Abstract
Patients' ability to effectively communicate with their health care providers is an essential aspect of proper self-care, especially for those with chronic conditions. We wanted to develop and validate a brief reliable measure of patient communication self-efficacy within clinical encounters. Consecutively recruited patients (n = 330) with diagnosed hypertension from seven primary care clinics in Chicago, Illinois, Grand Rapids, Michigan, and Shreveport, Louisiana completed an in-person interview including chronic disease self-efficacy, hypertension knowledge, health literacy assessments, and items modified from the Communication and Attitudinal Self-Efficacy (CASE) – Cancer scale. Six items from the CASE were candidates for a new scale due to their focus on the patient-provider relationship. Using principal components analysis with varimax rotation, four items strongly loaded onto one factor (Eigenvalue = 2.33; proportion of variance explained = 58%) with a Cronbach's α coefficient of 0.75. The measure, referred to as the Ask, Understand, Remember Assesment, (AURA) was moderately correlated with the total score from an existing chronic disease management self-efficacy scale (r = 0.31) and disease knowledge (beta coefficient = 0.2, 95% Confidence Interval 0.04 – 0.3, p = .03). Patients with low health literacy had lower scores on the AURA than those with marginal or adequate health literacy (p <.05). The AURA demonstrated high internal consistency and was correlated with both hypertension knowledge and a chronic disease self-efficacy scale. The AURA is brief, valid, has low reading demands, and is an appropriate tool for use among patients with chronic illness. It may also be useful in identifying and assisting patients who are at risk for errors or non-adherence with self-care behaviors.
Patient participation in the medical encounter is widely thought to have both inherent ethical value, and measureable benefits to patients (Cegala, Street, & Clinch, 2007; Greenfield, Kaplan, & Ware, 1985; Greenfield, Kaplan, Ware, Yano, & Frank, 1988; Guadagnoli et al., 2000; Harrington, Noble, & Newman, 2004; Street, Gordon, Ward, Krupat, & Kravitz, 2005; Street, Makoul, Arora, & Epstein, 2009). While several studies have examined the association between physician behaviors and patient participation (Cegala, 1997; Cegala, et al., 2007; Roter, 1984; Street & Gordon, 2006; Street et al., 2005), or patients' preferences for involvement in care (Abraido-Lanza, Chao, & Gates, 2005; Bruera, Willey, Palmer, & Rosales, 2002; Cassileth, Zupkis, Sutton-Smith, & March, 1980; Guadagnoli & Ward, 1998; National Institutes of Health; Stewart et al., 2000), less attention has been directed at more generally assessing an individual's innate ability to seek out information, understand, and remember physicians' explanations and instructions. Prior studies have found a high prevalence of inadequate question-asking, misunderstanding, and poor recall of health information within the clinical encounter, especially among individuals with limited health literacy (Davis, Wolf, Bass, Tilson, & Neuberger, 2006; Katz, Jacobson, Veledar, & Kripalani, 2007; Wolf et al., 2004). At the conclusion of a medical encounter, it is essential that patients are able to effectively obtain and use relevant information to support proper adherence with self-care instructions.
We sought to create a brief assessment of patients' self efficacy to obtain, understand, and recall information from their physicians. Self-efficacy refers to an individual's own perceived ability to perform a specified behavior or set of behaviors (Bandura, 1977). This is a construct central to social cognitive theory, which proposes that behaviors are determined not solely by knowledge, but rather by the outcome and efficacy expectations related to performing them (Bandura, 1977, 1986). Despite the plethora of health related self-efficacy scales already in existence (see Frei, Svarin, Steurer-Stey, & Puhan, 2009 for a limited review of instruments in a chronic disease setting), the focus on disease-related behaviors rather than communication limits their utility in understanding patient's ability to obtain and act on relevant health information. This scale therefore aims to explicitly assess patients' self-reported confidence and ability to ask, understand, and remember information in a clinical setting. The development of this new tool—the Ask, Understand, Remember Assessment (AURA)—is herein introduced and validated against a current chronic disease self-efficacy scale (Lorig, Chastain, Ung, Shoor, & Holman, 1989) and hypertension knowledge assessment (Gazmararian, Williams, Peel, & Baker, 2003).
