Cigarette smoking is the single biggest avoidable cause of death and disability in developed countries. Smoking is now increasing rapidly throughout the developing world and is one of the biggest threats to current and future world health. For most smokers, quitting smoking is the single most important thing they can do to improve their health. Encouraging smoking cessation is one of the most effective and cost effective things that doctors and other health professionals can do to improve health and prolong their patients' lives. This series will explore the reasons why smokers smoke, how to help them to quit, and how to reduce the prevalence of smoking more generally.
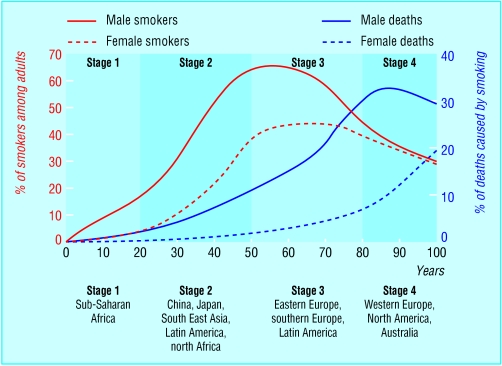
Figure 1.
Stages of worldwide tobacco epidemic. Adapted from Lopez et al. A descriptive model of the cigarette epidemic in developed countries. Tobacco Control 1994;3: 242-7
Who smokes tobacco?
Cigarette smoking first became a mass phenomenon in the United Kingdom and other more affluent countries in the early 20th century after the introduction of cheap, mass produced, manufactured cigarettes. Typically, a “smoking epidemic” in a population develops in four stages: a rise and then decline in smoking prevalence, followed two to three decades later by a similar trend in smoking related diseases. Usually, the uptake and consequent adverse effects of smoking occur earlier and to a greater degree among men.
In the United Kingdom there are about 13 million smokers, and worldwide an estimated 1.2 billion. Half of these smokers will die prematurely of a disease caused by their smoking, losing an average of eight years of life; this currently represents four million smokers each year worldwide. Deaths from smoking are projected to increase to more than 10 million a year by 2030, by which time 70% of deaths will be in developing countries.
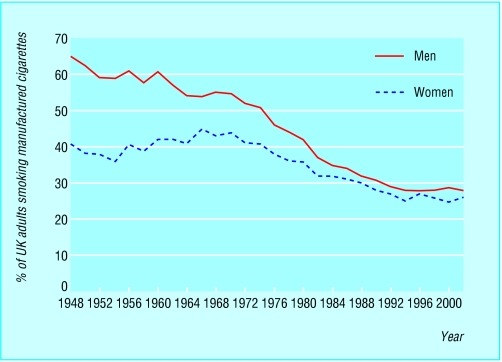
Figure 2.
Prevalence of smoking of manufactured cigarettes in Great Britain. Data from Tobacco Advisory Council (1948-70) and general household survey (1972-2001)
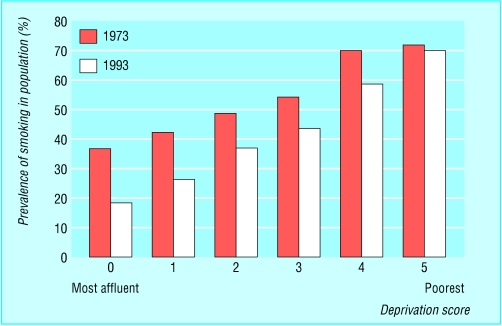
The prevalence of smoking among adults in the United Kingdom has declined steadily from peaks in the 1940s in men and the late 1960s in women. However, this reduction in overall prevalence during stage 4 of the epidemic disguises relatively static levels of smoking among socioeconomically disadvantaged groups, making smoking one of the most important determinants of social inequalities in health in the developed world. Smoking has also declined much more slowly among young adults in the United Kingdom. The decline in smoking in the United Kingdom and some other developed countries may now be coming to an end. For example, since 1994 the prevalence of smoking in UK adults has remained at about 28%.
Whereas countries in western Europe, Australasia, and the United States may be in stage 4 of the smoking epidemic, in many developing countries the epidemic is just beginning. Smoking in low and middle income countries is increasing rapidly—for example, the prevalence of smoking among males in populous Asian countries is now far higher than in Western countries—45% in India, 53% in Japan, 63% in China, 69% in Indonesia, and 73% in Vietnam.
