Abstract
Objective
To assess conflict styles and construct validity of the Thomas-Kilmann Mode of Conflict Instrument (TKI) among medical education personnel.
Methods
From 2006 to 2009, 23 board-certified physicians (faculty), 46 residents, and 31 graduate medical education (GME) administrators participated in 3 behavior surveys. We used self-reported data (as completed by participants on the questionnaire). The TKI defines 5 conflict styles: competing, collaborating, compromising, accommodating, and avoiding. The My Best Communication Style Survey assesses 4 styles of communication: bold, expressive, sympathetic, and technical. The Interpersonal Influence Inventory categorizes 4 behavior styles: openly aggressive, assertive, concealed aggressive, and passive behaviors. A P value of < .05 was significant.
Results
Avoiding was the conflict style most chosen, closely followed by compromising and accommodating, whereas collaborating was the least likely to be selected. Collaborating percentiles were highest in GME administrators and lowest in faculty. Competing percentiles decreased from faculty to GME administrators (r = −0.237, P = .017). Openly aggressive scores were highest in faculty and lowest in GME administrators (P = .028). Technical communication scores were highest in residents and lowest in GME administrators (P = .008). Technical communication scores were highest in African Americans (P = .000). Asian Americans were more likely to be high in accommodating style (P = .019). Midwest respondents selected the collaborating style more than others did (41.3% versus 25%) (P = .009). Competing conflict style correlated positively with openly aggressive behavior and bold communication but negatively with expressive and sympathetic communications.
Conclusion
There are differences in behavior patterns among faculty, residents, and GME administrators with suggestions of ethnic and geographic influences. Correlation among instruments supported theoretical relationships of construct validity.
Introduction
Emotional intelligence is described as the capacity for recognizing one's feelings and those of others; managing one's own emotions as well as those of others; and motivating oneself and others.1 Studies demonstrate that emotional intelligence outweighs intelligence quotient in determining leadership; when star performers were compared with average performers in senior leadership positions, nearly 90% of the difference was attributed to emotional intelligence.1
Medical education administrators, residents, and board-certified physicians navigate conflict and disagreement daily to foster teamwork among coworkers in complex work environments such as the hospital. The ability to effectively communicate and interact with various personality types enables physicians to maintain a work environment conducive to harmony, teamwork, and success. The ability to traverse human conflict in the work setting often rests on the concept of emotional intelligence.1
The components of emotional intelligence are self-awareness, self-regulation, social awareness, and relationship management.1 Self-awareness is defined as the ability to recognize and understand one's moods, emotions, and drives and their effect on others. High self-awareness is the basic building block of emotional intelligence. The primary cause of derailment in executives involves deficits in emotional intelligence, especially in difficulty handling change, not being able to work well in a team, and poor interpersonal relations.1 Thus, tools that measure behavior could be useful in developing self-awareness and potentially in improving emotional intelligence.
A commonly used tool for assessing self-awareness is the Thomas-Kilmann Conflict Mode Instrument (TKI). Conflict is inevitable and encountered frequently each day in all professions. The inability to resolve conflict appropriately can affect team function, which can contribute to medical errors and patient-safety concerns. The TKI describes 5 means of dealing with conflict: competing, collaborating, compromising, avoiding, and accommodating.2 Individuals with the competing style pursue personal concerns at the expense of others, in a win-lose model. Collaborating entails working with others to find a solution that is amenable to all involved. Compromising requires an expedient, mutually acceptable solution that partially satisfies both parties, such as seeking a quick, middle-ground position. Avoiding does not pursue personal concerns or the concerns of others by not addressing the conflict. The accommodating style neglects personal concerns to satisfy the concerns of others.2 Most studies in medical education regarding conflict have been in nursing with few studies of medical students, residents, or physicians.3,4 In a sample of nursing and allied health students, compromise was the prevalent style of nurses, followed by avoiding; avoiding and compromise and accommodation were the prevalent styles for the allied health students.4 Mean and normative values for the TKI have been developed from a group of middle- and upper-level managers in business and government organizations with a test-retest reliability of 0.61 to 0.68.2
The objective of this study was to assess the prevalence and differences in the conflict-management styles of a cohort of graduate medical education (GME) administrators, residents, and board-certified academic physician faculty. Construct validity examines the validity of a tool on a theoretical level. A construct is an abstract idea or concept for which theoretical relationships can be specified. These theoretical relationships can be empirically tested. If the presumed relationships exist, the instrument is thought to have high validity. Our second objective was to compare the TKI conflict styles measure with 2 other behavior-assessment tools: the Interpersonal Influence Inventory (III)5 and the My Best Communication Style (MBCS).6,7
We hypothesized there were differences among the preferred conflict styles of different medical education personnel and the 3 behavioral instruments surveyed would demonstrate those preferences with construct validity.
