Abstract
Background
Recent focus on resident work hours has challenged residency programs to modify their curricula to meet established duty hour restrictions and fulfill their mission to develop the next generation of clinicians. Simultaneously, health care systems strive to deliver efficient, high-quality care to patients and families. The primary goal of this observational study was to use a data-driven approach to eliminate examples of waste and variation identified in resident rounding using Lean Six Sigma methodology. A secondary goal was to improve the efficiency of the rounding process, as measured by the reduction in nonvalue-added time.
Methods
We used the “DMAIC” methodology: define, measure, analyze, improve, and control. Pediatric and family medicine residents rotating on the pediatric hospitalist team participated in the observation phase. Residents, nurses, hospitalists, and parents of patients completed surveys to gauge their attitudes toward rounds. The Mann-Whitney test was used to test for differences in the median times measured during the preimprovement and postimprovement phases, and the Student t test was used for comparison of survey data.
Results and Discussion
Collaborative, family-centered rounding with elimination of the “prerounding” process, as well as standard work instructions and pacing the process to meet customer demand (takt time), were implemented. Nonvalue-added time per patient was reduced by 64% (P = .005). Survey data suggested that team members preferred the collaborative, family-centered approach to the traditional model of rounding.
Conclusions
Lean Six Sigma provides tools, a philosophy, and a structured, data-driven approach to address a problem. In our case this facilitated an effort to adhere to duty hour restrictions while promoting education and quality care. Such approaches will become increasingly useful as health care delivery and education continue to transform.
Editor's Note: The online version of this article contains the 4 surveys used in this study (Resident Survey (101KB, ppt) , Attending Survey (100.5KB, ppt) , Nursing Survey (101KB, ppt) , Patient Family Survey (102KB, ppt) ).
Background
Recent focus on resident work hours has challenged residency programs across the nation to make modifications to meet established duty hour limits and fulfill their mission to develop the next generation of physicians.1–4 To date there have been few published articles about programs that have used a systematic, data-driven approach to guide the changes they have made. Such a standardized approach to quality improvement will become increasingly vital, particularly with additional duty hour standards set to take effect in 2011 and the emphasis on health care reform at the national level.
Over the last decade, health care institutions have borrowed performance improvement tools from manufacturing, including Lean,5 emphasized by Toyota, as well as Six Sigma, with its early roots at Motorola.6 The objective of Lean is to eliminate waste to maximize value to the customer. Waste is defined as activity that does not bring value to the customer; in simple terms, activity for which the customer (eg, patient, medical educator, resident) would not be willing to pay because it does not contribute meaningfully to the product or service requested. The goal of Six Sigma is to reduce variation within processes to produce a product that is closer to the customer's specification; the term refers to a process performed with an error rate of 3.4 errors per 1 million opportunities. Many hospitals have embraced these concepts to reduce cost, increase access to care, and increase capacity without any, or minimal, capital expenditures.7,8 This type of rigorous approach has not yet been used to improve graduate medical education.
The primary goal of this study was to use a data-driven approach to eliminate examples of waste and variation identified in the resident rounding process, using Lean Six Sigma. A secondary goal was to improve the efficiency of the rounding process, measured by a reduction in nonvalue-added time. Since prerounds, rounds, and the writing of orders and daily notes occur from 7:00 am until 12:00 pm, or approximately 50% of a resident's day at Akron Children's Hospital during inpatient rotations, successfully targeting this time period will provide the program with more time for educational offerings within the duty hour limits and enhance educational value for its residents.
Methods
Participants
Pediatric and family medicine residents were observed during the rounding process. Pediatric residents, nurses, hospitalists, and parents responded to the surveys.
Study Design
The study examined the weekday time period from 7:00 am until 12:00 pm, focusing on pediatric and family medicine residents on the hospitalist team at Akron Children's Hospital from October 2008 through June 2009. Akron Children's Hospital is a free-standing children's hospital with 9500 inpatient admissions annually and is a major teaching affiliate of the Northeastern Ohio Universities Colleges of Medicine and Pharmacy. Its pediatric residency comprised 47 residents and 3 chief residents. The ward-based hospitalist team included 2 senior residents, 4 to 6 interns, and 2 to 3 hospitalists serving as attending physicians. The team managed the care of general pediatric patients. Teams covered between 15 and 55 patients, depending on the time of year. The study proposal was submitted to the Institutional Review Board of Akron Children's Hospital and was determined to be exempt from Institutional Review Board oversight.