Figure 3.
Cigarette smoking by deprivation level in Great Britain. Data from general household survey
Adverse health effects
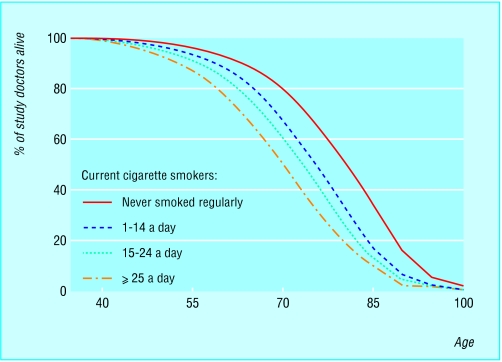
The adverse health effects of smoking are extensive, and have been exhaustively documented. There is a strong dose-response relation with heavy smoking, duration of smoking, and early uptake associated with higher risks of smoking related disease and mortality. Data from 40 years of follow up of smokers in a prospective cohort study of male British doctors show the impact of smoking on longevity at different levels of exposure. The strongest cause-specific associations are with respiratory cancers and chronic obstructive pulmonary disease; in numeric terms, the greatest health impacts of smoking are on respiratory and cardiovascular diseases.
Some of the increases in health risk associated with smoking are greater among younger smokers. The risk of heart attack among smokers, for example, is at least double over the age of 60 years, but those aged under 50 have a more than fivefold increase in risk. Smokers are also at greater risk of many other non-fatal diseases, including osteoporosis, periodontal disease, impotence, male infertility, and cataracts. Smoking in pregnancy is associated with increased rates of fetal and perinatal death and reduced birth weight for gestational age. Passive smoking after birth is associated with cot death and respiratory disease in childhood and lung cancer, heart disease, and stroke in adults.
Figure 4.
Survival by smoking status, according to study of male British doctors (follow up after 40 years, 1951-91). Adapted from Doll et al (see Further Reading box)
The effect on health services is considerable—for example, an estimated 364 000 admissions and £1.5bn ($2.4bn; €2.1bn) a year in health service costs are attributable to smoking in the United Kingdom alone.
Health benefits of smoking cessation
Stopping smoking has substantial immediate and long term health benefits for smokers of all ages. The excess risk of death from smoking falls soon after cessation and continues to do so for at least 10-15 years. Former smokers live longer than continuing smokers, no matter what age they stop smoking, though the impact of quitting on mortality is greatest at younger ages. For smokers who stop before age 35, survival is about the same as that for non-smokers.
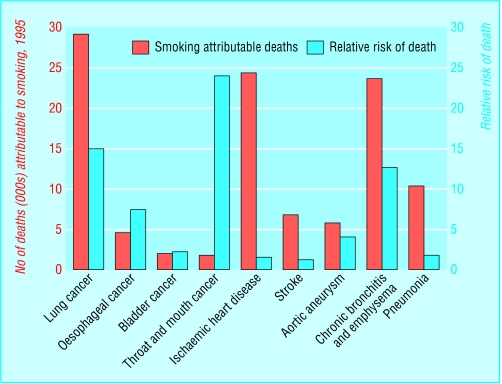
The rate and extent of reduction of risk varies between diseases—for lung cancer the risk falls over 10 years to about 30%-50% that of continuing smokers, but the risk remains raised even after 20 years of abstinence. There is benefit from quitting at all ages, but stopping before age 30 removes 90% of the lifelong risk of lung cancer. The excess risk of oral and oesophageal cancer caused by smoking is halved within five years of cessation.
Figure 5.
Numbers and relative risk of death (by cause) due to smoking, United Kingdom. Data from Tobacco Advisory Group of the Royal College of Physicians and Doll et al (see Further Reading box)
The risk of heart disease decreases much more quickly after quitting smoking. Within a year the excess mortality due to smoking is halved, and within 15 years the absolute risk is almost the same as in people who have never smoked. In a meta-analysis by Wilson and colleagues in 2000, the odds ratio for death for smokers who stopped smoking after myocardial infarction was 0.54, a far higher protective effect than the 0.75-0.88 odds ratio for death achieved by the conventional standard treatments for myocardial infarction, including thrombolysis, aspirin, β blockers, and statins. Smoking cessation also reduces the risk of death after a stroke and of death from pneumonia and influenza.
