Abstract
Background
Recent efforts to increase insurance coverage have revealed limits in primary care capacity, in part due to physician maldistribution. Of interest to policymakers and educators is the impact of nontraditional curricula, including global health education, on eventual physician location. We sought to measure the association between graduate medical education in global health and subsequent care of the underserved in the United States.
Methods
In 2005, we surveyed 137 graduates of a family medicine program with one of the country's longest-running international health tracks (IHTs). We compared graduates of the IHT, those in the traditional residency track, and graduates prior to IHT implementation, assessing the anticipated and actual involvement in care of rural and other underserved populations, physician characteristics, and practice location and practice population.
Results
IHT participants were more likely to practice abroad and care for the underserved in the United States in the first 5 years following residency than non-IHT peers. Their current practices were more likely to be in underserved settings and they had higher percentages of uninsured and non–English-speaking patients. Comparisons between pre-IHT and post-IHT inception showed that in the first 5 years following residency, post-IHT graduates were more likely to care for the underserved and practice in rural areas and were likely to offer volunteer community health care services but were not more likely to practice abroad or to be in an academic practice.
Conclusions
Presence of an IHT was associated with increased care of underserved populations. After the institution of an IHT track, this association was seen among IHT participants and nonparticipants and was not associated with increased long-term service abroad.
Editor's Note: The online version of this article contains the survey instrument (200.5KB, doc) used in this study.
Introduction
One of the lessons from the universal insurance mandate in Massachusetts is the need to address primary care infrastructure.1 Nearly 75% of US counties are health professional shortage areas and/or medically underserved areas. Geographic deficits and primary to specialty care ratio imbalances will not be successfully addressed by medical school expansion without curricular and policy changes that promote equitable workforce distribution.2,3 A recent Cochrane review found little evidence that existing educational, financial, and regulatory strategies were effective.4
At the same time, some evidence supports the impact of strategies that include targeted recruitment of rural-born individuals, individuals from underrepresented minorities, and those with primary care exposure on primary care specialty choice and underserved practice location.5,6
As health care reform measures may double the capacity of federally qualified health centers (FQHCs) for the second time in a decade, the absence of sufficient primary care physicians working in underserved areas is glaring.7–9 Funding of medical education expansion lacks targeted approaches to changing the distribution of the workforce toward underserved areas.10 This results in a need to identify and implement educational interventions that can affect the proportion of the workforce caring for underserved populations.
In 1994, The University of Cincinnati Family Medicine Residency Program initiated an international health track (IHT) to meet residents' demand for global health training. The basic structure consists of 3 components: (1) international health didactics, (2) clinical and public health experiences in developing nations, and (3) travel medicine training.
A survey of graduates was undertaken to determine if there was an association between participating in the IHT and caring for underserved populations in the United States. We investigated whether IHT graduates were more likely to care for underserved populations compared with nonparticipants (non-IHT) and whether all graduates following inception of the IHT (post-IHT), regardless of individual participation in the IHT, were more likely to enter practices caring for the underserved than graduates prior to its inception (pre-IHT). The study was conducted as part of a survey that also investigated 2 other questions: (1) changes in skills, knowledge, and attitudes regarding international health and (2) the effectiveness of the IHT as a recruitment tool for University of Cincinnati Family Medicine Residency Program (published elsewhere).11
Methods
Participants
The study population included graduates between 1989 and 2003 (N = 137). Subpopulations included IHT graduates (N = 43), non-IHT graduates (N = 52), and graduates during the 5 years prior to IHT implementation (N = 45).
Survey
Knowledge and attitude questions on the survey were adapted, with permission, from previous surveys of IHT graduates at Duke University and Yale University.12,13 Other questions, including practice descriptions (practice caring for an underserved population, practice in a community health care center including the Indian Health Service, nonprofit clinics, missionary clinics, or practice at an FQHC) and demographic information were developed by the research team (box). The instrument was refined after field testing on 5 individuals who graduated from the residency program in years not included in our study and is available as an online supplement.
box Survey Components
Physician demographics
Gender
Ethnic background
State/country of birth
Medical school attended
Year of graduation from UCFM
Involvement in IHT
Practice characteristics
Current practice setting
Current patient population traits
Current volunteerism
Knowledge and attitudes
Factors in choosing UCFM
Longitudinal attitudes and actions
International health knowledge
Abbreviations: IHT, international health track; UCFM, University of Cincinnati Family Medicine Residency Program.