The typical day began with sign-out at 7:00 am, followed by prerounds when residents and medical students obtained data, examined patients, and wrote notes and preliminary orders. Attending physicians completed similar activities during the same time period. Residents and students also attended a morning conference from 8:30 to 9:00, except on Fridays when Grand Rounds was scheduled from 8:00 to 9:00. The first formal sit-down rounding time occurred from 10:15 to 10:30, when the condition of patients from 2 of the units that comprised a smaller portion of the hospitalist service was discussed. Formal lectures occurred on Tuesdays through Thursdays from 10:30 to 11:15, followed by a second session of formal rounds from 11:15 to 11:45, during which the remainder of the patients were discussed. Residents finished their notes and orders before conference or clinic at noon.
The “DMAIC” methodology of Lean Six Sigma, comprising 5 separate phases, was used as the improvement strategy: define, measure, analyze, improve, and control.
Define
The problem and scope were defined, the goal was determined, and the team was formed. A multidisciplinary team was formed, made up of attending physicians, pediatric residents, nurses, administrators, and a Parent Advisory Council (PAC) representative. These individuals were identified as “stakeholders” of the rounding process. We included a representative from the PAC to capture the viewpoint of patients and families, the “customer.” The PAC comprises parent volunteers who use Akron Children's Hospital and are interested in the continued growth and development of comprehensive family-centered pediatric services.
Measure
We used direct observation to study resident behavior during the rounding process. The amount of time spent in each activity (eg, “walked from nurses' station to room 7204,” “looked up labs”) was recorded. Observations were conducted by members of the Center for Operations Excellence, individuals with formal training and experience in Lean Six Sigma, and 2 trained volunteers who documented their findings in a spreadsheet using Microsoft Excel (Redmond, WA). Residents, patients, and families were aware of the role of the observers and the study purpose. The identities of all patients and observed residents were protected.
Analyze
Collected data were used to construct a value stream map (VSM). A VSM outlines all the major steps that occur during the rounding process, along with an estimate of the average time that each step takes. Each activity was categorized into 1 of 15 major steps: sign-out, data collection, family interaction, physical examination, note writing, education, formal rounds, walking, waiting, order entry, physician interaction, nursing interaction, contacting consults, personal time, and other. The VSM entailed assigning “value” to each activity or process. In keeping with the hospital mission, value was determined from the perspective of the patient. An activity or process can be classified as “value-add,” “nonvalue-add,” or “necessary nonvalue-add.” A nonvalue-add(ed) activity or process was defined as one that does not directly contribute to the diagnosis, therapy, or discharge of the patient. The final category refers to activities that do not add value from the patient's point of view but are necessary for hospital operations (eg, billing, Joint Commission requirements). The finalized VSM allowed the team to examine the rounding process for waste and for the aspects of an activity that did not add value. Waste was categorized into 7 types: defects, overproduction, motion, overprocessing, waiting, inventory, and transportation.
Improve
The VSM and waste analysis were used to generate potential solutions. Solutions were developed on the basis of 3 major lean principles: smooth, continuous one-piece flow in which batching is eliminated; elimination of all forms of waste to the extent possible; and the implementation of standardized work.5 One-piece flow is the ultimate goal of lean production, in which 1 unit is processed at a time, resulting in such benefits as the elimination of waste, balance of workload, and built-in quality. Standardized work supports this goal by providing clearly outlined instructions on how to complete a task, promoting predictability, regular timing, and regular output.
Subsequently, potential solutions were prioritized by size of impact and feasibility of implementation. Prioritized solutions were then piloted, results were measured, and a process of continual evaluation and refinement was begun.
Control
Measures were designed to sustain improvements realized during the previous phase. This included the assignment of roles and responsibilities, frequency of audits, and a plan of action if the measure did not meet target specifications.
Surveys
A written survey was used as part of a qualitative analysis to gauge the attitudes of stakeholders toward the rounding process, with regard to education, communication, and efficiency. Before improvements were made, all residents, hospitalists, and nurses on the general care wards were surveyed; a small sample of parents of hospitalized children was surveyed over a 3-day period. After improvements were made, only those stakeholders who experienced the new process were eligible to complete the same survey. Surveys included 6 to 13 statements, and respondents were asked to choose a number that best described their opinion with regard to each statement (1, strongly disagree; 2, disagree; 3, neutral; 4, agree; 5, strongly agree).
