Abstract
Acute myocardial infarction (AMI) is caused by thrombus formation over a disrupted plaque occluding an epicardial coronary artery. Mechanical thrombectomy is effective in removing thrombus burden from native vessels and saphenous vein grafts. Here we report a case of an aneurysmatic dilatation of an infarct-related artery (IRA) referred to our Institute for rescue PCI, after failed fibrinolysis, successfully treated with only rheolytic thrombectomy (AngioJet, Possis Medical, Minneapolis, Minnesota, USA) without the need for adjunctive balloon or stent implantation.
KEY WORDS: Thrombectomy, Coronary aneurysm, Acute myocardial infarction, PCI rescue
INTRODUCTION
Acute myocardial infarction (AMI) is caused by thrombus formation over a disrupted plaque occluding an epicardial coronary artery. The strategies to reperfuse an occluded coronary artery in the setting of AMI are either pharmacological (eg, fibrinolysis) or mechanical such as primary percutaneous coronary intervention (PCI). A great deal of evidence indicates that expeditious restoration of flow in the obstructed infarct artery after the onset of symptoms in ST Elevation Myocardial Infarction (STEMI) patients is a key determinant of short- and long-term outcomes, regardless of whether reperfusion is accomplished by fibrinolysis or PCI (1–3). However, even after successful recanalization of the occluded artery, with consequent restoration of epicardial flow, distal perfusion at the tissue level may become impaired (i.e., “no-reflow”), secondary to impairment of microcirculation (4). This phenomenon is particularly relevant when a heavy thrombus burden is present in the artery lumen, as may happen in particular circumstances like mechanical recanalization of saphenous vein grafts or coronary artery aneurysm due to the possibility of distal embolization of thrombus material (5). So the rationale for mechanical thrombectomy in removing thrombus burden from IRA is to minimize embolization.
Here we report a case of an aneurysmatic dilatation of an infarct-related artery (IRA) referred to our Institute for rescue PCI after failed fibrinolysis, successfully treated with only rheolytic thrombectomy (AngioJet, Possis Medical, Minneapolis, Minnesota, USA), without the need for adjunctive balloon or stent implantation.
CASE REPORT
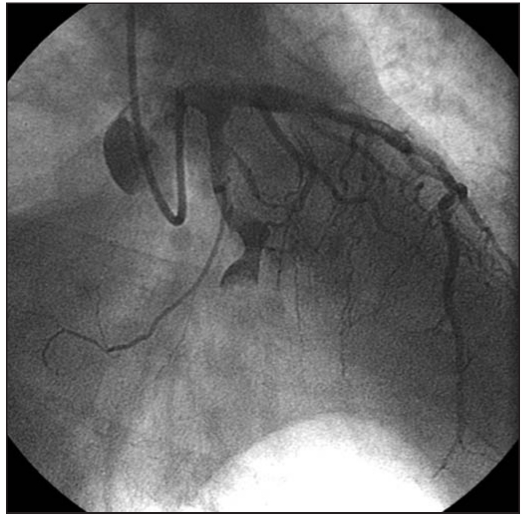
A 68-year-old man was admitted to our coronary care unit (CCU) for acute myocardial infarction. ECG revealed ST-segment elevation in leads II, III, aVF. Intravenous fibrinolysis with TNK-tPA and adjunctive antithrombotic and antiplatelet therapy with heparin and aspirin respectively, was initiated as soon as he arrived in CCU. Time from onset symptoms to lysis therapy was one hour and 20 minutes. Because of the persistence of ST-segment elevation and chest pain 90 minutes after thrombolytic therapy, he underwent coronary angiography by transradial approaches that revealed acute thrombotic occlusion of the left circumflex coronary (LCx) artery at the proximal tract (TIMI 0) with aneurysmal dilatation, fusiform type, (Fig. 1) and 80% stenosis of the mid segment of the left anterior descending (LAD) coronary artery; no significant stenosis were seen in the right coronary artery. Activated clotting time (ACT) was out of range, so no adjunctive unfractioned heparin or glycoprotein IIb/IIIa inhibitors could be administered. The left coronary artery was then selectively engaged with a 6Fr guiding catheter (Amplatz 1, Cordis, Johnson & Johnson, Miami, FL, USA) by transradial approaches too. A guidewire (ACS HI-Torque Intermediate 0.014”, Guidant, Indianapolis, IN, USA) was crossed through the occlusion; the angiogram showed a TIMI 0 flow. Because of the image of heavy thrombus contained in the coronary aneurysm we decided to remove it by the rheolytic thrombectomy system 4Fr monorail catheter (AngioJet, Possis Medical, Minneapolis, Minnesota, USA).