Materials and Methods
This study is based on a convenience sample of respondents who completed 3 behavioral surveys (the TKI, the III, and the MBCS) at educational conferences from 2006 to 2009 as part of educational seminars on emotional intelligence. The time to complete the surveys ranged from 25 to 45 minutes. The conferences included the American College of Obstetricians and Gynecologists Annual Conference, the Accreditation Council for Graduate Medical Educational Annual Conference, and a Residents' Forum at the National Medical Association Annual Conference. Exempt status was granted by the Institution Review Board because only deidentified information was used in this study.
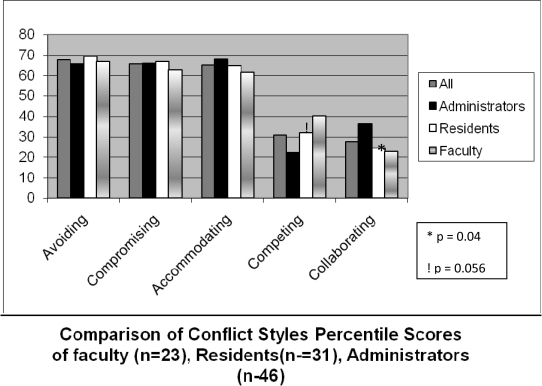
The TKI is a forced-choice measure consisting of 30 statement pairs, each illustrating one of the 5 conflict modes. Respondents must choose one statement from each pair that best describes how they respond to conflict situations. Each conflict mode is represented 12 times, and a maximum score of 12 can be achieved for each mode. Scores are categorized as high or low for each conflict mode if they are in the top or bottom 25th percentile, respectively. Respondents were asked to complete the TKI instrument as they would respond at work, not at home. The figure gives an example of a TKI profile.
FIGURE.
Example of a Thomas-Kilmann Mode of Conflict Instrument (TKI) Profile
Definitions: faculty, board-certified physicians who were residency program directors or academic faculty who supervised residents; GME administrator, nonphysician personnel in graduate medical education administration or residency program coordinators; residents, postgraduate trainees in an approved Accreditation Council for Graduate Medical Education residency training program.
The III is based on an assertive-behavior model and assesses how the participant chooses to influence others. The model determines 2 sets of behaviors to create 4 influence styles. The 2 behaviors are (1) the degree of openness in communication or candor (willingness to reveal thoughts, feelings, or experiences), and (2) consideration for others. The 4 influence styles are (1) openly aggressive, in which the individual has a high degree of openness in communication but little consideration for the thoughts and feelings of the other party; (2) assertive, in which the individual has a high degree of openness in communication and is also respectful of the rights of others; (3) concealed aggressive, in which the individual is not open in communication, is not open about motives, and does not consider the rights of others; and (4) passive behavior, which is self denying and accords more rights to others. The instrument contains 40 questions relating to each of the 4 influence patterns. Each question is assigned a value of 0 to 4 depending on how well the respondent believes the statement is characteristic of his or her behavior. The scores are plotted on an influence profile, which is normalized from a sample of department managers and retail buyers.5–9
The MBCS survey determines 4 styles: expressive, bold, sympathetic, and technical. Expressive communicators enjoy talking to people, are good presenters, and relate well to people. Bold communicators are direct, like the bottom line, are blunt, and are practical. They are good problem solvers but can be accused of not listening. Sympathetic communicators are quiet and calm. They are good listeners. Technical communicators are orderly, detailed, and logical. They work well with numbers and may be perceived as perfectionists. The MBCS survey contains 18 questions on styles of communication, with each having 4 options to represent the different communication styles.9–12
