Abstract
Several studies in recent years have provided evidence that Pseudomonas aeruginosa has a non-clonal population structure punctuated by highly successful epidemic clones or clonal complexes. The role of recombination in the diversification of P. aeruginosa clones has been suggested, but not yet demonstrated using multi-locus sequence typing (MLST). Isolates of P. aeruginosa from five Mediterranean countries (n = 141) were subjected to pulsed-field gel electrophoresis (PFGE), serotyping and PCR targeting the virulence genes exoS and exoU. The occurrence of multi-resistance (≥3 antipseudomonal drugs) was analyzed with disk diffusion according to EUCAST. MLST was performed on a subset of strains (n = 110) most of them had a distinct PFGE variant. MLST data were analyzed with Bionumerics 6.0, using minimal spanning tree (MST) as well as eBURST. Measurement of clonality was assessed by the standardized index of association (IA S). Evidence of recombination was estimated by ClonalFrame as well as SplitsTree4.0. The MST analysis connected 70 sequence types, among which ST235 was by far the most common. ST235 was very frequently associated with the O11 serotype, and frequently displayed multi-resistance and the virulence genotype exoS −/exoU +. ClonalFrame linked several groups previously identified by eBURST and MST, and provided insight to the evolutionary events occurring in the population; the recombination/mutation ratio was found to be 8.4. A Neighbor-Net analysis based on the concatenated sequences revealed a complex network, providing evidence of frequent recombination. The index of association when all the strains were considered indicated a freely recombining population. P. aeruginosa isolates from the Mediterranean countries display an epidemic population structure, particularly dominated by ST235-O11, which has earlier also been coupled to the spread of ß-lactamases in many countries.
Introduction
Pseudomonas aeruginosa has an extraordinary metabolic versatility, enabling the bacterium to thrive and persist in diverse ecological niches. It is ubiquitously distributed in water, soil, plants, animals and humans, and it is one of the most common nosocomial pathogens in intensive care units (ICUs) [1]. In addition, this opportunistic pathogen is a major cause of morbidity and mortality in cystic fibrosis patients [2].
The pathogenicity of P. aeruginosa is conferred by numerous secreted virulence factors. These include elastase, exotoxin A, phospholipase, and protease alkaline [3], [4]. Similar to other gram-negative bacilli, the type III secretion system (TTSS) is considered an important determinant of cytotoxicity and invasion process in which P. aeruginosa directly delivers several effector proteins into the cytoplasm of the host cell [5], [6]. Dispersal is also facilitated by the emergence and persistence of multidrug resistant (MDR) clones in hospitals, mainly in intensive care units [7]. The increasing prevalence of MDR organisms is a global health problem [8], because of the limited choice of drugs for clinical treatment. Several studies reported that global dissemination is facilitated by MDR, often belonging to the serotypes O11 [9], [10], [11] and O12 [12], [13], [14], [15].
The sequencing of the whole genome of P. aeruginosa PAO1 unveiled one of the largest bacterial genome sequenced, counting 6.3 Mbp and encoding 5,570 open reading frames, the majority of which still have an unknown function. Generally, the size and complexity of the P. aeruginosa genome reflects an evolutionary adaptation enabling it to colonize diverse environments and resist a variety of antimicrobial substances [16]. Furthermore, P. aeruginosa isolates are known to possess extensive genome plasticity, fluctuating from to 5.2 to 7.1 Mbp [17]. The P. aeruginosa genome is a mosaic of a conserved core and variable accessory segments [18], [19]. The core genome is characterized by a conserved synteny of genes, and a low average nucleotide divergence of 0.5. The accessory genome consists of a variable set of genomic islets and genomic islands, most of which belong to an ancient tRNA-integrated island type [20], [21], [22]. This diversity has been a starting point for several attempts of exploring the evolution of this organism and to follow up the global epidemiology.
In a bacterial population, clones are defined as groups of genetically indistinguishable isolates that are asexually descended from a common ancestor [23]. Bacterial population genetics as a discipline has developed over many decades, using Escherichia coli as the first model of study [24]. During this investigation the genetic population structure was investigated with multi-locus enzyme electrophoresis (MLEE). This technique aims to detect allelic variation within several metabolic genes simultaneously, on the basis of the differing electrophoretic mobilities of their gene products [25]. This technique has been used for several species [26], [27], [28], [29], [30]. The population structure of most of bacterial species was thought to be clonal [31], [32] until 1993 when Maynard-Smith et al. showed that they could vary from strictly clonal to highly sexual [33].
Multi-locus sequence typing (MLST) is based on the nucleotide sequences of housekeeping genes. Although it can evaluate only the genetic diversity of the core genome it is a robust, standardizable, and portable methodology that can be used in studies of genetic population structures [34], [35] which are facilitated by searchable web-based databases [http://pubmlst.org/paeruginosa]. The MLST database for P. aeruginosa, similar to most other MLST databases, is skewed towards isolates displaying particular types of resistance [36], [37], [38], [39], particular infection types (e.g. cystic fibrosis) [40], [41], [42], or particular geographical regions [43], [44] that have been investigated more thoroughly. For this reason available data do not necessarily elucidate population structures as they are prone to phylogenetic discovery bias. Lastly, diversification of P. aeruginosa clones has been attributed to frequent recombination, but not comprehensively demonstrated by using MLST-data.
Current evidence suggests that several pathogenic strains belong to epidemic clones that spread over large part of Mediterranean Europe, and that they frequently belong to the O11 and O12 serotypes [45]. However, isolates from the southern side of the Mediterranean basin have not yet been sufficiently characterized. In this present study we analyzed a collection of P. aeruginosa isolated from five Mediterranean countries (Tunisia, Libya, Spain, Italy and France) by genotypic and phenotypic methods, including serotyping, antimicrobial susceptibility, virulence gene screening, Pulsed Field Gel electrophoresis (PFGE) and Multi-Locus Sequence Typing (MLST). The aims were to explore the genetic structure of the population, to evaluate the role of recombination in shaping the population structure, and finally to characterize epidemic clones.
Materials and Methods
Bacterial strains
Strains were collected from France (n = 30), Italy (n = 6), Spain (n = 20), Libya (n = 25), and Tunisia (n = 60). Isolates were selected to represent various sources to achieve both geographical spread and to elucidate potential relationships between clinical and environmental isolates. P. aeruginosa strains were collected from five Mediterranean countries most of which were clinical isolates derived from several sources (Table S1), whereas 18 isolates were environmental strains. We also included P. aeruginosa ATCC 27853 and PAO1, as well as the two Clone C strains CSGB8 (clinical) and SG17M (environmental). Strains were identified by standard microbiologic methods such as colony morphology, oxidase reaction, growth at 42°C, and ability to produce characteristic pigmentations on cetrimide agar. A few strains with atypical features were subjected to multiplex PCR targeting the lipoprotein genes oprI and oprL [46].