Measures
The main quantitative outcome measure was the nonvalue-add time per patient during the resident rounding process. Only time that could be attributed to specific patients was analyzed; activities such as formal education and personal time were excluded. In addition, the total rounding time per patient and the value-add time per patient were secondary outcomes. Survey responses before and after interventions were also recorded.
Statistical Analysis
All statistical analysis was performed with Minitab, version 15 (State College, PA). The Mann-Whitney test was used to test for significant differences in the median times measured during the preimprovement and postimprovement phases, as the data were not normally distributed. The Student t test was used for comparison of survey data.
Results
Preimprovement Phase and Waste Analysis
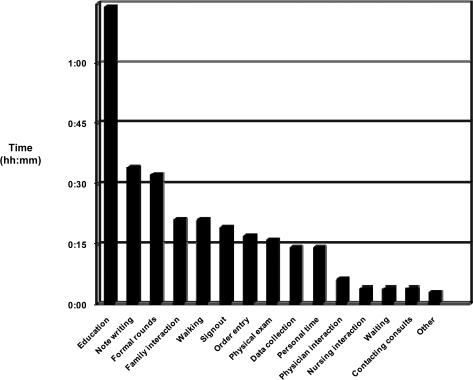
Most of the time was spent in formal educational activities, note writing, and formal sit-down rounds (figure 1). Residents spent on average the same amount of time walking as they did interacting with families, and even less time performing physical examinations and discussing plans with the nursing staff. In fact, residents walked approximately one-half mile, completing their tasks each morning. From the patient's point of view, only 17% of a resident's time could be classified as value-add (data not shown). Most of the waste could be classified as inventory, in the form of information that was available to use but not acted upon until later, and overprocessing, in which unnecessary steps were taken to complete a task. Examples included formal lectures during morning rounds (inventory); waiting until formal rounds to discuss the plans of care (inventory); discussing the plan of care with the medical team and then again with the nurses and families (overprocessing); and multiple notes written for the same patient (overproduction).
FIGURE 1.
Average Time (hours∶minutes) Spent During Each Step in the Preimprovement Phase
Data were collected from 5 rounding sessions covering a total of 88 patients, including 23 primary patients covered by the observed residents.
Interventions
Potential solutions were then generated to address the examples of waste uncovered during analysis of the VSM. The main intervention entailed implementing “family-centered rounds,” in which the residents, attending physician, nurses, and families discussed the patient at the bedside. The team developed this solution because it best allowed the team to eliminate many of the examples of waste and address the disproportionate use of time in activities that did not add value to the patient or residents (figure 1). The traditional “prerounding” process, in which the residents and attending physicians separately gathered data and examined patients before formal rounds, was eliminated. The physical examination and data analysis took place at the bedside, conducted by the senior resident, primary intern or student, and attending physician. Standard work instructions were used to guide the format of bedside rounds. Standard work instructions allow for the same information to be conveyed for every patient in the same order. The other residents had specific responsibilities, such as order or note writing. The senior resident was responsible for leading the encounter, with additional input from the attending physician as needed. Medical students presented their primary patients as well, much like an intern would. Education directly relevant to the care of the patient was integrated into the process, allowing for patients, families, and nurses to participate. “Takt” time, the pace of a process needed to meet customer demand, was calculated to provide an estimate of the amount of time that should be spent with each patient. The time was calculated on the basis of the target length of time available, total number of patients, complexity of the patient's condition, and whether the patient was new or established. This also allowed the team to provide the nurses and families with a specific time frame for rounds to occur, which allowed them to plan their schedules to be present for rounds. A single collaborative note was written in the chart. All orders were written and questions answered before moving on to the next patient.
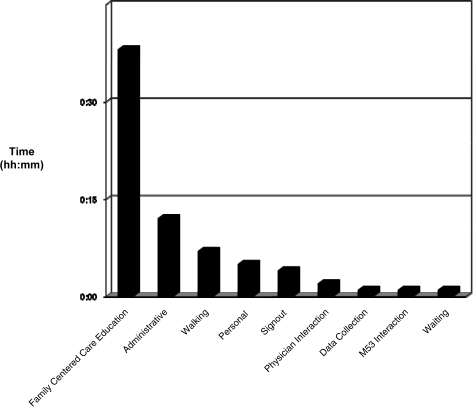
Postimprovement Phase
During the postimprovement phase, family-centered care and integrated education comprised most of the residents' time (figure 2). During this step, data collection, physical examination, family interaction, development of a plan, nursing interaction, and education took place at the bedside. Note writing and order entry were subsequently combined into an “administrative” step, which comprised the next largest portion of time. Approximately 55% of resident time could be classified as value-add (data not shown). By moving as a team from room to room in sequential order, the time spent walking was also reduced.