Refer to online supplementary material for survey instrument.
Three options for completion were offered: Web-based, mailed, and telephone interview. The same instrument was used for all 3 options, and each required 10 to 20 minutes to complete. No incentives were offered to encourage participation.
This study was granted exempt status by the Institutional Review Board of the University of Cincinnati Medical Center.
Analysis
Descriptive data analysis, including measures of central tendency, frequencies, cross-tabulations, and correlations was conducted. Group comparisons were performed using χ2 and Mann-Whitney U tests.
Future practice plans (prior to residency graduation) and actual practice behaviors (during the 5 years following graduation) were compared for IHT versus non-IHT and pre-IHT versus post-IHT graduates. Comparisons of the current practice characteristics at the time the survey was completed were made between these same subgroups, plus pre-IHT versus IHT and pre-IHT versus non-IHT.
Results
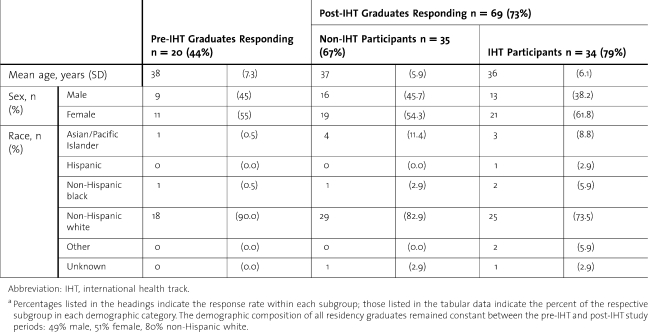
Eighty-nine graduates participated in the study, yielding a 65% response rate (table 1).
TABLE 1.
Demographic Data on Survey Respondersa
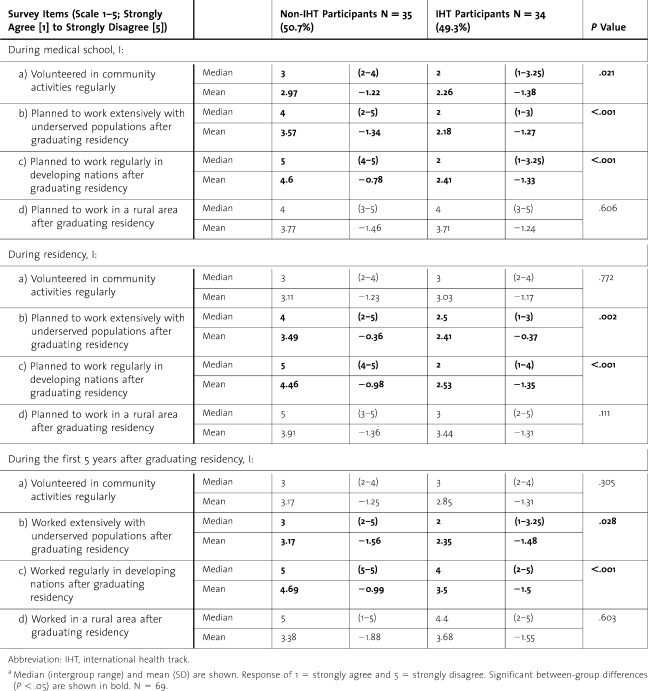
IHT Compared With Non-IHT
In their first 5 years postresidency, IHT participants were more likely to practice abroad and care for the underserved in the United States than their non-IHT peers (table 2). Differences in practice settings were consistent with differences between the groups in career goals reported in medical school and residency. Although a difference remained between the IHT and non-IHT groups in both areas during their progression from medical school to early practice, the degree of significance diminished as time progressed. There was no difference between groups in the percentage entering rural practice.
TABLE 2.
Medical Service Careers, Non-IHT Versus IHT Participantsa
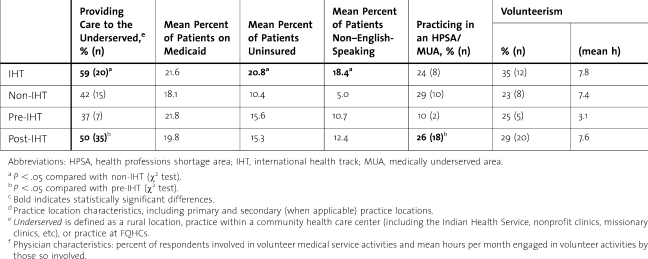
IHT graduates were more likely to provide care for the underserved and had a higher percentage of uninsured patients and non–English-speaking patients than their non-IHT peers. There was no difference between IHT (47%, n = 16) and non-IHT (43%, n = 15) participants in the percentage offering community service in a health care setting outside of their primary office, and there was no difference with respect to the proportion or extent of involvement in volunteer activities (table 3).