Pulsed-Field Gel Electrophoresis (PFGE)
PFGE typing was performed according to Giske et al [47] with minor modifications. All strains were digested with SpeI and the resulting fragments were separated by electrophoresis in 1.2% agarose in a CHEF-Mapper (Bio-Rad, Hercules, USA) in 0.5× Tris-Borate EDTA (TBE) running buffer at 12°C and 6 V/cm for 30 hours with pulse time ranging from 1 to 50 s. P. aeruginosa ATCC 27853 was used as reference and included in every 6 lanes to allow calibration and normalization of gels. Gels were stained with ethidium bromide and photographed in a Geldoc EQ (BioRad Laboratories, Hercules, CA). The resulting photographic images were analyzed with the GelCompar II software (Applied Maths, NV St-Martens-Latem, Belgium). The band patterns were compared using the Dice-coefficient by using the unweighted pair group method to determine band similarity accordingly to the criteria established by Tenover et al [48]. A Dice coefficient of ≥0.80 was considered suggestive of possible clonal relatedness.
Multi-Locus Sequence Typing (MLST)
A total of 110 P. aeruginosa strains, most of which contained different SpeI macro-restriction profiles, were typed using MLST. MLST was performed according to Curran et al [43] but with slight modifications concerning the annealing temperature of housekeeping gene (acsA, aroE, guaA, mutL, nuoD, ppsA and trpE) amplification and the designing of new nested sequencing primers for the acsA (Forward primer: 5-TGT TCG ARG GYG TRC CGA ACT A-3) and nuoD (forward primer: 5-AAC CAY CCB TCC GCC CAC GG-3) genes. For DNA extraction, overnight cultured P. aeruginosa isolates were heated to 100°C for 10 min. Housekeeping genes were amplified by real-time PCR. Reactions were performed on a Rotorgene 6000 (Corbett Robotics Inc; San Francisco, CA, USA) using the QuantiTect SYBR Green PCR mix (Qiagen, Valencia, CA, USA). Amplification reaction mixture comprised 25 µl Quantitect SYBR 2 X Green PCR Mastermix, 1 µM of each primer, template DNA 5 µl and H2O to a final volume 50 µl. The PCR program was as follows: 15 min of initial denaturation at 95°C, then 40 cycles at 95°C for 30 s, between 58 to 62°C depending on locus at 30 s, and 72°C for 90 s. A final melting curve analysis was performed to determine the presence or absence of non-specific amplification products. PCR products were purified using Jetquick Spin Column Technique (Genomed GMBH, Löhne, Germany) and used as template for DNA sequencing reaction. Templates were sequenced on both strands with the published primers and the new designed primers using the BigDye Terminator Ready Reaction Mix v3.1. Nucleotide sequences were determined for both strands by ABI Prism 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA). New allelic variants were repeated and confirmed in triplicate.
Serotyping
Strains were grown overnight on LEC agar at 37°C and subjected to O-antigen serotyping using slide agglutination according to the International Antigenic Typing Scheme (IATS) for P. aeruginosa [49]. The serotyping protocol is based on 4 polyclonal and 16 monovalent antisera (Bio-Rad Laboratories, Marnes-La-Coquette, France). Association between serotypes and presence of virulence genes and multidrug-resistance was analyzed with two-tailed Fisher's exact test.
Detection of exoS and exoU
Virulence gene were detected by PCR amplifications: the reactions were carried out on PTC 200: the 25 µl of volume reaction contained 12.5 µl 2X GoTaq® Green Master Mix (Promega), 0.25 µM of each forward and reverse primer, 2,5 µl of chromosomal DNA and H2O to final volume. The PCR program of exoS and exoU genes was performed as described by Feltman et al [50].
Antimicrobial susceptibility testing
All isolates were subjected to disk diffusion (Oxoid, Basingstoke, UK) susceptibility testing versus ceftazidime, piperacillin-tazobactam, imipenem, meropenem, ciprofloxacin and gentamicin, according to the guidelines of the European Committee for Antimicrobial Susceptibility Testing (http://www.eucast.org/clinical_breakpoints/; accessed on 18 May 2011). Isolates resistant to ≥three antibiotics from different classes were considered multidrug-resistant (MDR) [51] .
Analysis of MLST-data
All chromatograms were imported, assembled, edited and trimmed in Bionumerics (6.0: Applied-Maths, Sint Maartens-Latem, Belgium). For each locus, distinct allelic variants were assigned an allelic number and each unique combination of seven allele numbers was assigned a novel sequence type (ST). Based on allelic profiles the evolutionary relationship between isolates was assessed by the algorithm Minimal Spanning Tree (MST) implemented in Bionumerics. The MST is a graphical tool that links the nodes by unique minimal paths in a given dataset, i.e. total summed distance of all branches is minimized [52]. The algorithm uses an ST with the highest numbers of single locus variants (SLVs) as a root node and derives other STs from it. Using a stringent definition of 5/7 shared alleles, MST could then connect all strains and link all related STs into clonal complexes. Accordingly, singletons were defined as STs having at least three allelic mismatches with all other STs.
Descriptive analyses of the genetic variability at MLST loci such as the determination of the mean G+C content, average number of synonymous and non-synonymous sites, average non-synonymous/synonymous ratio (dN/dS), the number of polymorphic sites, the nucleotide diversity per site (π) and the average number of nucleotide differences per site (è) were performed with DnaSPv5 [53]. The software MEGA 4 [54] was used to build a neighbor-joining tree from the concatenated seven sequences using the Kimura-2-parameter distance measure. The eBURSTv3 software (http://eburst.mlst.net) [55], was used also to relate the STs detected in our study to the entire dataset in the MLST database (http://pubmlst.org/paeruginosa/). START2 [56] was used to calculate the index of association (IA S) between all STs (http://pubmlst.org/software/analysis/start2/). The Neighbor-Net implemented in the software SplitsTree 4.0 [57] with 1,000 bootstrap replicates was used to create the phylogenic network for the individual loci and for concatenated sequences. Further, we used the pairwise homoplasy index (PHI) [58] implemented in SplitsTree 4.0 in order to test the role of past recombination in generating allelic variation. ClonalFrame [59] was used to investigate the population structure by inferring relationship among STs. The basis for this software is a model of genetic diversification that estimates the relative probabilities that a nucleotide is changed as the result of recombination relative to point mutation (r/m ratio). Concatenated sequences were formatted as an eXtended Multi-Fasta Alignment (XMFA). A 50% consensus tree was constructed from 6 runs using the defaults settings. Evidence of recombination events were also searched between sequences of single and concatenated loci using seven algorithms (RDP, Geneconv, BootScan, MaxChi, 3Seq, Chimaera, and SiScan implemented in the RDP 3.27 software [60]. Only recombination events detected by at least three methods and involving parental sequences present in the MLST data set were considered.