FIGURE 2.
Average Time (hours∶minutes) Spent During Each Step in the Postimprovement Phase
Data were collected from 5 rounding sessions covering a total of 86 patients, including family-centered rounds on 8 primary patients covered by the observed residents.
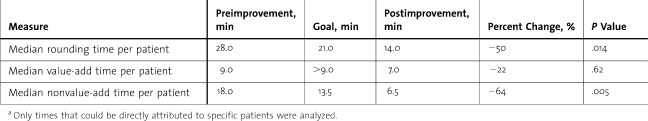
Analysis of Outcome Measures
The median nonvalue-add time per patient served as the main outcome measure. During the postimprovement phase, the median time per patient was significantly reduced from 18.0 minutes to 6.5 minutes, a 64% reduction (table). Similarly, the median total rounding time per patient was significantly decreased from 28.0 minutes to 14.0 minutes, a 50% reduction. The median value-add time also decreased by 22% from 9.0 minutes to 7.0 minutes, but the change was not significant. As can be seen in the I-chart, the intervention resulted in a process with a lower average time, with less variation around that time (figure 3).
TABLE.
Difference in Times Between the Preimprovement and Postimprovement Phasesa
FIGURE 3.
Individuals-chart (I-chart) for Nonvalue-Add Time
The chart demonstrates that the process has been controlled with a shorter mean time (hours∶minutes) and less variation around the mean, reflecting stability. UCL, upper control limit, reflects the 25% reduction goal; x̄, mean time; LB, lower bounds, set at 0.
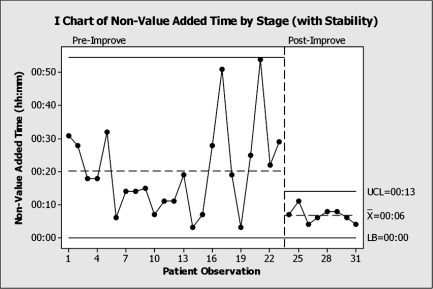
Assessment of Survey Results
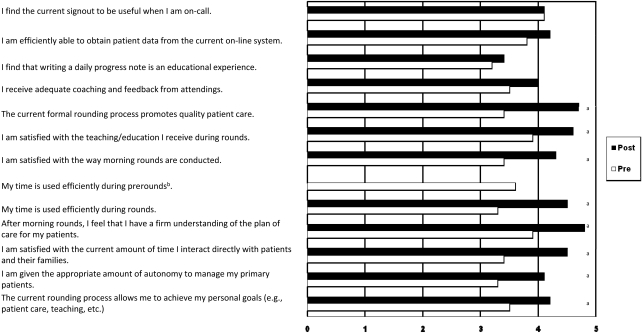
Survey response rates were as follows: residents, 37 of 50 (74%) in preimprovement group and 11 of 11 (100%) in postimprovement group; attending physicians, 5 of 5 (100%) in preimprovement group and 2 of 2 (100%) in postimprovement group; nurses, 48 of 195 (25%) in preimprovement group and 6 of 9 (67%) in postimprovement group; parents, 33 of 100 (33%) responded preimprovement and 15 of 15 (100%), postimprovement. Residents preferred the family-centered approach over the current method (figure 4). The residents in the postimprovement group felt that the family-centered approach better promoted efficiency, education, and quality patient care. Attending physicians and nurses also preferred the family-centered approach, while there was no statistical difference in parental responses (data not shown).
FIGURE 4.
Survey of Resident Attitudes Toward the Rounding Process
The survey demonstrated a preference for the family-centered care model, with N = 37 (74%) preimprovement and N = 11 (100%) postimprovement. 1, strongly disagree; 2, disagree; 3, neutral or no opinion; 4, agree; 5, strongly agree.
a Indicates statistical significance at P < .05.
b There is no prerounding step in the family-centered care model.