Fig. 1.
- LCx before primary PCI. The arrow indicates the coronary aneurysm and the presence of thrombus.
The rheolytic thrombectomy system AngioJet removes thrombi via rheolytic fragmentation and simultaneous active removal through hydrostatic suction. The catheter is attached to a drive unit with a piston pump that generates a high-pressure pulsed flow rate of 10,000 psi at 60cc/min through a hypotube. The hypotube ejects saline at a loop in the catheter tip. The jets of high-velocity saline are directed back into an exhaust lumen. This creates a vortex (Venturi effect) that fragments and aspirates thrombus and loose debris. The vortex is centered at side holes within the catheter to drive the aspiration of thrombus. Rheolytic thrombectomy was successful, with a final TIMI grade 3 flow and ST-segment resolution without the need for balloon or stent (Fig. 2). No temporary pacemaker is needed during rheolytic thrombectomy with AngioJet. The patient returned to the CCU in stable condition asymptomatic. Peak concentration of CK, MB fraction and Troponin I reached 4418 UI/L, 242.8 ng/mL and 177 ng/mL respectively. Blood chemistry was otherwise normal. The patient was discharged in good condition after five days, with oral anticoagulation therapy, and remains free of major adverse cardiac events at 30 days.
Fig. 2.
- LCx after rheolytic thrombectomy with AngioJet; note the complete absence of image suggesting the presence of a thrombus in the coronary aneurysm.
DISCUSSION
Coronary artery aneurysms are classified as either saccular or fusiform type. Coronary aneurysm can cause angina pectoris or AMI. In one study, 2.6% of patients undergoing primary PCI was found to have a coronary aneurysm in the IRA (6). Aneurysmal dilatation of an IRA is associated with high-burden thrombus formation and a lower incidence of successful pharmacological or mechanical reperfusion (7, 8). PCI-treated patients experience lower short-term mortality rates, less nonfatal reinfarction, and less hemorrhagic stroke than those treated by fibrinolysis (9). However, PCI and stenting carry the risk of mobilizing thrombotic and thrombogenic material, causing distal embolization and microcirculatory impairment, which may limit myocardial salvage achieved by these techniques. In the setting of AMI the presence of coronary aneurysm of the IRA filled with heavy thrombus represent a challenge case for the interventional cardiologist. In fact the presence of thrombus predispose PCI to a high rate of thrombus embolization and no-reflow phenomenon. Also a pharmacological approach such as glycoprotein IIb/IIIa inhibitors could be dangerous after lysis and when a high degree of ACT is present. Direct stenting without predilation may decrease embolization and the incidence of the no-reflow phenomenon (10). More specific approaches to the problem of microvessel embolization during PCI include thrombectomy by different techniques and the use of anti-embolic protection devices. However distal embolization filter are not suitable for all coronary artery anatomy. Two randomized trials have reported rheolytic thrombectomy with AngioJet to be effective in decreasing embolization in patients who underwent PCI on venous grafts or native coronary vessel with massive thrombosis (11, 12). Only one case report described the use of the AngioJet rheolytic thrombectomy device in a coronary aneurysm, but with the subsequent implantation of a JoStent coronary artery graft (13). Fibrinolysis or primary PCI have a high degree of failure in the treatment of coronary aneurysm in AMI (7,8). So the rheolytic thrombectomy system AngioJet represents a novel, extraordinary and useful tool also to treat this complicated and rare case in which there is a high degree of thrombus burden. AngioJet had an excellent pushability and trackability also in torturous coronary artery and in the mid and distal tract of the LCx: this device may allow removal of soft material immediately before PCI or stenting to avoid or minimize distal embolization. Initial thrombus removal also permits early identification of lesion characteristics and more site-specific treatment of the underlying culprit lesion, particularly in patients with total occlusion. To our knowledge, this is the first report of the use of the AngioJet rheolytic trombectomy in a coronary aneurysm, as the culprit lesion in the setting of AMI, without the need for subsequent use of balloon or stent implantation.