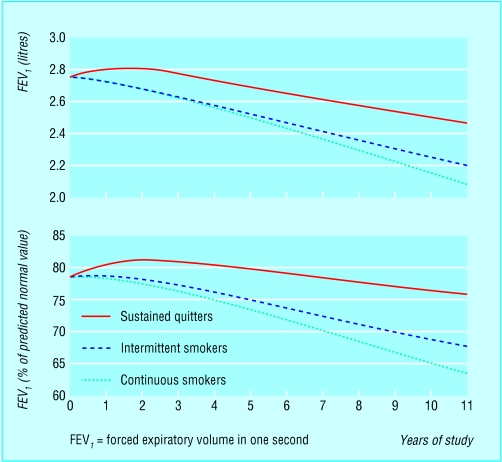
Smoking is associated with an accelerated rate of decline in lung function with age. Cessation results in a small increase in lung function and reverses the effect on subsequent rate of decline, which reverts to that in non-smokers.
Figure 6.
Effect of smoking cessation on rate of decline in lung function in chronic obstructive pulmonary disease. Adapted from Anthonisen et al. Am J Respir Crit Care Med 2002;166: 675-9
Thus, early cessation is especially important in susceptible individuals to prevent or delay the onset of chronic obstructive pulmonary disease. In patients with this disease, mortality and symptoms are reduced in former smokers compared with continuing smokers. Recent evidence shows that the benefits occur even in older patients with severe chronic obstructive pulmonary disease.
At a population level, the importance of smoking cessation is paramount. Peto has estimated that current cigarette smoking will cause about 450 million deaths worldwide in the next 50 years. Reducing current smoking by 50% would prevent 20-30 million premature deaths in the first quarter of this century and about 150 million in the second quarter. Preventing young people from starting smoking would have a more delayed but ultimately even greater impact on mortality.
Table 1.
Key points
| • Cigarette smoking is one of the greatest avoidable causes of premature death and disability in the world |
| • Helping smokers to stop smoking is one of the most cost effective interventions available in clinical practice |
| • Promoting smoking cessation should therefore be a major priority in all countries and for all health professionals in all clinical settings |
Effective prevention of cigarette smoking and help for those wishing to quit can therefore yield enormous health benefits for populations and individuals. Promoting and supporting smoking cessation should be an important health policy priority in all countries and for healthcare professionals in all clinical settings. However, this has not so far generally been reflected at a policy level or in the practice of individual healthcare professionals.
Stopping smoking before or in the first three to four months of pregnancy protects the fetus against the reduced birth weight associated with smoking. Preoperative cessation reduces perioperative mortality and complications
Richard Edwards is senior lecturer in public health in the evidence for population health unit at the Medical School, University of Manchester.
The ABC of smoking cessation is edited by John Britton, professor of epidemiology at the University of Nottingham in the division of epidemiology and public health at City Hospital, Nottingham. The series will be published as a book in the late spring.
Competing interests: RE is chairman of North West ASH (Action on Smoking and Health); he receives no financial reward for this work. JB has been reimbursed by GlaxoWellcome (now GlaxoSmithKline) for attending two international conferences, has received a speaker's honorarium from GlaxoWellcome, and has been the principal investigator in a clinical trial of nicotine replacement therapy funded by Pharmacia. Both these companies manufacture nicotine replacement products.
References
- • Tobacco Advisory Group of the Royal College of Physicians. Nicotine addiction in Britain. London: Royal College of Physicians of London, 2000. www.rcplondon.ac.uk/pubs/books/nicotine/index.htm
- • Jha P, Chaloupka F, eds. Tobacco control in developing countries. Oxford: Oxford University Press, 1999.
- • Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking: 40 years' observations on male British doctors. BMJ 1994;309: 901-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- • World Bank. Curbing the epidemic: governments and the economics of tobacco control. Washington, DC: World Bank, 1999. www1.worldbank.org/tobacco/reports.asp [DOI] [PMC free article] [PubMed]
- • US Department of Health and Human Services. The health benefits of smoking cessation: a report of the surgeon general. Rockville, MD: US Government Printing Office, 1990. (DHHS publication No (CDC) 90-8416.)
- • Wilson K, Willan A, Cook D. Effect of smoking cessation on mortality after myocardial infarction. Arch Intern Med 2000;160: 939-44. [DOI] [PubMed] [Google Scholar]