Discussion
Lean Six Sigma provides a set of tools and a philosophy allowing one to use a structured, data-driven approach to address a problem, in this case facilitating a residency program's attempt to adhere to duty hour restrictions while promoting education and quality care. While several institutions have reported a positive impact on residents, as well as patients and families, the use of the DMAIC approach to understand the benefits of family-centered care quantitatively and qualitatively has not been previously reported.9–14 Our preliminary study demonstrated that this methodology could be successfully applied to the educational setting.
The amount of nonvalue-add time was significantly reduced. With the amount of time available for resident education gradually decreasing, it is imperative that residency programs maximize the value of time spent in the hospital and increase the amount of time spent directly with patients and their attending physicians. Resident survey results supported the hypothesis that family-centered care would foster better learning opportunities, patient interaction, and communication. Residents appreciated the opportunity to make decisions in real time, rather than waiting to see if their plan of care matched that of the attending physician several hours later in formal rounds, and benefited from additional face-to-face time with attending physicians, guidance that may not be available at night when they were on-call, for example.
The amount of value-add time also decreased, but not significantly. As all face-to-face time with patients or families was classified as value-add, the team hypothesized that the decrease resulted from improved flow of information during the patient interaction, as well as a decreased need for residents to go back to the patient room to clarify information discussed during sit-down rounds. The survey of parents did not show a significant improvement, most likely for 2 reasons. First, scores before the intervention were high, making it difficult to demonstrate significant improvement. Second, the survey itself may not have been adequately designed to detect differences before and after the intervention.
Several challenges were uncovered during the course of the study. First, the collection of observational data is both labor-intensive and time-consuming. Second, the new approach required a significant culture change, as is common for Lean Six Sigma projects. Residents and medical students needed to become comfortable presenting at the bedside and having their thought process probed in front of parents. Likewise, attending physicians needed to facilitate resident autonomy during the bedside interaction, sometimes needing to take a step back to allow residents to arrive at their own conclusions. It also required that all stakeholders make changes to their rounding routines. Such behavior changes take time.
One limitation of the study is the number of observations and survey responses. A key teaching of Lean Six Sigma is to make small changes, measure again, and then continually improve the process. Data collection is important but should not hinder the process of continuous improvement. The project team felt that the information conveyed a trend that appeared to accurately reflect the current state, and significant differences were seen in key outcome measures. There were fewer survey responses after the intervention because only those stakeholders who took part in the pilot phase were eligible; nevertheless, the trends and comments suggested no negative impact from the changes.
The initial portion of the project has been limited to the hospitalist service. It is anticipated that future work will examine how successful interventions can be generalized to subspecialty and surgical services as well. Many of the data-driven solutions addressed in this study would need to be individually tailored to meet the needs of other training programs. At the same time, a key tenet of Lean Six Sigma is the use of standardized work: clearly outlined instructions that detail the steps to be used each and every time a process is completed. This makes it easy to transfer solutions across departments and even institutions.
It would be informative to include objective measures of quality (eg, length of stay, number of adverse events) and education (eg, board scores, pretest and posttest scores) in a future longitudinal study. Nevertheless, it is reasonable to infer that eliminating nonvalue-add activities, increasing the time residents spend face-to-face with patients and attending physicians, and reducing the number of separate occurrences that information must be transferred from individual to individual will facilitate quality care and medical education.
Conclusions
As a data-driven approach, quite similar to the scientific method, Lean Six Sigma serves as a useful tool for addressing the problems encountered not only in graduate medical education but also in health care in general. While the tools and methods are easy to learn, the willingness to change and the culture of continuous improvement that needs to be embraced can be difficult to instill. As health care and the education of its providers continue to transform, the ability to continuously improve and a proven method by which to do so will become essential for organizations to survive and flourish.
Footnotes
David V Chand, MD is a Deployment Director at the Center for Operations Excellence, Akron Children's Hospital.
Funding/support: The study was supported by the Center for Operations Excellence at Akron Children's Hospital. No additional external funding/support was received.
Previous presentation: The content of this manuscript was presented in poster format at the Institute for Healthcare Improvement's 21st Annual National Forum on Quality Improvement in Health Care, December 2009.
