Abstract
Background
Extramammary Paget's disease is a cutaneous neoplasm that presents as erythematous crusted patches and plaques reminiscent of contact dermatitis or inverse psoriasis that can be a challenge to treat in a tissue-sparing manner. The most commonly involved site for this rare disorder is the anogenital region. Surgery is considered as the gold standard therapy. In the last years, the topical use of imiquimod cream in the treatment of this condition has been reported.
Main observations
We present a case of a 59-year-old woman with primary extramammary Paget's disease of the vulva, in which a conservative approach to therapy was desired, and who underwent complete and stable remission with imiquimod cream. We also review the previous reports of patients with extramammary Paget's disease treated with imiquimod cream.
Conclusions
Imiquimod therapy may be an alternative for primary as well as recurring extramammary Paget's disease. Treatment-associated morbidity is minimal compared with other therapies, such as surgery which may be debilitating.
Keywords: imiquimod, intraepithelial adenocarcinoma, Paget's disease, therapy, topical, vulva
Introduction
Extramammary Paget's disease (EMPD) is an uncommon intraepithelial adenocarcinoma, which occurs most commonly in the anogenital region, but can also arise in any area of skin or mucosa.[1] It is thought to originate from intraepidermal apocrine glands or from pluripotent keratinocyte stem cells. This disease occurs most frequently in postmenopausal women and on the vulva. Because of its multifocal nature with indistinct demarcation and the resulting high recurrence rate, EMPD is difficult to treat, and radical surgery with large margins is often considered. The well-known association of EMPD with underlying malignancy contributes also to the therapeutic challenge.[2]
Current recommended treatments for EMPD are surgical excision, preferably Mohs' micrographic surgery, laser ablation, electrodessication and curettage, photodynamic therapy, radiotherapy as well as topical use of 5-fluorouracil.[3] Topical application of imiquimod 5% cream has been reported in the last years with successful results.[3–14] We report the case of a woman with primary vulvar Paget's disease, who underwent successful treatment with imiquimod cream, and review the published cases with EMPD treated to date with this therapy.
Case Report
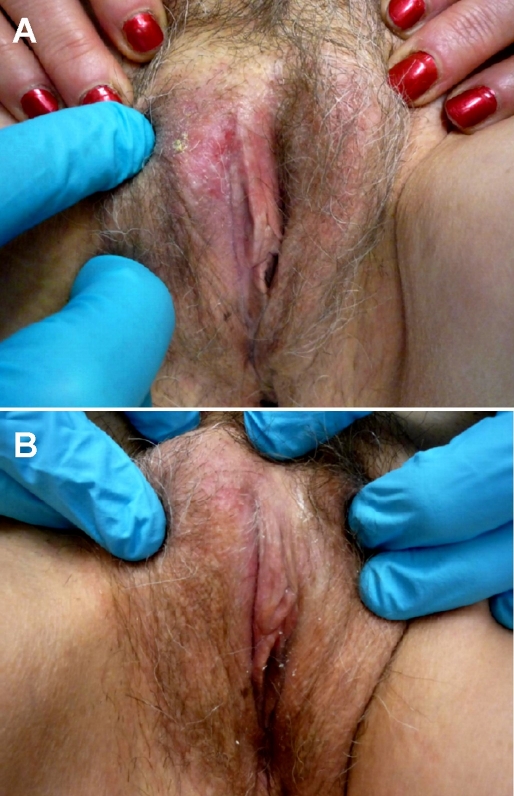
A 59-year-old female patient consulted for a fluctuating sore and itchy zone in her vulva, present since several months. Physical examination revealed a poorly delimited erythemato-squamous patch on the right labia major, with a diameter of 1-2 cm [Fig. 1A]. The lesion was preliminary diagnosed as genital seborrhoic dermatitis and probatorily treated with a cream containing lithium succinate and zinc sulfate. As the lesion didn't improve, and aeras of superficial maceration and erosion developed a larger differential diagnosis was considered, including contact dermatitis, psoriasis inversa, Bowen's disease and EMPD.
Figure 1.
1A. Lesion at diagnosis, before Imiquimod therapy. 1B. Lesion 3 months after the end of Imiquimod therapy.