CONCLUSION
The presence of coronary aneurysm of the IRA is a quite rare situation. The presence of a high grade of thrombus in the coronary aneurysm during AMI, predispose PCI to a high rate of thrombus embolization, no-reflow phenomenon and failure. The rheolytic thrombectomy system AngioJet is a very useful tool and may be a novel approach to reperfuse coronary aneurysms during PCI also in these difficult and rare circumstances to warrant a high rate of complete reperfusion.
ACKNOWLEDGEMENTS
Appreciation is expressed to Mr Maurizio Proietti and Mr Paolo Tiradosso for nursing assistance.
REFERENCES
- 1.De Luca G, Suryapranata H, Zijlstra F, van’t Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ, ZWOLLE Myocardial Infarction Study Group Symptomonset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991–7. doi: 10.1016/s0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- 2.Boersma E, Mercado N, Poldermans D, Gardien M, Vos J, Simoons ML. Acute myocardial infarction. Lancet. 2003;361:847–58. doi: 10.1016/S0140-6736(03)12712-2. [DOI] [PubMed] [Google Scholar]
- 3.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation. 2004;109:1223–5. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 4.Ambrosio G, Weisman HF, Mannisi JA, Becker LC. Progressive impairment of regional myocardial perfusion following initial restoration of post-ischemic blood flow. Circulation. 1989;80:1846–61. doi: 10.1161/01.cir.80.6.1846. [DOI] [PubMed] [Google Scholar]
- 5.Mathew V, Lennon RJ, Rihal CS, Bresnahan JF, Holmes DR., Jr Applicability of distal protection for aortocoronary vein graft interventions in clinical practice. Catheter Cardiovasc Interv. 2004;63:148–51. doi: 10.1002/ccd.20102. [DOI] [PubMed] [Google Scholar]
- 6.Yip HK, Chen MC, Wu CJ, Hang CL, et al. Clinical features and outcome of coronary artery aneurysm in patients with acute myocardial infarction undergoing a primary percutaneous coronary intervention. Cardiology. 2002;98:132–40. doi: 10.1159/000066322. [DOI] [PubMed] [Google Scholar]
- 7.Otsuka M, Minami S, Hato K, et al. Acute myocardial infarction caused by thrombotic occlusion of a coronary aneurysm. Cathet Cardiovasc Diagn. 1997;41:423–5. doi: 10.1002/(sici)1097-0304(199708)41:4<423::aid-ccd19>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 8.Erdol C, Celik S, Baykan M, Gokce M, Karahan B, Bayram A. A coronary aneurysm complicated by acute myocardial infarction. A case report. J Cardiovasc Surg. 2001;42:65–7. [PubMed] [Google Scholar]
- 9.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 10.Loubeyre C, Morice MC, Lefevre T, Pichaud J-F, Louvard Y, Dumas P. A randomized comparison of direct stenting with conventional stent implantation in selected patients with acute myocardial infarction. J Am Coll Cardiol. 2002;39:15–21. doi: 10.1016/s0735-1097(01)01701-6. [DOI] [PubMed] [Google Scholar]
- 11.Kuntz RE, Baim DS, Cohen DJ, et al. A trial comparing rheolytic thrombectomy with intracoronary urokinase for coronary and vein grafts thrombus (the Vein Graft Angio-Jet Study) Am J Cardiol. 2002;89:326–30. doi: 10.1016/s0002-9149(01)02235-4. [DOI] [PubMed] [Google Scholar]
- 12.Antoniucci D, Valenti R, Migliorini A, et al. Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2004;93:1033–5. doi: 10.1016/j.amjcard.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Lee MS, Nero T, Makkar RR, Wilentz JR. Treatment of coronary aneurysm in acute myocardial infarction with Angio-Jet thrombectomy and JoStent coronary stent graft. J Invasive Cardiol. 2004;16:294–6. [PubMed] [Google Scholar]