Acknowledgments and additional contributions: The author would like to thank the following persons at Akron Children's Hospital: Mark Watson, President, Akron Children's Regional Network, and Walt Schwoeble, Vice President, Human Resources, for their executive-level support of the project and manuscript review; Anne Musitano, PharmD, MBOE, Center for Operations Excellence, for observational data collection as well as critical evaluation of the project and manuscript; Samuel Scott, BS, and Lyndsey Planicka, BA, for assisting with observational data collection; Michael Antochow, BS, Center for Operations Excellence, for assistance with statistical analysis and critical evaluation of the project and manuscript; Doug Dulin, LM, MBB, Trauda Gilbert, BS, MBOE, Heidi Kline, BA, Sherry Valentine, RN, BSN, MBA, and Chris Weisbrod, MBA, from the Center for Operations Excellence, for critical evaluation of the project and the manuscript; Michael Reed, PharmD, Director of The Rebecca D. Considine Clinical Research Institute and the Clinical Pharmacology and Toxicology Division, and Norman Christopher, MD, Noah Miller Chair of Pediatrics, for critical evaluation of the manuscript. The author would also like to thank Laura Winner, BSN, MBA, Lean Sigma Deployment Leader, Johns Hopkins Medicine, for her mentorship and critical evaluation of the project.
References
- 1.Institute of Medicine. Resident duty hours: enhancing sleep, supervision and safety. N Engl J Med. 2008;359:2633–2635. [Google Scholar]
- 2.Ogden PE, Sibbitt S, Howell M, et al. Complying with ACGME resident duty hour restrictions: restructuring the 80-hour workweek to enhance education and patient safety at Texas A&M/Scott & White Memorial Hospital. Acad Med. 2006;81(12):1026–1031. doi: 10.1097/01.ACM.0000246688.93566.28. [DOI] [PubMed] [Google Scholar]
- 3.Fields RC, Bowman MC, Freeman BD, Klingensmith ME. Implementation of an “after hours” resident educational program in general surgery residency: a paradigm for increasing formal didactic training outside of the hospital setting in the era of the 80-hour workweek. J Surg Educ. 2009;66(6):340–343. doi: 10.1016/j.jsurg.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 4.Schneider JR, Coyle JJ, Ryan ER, Bell RH, Jr, DaRosa DA. Implementation and evaluation of a new surgical residency model. J Am Coll Surg. 2007;205(3):393–404. doi: 10.1016/j.jamcollsurg.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Liker, Jeffrey K. The Toyota Way. New York, NY: McGraw-Hill; 2004. [Google Scholar]
- 6.The history of Six Sigma. iSixSigma website. Available at: http://www.isixsigma.com/index.php?option=com_k2&view=item&id=1505&Itemid=1&Itemid=1. Accessed April 23, 2010. [Google Scholar]
- 7.Child Health Corporation of America. Lean healthcare: a journey, not a destination, part I. CHCA Executive Institute Special Report. September 2007 [Google Scholar]
- 8.Child Health Corporation of America. Lean healthcare: building patient-centered systems, part II. CHCA Executive Institute Special Report. November 2007 [Google Scholar]
- 9.McMahon GT, Katz JT, Thorndike ME, Levy BD, Loscalzo J. Evaluation of a redesign initiative in an internal-medicine residency. N Engl J Med. 2010;362(14):1304–1311. doi: 10.1056/NEJMsa0908136. [DOI] [PubMed] [Google Scholar]
- 10.Rappaport DI, Cellucci MF, Leffler MG. Implementing family-centered rounds: pediatric residents' perceptions. Clin Pediatr (Phila) 2010;49(3):228–234. doi: 10.1177/0009922809346568. [DOI] [PubMed] [Google Scholar]
- 11.Knoderer HM. Inclusion of parents in pediatric subspecialty team rounds: attitudes of the family and medical team. Acad Med. 200984(11):1576–1581. doi: 10.1097/ACM.0b013e3181bb2bed. [DOI] [PubMed] [Google Scholar]
- 12.Aronson PL, Yau J, Helfaer MA, Morrison W. Impact of family presence during pediatric intensive care unit rounds on the family and medical team. Pediatrics. 2009;124(4):1119–1125. doi: 10.1542/peds.2009-0369. [DOI] [PubMed] [Google Scholar]
- 13.Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292–297. doi: 10.1097/ACM.0b013e3181637e21. [DOI] [PubMed] [Google Scholar]
- 14.O'Mahony S, Mazur E, Charney P, Wang Y, Fine J. Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22(8):1073–1079. doi: 10.1007/s11606-007-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]