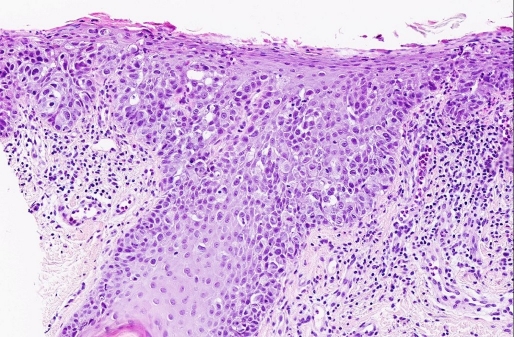
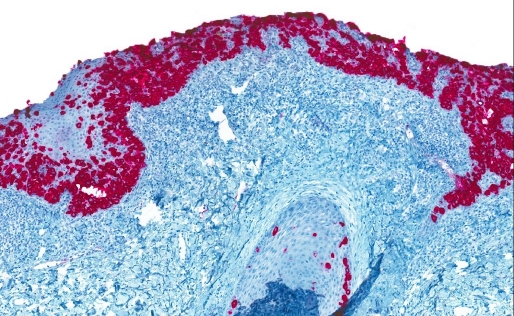
A skin biopsy revealed the presence of large cells with abundant pale cytoplasm and pleomorphic nuclei in all layers of the epidermis [Fig. 2], spreading in the epithelium of the follicular structures, without invasion of the dermis. Immunohistochemical staining was positive for total keratins and cytokeratin 7 [Fig. 3], while staining for S100 was negative. A diagnosis of vulvar Paget's disease was made. The patient was addressed to our clinic for management and therapy.
Figure 2.
HE staining: large atypical cells with abundant cytoplasm in the epidermis.
Figure 3.
Immunohistochemical staining with cytokeratin 7.
Upon further examination, total body skin and lymph nodes palpation examination was normal. A tumour screening including a computer tomography of the thorax and abdomen, blood inflammatory parameters, the tumour marker CA-125, as well as an ileocoloscopy, a gynaecological and a urological examination with urine cytology revealed no pathology.
Because of the good prognosis of EMPD at this location in the absence of underlying or associated disease in a relatively young patient, we were reluctant to choose a surgical therapy in first intention. Given the age of the patient, radiotherapy, associated to possible late side effects, was also considered as second- or third-line. Furthermore, the lesion was deep as assessed by histology for an approach with photodynamic therapy.
As the patient also privileged a non-invasive therapy if possible, a treatment with imiquimod 5% cream in first intention was initiated. Imiquimod 5% cream was applied to the vulvar lesion, including a 1-2 cm circumferential margin of normal-appearing skin, before bedtime three times a week, for 18 weeks.
Under therapy the patient developed moderate to at moment intense inflammation of the site of imiquimod application, but without other side effects. Clinical controls at 1, 3, 6 months and one year after the end of therapy revealed complete healing and normal skin without clinical signs of recurrence of EMPD [Fig. 1B]. Blood parameters, gynaecological and urological examinations, thorax-radiography, ultrasonography of the abdomen, basin and lymph nodes were all normal at 1 year after therapy, confirming the complete remission. A follow-up screening with yearly gynaecological and urological examinations was recommended to the patient.
Discussion
Local surgical excision with a 1 cm margin of normal skin is the standard treatment option for EMPD.[2] Since recurrence rates between 16-50% are seen after regular surgery,[15] Mohs micrographic surgery has become the preferred treatment modality for EMPD.[16] Despite this, recurrences rates of 27% following Mohs surgery have been reported.[17] Other treatment options are laser ablation, electrodessication and curettage, photodynamic therapy, radiotherapy as well as topical use of bleomycine and 5-fluorouracil.3 Recently, immunotherapy with topical imiquimod 5% cream has been successfully used to treat isolated cases of EMPD. Table 1 summarizes the reported cases to date. According to published reports and our experience, use of imiquimod in the treatment of EMPD is safe and effective. Treatment of primary or recurrent EMPD with imiquimod has been reported in a total of 17 patients, with a complete response reported in 15. The total treatment duration varied from 6 to 24 weeks with a regimen usually starting as a daily application and then tapering of the treatment to one application every other day. The longest follow-up period reported in the literature is 26 months (1 case).
Table 1. Case reports/series of extramammary Paget disease treated by imiquimod.