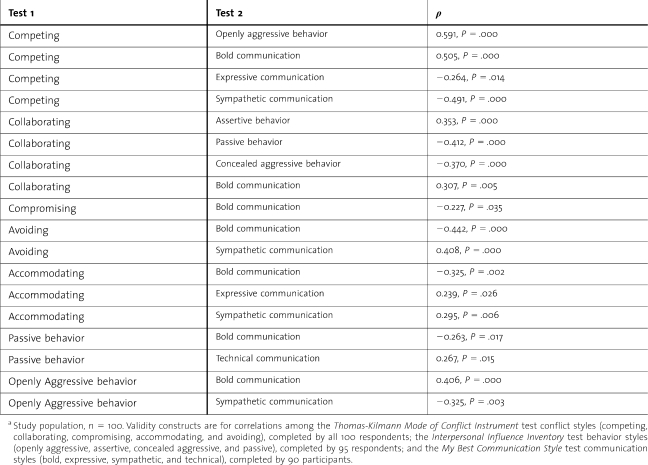
Construct validity theory suggests that the construct of competing on the TKI should correlate with openly aggressive behavior on the III and bold communication on the MBCS. Conversely, the competing conflict style should correlate negatively with passive behavior on the III and sympathetic communication on the MBCS.
Statistical analysis was performed using SPSS 17.0 software (SPSS Inc, Chicago, IL) to assess the associations among the conflict-style scores, the other behavior instruments, and respondents' self-reported medical education personnel categories, gender, ethnicity, and geographic distribution of respondents. Significance was established at P < .05. A χ2 test was used for comparison of discrete variables, a Student t test for continuous variables, and a Spearman rank analysis for correlation analysis. An analysis of variance was used for multiple comparisons, and a Bonferroni post hoc test was performed for multiple comparisons.
Results
The study population consisted of 100 medical education professionals, including 23 board-certified physicians (faculty), 46 residents, and 31 GME administrators. We excluded 15 respondents because of incomplete data. The TKI was completed by all 100 respondents, 95 completed the III, and the My Best Communication Style survey was completed by 90 participants. The faculty cohort consisted of board-certified physicians who were residency program directors or academic faculty members who trained residents. The GME administrators were nonphysician personnel in GME administration or residency program coordinators. Both academic faculty and GME administrators included all medical specialties, whereas the residents were mainly from obstetrics and gynecology. The regional distributions of the participants in United States were 53% from the West, 19% from the South, 16% from the Midwest, and 13% from the Northeast. Of the participants, 68% were women; 64% were non-Hispanic whites, 21% Asian Americans, 9% African American, and 6% Hispanic. Of the residents in the study, 32% were postgraduate year (PGY)-1, 22% PGY-2, 24% PGY-3, and 22% PGY-4.
The figure shows mean percentiles for all participants and the categories of residents, administrators, and faculty for each of the conflict management styles. Avoiding was selected as the most common conflict style of the complete set of respondents, followed closely by compromising and accommodating. The participants as a group selected collaborating as the style least likely to be used. The GME administrators had the highest collaborating percentiles, whereas the faculty had the lowest (faculty, 22.7%; residents, 24.4%; GME administrators, 36.1%; P = .08). Faculty had the highest competing scores, and GME administrators had the lowest (faculty, 40.3%; residents, 31.9%; GME administrators, 22.0%; P = .057). The GME administrators, when compared with all physicians (residents and physician faculty), had significantly higher collaborating percentile scores (35.6% versus 23.8%; P = .014) and significantly lower competing scores (22.4% versus 34.7%; P = .04). Respondents from the Midwest selected the collaborating style more than did respondents from other US regions (mean percentile for Midwest was 41.3% compared with 25.0% for all other regions; P = .009). The percentile scores for conflict style for men versus women were as follows: competing, 37.5% versus 28.6%; collaborating, 23.6% versus 29.8%; compromising, 64.2% versus 65.9%; avoiding, 65.9% versus 68.1%; accommodating, 59.4% versus 67.3%; and none of these differences were statistically significant.