Results
Antimicrobial susceptibility testing, serotyping and exoS/exoU detection
Antimicrobial susceptibility testing according to EUCAST yielded 52 (35.8%) multidrug resistant (MDR) strains. Most of the MDR isolates were clinical, except three isolates which were environmental: TN310, TN500 and LB30.
Serotyping (Table S1) revealed that serotype O11 with 35.1% frequency was the most prevalent among the isolates (51/145). The other prevalent serotypes were O6 (13.1%), O1 (11%), O4 (8.2%) and O12 (6.2%). Serotypes O3, O10, O5, O7, O9, O2 and O15 were all detected in less than 5% of the isolates. The remaining non-serotypeable strains (9.6%), consisted of 11 polyagglutinable and 3 nonagglutinable isolates. Multidrug-resistance was significantly more common among the O11 isolates (29/51) than among the non-O11 isolates (23/94) (p = 0.0001).
Screening of exoS and exoU genes was performed in all isolates (Table S1). A total of 61% of strains harbored exoS genes, 35% had exoU, and 1.3% contained both exoS and exoU. Among O11 isolates 78% (40/51) had exoU, whereas only 12% of the non-O11 isolates (12/94) were positive for exoU (p<0.0001). Among the non-O11 isolates exoS was more common (83 vs 12%, p<0.0001). Only two strains featured both exoS/exoU and in five isolates amplification was negative for both genes.
PFGE
The PFGE analysis was performed on all P. aeruginosa isolates except the two Clone C strains. By applying the criteria proposed by Tenover et al [48] for the differentiation of P. aeruginosa by pulsed-field gel electrophoresis for possible genetic relatedness (maximum 6 band difference; Dice coefficient 80%). A total of 93 distinct genotypes were recovered from this collection from which 72 strains were singletons and 71 strains segregated into 21 cluster or groups of related isolates comprised of two or more isolates and denoted A–U (Table S1). All these groups displayed close relationship by sharing traits such as MDR profile, serotypes and source of infection or country.
Each strain representative of a distinct profile (Table S1) was subjected to MLST. Occasionally several representatives of a distinct profile were typed with MLST when divergence in serotype, source of infection, geographical origin, MDR profile or genotype of virulence genes was ascertained.
MLST analysis and phylogenetic relationship
MLST identified 70 STs among 110 strains, most of them with distinct PFGE-profiles (<80% similarity). All selected strains were successfully typed except two strains (excluded from MLST analysis) for which we were not able to amplify the trpE locus (strain CECT119), and one strain where both trpE and ppsA were not successfully amplified (strain FC1). The characteristics of each locus are displayed in Table 1. The G+C content was relatively high, and ranged from 63 (nuoD) to 70% (aroE) which is similar to the G+C content of the entire genome of the reference strain P. aeruginosa PAO1 (67%) [16]. The number of alleles at each locus ranged from 15 to 26. The number of polymorphic sites was overall low and found to be 5.5% for the concatenated sequences, indicating as expected a very low values of π and è (Table 1). The ratio of non-synonymous to synonymous nucleotide changes (dN/dS) was calculated for all 7 gene loci and found equal to 0 for nuoD and trpE genes but ranged from 0.13% to 9.43% for the remaining genes. A ratio of dN/dS <1 indicates that genes are evolving predominantly by purifying selection.
Table 1. Characteristics and polymorphism of housekeeping gene of Pseudomonas aeruginosa. π, nucleotide diversity per site; π, average number of nucleotide differences per site; dS: No. of synonymous changes per synonymous site.
| Allele | Size | Haplotype | Polymorphicsites | π | π | G+C | dN | dS | dN/dS | PHI test |
| acsA | 390 | 24 | 21 | 0.011593 | 0.010698 | 0.6879 | 0.00006 | 0.04454 | 0.0013 | 0.011 |
| aroE | 495 | 22 | 34 | 0.011903 | 0.013026 | 0.7083 | 0.00325 | 0.03444 | 0.0943 | 0.004 |
| guaA | 372 | 26 | 17 | 0.007513 | 0.008666 | 0.6584 | 0.00007 | 0.03001 | 0.0023 | 0.036 |
| mutL | 441 | 20 | 22 | 0.005358 | 0.009461 | 0.6705 | 0.00054 | 0.01935 | 0.0279 | 0.5 |
| nuoD | 366 | 15 | 18 | 0.004525 | 0.009327 | 0.6308 | 0.00000 | 0.01879 | 0.0000 | 0.018 |
| ppsA | 369 | 20 | 19 | 0.007714 | 0.010279 | 0.6656 | 0.00020 | 0.02972 | 0.0067 | 0.008 |
| trpE | 441 | 24 | 28 | 0.009903 | 0.012901 | 0.6661 | 0.00000 | 0.03671 | 0.0000 | 0.001 |
| Concatenate | 2874 | 70 | 159 | 0.008504 | 0.010756 | 0.6722 | 0.00067 | 0.03089 | 0.0216 | 0.000 |
dN: No. of non-synonymous changes per non-synonymous site.
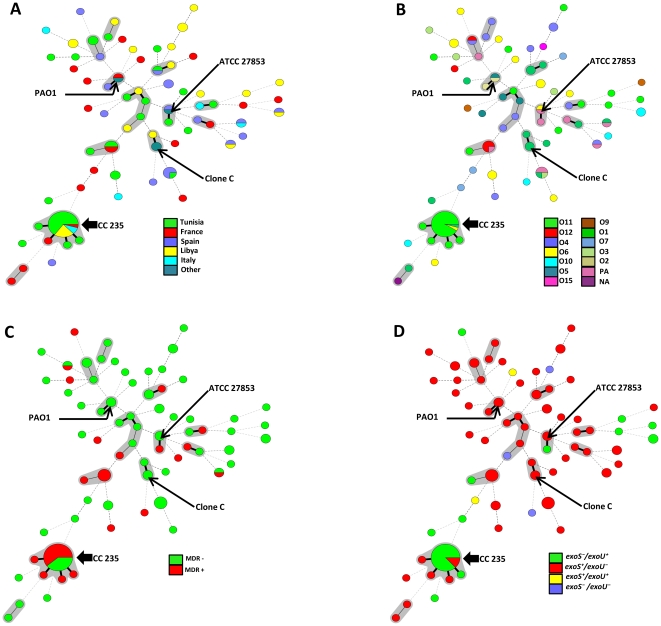
In order to determine the clonal relationship between isolates, we used Minimal Spanning Tree (MST) method based on allelic profiles. Two allelic mismatches were allowed for group definition, similar to what is used for group definition with eBURST. The 110 sequence typed isolates were distributed into 50 isolates not belonging to any clonal complexes and 12 groups of a total of 60 isolates corresponding to clonal complexes found in the database (Figure 1). The main clonal complex detected was CC235, consisting of five STs (235, 989, 979, 230 and 227, with ST 235 as the primary founder). The second most frequently encountered clonal complex CC244 consisted of five STs (244, 990, 986, 993 and 654 with ST 244 as the primary found). The 10 others groups or simple complexes were doublets with the following STs linked: 155 and 811, 996 and 242, 992 and 527, 111 and 229, 549 and 699, 228 and 175, 224 and 977, 252 and 984, 17 and 845, 988 and 980.