| Author (year) | Nr of cases | Age | Disease | Dosage | Treatment duration (weeks) | Follow-up (months) | Outcome | Adverse events |
|---|---|---|---|---|---|---|---|---|
| Zampogna (2002)15 | 2 | 54 72 |
scrotum, recurrent perineal, primer | 1x/d: 6d, every other day: 15w; every other day: 7.5w |
16 7.5 |
12 4 |
CR CR |
flu-like symptoms; nausea, vomiting |
| Berman (2003)14 | 1 | 68 | scrotum, recurrent | 1x/d | 6 | 6 | CR, HR | local erythema |
| Qian (2003)12 | 1 | 73 | penile shaft | 3x/week | 6 | 14 | CR, HR | minimal |
| Wang (2003)11 | 1 | 75 | vulva, recurrent | 1x/d: 6d, 2x/week: 1w, 3x/week: 5w | 7 | 0.5 | CR, HR | local irritation |
| Cohen (2006)3 | 1 | 75 | suprapubic, primer | 3x/week | 16 | 9 | CR, HR | local erythema |
| Vereecken (2007)10 | 1 | 66 | perianal, recurrent | 1x/day | 12 | 12 | CR, HR | - |
| Geisler (2008)9 | 1 | 80 | vulva, reccurent | - | - | 12 | CR, HR | - |
| Hatch (2008)8 | 2 | 68 60 |
vulva, reccurent vulva, reccurent |
every other day, 1x/d: 4w; 2x/day: 2w, every day:5w |
24 20 |
4 7 |
CR, HR CR, HR |
pain, erosion; pain, ulceration |
| Challenor (2009)7 | 2 | 48 66 |
surgical not in toto surgical not in toto |
3x/week 3x/week |
12 12 |
4 3 |
follow-up follow-up |
- |
| Bertozzi (2009)6 | 1 | 71 | vulva, reccurent | - | 8 | - | CR | local itching |
| Sendagorta (2010)5 | 3 | 66 58 82 |
vulva, primer vulva, primer vulva, primer |
both: 1x/d: 3w, every other day: 3w | 6 6 6 |
26 22 20 |
CR, HR CR, HR CR, HR |
- local irritation - |
| Tonguc (2010)4 | 1 | 65 | vulva, reccurent | every day: 3w; 1w break; every other day: 14w | 18 | 24 | CR | erosion |
| Summary of reported cases | Total: 17 |
mean: 11.4 median: 10 range: 6-24 |
mean: 11.2 median: 10.5 range: 0.5-26 |
|||||
| CR: complete clinical remission; PR: partial clinical remission; HR: histological remission; d: day; w: week | ||||||||
Imiquimod is a topically applied imidazoquinoline immunomodulator that binds to the toll-like receptor 7 and locally induces the production of proinflammatory chemokines and cytokines. Its use has been approved in the treatment of human papilloma virus warts.
On average, 25% of cases of EMPD are associated with an underlying cutaneous adnexal adenocarcinoma and show a higher mortality rate (46%) than that of patients with EMPD without underlying cutaneous adnexal adenocarcinoma.[18] The location of the underlying internal malignancy is generally closely related to the location of the EMPD. A directed search for internal malignancy is therefore mandatory in patients who are diagnosed with EMPD[18] including a complete skin examination, palpation of lymph nodes, rectal examination, colonoscopy, and cystoscopy, in addition a gynaecological examination including pelvic and breast examination as well as colposcopy in women.[19] Pelvic and abdominal ultrasonography have been also recommended.[20]
Conclusion
The advantages of imiquimod therapy are the minimal morbidity associated with the treatment in comparison to the currently alternative therapies available, as well as the self-application by the patient. In our opininion, imiquimod should be used exclusively in cases of EMPD limited to the skin (primary cutaneous form). Our case and the review of other cases reported to date underline the potential of imiquimod as first-line treatment of primary cutaneous EMPD. Larger controlled trials are needed before this option can be accepted as a standard first-line therapy for primary cutaneous EMPD. Furthermore, the frequency of application and total duration of therapy should be harmonized and validated. Cohen et al. recommend topical therapy with imiquimod at least 3 times each week for a minimum of 8 weeks, and as long as 16 weeks[3], whereas Sendagorta et al. recommended daily application for 3 weeks, followed by an every other day application for another 3 weeks.[5] Long-term follow-up of these patients is mandatory.