TABLE 3.
Practice Location Characteristics,d Practice Population Traits, and Physician Characteristicsc,f
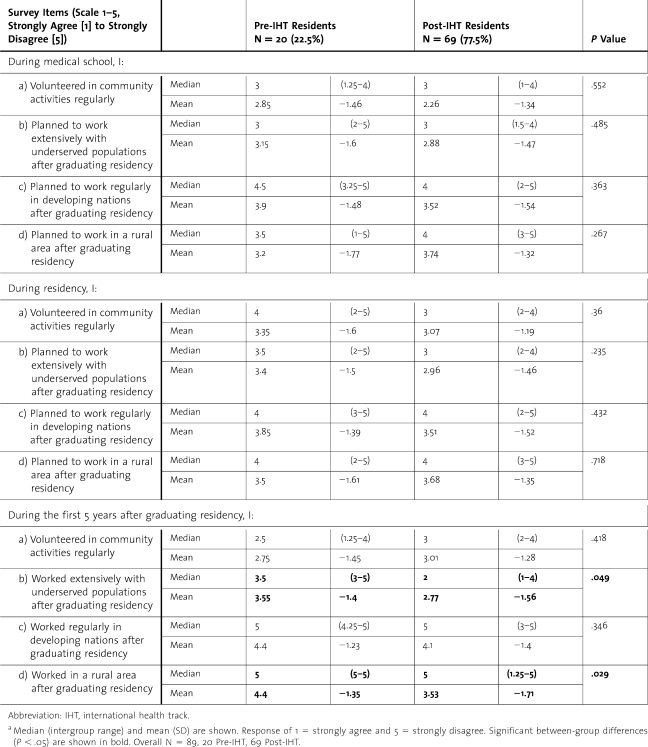
Pre-IHT Compared With Post-IHT
Compared with residents graduating prior to implementation of the IHT, post-IHT graduates were more likely to care for the underserved or practice in a rural area during their first 5 postgraduate years. There were no differences between the groups in interest or plans in these areas during medical school or residency (table 4) or with respect to practice abroad.
TABLE 4.
Medical Service Careers, Pre-IHT Versus Post-IHTa
Practice characteristics at the time of the survey (table 3) indicated that post-IHT graduates were more likely to provide care for the underserved than their pre-IHT counterparts and also were more likely to be practicing in health professional shortage areas or medically underserved areas. There was no difference in the presence of a sliding fee scale between any of the practices. The subpopulations of graduates practicing in FQHCs were insufficient to provide adequate power for analyses.
Post-IHT residents (45%) were more likely than pre-IHTs (16%) to offer volunteer community health care services (P < .0001). There were no differences in the proportion or extent of involvement in volunteer activities overall (table 3). Significantly more pre-IHTs pursued academic careers (25%, n = 5) than post-IHTs (10%, n = 7), P < .004, regardless of participation in the IHT.
Discussion
Recent health care reform has focused policymaker and academic attention on a looming shortage of physician supply. However, the debate has failed to address another persistent and central problem: a maldistribution of physician workforce geographically and across specialties. The solution to this problem is more complex than producing more physicians or even pairing increased production with financial incentives that encourage better distribution. One policy solution entails fostering or developing social responsibility in residents that might prompt them to practice in the areas of significant need.14 Family physicians are more likely than other providers to serve in health professional shortage areas,15 and this might be further encouraged as defensible as a social good. Our findings add to a literature suggesting that the presence of a residency-based IHT should be considered among these means.
Our findings show that graduates of a residency with an IHT were more likely to provide care for the underserved. The effect was not limited to participants in the IHT but also included nonparticipants. This suggests that the presence of an IHT, beyond providing specific didactic and practical opportunities, could influence the professional, educational, and philosophical culture within the residency. How this affects non-IHT residents is uncertain, and our findings should not infer that an IHT changes their orientation and alters their ultimate career destination. Identifying the components responsible for potential program-wide impact of an IHT track is an intriguing avenue for further inquiry.