Methods
Setting and Participants
Consecutive patients with diagnosed hypertension and scheduled appointments were recruited from safety-net clinics in Grand Rapids, Michigan, Chicago, Illinois, and Shreveport, Louisiana. Methods have been described previously (Pandit et al., 2009; Persell, Bailey, Tang, Davis, & Wolf, 2010). Clinics in Grand Rapids and Chicago were affiliated with federally qualified health centers. Study procedures were approved by Institutional Review Boards at each location. Eligible participants were at least 18 years old, had a diagnosis of hypertension in their medical record, and had a clinic appointment between July 2006 and August 2007. Patients were ineligible if they did not speak English or if the clinic nurse determined (by interaction or chart documentation) they were too ill or cognitively impaired to participate. Nurses reviewed medical records of scheduled patients, identified those potentially eligible for the study, and referred them to study staff. The study staff then met with interested patients, obtained consent, and scheduled interviews.
Procedure
Study personnel conducted in-person interviews in the clinic waiting-room while patients waited for their appointment. The demographic and health status variables, age, sex, race/ethnicity, education, and employment status, self-reported overall health, height, weight, chronic medical conditions, smoking history, and alcohol use were collected. Health literacy was assessed using the short version of the Test of Functional Health Literacy in Adults (S-TOFHLA) (Parker, Baker, Williams, & Nurss, 1995). Scores on the S-TOFHLA range from 0 to 100. Patients were classified as having ‘inadequate’ literacy when they scored between 0 and 55, “marginal” literacy when they scored between 56 and 66, or “adequate” literacy when they scored between 67 and 100.
Measures Used for Scale Validation
Hypertension knowledge was assessed by asking patients a series of questions about the characteristics and symptoms of high blood pressure. Fourteen hypertension-specific multiple choice items made up the scale and a total score was taken from all questions (Gazmararian et al., 2003). Patients were asked about a normal blood pressure reading, common activities that change blood pressure readings, symptoms of high blood pressure, and possible outcomes. Chronic disease self efficacy was measured using the General Self Efficacy/Manage Disease in General Subscale of a previously validated scale (Lorig et al., 1989; Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001).
Ask, Understand, Remember Assessment (AURA) Scale Development
Items from two subscales from the Communication and Attitudinal Self-Efficacy (CASE) – Cancer measure (Wolf, Chang, Davis, & Makoul, 2005) were modified to more generally reflect seeking and understanding health information, removing any specific disease context (i.e., cancer). Each of the items was written at a fifth to sixth grade reading level or below, as determined by Lexile analysis, a widely used measure of reading difficulty applied to texts (MetaMetrics; Stenner, Horabin, Smith, & Smith, 1998; White & Clement, 2001). Even though the questionnaire is meant to be administered and facilitated by research staff, the readability of the document indicates that the phrasing of questions, statements, and instructions should be understandable for most patients un-assisted. Twelve items made up the original CASE-Cancer. Cancer-specific questions or those that were relevant to inpatient care were removed, leaving six items that best reflected the purpose intended.
Data Analyses
All analyses were performed using STATA version 9 (College Station, TX). Principal components (PC) analysis with Varimax rotation was used to assess if there was an underlying factor related to communication self efficacy (construct validity), while Cronbach's alpha was used to determine if examine reliability (internal consistency) of the scale. To examine the predictive validity of the tool, it was postulated that higher scores would correspond with greater disease and treatment knowledge.
Results
The sample for this study was largely female and African American; Table 1 summarizes the sociodemographic and clinical characteristics of patients. Most patients had at least one comorbid condition, and all were prescribed at least one medication for hypertension. There was good distribution of health literacy scores, categorized as low (n=100; 30.3%), marginal (n=27; 8.2%), or adequate (n=203; 61.5%).