Figure 1. Minimal Spanning Tree (MST) analysis of Pseudomonas aeruginosa strains based on MLST data.
Each circle corresponds to an ST. The area of each circle corresponds to the number of isolates. The relationships between strains are indicated by the connections between the isolates and the lengths of the branches linking them. Black lines connecting pairs of STs indicate that they differ in one allele (thick lines), two alleles (thin), or three to seven alleles (dashed). Grey zones surround STs that belong to the same clonal complex (clonal complex were defined from this collection, and CC235 was the predominant). Four MST graphs were generated separately based on the following associations. A: ST vs countries, B: ST vs serotype, C: ST vs multidrug-resistance and D: ST vs exoS/exoU.
The MST analysis revealed several interesting relations between countries, serotype, MDR phenotype and presence of virulence genes (Figure 1). MST disclosed the relatedness of STs and displayed a random repartition, especially of the countries and serotypes among isolates. Several STs and some minor clonal complexes were shared by more than one country and one serotype, but most of them were non-MDR and carried the gene exoS. Noteworthy, CC235 was identified as a major clonal complex consisting of 27 strains, whereof 25 were serotype O11. Two of the ST235 isolates (TN310 and TN330) were environmental strains. Most of the isolates in ST235 contained the exoU virulence gene (n = 20), and 14/27 isolates were MDR.
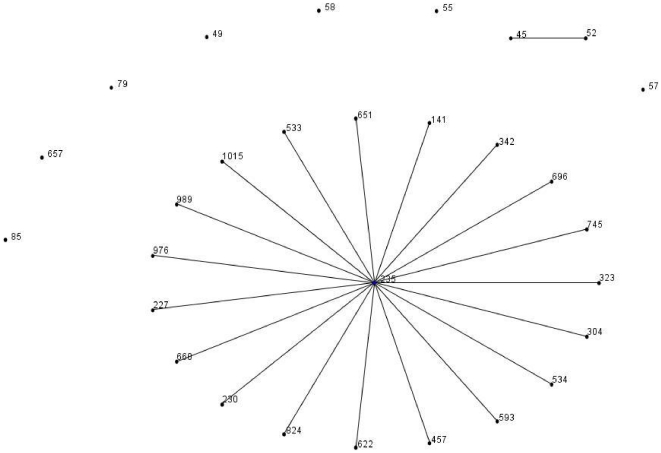
By applying eBURST on all P. aeruginosa databases, we could demonstrate several clonal lineages. Of them, CC235 consisted of 29 STs whereof ST235 is a primary founder surrounded by 19 SLVs, two double-locus variants (DLV), three triple-locus variant (TLV) and four satellites (>three locus variant; SAT) (Figure 2).
Figure 2. eBURST diagram of the lineage CC235 of all P.aeruginosa MLST database displayed like a star-like tree.
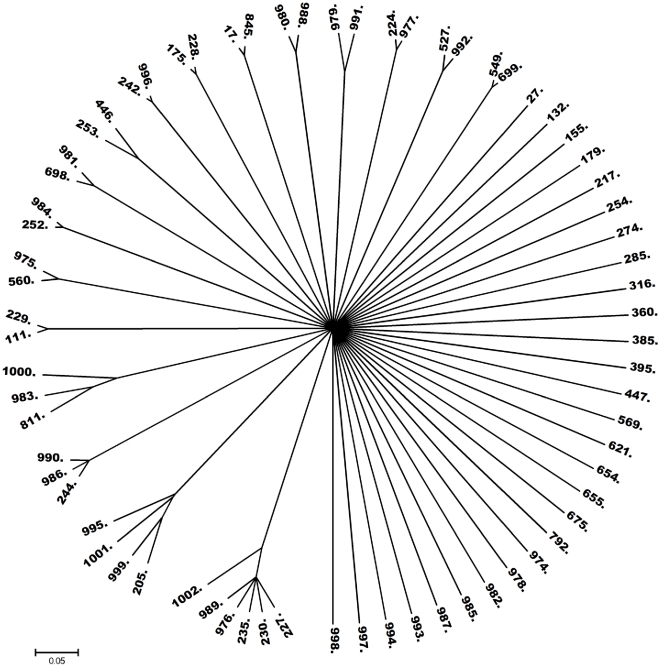
Further analysis of the MLST data was conducted with neighbor-joining tree analysis based on concatenated sequences (Figure S1). The analysis revealed a weak bootstrapping value especially with major branches. The dendrogram did not show a clear phylogenetic structure presenting as well defined groups. Instead most of the branches were equidistant with the exception of a few clusters corresponding to clonal complexes previously defined by eBURST. ClonalFrame generated a 50% majority-rule consensus tree from the combination of 6 runs (Figure 3). The resulting dendrogram displays the relationships between STs. Several clusters were identified which were previously obtained by Minimal Spanning Tree (MST) or eBURST.
Figure 3. Radial phylogenetic tree of 70 STs of P. aeruginosa: A 50% majority consensus tree for the clonal genealogies obtained after six ClonalFrame runs.
Correlation between PFGE and MLST
With PFGE we obtained 93 genotypes or profiles based on a similarity cut-off at 80%. With MLST 70 STs were obtained from 110 strains and 12 clonal complexes were identified. A one-to-one correlation between PFGE patterns and STs existed in 48 cases (Table S1), most of them ST singletons that had unique PFGE patterns (similarity <80%). As expected, several isolates belonging to same PFGE groups (similarity ≥80%) (A, C, E, F, H, I, K, M, O, Q, S and T) were shown to have the same STs (Table S1). Although the correlation was mostly excellent, PFGE groups D (similarity >80%) comprised two isolates displaying different STs. We observed that isolates with identical STs were found in multiple PFGE-types. Seven pairs of strains had respectively the same ST (792, 155, 252, 254. 253 and 111), but all of them had distinct PFGE types. STs 274 comprised 3 isolates, that were all unrelated by PFGE. Interestingly ST 235, identified in 23 strains, was found also in isolates with similarity levels below 80%.