There may be other explanations for the differences after the implementation of the IHT track. It is conceivable that the priorities and philosophy of applicants in the late 1980s and early 1990s differed from that of later applicants. We believe this is less likely, in light of the similarity of plans between the 2 groups during medical school and residency, followed by differences in practice after graduation (table 4) and level of volunteerism in their current practices (table 3). The presence of an IHT during residency was associated with an increased likelihood of providing service to underserved populations, regardless of the applicants' intentions prior to completion of residency.
Unexpectedly, though the IHT is associated with increased care of underserved populations, it was not associated with an increased likelihood of long-term service abroad (table 4). There was a difference between IHT participants and non-IHTs in service abroad (table 2), which may represent segregation of those with a global health interest into the IHT once it became available, rather than attracting a higher proportion of applicants with a global health interest. Although beneficial in promoting care of domestic underserved populations, this IHT did not appear to increase interest in foreign service. A common objection raised by critics of IHTs is that it is not appropriate to devote educational time and tax dollars to a program that benefits foreign populations rather than domestic constituencies. The evidence reported here suggests that this concern may be unfounded.
The finding that pre-IHT graduates were more likely to enter academic practice was not surprising. Most of those in academic family medicine gain practice experience prior to pursuing faculty positions16; a higher likelihood of an academic position would be expected of those whose graduation was remote than of graduates earlier in their career. Academic practice by itself is not defined as targeting the underserved, yet many academic primary care settings do provide care for these populations. It was interesting to note that in our survey data, 100% of the academic practices entered by IHT graduates were also FQHCs, while none of the academic practices among the pre-IHT group classified as FQHCs.
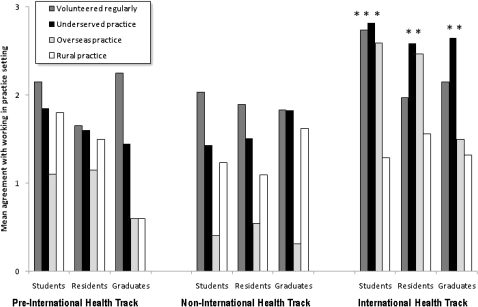
It is worth noting the trends from anticipated practice to actual practice (figure). Among pre-IHTs, interest in serving foreign, rural, or underserved populations diminished between training and practice, while interest in practicing in rural and underserved communities increased among the non-IHT graduates after IHT implementation. IHT graduates exhibited constant levels of interest in rural and underserved communities, though their interest in international involvement decreased. The decreased interest in caring for underserved populations among pre-IHT graduates occurred despite an essentially unchanged involvement in regular volunteer activities. This loss of idealism in the course of medical education, which has been documented previously,17–19 appeared to be inhibited—or perhaps even reversed—by the presence of the IHT.
FIGURE.
Anticipated Versus Actual Practice
A comparison between medical school, residency, and practice. Underserved, overseas, and rural denote (1) envisioned future practice settings while in medical school and residency and (2) actual practice settings after graduation. “Mean agreement with working in practice setting” is derived as the inverse of survey responses so that higher numbers indicate a higher intent or realization of intent to work in the practice setting. *P < .05 compared with non-IHT graduates.
Limitations of this study include the potential that persons interested in care for the underserved may have served these populations regardless of which residency they chose. Additionally, socially conscious individuals may select a residency with an IHT, regardless of personal participation in the track, because of perceived congruence of personal and program values. We investigated these possibilities by asking questions related to graduates' attitudes prior to residency, while in residency, and after graduation and found no differences in early anticipated career features yet there was significant difference in actual practice following completion of the residency once the IHT was in place. This should have reduced the impact of self-selection as an explanation for the differences.
Our study was subject to recall bias. The dependence on self-reporting introduced some degree of subjectivity into the data. This may have made it more likely for individuals with an interest in the IHT to complete the survey.
Although the survey instrument was drafted using a number of sources, its psychometric properties have not been externally validated. We consulted with experienced survey authors to attempt to make our instrument as usable and informative as possible.
International health training is incorporated into many medical school curricula and residencies.20–25 Medical student interest in international rotations is increasing. The percentage of graduating medical students who had participated in international rotations was 27.2% in 2006, up from 15.3% in 1989 and 6.2% in 1984.20 Although family medicine residency programs have seen a sharp decline in applications in recent years, interest in IHT at these residencies has increased,11 and the availability of IHT experiences has been successfully used in recruiting.