Table 1. Sociodemographic and clinical characteristics of sample (N=330).
| Variable | Summary value |
|---|---|
| Age, M (SD) | 53.58 (12.0) |
| Female, % | 67.9 |
| African American, % | 78.5 |
| Education, % | |
| <High School | 13.0 |
| Some High School | 26.1 |
| High School Graduate | 31.2 |
| >High School | 29.1 |
| Married, % | 30.7 |
| Insurance Coverage, % | |
| Private | 19.4 |
| Medicare | 9.9 |
| Medicaid | 27.8 |
| None/free care | 42.9 |
| Employment, % | |
| Full-time | 20.9 |
| Part-time | 13.3 |
| Unemployed/retired | 65.8 |
| Site, % | |
| Chicago, IL | 30.6 |
| Grand Rapids, MI | 36.1 |
| Shreveport, LA | 33.3 |
| Number of hypertension medications, % | |
| 1 | 44.3 |
| 2 | 34.1 |
| ≥3 | 21.6 |
| Number of comorbidities, % | |
| 0 | 15.6 |
| 1 | 33.7 |
| 2 | 28.3 |
| ≥3 | 23.5 |
| Systolic, mean (SD) mmHg | 139.2 (21.8) |
| Diastolic, mean (SD) mmHg | 81.9 (15.4) |
As shown in Table 2, four of six items strongly loaded to a single factor, with a Cronbach's alpha of 0.75. Two items were dropped, as factor loadings were <0.60—“It is easy for me to ask nurses questions” and “It is easy for me to follow through on my doctor's instructions”—further demonstrating strong internal consistency. The four items that remained in the AURA have a reading level estimated at the fifth grade as documented by Lexile analysis. With a range from 4 to 16, the mean score on the AURA was 14.4 (SD=2.2). In assessing construct validity, AURA scores were strongly correlated with the total score from the Lorig chronic disease self-management self-efficacy scale (range 5 to 50, M = 37.2 (SD = 9.6); r = 0.31) and moderately correlated with disease knowledge (range 2 to 15, M = 11.0 (SD = 2.3); r = .11). Patients with low health literacy had lower total scores on the AURA than those with marginal or adequate health literacy (14.0 v. 14.9 v. 14.6, p < .05). In multivariate regression analysis, no other significant differences in AURA performance were noted by age, number of comorbidities, number of hypertension medications, or clinic site.
Table 2. Principal components analysis.
| Items | Factor loading | Proportion of variance explained (Eigenvalue) | Cronbach α |
|---|---|---|---|
| 1. It is easy for me to ask my doctor questions. | 0.78 | 0.58 (2.33) | 0.75 |
| 2. It is easy for me to ask for help if I don't understand something. | 0.76 | ||
| 3. It is easy for me to understand my doctor's instructions. | 0.76 | ||
| 4. It is easy for me to remember my doctor's instructions. | 0.74 | ||
| 5. It is easy for me to follow through on my doctor's instructions | <0.6 | ||
| 6. It is easy for me to ask nurses questions | <0.6 |
Discussion
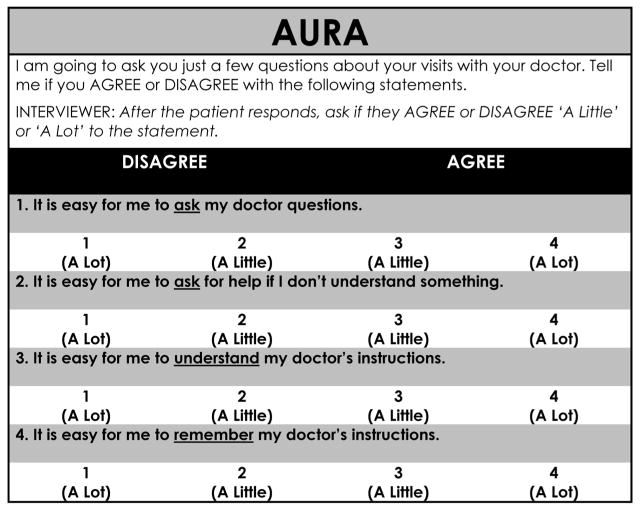
The AURA was designed to be a brief and simple measure of a patient's perceived self-efficacy to obtain, understand, and remember health information from his or her physician. Self-efficacy may be relevant to a patient's ability to participate in and act on information from medical encounters. We found that the AURA is strongly correlated with a previously validated self-efficacy scale for chronic disease patients. However, due to its general nature, we believe the AURA is appropriate for patients both with and without chronic illness (see Figure 1).
Figure 1.
The Ask, Understand, Remember Assessment (AURA).