Evidence of recombination
Based on findings in previous studies [43], [61], [62], [63], [64], [65], [66] we attempted to unravel the evolution and diversity in the population of P. aeruginosa from Mediterranean countries. The test of clonality was assessed with a standardized index of association (IA S), this statistical test attempts to measure the extent of linkage equilibrium within a population by quantifying the amount of recombination among a set of sequences and detecting associations between alleles at different loci. Analysis of the entire dataset of 110 isolates yielded an IA S of 0.35 (p< 0.001) and that for the 70 singleton STs was found to be 0.07 (p< 0.001). The obtained values indicate that recombination plays a key role in the distribution of alleles.
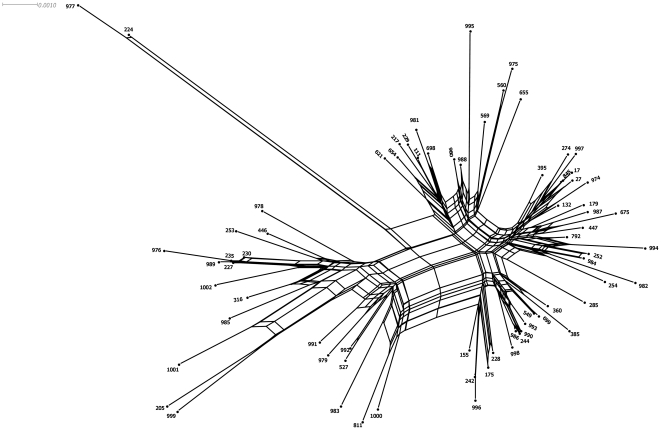
To gather further evidence on the presence of frequent recombination we used SplitsTree v.4 to perform a phylogenetic network analysis with the Neighbor-Net method. This algorithm was conducted separately for each locus (Figure S2) and for the concatenated sequences (Figure 4). The result of PHI test for each locus showed statistically significant recombination, except for the mutL allele. Using concatenate sequences, this test produced statistically significant evidence of recombination (p<0.05). Evidence of recombination was also supported by visual inspection of the bushy network structure (Figure 4) with complex parallelogram formation indicative of extensive homologous recombination. In contrast, the Neighbor-Net graph of mutL showed a tree-like structure this indicating probably that this gene was not affected by intragenic recombination (Figure S2). Moreover, ClonalFrame confirmed our previous finding and the inferred value of recombination to mutation, r/m, was estimated to be 8.4 (95% CI 4.7–13.7), strongly suggesting that nucleotide change in housekeeping genes occurs more frequently by recombination than de novo mutation. Finally, the events of recombination were not accurately identified by the software RDP 3.27.
Figure 4. Neighbor-Net graph based on concatenated sequences on 7 housekeeping genes of Pseudomonas aeruginosa showing a bushy network structure indicating of a pervasive homologous recombination.
Discussion
Several studies suggest that P. aeruginosa possesses an epidemic panmictic population structure [67], [68]. The sequencing of 6 loci from 19 clinical and environmental strains revealed a net-like population structure marked by high level of recombination [62]. Lomholt et al, favoured an epidemic structure, consisting of epidemic clones pathogenic in ocular infections with distinct combination of virulence factors [61]. Combined sequence-based techniques, such as sequencing of the outer membrane lipoprotein, with serotyping and pyoverdine type were used by Pirnay et al in a polyphasic approach to reveal extensive genetic mosaicism, particularly in the oprD gene [65]. A later study of a large collection of 328 strains from diverse origins and habitats was in accordance with the first one, confirming the non-clonal epidemic population structure of P. aeruginosa and indicating that there are no widespread cystic fibrosis epidemic clones [64]. More recently, Curran et al analysed population structure by developing a Multi-Locus Sequence Typing (MLST) scheme and suggested a non-clonal structure punctuated by closely related genotypes or clonal complexes [43]. Furthermore, in 2007 Wiehlmann and colleagues analyzed 240 P. aeruginosa strains with a DNA array tube assay which is an informative genotyping method designated for typing strains in both the conserved core and flexible accessory genome. However, this work strongly indicated that the population structure was more complex than previously reported [66].
The findings in this study are in support of a panmictic population structure for P. aeruginosa clinical and environmental isolates from both sides of the Mediterranean basin, punctuated by epidemic clones. We demonstrated an index of association of 0.35 for the entire population, and 0.07 when looking separately at the singleton sequence types. Under panmixis, linkage equilibrium will be observed and the IA S approaches 0, whereas a clonal population will display an IA S value that differs significantly from 0. More recently; by applying multilocus SNP typing on two unrelated strain collections, the index of association was consistently calculated in two independent studies to be 0.29 [43] and 0.31 [62]. This finding strongly indicates that the studied isolates of P. aeruginosa exhibited an epidemic non-clonal population structure.
The minimal spanning tree (MST) analysis shed further light on the role of epidemic clones, demonstrating a very important role of clonal complex 235. ST235 is the primary founder of this clonal complex, surrounded by 4 single locus variants, and isolates sharing this ST were found in all countries except Spain. Previous reports have linked this ST also to Spain. ST235 and also some other STs (17, 27,111, 155, 175, 179, 244 and 253) which have been encountered in different countries over several years were detected in this study, but not the worldwide dispersed ST277 [69]. Several new STs were detected (ST972-ST1002), demonstrating that the MLST database is still novel and continuously growing.
Remarkably, our dataset roughly disclosed CC235 as a highly successful clone widespread in the population. Maynard Smith et al. [33] first pointed out that the over-representation of closely related, high frequency (epidemic) clones in a sample will lead to an inflated estimate of clonality of such population as a whole. Oversampling of a single clone in an epidemic population structure will therefore result in an underestimation of homologous recombination rates. A wide spectrum of methods exist to estimate this ratio, however they vary in their ability to detect recombination [59], [70], [71]. For example, eBURST [55], [72] can estimate the ratio of r/m. We have rejected this test for two reasons, the first because this method has the disadvantage of scanning the clonal diversification between close relatives within clonal complexes, and could therefore produce inflated results if the role of recombination has increased in recent time. The second reason was that our dataset contained few larger clonal complexes; in fact only two dominant clonal complexes were detected.
