurosci. 2006;31(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 54.Coyne JC, Schwenk TL, Fechner-Bates S. Nondetection of depression by primary care physicians reconsidered. Gen Hosp Psychiatry. 1995;17(1):3–12. doi: 10.1016/0163-8343(94)00056-j. [DOI] [PubMed] [Google Scholar]
- 55.Rost K, Zhang M, Fortney J, et al. Persistently poor outcomes of undetected major depression in primary care. Gen Hosp Psychiatry. 1998;20(1):12–20. doi: 10.1016/s0163-8343(97)00095-9. [DOI] [PubMed] [Google Scholar]
- 56.Young AS, Klap R, Sherbourne CD, et al. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 57.Coyne JC, Klinkman MS, Gallo SM, et al. Short-term outcomes of detected and undetected depressed primary care patients and depressed psychiatric patients. Gen Hosp Psychiatry. 1997;19(5):333–343. doi: 10.1016/s0163-8343(97)00055-8. [DOI] [PubMed] [Google Scholar]
- 58.Linzer M, Spitzer R, Kroenke K, et al. Gender, quality of life, and mental disorders in primary care: results from the PRIME-MD 1000 study. Am J Med. 1996;101(5):526–533. doi: 10.1016/s0002-9343(96)00275-6. [DOI] [PubMed] [Google Scholar]
- 59.Ansseau M, Dierick M, Buntinkx F, et al. High prevalence of mental disorders in primary care. J Affect Disord. 2004;78(1):49–55. doi: 10.1016/s0165-0327(02)00219-7. [DOI] [PubMed] [Google Scholar]
- 60.Roca M, Gili M, Garcia-Garcia M, et al. Prevalence and comorbidity of common mental disorders in primary care. J Affect Disord. 2009;119(1-3):52–58. doi: 10.1016/j.jad.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 61.Verhaak PF, Schellevis FG, Nuijen J, et al. Patients with a psychiatric disorder in general practice: determinants of general practitioners' psychological diagnosis. Gen Hosp Psychiatry. 2006;28(2):125–132. doi: 10.1016/j.genhosppsych.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 62.Price D, Beck A, Nimmer C, et al. The treatment of anxiety disorders in a primary care HMO setting. Psychiatr Q. 2000;71(1):31–45. doi: 10.1023/a:1004662600803. [DOI] [PubMed] [Google Scholar]