Other scales have attempted to measure related constructs such as patient activation (Hibbard, Mahoney, Stockard, & Tusler, 2005; Hibbard, Stockard, Mahoney, & Tusler, 2004), health locus of control (Wallston, 2005; Wallston, Wallston, & DeVellis, 1978), and self efficacy in specific contexts such as chronic disease (Frei et al., 2009; Lorig et al., 1989; Lorig et al., 2001), and behavior change (Velicer, Diclemente, Rossi, & Prochaska, 1990). However, these are all limited in their utility in a more general clinical sense. First, these measures are longer and less likely to be used in a clinical context. Second, self-efficacy measures for chronic disease and behavior change may not specifically address patients' perceived ability to communicate with providers, which is increasingly seen as a target for many health promotion and health literacy strategies. Third, as Frei and coworkers (2009) pointed out in their recent review, many of these self-efficacy scales have methodological limitations. These authors also delineated a systematic approach to development and validation of self-efficacy instruments. In line with their recommendations, the AURA was developed with a clear aim and used statistical techniques to select items and evaluate the final instrument. Our scale may complement tools such as the Patient Activation Measure (Hibbard et al., 2005; Hibbard et al., 2004) which appropriately addresses motivational factors in the context of healthcare, but does not assess the interaction between patients and clinicians.
The AURA indicates one's confidence in the ability to perform certain necessary tasks for participating in one's health care, and it may be particularly useful for testing the effect of interventions designed to improve patient participation, communication, or other enhancements to the patient-provider relationship. As patients with low self-efficacy may not articulate their lack of understanding or ask questions, the AURA may also be useful in identifying and assisting patients who are at risk for errors or non-adherence with self-care behaviors. Because of its very low level of reading difficulty, it may also be used as a patient-reported written measure among many patients with inadequate or marginal health literacy.
Limitations to this study should be noted. Subjects recruited for this study were patients of safety-net clinics and were diagnosed with hypertension; our results may not be generalizable to patients receiving care in other setting or who have other health conditions. The items in the scale are specific to patient interactions with a physician. Health care services and treatment are often provided by other medical professionals such as nurses, physician's assistants, and medical assistants, especially in clinics with few resources. Further psychometric testing should be conducted in a general patient population, and the association between performance on the AURA and actual clinical outcomes should be further studied. The AURA has promise to assess perceived self-efficacy that supports the asking, understanding, and remembering of important self-management information in a clinical setting.
Acknowledgments
Research and faculty support was provided by research grants from the Michigan Department of Community Health and Pfizer Corporation.
References
- Abraido-Lanza AF, Chao MT, Gates CY. Acculturation and cancer screening among Latinas: Results from the National Health Interview Survey. Annals of Behavior Medicine. 2005;29(1):22–28. doi: 10.1207/s15324796abm2901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychology Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. A social foundation of thought and action A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bruera E, Willey JS, Palmer JL, Rosales M. Treatment decisions for breast carcinoma: Patient preferences and physician perceptions. Cancer. 2002;94(7):2076–2080. doi: 10.1002/cncr.10393. [DOI] [PubMed] [Google Scholar]
- Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Annals of Internal Medicine. 1980;92(6):832–836. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- Cegala DJ. A study of doctors' and patients' communication during a primary care consultation: Implications for communication training. Journal of Health Communication. 1997;2(3):169–194. doi: 10.1080/108107397127743. [DOI] [PubMed] [Google Scholar]
- Cegala DJ, Street RL, Jr, Clinch CR. The impact of patient participation on physicians' information provision during a primary care medical interview. Health Communication. 2007;21(2):177–185. doi: 10.1080/10410230701307824. [DOI] [PubMed] [Google Scholar]