Despite this, few studies have assessed the effect of IHTs or international student electives,26-27 and there are few reports that objectively qualify or quantify the outcomes of these programs. Although previous studies in internal medicine focused primarily upon attitudes and knowledge rather than practice outcomes,12,13 they offered some indirect evidence that participants in these electives were more likely to enter practices that care for the underserved. 13
Conclusions
We report here the first investigation to specifically quantify the effects of an IHT curriculum on ultimate practice outcomes. Our educational intervention was associated with a shift in primary care physician workforce toward underserved populations. This shift appeared to be independent of their original orientations. At a time when there are growing numbers of patients who cannot access the health care system, and a shortage of physicians willing to serve those patients, any interventions that increases the likelihood of medical providers entering a career of caring for these populations is valuable. More widespread implementation of IHT in residency training, with the goal of increasing the health care workforce among the underserved, may be warranted. Further investigations of the components of IHT responsible for the associations reported in our study and the transferability of our findings to other programs are indicated.
Footnotes
Andrew W. Bazemore, MD, MPH, is an Assistant Director at the Robert Graham Center, American Academy of Family Physicians; Linda M. Goldenhar, PhD, is a Research Professor of Pediatrics at the University of Cincinnati College of Medicine Christopher J. Lindsell, PhD, is an Associate Professor at the University of Cincinnati College of Medicine, Department of Emergency Medicine; Philip M. Diller, MD, PhD, is a Professor and Interim Chair at University of Cincinnati College of Medicine, Department of Family Medicine; and Mark K. Huntington, MD, PhD, is the Assistant Director of the Sioux Falls Family Medicine Residency Program and an Associate Professor of Family Medicine at the Sanford School of Medicine of the University of South Dakota.
Funding: The study did not receive any external funding.
References
- 1.Turner GM, Perisco T. Massachusetts Healthcare Reform. Available at: http://www.galen.org/fileuploads/MAHealthReform.pdf. Accessed April 10, 2011. [Google Scholar]
- 2.Green LA, Dodoo MS, Ruddy G, et al. The physician workforce in the United States: a family medicine perspective. Available at: http://www.graham-center.org/online/graham/home/publications/monographs-books/2004/rgcmo-physician-workforce1.html. Accessed April 8, 2011. [Google Scholar]
- 3.Phillips RL, Dodoo MS, McCann JL, et al. Report to the task force on the care of children by family physicians. Available at: http://www.graham-center.org/online/graham/home/publications/monographs-books/2005/rgcmo-care-children0.html. Accessed April 8, 2011. [Google Scholar]
- 4.Grobler L, Marais BJ, Mabunda SA, Marindi PN, Reuter H, Volmink J. Interventions for increasing the proportion of health professionals practicing in rural and other underserved areas. Cochrane Database Syst Rev. 2009(1):CD005314. doi: 10.1002/14651858.CD005314.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Ricketts TC, Hart LG, Pirani M. How many rural doctors do we have. J Rural Health. 2000;16(3):198–207. doi: 10.1111/j.1748-0361.2000.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 6.Phillips RL, Dodoo MS, Petterson S, et al. What influences medical student and residency choices? Report from the Robert Graham Center and Josiah Macy Foundation. Available at: http://www.aafp.org/online/etc/medialib/aafp_org/documents/press/2011-match-media-kit/what-influences-medical-student-and-resident-choices.Par.0001.File.tmp/Wh-Influence-Stu-Choice-Rpt.pdf;jsessionid=782caaa1-3ec1-f141-819d-9b0729c3ee38. Accessed April 8, 2011. [Google Scholar]
- 7.Rosenblatt RA, Andrilla CH. A, Curtin T, Hart LG. Shortages of medical personnel at community health centers: implications for planned expansion. JAMA. 2006;295(9):1042–1049. doi: 10.1001/jama.295.9.1042. [DOI] [PubMed] [Google Scholar]
- 8.National Association of Community Health Centers, Robert Graham Center. Access denied: a look at America's medically disenfranchised. Available at: http://www.graham-center.org/online/graham/home/publications/monographs-books/2007/rgcmo-access-denied.html. Accessed April 8, 2011. [Google Scholar]