References
- Bolognia J, Jorizzo J, Rapini R. Dermatology, Second edition edn., Vol. 1. Mosby Elsevier; 2008. [Google Scholar]
- Lloyd J, Flanagan AM. Mammary and extramammary Paget's disease. J Clin Pathol. 2000;53:742–749. doi: 10.1136/jcp.53.10.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen PR, Schulze KE, Tschen JA, Hetherington GW, Nelson BR. Treatment of extramammary Paget disease with topical imiquimod cream: case report and literature review. South Med J. 2006;99:396–402. doi: 10.1097/01.smj.0000209223.68763.b1. [DOI] [PubMed] [Google Scholar]
- Tonguc E, Güngor T, Var T, Ozat M, Sahin I, Sirvan L. Treatment of recurrent vulvar Paget disease with imiquimod cream: a case report and review of the literature. Arch Gynecol Obstet. 2011;283:97–101. doi: 10.1007/s00404-010-1653-4. [DOI] [PubMed] [Google Scholar]
- Sendagorta E, Herranz P, Feito M, Ramírez P, Floristán U, Feltes R, Benito DM, Casado M. Successful treatment of three cases of primary extramammary Paget's disease of the vulva with Imiquimod--proposal of a therapeutic schedule. J Eur Acad Dermatol Venereol. 2010;24:490–492. doi: 10.1111/j.1468-3083.2009.03451.x. [DOI] [PubMed] [Google Scholar]
- Bertozzi S, Londero AP, Fruscalzo A, Marchesoni D, Lellé RJ. Paget disease of the vulva: resolution after local treatment with imiquimod--report of a case and review of the literature. Gynakol Geburtshilfliche Rundsch. 2009;49:326–330. doi: 10.1159/000301110. [DOI] [PubMed] [Google Scholar]
- Challenor R, Hughes G, Fitton AR. Multidisciplinary treatment of vulval extramammary Paget's disease to maintain sexual function: an imiquimod success story. J Obstet Gynaecol. 2009;29:252–254. doi: 10.1080/01443610902745107. [DOI] [PubMed] [Google Scholar]
- Hatch KD, Davis JR. Complete resolution of Paget disease of the vulva with imiquimod cream. J Low Genit Tract Dis. 2008;12:90–94. doi: 10.1097/LGT.0b013e31815a58a5. [DOI] [PubMed] [Google Scholar]
- Geisler JP, Manahan KJ. Imiquimod in vulvar Paget's disease: a case report. J Reprod Med. 2008;53:811–812. [PubMed] [Google Scholar]
- Vereecken P, Awada A, Ghanem G, Marques da Costa C, Larsimont D, Simoens C, Mendes da Costa P, Hendlisz A. A therapeutic approach to perianal extramammary Paget's disease: topical imiquimod can be useful to prevent or defer surgery. Med Sci Monit. 2007;13:CS75–77. [PubMed] [Google Scholar]
- Wang LC, Blanchard A, Judge DE, Lorincz AA, Medenica MM, Busbey S. Successful treatment of recurrent extramammary Paget's disease of the vulva with topical imiquimod 5% cream. J Am Acad Dermatol. 2003;49:769–772. doi: 10.1067/s0190-9622(03)02107-8. [DOI] [PubMed] [Google Scholar]
- Qian Z, Zeitoun NC, Shieh S, Helm T, Oseroff AR. Successful treatment of extramammary Paget's disease with imiquimod. J Drugs Dermatol. 2003;2:73–76. [PubMed] [Google Scholar]
- Hiraldo-Gamero A, Gómez-Moyano E, Segura-Palacios JM, Sánchez-Fajardo F, Sanz-Trelles A. Extramammary Paget Disease Treated With 5% Imiquimod Cream. Actas Dermosifiliogr. 2011;102:554–556. doi: 10.1016/j.ad.2010.12.014. [DOI] [PubMed] [Google Scholar]
- Berman B, Spencer J, Villa A, Poochareon V, Elgart G. Successful treatment of extramammary Paget's disease of the scrotum with imiquimod 5% cream. Clin Exp Dermatol. 2003;28 Suppl 1:36–38. doi: 10.1046/j.1365-2230.28.s1.12.x. [DOI] [PubMed] [Google Scholar]
- Zampogna JC, Flowers FP, Roth WI, Hassenein AM. Treatment of primary limited cutaneous extramammary Paget's disease with topical imiquimod monotherapy: two case reports. J Am Acad Dermatol. 2002;47(4 Suppl):S229–235. doi: 10.1067/mjd.2002.126584. [DOI] [PubMed] [Google Scholar]
- Gunn RA, Gallager HS. Vulvar Paget's disease: a topographic study. Cancer. 1980;46:590–594. doi: 10.1002/1097-0142(19800801)46:3<590::aid-cncr2820460327>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Hendi A, Brodland DG, Zitelli JA. Extramammary Paget's disease: surgical treatment with Mohs micrographic surgery. J Am Acad Dermatol. 2004;51:767–773. doi: 10.1016/j.jaad.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Coldiron BM, Goldsmith BA, Robinson JK. Surgical treatment of extramammary Paget's disease. A report of six cases and a reexamination of Mohs micrographic surgery compared with conventional surgical excision. Cancer. 1991;67:933–938. doi: 10.1002/1097-0142(19910215)67:4<933::aid-cncr2820670413>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Chanda JJ. Extramammary Paget's disease: prognosis and relationship to internal malignancy. J Am Acad Dermatol. 1985;13:1009–1014. doi: 10.1016/s0190-9622(85)70254-x. [DOI] [PubMed] [Google Scholar]
- Heymann WR. Extramammary Paget's disease. Clin Dermatol. 1993;11:83–87. doi: 10.1016/0738-081x(93)90101-h. [DOI] [PubMed] [Google Scholar]