- Davis T, Wolf M, Bass P, Tilson H, Neuberger M. Literacy and misunderstanding of prescription drug labels. Annals of Internal Medicine. 2006;145:887–894. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- Frei A, Svarin A, Steurer-Stey C, Puhan MA. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations—A systematic review. Health Quality and Life Outcomes. 2009;7:86–95. doi: 10.1186/1477-7525-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Education Counseling. 2003;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Annals of Internal Medicine. 1985;102(4):520–528. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients' participation in medical care: Effects on blood sugar control and quality of life in diabetes. Journal of General Internal Medicine. 1988;3(5):448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- Guadagnoli E, Soumerai SB, Gurwitz JH, Borbas C, Shapiro CL, Weeks JC, et al. Improving discussion of surgical treatment options for patients with breast cancer: local medical opinion leaders versus audit and performance feedback. Breast Cancer Research and Treatment. 2000;61(2):171–175. doi: 10.1023/a:1006475012861. [DOI] [PubMed] [Google Scholar]
- Guadagnoli E, Ward P. Patient participation in decision-making. Social Science Medicine. 1998;47(3):329–339. doi: 10.1016/s0277-9536(98)00059-8. [DOI] [PubMed] [Google Scholar]
- Harrington J, Noble LM, Newman SP. Improving patients' communication with doctors: A systematic review of intervention studies. Patient Education and Counseling. 2004;52(1):7–16. doi: 10.1016/s0738-3991(03)00017-x. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Service Research. 2005;40(6 Pt 1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Service Research. 2004;39(4 Pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: A mixed-methods analysis. Journal of General Internal Medicine. 2007;22(6):782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Chastain R, Ung E, Shoor S, Holman H. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis and Rheumatism. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice. 2001;4(6):256–262. [PubMed] [Google Scholar]
- MetaMetrics, I. MetaMetrics, Inc. 1000 Park Forty Plaza Drive, Suite 120, Durham, North Carolina 27713. Lexile Analyzer: www.lexile.com
- National Institutes of Health. The Patient Reported Outcomes Measurement Information System (PROMIS): Dynamic tools to measure health outcomes from the patient perspective. Available at http://www.nihpromis.org/default.aspx.
- Pandit AU, Tang JW, Bailey SC, Davis TC, Bocchini MV, Persell SD, et al. Education, literacy, and health: Mediating effects on hypertension knowledge and control. Patient Education and Counseling. 2009;75(3):381–385. doi: 10.1016/j.pec.2009.04.006. [DOI] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. Journal of General Internal Medicine. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- Persell SD, Bailey SC, Tang J, Davis TC, Wolf MS. Medication reconciliation and hypertension control. American Journal of Medicine. 2010;123(2):182.e9–182.e15. doi: 10.1016/j.amjmed.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Roter DL. Patient question asking in physician-patient interaction. Health Psychology. 1984;3(5):395–409. [PubMed] [Google Scholar]
- Stenner A, Horabin I, Smith D, Smith M. The Lexile framework. Durham, NC: Metametrics, Inc; 1998. [Google Scholar]
- Stewart DE, Wong F, Cheung AM, Dancey J, Meana M, Cameron JI, et al. Information needs and decisional preferences among women with ovarian cancer. Gynecologic Oncology. 2000;77(3):357–361. doi: 10.1006/gyno.2000.5799. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Gordon HS. The clinical context and patient participation in post-diagnostic consultations. Patient Education and Counseling. 2006;64(1–3):217–224. doi: 10.1016/j.pec.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: Why some patients are more involved than others. Medical Care. 2005;43(10):960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- Street RL, Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Education and Counseling. 2009;74(3):295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- Velicer W, Diclemente C, Rossi J, Prochaska J. Relapse situations and self-efficacy: An integrative model. Addictive Behavior. 1990;15:271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- Wallston KA. The validity of the multidimensional health locus of control scales. Journal of Health Psychology. 2005;10(5):623–631. doi: 10.1177/1359105305055304. [DOI] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) scales. Health Education Monographs. 1978;6(2):160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- White S, Clement J. Assessing the Lexile Framework: Results of a panel meeting. NCES Working Paper Series, Working Paper No. 2001–08 2001 [Google Scholar]
- Wolf MS, Chang CH, Davis T, Makoul G. Development and validation of the Communication and Attitudinal Self-Efficacy scale for cancer (CASE-cancer) Patient Education and Counseling. 2005;57(3):333–341. doi: 10.1016/j.pec.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Davis TC, Cross JT, Marin E, Green K, Bennett CL. Health literacy and patient knowledge in a Southern US HIV clinic. International Journal of Sexually Transmitted Diseases and AIDS. 2004;15(11):747–752. doi: 10.1258/0956462042395131. [DOI] [PubMed] [Google Scholar]