Individuals in the 75th percentile and greater in choosing a conflict management style were classified as high for the specific conflict style. Percentage of respondents classified as high for each conflict style were as follows: high competing, 9%; high collaborating, 7%; high compromising, 39%; high avoiding, 51%; and high accommodating, 34%. Conflict style with the highest percentile for each individual is classified as the primary style. Percentage of respondents who were primary for each conflict style were as follows: primary competing, 11%; primary collaborating, 4%; primary compromising, 32%; primary avoiding, 39%; and primary accommodating, 21%. Avoiding and compromising were the most common high and primary styles of the participants in this study. Analysis showed that competing as a primary style was significantly different among faculty (22%), residents (13%), and GME administrators (0%) (P = .034). Asian Americans were more likely to be high in the accommodating style (57% versus 28%; P = .019; odds ratio [OR] = 3.5) and non-Hispanic whites were also significantly more likely not to be in the high quartile in the accommodating style (27% versus 47%; P = .048; OR = 2.47). Because there were so few respondents who selected collaborating as a primary or high style, we analyzed the collaborating style by comparing the lowest quartile versus those in moderate and high quartiles. Faculty had the lowest quartile for the collaborating style at 70%, compared with residents at 59%, and GME administrators at 42% (P = .04).
Correlation analysis showed that percentiles for the competing style significantly decreased from faculty to residents to GME administrators (r = −0.241; P = .016), whereas the collaborating scores increased from faculty through residents to GME administrators (r = 0.228; P = .0236).
Interpersonal Influence Inventory
The mean scores for all participants for assertive behavior was 26.8, passive behavior was 19.7, concealed aggressive behavior 15.9, and openly aggressive behavior was 12.6. Compared with the norms for the III, the total participant group was in the low-average range for assertive behavior, very high for passive behavior, middle-average for concealed aggressive behavior, and low for openly aggressive behavior scores. Openly aggressive scores were highest in faculty and were lowest in GME administrators (faculty, 17.9; residents, 16.3; GME administrators, 14.7; P = .032). Correlation analysis also showed that scores for openly aggressive behavior decreased from all physicians (faculty and residents) to GME administrators; (r = −0.274; P = .007). Residents in PGY-2 had significantly higher scores for concealed aggressive behavior than did other residents (PGY-1, 10.13; PGY-2, 16.30; PGY-3, 14.27; PGY-4, 12.6; P = .026).
The communicati`on style mean scores for the total participant population were as follows: sympathetic communication, 5.24; technical, 4.76; bold, 4.75; and expressive, 3.67. The only significant differences were found with technical communication, which was highest in residents and lowest in GME administrators (faculty, 4.67; residents, 5.7; GME administrators, 3.77; P = .008). Technical communication was also higher for African Americans compared with other ethnicities (African Americans, 8; non-Hispanic whites, 4.62; Asian, 4.33; Hispanic 4.78; P = .000).
Construct Validity Testing
The table shows the significant correlations among the behavior assessment tools. This shows that the competing conflict style correlated strongly and positively with openly aggressive behavior and bold communication but correlated negatively with both expressive and sympathetic communication. The collaborating conflict style correlated positively with assertive behavior and bold communication but negatively with passive behavior and concealed aggressive behavior. The avoiding conflict style correlated positively with sympathetic communication but negatively with bold communication. The accommodating conflict style correlated positively with both expressive and sympathetic communication but negatively with bold communication. In addition, the passive behavior style correlated positively with technical communication but negatively with bold communication, whereas openly aggressive behavior correlated positively with bold communication but negatively with sympathetic communication.
TABLE.