ClonalFrame was developed to handle MLST data and is able to infer the rates at which mutation and recombination events occur over time, as well as the average size of recombination events [59]. By analysing our data with ClonalFrame we determined the r/m ratio to 8.4 (95% CI 4.7–13.7) demonstrating that homologous recombination has more impact on sequence evolution than mutation. Phylogenetic networks, such as the one constructed by the Neighbor-Net method, can represent the evolutionary relationships among recombining bacteria, as conflicting signals can be represented as a network instead of bifurcating tree. Using individual loci and concatenated sequences we found highly statistically significant recombination, supported also by visual inspection of the bushy network structure with complex parallelogram formation indicating a history of intragenic and intergenic recombination among housekeeping genes and responsible for the diversification of genotypes or sequences types. Here for P. aeruginosa, divergence among genotypes appeared to be mainly driven by recombination. The rate of homologous recombination within bacterial species can differ widely from one species to another [33], [73]. One of the striking features of P. aeruginosa is its capability to customize its genome to fit the needs for thriving in any actual and virtual environment [74]. This genomic reorganization is favored by the acquisition of blocks of genes through horizontal gene transfer for some strains and the deletions of specific chromosomal segments in others [19], [20], [22], [74]. As natural transformation is not encountered in P. aeruginosa, horizontal gene transfer appears to play a major role for the observed dynamic genome. As a consequence horizontal gene transfer enables P. aeruginosa to adapt to different habitats with acquisition of new traits without eliminating others, and hence the organism retains its ability to thrive in a wide range of environments [74].
The present study revealed that the clonal complex CC235 was strongly associated with O11 serotype strains from several countries, not restricted to particular clinical syndromes, and was also found in sea water and in the hospital environment (Table S1). Most of the CC235 strains featured virulence gene exoU and more than the half were MDR. Hence, CC235 is a successful epidemic clone associated with particular traits, but heterogeneous for others. This finding corroborates earlier observations that there is no correlation between P. aeruginosa clones and disease or habitats. [62], [63], [64], [75], [76].
The type III secretion system (TTSS) is considered as an important determinant of virulence for P. aeruginosa [5], [6], being present in some isolates and absent in others [77], and they are dispersed through the genome of P. aeruginosa [16]. Using TTSS, P. aeruginosa is able to deliver among others ExoS and ExoU inside eukaryotic cells. Exoenzyme S (exoS), a major cytotoxin involved in colonisation, invasion and dissemination of bacteria during infection, is regarded the most prevalent of the TTSS proteins [78]. Genes encoding these toxins are inconstant in P. aeruginosa isolates. In fact, exoS prevalence among cystic fibrosis patients is significantly higher than that in non-CF isolates [64], [79]. ExoU has been found to be associated with diverse infections [80]. In a mouse model of acute pneumonia, ExoU had the greatest impact on disease severity [81]. It has also been shown in one study that ExoU is substantially more cytotoxic than ExoS [82]. The prevalence of virulence genes in our collection corroborates previous reports [50]. Our study revealed that the genotype exoU was frequently associated with ST235-O11 isolates, and rarely occurred among O1, O10, O6 and O7 isolates. Earlier studies were partially in agreement with our findings [83], [84]. By comparing various genomes of various strains harbouring the exoU gene, Kulasekara et al. pointed out the evolutionary history of exoU locus, the mechanism including transposition of exoU determinants via horizontal transmission on plasmid followed by integration into different P. aeruginosa isolates [78]. Even though exoS and exoU are located in distinct loci [16], [85], the simultaneous carriage of both genes does usually not occur [22], [50], [84]. The mechanism of their incompatibility is still ambiguous. Our work revealed that few strains encoded both exoS and exoU, however this combination has been described earlier on rare occasions [64]. The explanation might be that exoU is transferred with genomic islands, and the acquisition of this gene through horizontal gene transfer may enhance colonisation and survival in different host environments [22]. Consequently, selective pressure probably acted as a driving force of these genomes in different environmental niches by mutual exclusion of exoS or exoU [22].
Most CC235 strains were shown to have distinct or unrelated PFGE patterns types and in some cases the similarity was below 80%. Similar observations have been made for e.g. the successful E. coli clone ST131, which can also exist in many PFGE-variants [86]. The diversity of PFGE-patterns in ST235 (data not shown) suggests the presence of microevolution within this sequence type.
By using MLST and PFGE, several independents studies focused on the underlying mechanisms of P. aeruginosa MDR. These studies provided evidence that ST235 is an international clone belonging to the BG11 complex that has been detected in Greece, Italy, Hungary, Poland, Sweden, Spain, France, Russia, USA, Japan [38], [47], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97] Singapore, and Brazil (http://pubmlst.org/paeruginosa/). Interestingly, the resistance determinants of ST235 isolates were mapped and examined and found to be associated with several acquired ß-lactamases: PER, OXA GES, VIM and IMP. ST235 has been linked to a variety of horizontally acquired genetic elements (integrons, transposons and plasmids) [93], [98]. Here we suggest an impact of microevolution discerned by a genetic capacity of ST235 isolates having undergone several genetic events giving rise to successful strains carrying out specific traits (MDR and O11).
The flexibility of the genome of ST235 clone and its trend to be widely dispersed in the world is reflected by the birth of several single locus variants (SLVs). Two novel SLVs were determined in our work. When, applying eBURST on MLST database (data not shown) we observed several groups, from which the CC235 is an interesting lineage that consisted of 29 STs (Figure 2; ST235 is primary founder surrounded by 19 SLVs). Strikingly and accordingly to the MLST database, CC235 displayed as a star like-tree with ST235 representing the parsimonious founder, it was indeed associated with the greatest number of SLVs (Figure 2). On the basis of these findings we argue that such a versatile genetic background enables clones such as ST235 clones to be successful and prevalent in many diverse habitats. However, we have likely shown a local polymorphism in CC235 strains which could influence their fitness in a drug resistance point of view. Also, ST235 clones were first described in the last few years, and the origin of them has not yet been defined.
In conclusion, this study confirms the hypothesis of a non-clonal epidemic population structure, and expands the current database to countries south of the Mediterranean basin. An important subtype was identified as CC235 O11 clone, often associated with exoU and multidrug-resistance and largely successful. Importanly, this clone plays a defining role in the dissemination of class A ESBLs and metallo-β-lactamases with potentially significant implications for public health. Lastly, the study demonstrates unequivocally that recombination is the most decisive factor for diversification of P. aeruginosa clones. Although the database includes non-MDR isolates, it would greatly benefit from a larger sample collection from different parts of the world. More work is necessary to further understand the phylogeny of P. aeruginosa and its population biology on a global level.
Supporting Information
Neighbor-joining tree constructed using MEGA 4, showing relationships between the concatenated sequences of all P. aeruginosa STs (n = 70). Bootstrap values are indicated at corresponding nodes and STs at end of branches. Bar is 0.002 substitutions per site.
(TIFF)
SplitsTree networks for each individual locus of Pseudomonas aeruginosa housekeeping gene.
(TIFF)
Database displaying the phenotypic and genotypic features of the studied strains: strains, sources, countries, allelic profiles, STs, serotypes, virulence genes, presence of multidrug-resistance, PFGE patterns, PFGE groups, clonal complexes. Representative isolates for PFGE-clusters that were subjected to MLST are highlighted in column 1.