- 9.National Association of Community Health Centers, Robert Graham Center. Access transformed: building a primary care workforce for the 21st century. Available at: http://www.graham-center.org/online/graham/home/publications/monographs-books/2008/rgcmo-access-transformed.html. Accessed April 8, 2011. [Google Scholar]
- 10.Council on Graduate Medical Education. Physician Workforce Policy Guidelines for the United States, 2000-2020. Available at: http://www.cogme.gov/16.pdf. Accessed March 31, 2011. [Google Scholar]
- 11.Bazemore AW, Henein M, Goldenhar LM, Szaflarski M, Lindsell CJ, Diller P. The effect of offering international health training opportunities on family medicine residency recruiting. Fam Med. 2007;39(4):255–260. [PubMed] [Google Scholar]
- 12.Miller WC, Corey GR, Lallinger GJ, Durack DT. International health and internal medicine residency training: the Duke University experience. Am J Med. 1995;99(3):291–297. doi: 10.1016/s0002-9343(99)80162-4. [DOI] [PubMed] [Google Scholar]
- 13.Gupta AR, Wells CK, Horwitz RI, Bia FJ, Barry M. The international health program: the fifteen-year experience with Yale University's internal medicine residency program. Am J Trop Med Hyg. 1999;61(6):1019–1023. doi: 10.4269/ajtmh.1999.61.1019. [DOI] [PubMed] [Google Scholar]
- 14.Goodman DC. The physician workforce crisis: where is the evidence. Health Aff. 2005;W5:108–110. doi: 10.1377/hlthaff.w5.108. [DOI] [PubMed] [Google Scholar]
- 15.Grumbach K, Hart LG, Mertz E, Coffman J, Palazzo L. Who is caring for the underserved?: a comparison of primary care physicians and nonphysician clinicians in California and Washington. Ann Fam Med. 2003;1(2):97–104. doi: 10.1370/afm.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huntington M. A majority of residency faculty have practice experience prior to entering academia. Fam Med. 2010;42(1):6–7. [PubMed] [Google Scholar]
- 17.Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: a cohort study. Med Educ. 2004;38(5):522–534. doi: 10.1046/j.1365-2929.2004.01820.x. [DOI] [PubMed] [Google Scholar]
- 18.Crandall SJ, Reboussin BA, Michielutte R, Anthony JE, Naughton MJ. Medical students' attitudes toward underserved patients: a longitudinal comparison of problem-based and traditional medical curricula. Adv Health Sci Educ Theory Pract. 2007;12(1):71–86. doi: 10.1007/s10459-005-2297-1. [DOI] [PubMed] [Google Scholar]
- 19.Crandall SJ, Davis SW, Broeseker AE, Hildebrandt C. A longitudinal comparison of pharmacy and medical students' attitudes toward the medically underserved. Am J Pharm Educ. 2008;72(6):148. doi: 10.5688/aj7206148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Association of American Medical Colleges (AAMC) Medical Student Graduate Questionnaire. Washington DC: AAMC; 2003. [Google Scholar]
- 21.Nelson BD, Lee AC, Newby PK, Chamberlin MR, Huang CC. Global health training in pediatric residency programs. Pediatrics. 2008;122(1):28–33. doi: 10.1542/peds.2007-2178. [DOI] [PubMed] [Google Scholar]
- 22.Powell AC, Mueller C, Kingham P, Berman R, Pachter HL, Hopkins MA. International experience, electives, and volunteerism in surgical training: a survey of resident interest. J Am Coll Surg. 2007;205(1):162–168. doi: 10.1016/j.jamcollsurg.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 23.Dey CC, Grabowski JG, Gebreyes K, Hsu E, VanRooyen MJ. Influence of international emergency medicine opportunities on residency program selection. Acad Emerg Med. 2002;9(7):679–683. doi: 10.1111/j.1553-2712.2002.tb02145.x. [DOI] [PubMed] [Google Scholar]
- 24.Jense RJ, Howe CR, Bransford RJ, Wagner TA, Dunbar PJ. University of Washington orthopedic resident experience and interest in developing an international humanitarian rotation. Am J Orthop. 2009;38(1):E18–E20. [PubMed] [Google Scholar]
- 25.Powell AC, Casey K, Liewehr DJ, Hayanga A, James TA, Cherr GS. Results of a national survey of surgical resident interest in international experience, electives, and volunteerism. J Am Coll Surg. 2009;208(2):304–312. doi: 10.1016/j.jamcollsurg.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 26.Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: current status, needs, and opportunities. Acad Med. 2009;84(3):320–325. doi: 10.1097/ACM.0b013e3181970a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thompson MJ, Huntington MK, Hunt DD, Pinsky LE, Brodie JJ. Educational effects of international health electives on U.S. and Canadian medical students and residents: a literature review. Acad Med. 2003;78(3):342–347. doi: 10.1097/00001888-200303000-00023. [DOI] [PubMed] [Google Scholar]