Significant Correlations Among Behavior Assessment Tools in a Cohort of Medical Personnel Supporting Construct Validitya
Discussion
Our study demonstrates that competing and collaborating conflict styles were least used by this cohort of board-certified physicians in academic medicine, residents, and GME administrators. This is comparable with the findings from previous studies in health care, demonstrating that compromising, avoiding, and accommodating were the preferred styles of nurses, nursing students, and allied health students with a low use of collaboration.3,4 Successful collaboration involves being able to manage one's emotions appropriately (self-management) while using the awareness of the emotions of other people (social awareness) involved in the conflict to manage the conflict to a successful outcome (relationship management). This suggests that emotional intelligence training may be helpful in problem-solving and team-building in health care teams. The higher collaborating and lower competing styles of the GME administrators in this study may reflect the conundrum of their positions. The GME administrators have to understand and implement the dictates of busy faculty and program directors while creating a trusting relationship with trainees to facilitate compliance with program requirements.
The finding that respondents from the Midwest were significantly more likely to use the collaboration style suggests a geographic influence on behavior while the result showing that Asian Americans had significantly higher scores for the accommodating style suggests a cultural influence. This is comparable to a survey13 demonstrating that Asian medical students were less assertive and more reticent than other racial/ethnic cohorts. A recent study14 on emotional intelligence using the Mayer-Salovey-Caruso Emotional Intelligence test also suggested that Asian medical students had higher emotional intelligence scores. These demographic findings may emphasize the importance of local customs, traditions and cultural preferences, or communication influences on behavior.
The high scores for passive behavior may be compatible with humanistic attributes and a demonstration of empathy because passive behavior is associated with self-denial and a high consideration for others.15,16 Although openly aggressive behavior scores were low overall, they were still highest in faculty and lowest in GME administrators. The higher use of a competing style and aggressive behavior by faculty is consistent with the principle that competing is the power mode and it is more likely to be used by those in higher authority to resolve conflicts.17
Sympathetic communication was chosen as the preferred style of communication. This may also be compatible with good bedside manners and interpersonal skills because the sympathetic communicator is a good listener, quiet, and calm when communicating.
The correlations among the 3 assessment tests that are based on theoretical concepts support the construct validity of the utility of these behavior tests for health care professionals. Behavior assessment tools can be used to instruct and intervene in the dynamics of the health care team to improve patient safety and decrease medical errors. Curricula on teamwork, conflict resolution, and quality improvement have been shown to be helpful in teaching these principles to residents.18
The limitations of this study include its small sample size, that residents were from one specialty (obstetrics-gynecology), and that the data were collected for educational reasons. All of this reduce the generalizability of the findings. At the same time, to our knowledge, this is the first study that has evaluated 3 different behavior instruments in different groups of medical education personnel from different regions of the United States. It is important that future large-scale studies be conducted to the determine behavior styles of health care professionals. The findings may help provide information on emotional intelligence that can be used to select, counsel, and train future physicians.
In conclusion, we have shown that in a cohort of medical education personnel, the conflict management style most often chosen was the avoiding style, closely followed by compromising and accommodating styles. Competing styles were highest in board-certified physicians, whereas collaborating skills were highest in GME administrators, with residents intermediate in both categories.
Footnotes
All authors are at Cedars-Sinai Medical Center. Dotun Ogunyemi, MD, Chief of In-Patient Obstetrics in the Department of Obstetrics and Gynecology and Associate Professor at the University of California at Los Angeles School (UCLA) of Medicine/Charles R. Drew University of Medicine and Science; Edward Tangchitnob, MD, is TITLE in the Department of Obstetrics and Gynecology; Yonathan Mahler, MD, is TITLE in the Department of Obstetrics and Gynecology; Connie Chung, MD, is TITLE in Department of Obstetrics and Gynecology; Carolyn Alexander, MD, is Associate Director of the Residency Program in the Department of Obstetrics, a member of the Division of Reproductive Endocrinology and Infertility and the Center for Androgen Related Research and Discovery, and an Assistant Professor at the David Geffen School of Medicine at UCLA; and Devra Korwin, MA, is the Senior Organization Development Specialist in the Organization Development Services.
Funding: The authors report no external funding source.