(XLS)
Acknowledgments
We thank Inga Karlsson, Saber Yousefi, Marie Andersson and Petra Edquist for excellent technical assistance. We would also like to thank Ute Römling for providing two P. aeruginosa clone C strains. This publication made use of the Pseudomonas aeruginosa MLST website (http://pubmlst.org/paeruginosa/) developed by Keith Jolley and sited at the University of Oxford, U.K.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Internal funding at the Karolinska University Hospital and funding from the Ministry of Higher Education and Scientific Research in Tunisia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bergmans DC, Bonten MJ, Gaillard CA, van Tiel FH, van der Geest S, et al. Indications for antibiotic use in ICU patients: a one-year prospective surveillance. J Antimicrob Chemother. 1997;39:527–535. doi: 10.1093/jac/39.4.527. [DOI] [PubMed] [Google Scholar]
- 2.Lyczak JB, Cannon CL, Pier GB. Lung infections associated with cystic fibrosis. Clin Microbiol Rev. 2002;15:194–222. doi: 10.1128/CMR.15.2.194-222.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doring G, Maier M, Muller E, Bibi Z, Tummler B, et al. Virulence factors of Pseudomonas aeruginosa. Antibiot Chemother. 1987;39:136–148. doi: 10.1159/000414341. [DOI] [PubMed] [Google Scholar]
- 4.Van Delden C, Iglewski BH. Cell-to-cell signaling and Pseudomonas aeruginosa infections. Emerg Infect Dis. 1998;4:551–560. doi: 10.3201/eid0404.980405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holder IA, Neely AN, Frank DW. Type III secretion/intoxication system important in virulence of Pseudomonas aeruginosa infections in burns. Burns. 2001;27:129–130. doi: 10.1016/s0305-4179(00)00142-x. [DOI] [PubMed] [Google Scholar]
- 6.Roy-Burman A, Savel RH, Racine S, Swanson BL, Revadigar NS, et al. Type III protein secretion is associated with death in lower respiratory and systemic Pseudomonas aeruginosa infections. J Infect Dis. 2001;183:1767–1774. doi: 10.1086/320737. [DOI] [PubMed] [Google Scholar]
- 7.Obritsch MD, Fish DN, MacLaren R, Jung R. National surveillance of antimicrobial resistance in Pseudomonas aeruginosa isolates obtained from intensive care unit patients from 1993 to 2002. Antimicrob Agents Chemother. 2004;48:4606–4610. doi: 10.1128/AAC.48.12.4606-4610.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Giske CG, Monnet DL, Cars O, Carmeli Y. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother. 2008;52:813–821. doi: 10.1128/AAC.01169-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deplano A, Denis O, Poirel L, Hocquet D, Nonhoff C, et al. Molecular characterization of an epidemic clone of panantibiotic-resistant Pseudomonas aeruginosa. J Clin Microbiol. 2005;43:1198–1204. doi: 10.1128/JCM.43.3.1198-1204.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kettner M, Milosovic P, Hletkova M, Kallova J. Incidence and mechanisms of aminoglycoside resistance in Pseudomonas aeruginosa serotype O11 isolates. Infection. 1995;23:380–383. doi: 10.1007/BF01713571. [DOI] [PubMed] [Google Scholar]
- 11.Sekiguchi J, Asagi T, Miyoshi-Akiyama T, Kasai A, Mizuguchi Y, et al. Outbreaks of multidrug-resistant Pseudomonas aeruginosa in community hospitals in Japan. J Clin Microbiol. 2007;45:979–989. doi: 10.1128/JCM.01772-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bingen E, Bonacorsi S, Rohrlich P, Duval M, Lhopital S, et al. Molecular epidemiology provides evidence of genotypic heterogeneity of multidrug-resistant Pseudomonas aeruginosa serotype O:12 outbreak isolates from a pediatric hospital. J Clin Microbiol. 1996;34:3226–3229. doi: 10.1128/jcm.34.12.3226-3229.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crespo MP, Woodford N, Sinclair A, Kaufmann ME, Turton J, et al. Outbreak of carbapenem-resistant Pseudomonas aeruginosa producing VIM-8, a novel metallo-beta-lactamase, in a tertiary care center in Cali, Colombia. J Clin Microbiol. 2004;42:5094–5101. doi: 10.1128/JCM.42.11.5094-5101.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grattard F, Gaudin OG, Pozzetto B, Ros A, Mbida AD. Genotypic homogeneity of nosocomial Pseudomonas aeruginosa O12 strains demonstrated by analysis of protein profiles, DNA fingerprints and rRNA gene restriction patterns. Eur J Clin Microbiol Infect Dis. 1993;12:57–61. doi: 10.1007/BF01997061. [DOI] [PubMed] [Google Scholar]
- 15.Pitt TL, Livermore DM, Pitcher D, Vatopoulos AC, Legakis NJ. Multiresistant serotype O 12 Pseudomonas aeruginosa: evidence for a common strain in Europe. Epidemiol Infect. 1989;103:565–576. doi: 10.1017/s095026880003096x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stover CK, Pham XQ, Erwin AL, Mizoguchi SD, Warrener P, et al. Complete genome sequence of Pseudomonas aeruginosa PAO1, an opportunistic pathogen. Nature. 2000;406:959–964. doi: 10.1038/35023079. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt KD, Tummler B, Romling U. Comparative genome mapping of Pseudomonas aeruginosa PAO with P. aeruginosa C, which belongs to a major clone in cystic fibrosis patients and aquatic habitats. J Bacteriol. 1996;178:85–93. doi: 10.1128/jb.178.1.85-93.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ernst RK, D'Argenio DA, Ichikawa JK, Bangera MG, Selgrade S, et al. Genome mosaicism is conserved but not unique in Pseudomonas aeruginosa isolates from the airways of young children with cystic fibrosis. Environ Microbiol. 2003;5:1341–1349. doi: 10.1111/j.1462-2920.2003.00518.x. [DOI] [PubMed] [Google Scholar]
- 19.Spencer DH, Kas A, Smith EE, Raymond CK, Sims EH, et al. Whole-genome sequence variation among multiple isolates of Pseudomonas aeruginosa. J Bacteriol. 2003;185:1316–1325. doi: 10.1128/JB.185.4.1316-1325.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He J, Baldini RL, Deziel E, Saucier M, Zhang Q, et al. The broad host range pathogen Pseudomonas aeruginosa strain PA14 carries two pathogenicity islands harboring plant and animal virulence genes. Proc Natl Acad Sci U S A. 2004;101:2530–2535. doi: 10.1073/pnas.0304622101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larbig KD, Christmann A, Johann A, Klockgether J, Hartsch T, et al. Gene islands integrated into tRNA(Gly) genes confer genome diversity on a Pseudomonas aeruginosa clone. J Bacteriol. 2002;184:6665–6680. doi: 10.1128/JB.184.23.6665-6680.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolfgang MC, Kulasekara BR, Liang X, Boyd D, Wu K, et al. Conservation of genome content and virulence determinants among clinical and environmental isolates of Pseudomonas aeruginosa. Proc Natl Acad Sci U S A. 2003;100:8484–8489. doi: 10.1073/pnas.0832438100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spratt BG. Exploring the concept of clonality in bacteria. Methods Mol Biol. 2004;266:323–352. doi: 10.1385/1-59259-763-7:323. [DOI] [PubMed] [Google Scholar]