References
- 1.Goleman D. What makes a leader. Harv Bus Rev. 1998;76(6):93–102. [PubMed] [Google Scholar]
- 2.Kilmann RH, Thomas KW. Developing a forced-choice measure of conflict management behavior: the MODE instrument. Educ Psychol Measures. 1977;37(2):309–325. [Google Scholar]
- 3.Whitworth BS. Is there a relationship between personality type and preferred conflict-handling styles? an exploratory study of registered nurses in southern Mississippi. J Nurs Manag. 2009;16(8):921–932. doi: 10.1111/j.1365-2834.2008.00918.x. [DOI] [PubMed] [Google Scholar]
- 4.Sportsman S, Hamilton P. Conflict management styles in the health professions. J Prof Nurs. 2007;23(3):157–166. doi: 10.1016/j.profnurs.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Teambuilding, Inc. The training catalog: Interpersonal Influence Inventory. 4th ed. Available at: https://webmail.csmc.edu/exchweb/bin/redir.asp?URL=http://store.teambuildinginc.com/items/; http://store.teambuildinginc.com/items/’ ’/t “_blank” http://store.teambuildinginc.com/items/team profiles, assessments/interpersonal-influence-inventory/list.htm. Feb 1, 2010. [Google Scholar]
- 6.Glaser R. The Interpersonal Influences Inventory. Bryn Mawr, PA: Organizational Design and Development; 1983. Feb 1, 2010. [Google Scholar]
- 7.Furnham A, Rawles R. Interpersonal influence and coping strategies. Pers Individ Differ. 1994;16(2):357–361. [Google Scholar]
- 8.Glaser R. Interpersonal Influence Inventory. 4th ed. King of Prussia, PA: HRDQ; 2004. [Google Scholar]
- 9.Glaser R. The Interpersonal Influences Inventory. Bryn Mawr, PA: Organizational Design and Development; 1983. [Google Scholar]
- 10.Bastille L, Benowitz A, Gebremichael Y, Kuprasova N, O'Rourke K, Tiamiyu A. Effective communication Available at: https://webmail.csmc.edu/exchweb/bin/redir.asp? http://isites.harvard.edu/fs/docs/icb“ /t “_blank”http://isites.harvard.edu/fs/docs/icb. topic600003.files/Effective Communication-Final.ppt. Feb 1, 2010. [Google Scholar]
- 11.Brewer JH. My BEST Communication Style Interpretation. Niceville, FL: Best Instruments; 1990. http://www.bestinstruments.net/. Feb 1, 2010. [Google Scholar]
- 12.BEST Instruments. BEST User's Guide. Niceville, FL: BEST; 2003–2010; Available at: http://www.bestinstruments.net/home_catalog.htm. Accessed Feb 1, 2010. [Google Scholar]
- 13.Lee KB, Vaishnavi SN, Lau SK. M, Andriole DA, Jeffe DB. “Making the grade:” Noncognitive predictors of medical students' clinical clerkship grades. J Natl Med Assoc. 2007;99(10):1138–1150. [PMC free article] [PubMed] [Google Scholar]
- 14.Carr SE. Emotional intelligence in medical students: does it correlate with selection measures. Med Educ. 2009;43(11):1069–1077. doi: 10.1111/j.1365-2923.2009.03496.x. [DOI] [PubMed] [Google Scholar]
- 15.Crandall SJ, Marion GS. Commentary: identifying attitudes towards empathy: an essential feature of professionalism. Acad Med. 2009;84(9):1174–1176. doi: 10.1097/ACM.0b013e3181b17b11. [DOI] [PubMed] [Google Scholar]
- 16.Brannick MT, Wahi MM, Arce M, Johnson H, Nazian S, Goldin SB. Comparison of trait and ability measures of emotional intelligence in medical students. Med Educ. 2009;43(11):1062–1068. doi: 10.1111/j.1365-2923.2009.03430.x. [DOI] [PubMed] [Google Scholar]
- 17.Vivar CG. Putting conflict management into practice: a nursing case study. J Nurs Manag. 2006;14(3):201–206. doi: 10.1111/j.1365-2934.2006.00554.x. [DOI] [PubMed] [Google Scholar]
- 18.Stergiopoulos V, Maggi J, Sockalingam S. Teaching the physician-manager role to psychiatric residents: development and implementation of a pilot curriculum. Acad Psychiatry. 2009;3(2)3):125–130. doi: 10.1176/appi.ap.33.2.125. [DOI] [PubMed] [Google Scholar]