- 24.Selander RK, Levin BR. Genetic diversity and structure in Escherichia coli populations. Science. 1980;210:545–547. doi: 10.1126/science.6999623. [DOI] [PubMed] [Google Scholar]
- 25.Selander RK, Caugant DA, Ochman H, Musser JM, Gilmour MN, et al. Methods of multilocus enzyme electrophoresis for bacterial population genetics and systematics. Appl Environ Microbiol. 1986;51:873–884. doi: 10.1128/aem.51.5.873-884.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin C, Boyd EF, Quentin R, Massicot P, Selander RK. Enzyme polymorphism in Pseudomonas aeruginosa strains recovered from cystic fibrosis patients in France. Microbiology. 1999;145(Pt 9):2587–2594. doi: 10.1099/00221287-145-9-2587. [DOI] [PubMed] [Google Scholar]
- 27.Musser JM, Bemis DA, Ishikawa H, Selander RK. Clonal diversity and host distribution in Bordetella bronchiseptica. J Bacteriol. 1987;169:2793–2803. doi: 10.1128/jb.169.6.2793-2803.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Musser JM, Kroll JS, Moxon ER, Selander RK. Clonal population structure of encapsulated Haemophilus influenzae. Infect Immun. 1988;56:1837–1845. doi: 10.1128/iai.56.8.1837-1845.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Piffaretti JC, Kressebuch H, Aeschbacher M, Bille J, Bannerman E, et al. Genetic characterization of clones of the bacterium Listeria monocytogenes causing epidemic disease. Proc Natl Acad Sci U S A. 1989;86:3818–3822. doi: 10.1073/pnas.86.10.3818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Selander RK, McKinney RM, Whittam TS, Bibb WF, Brenner DJ, et al. Genetic structure of populations of Legionella pneumophila. J Bacteriol. 1985;163:1021–1037. doi: 10.1128/jb.163.3.1021-1037.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Achtman M, Mercer A, Kusecek B, Pohl A, Heuzenroeder M, et al. Six widespread bacterial clones among Escherichia coli K1 isolates. Infect Immun. 1983;39:315–335. doi: 10.1128/iai.39.1.315-335.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selander RK, Musser JM, Caugant DA, Gilmour MN, Whittam TS. Population genetics of pathogenic bacteria. Microb Pathog. 1987;3:1–7. doi: 10.1016/0882-4010(87)90032-5. [DOI] [PubMed] [Google Scholar]
- 33.Maynard Smith J, Smith NH, O'Rourke M, Spratt BG. How clonal are bacteria? Proc Natl Acad Sci U S A. 1993;90:4384–4388. doi: 10.1073/pnas.90.10.4384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feil EJ, Enright MC. Analyses of clonality and the evolution of bacterial pathogens. Curr Opin Microbiol. 2004;7:308–313. doi: 10.1016/j.mib.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Maiden MC. Multilocus sequence typing of bacteria. Annu Rev Microbiol. 2006;60:561–588. doi: 10.1146/annurev.micro.59.030804.121325. [DOI] [PubMed] [Google Scholar]
- 36.Glupczynski Y, Bogaerts P, Deplano A, Berhin C, Huang TD, et al. Detection and characterization of class A extended-spectrum-beta-lactamase-producing Pseudomonas aeruginosa isolates in Belgian hospitals. J Antimicrob Chemother. 2011;65:866–871. doi: 10.1093/jac/dkq048. [DOI] [PubMed] [Google Scholar]
- 37.Koh TH, Khoo CT, Tan TT, Arshad MA, Ang LP, et al. Multilocus sequence types of carbapenem-resistant Pseudomonas aeruginosa in Singapore carrying metallo-beta-lactamase genes, including the novel bla(IMP-26) gene. J Clin Microbiol. 2010;48:2563–2564. doi: 10.1128/JCM.01905-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kouda S, Ohara M, Onodera M, Fujiue Y, Sasaki M, et al. Increased prevalence and clonal dissemination of multidrug-resistant Pseudomonas aeruginosa with the blaIMP-1 gene cassette in Hiroshima. J Antimicrob Chemother. 2009;64:46–51. doi: 10.1093/jac/dkp142. [DOI] [PubMed] [Google Scholar]
- 39.Nemec A, Krizova L, Maixnerova M, Musilek M. Multidrug-resistant epidemic clones among bloodstream isolates of Pseudomonas aeruginosa in the Czech Republic. Res Microbiol. 2010;161:234–242. doi: 10.1016/j.resmic.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 40.van Mansfeld R, Jongerden I, Bootsma M, Buiting A, Bonten M, et al. The population genetics of Pseudomonas aeruginosa isolates from different patient populations exhibits high-level host specificity. PLoS One. 2010;5:e13482. doi: 10.1371/journal.pone.0013482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Mansfeld R, Willems R, Brimicombe R, Heijerman H, van Berkhout FT, et al. Pseudomonas aeruginosa genotype prevalence in Dutch cystic fibrosis patients and age dependency of colonization by various P. aeruginosa sequence types. J Clin Microbiol. 2009;47:4096–4101. doi: 10.1128/JCM.01462-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Waine DJ, Honeybourne D, Smith EG, Whitehouse JL, Dowson CG. Cross-sectional and longitudinal multilocus sequence typing of Pseudomonas aeruginosa in cystic fibrosis sputum samples. J Clin Microbiol. 2009;47:3444–3448. doi: 10.1128/JCM.00459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Curran B, Jonas D, Grundmann H, Pitt T, Dowson CG. Development of a multilocus sequence typing scheme for the opportunistic pathogen Pseudomonas aeruginosa. J Clin Microbiol. 2004;42:5644–5649. doi: 10.1128/JCM.42.12.5644-5649.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khan NH, Ahsan M, Yoshizawa S, Hosoya S, Yokota A, et al. Multilocus sequence typing and phylogenetic analyses of Pseudomonas aeruginosa Isolates from the ocean. Appl Environ Microbiol. 2008;74:6194–6205. doi: 10.1128/AEM.02322-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Woodford N TJ, Livermore DM. Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiol Rev. 2011;35:736–755. doi: 10.1111/j.1574-6976.2011.00268.x. [DOI] [PubMed] [Google Scholar]
- 46.De Vos D, Lim A, Jr, Pirnay JP, Struelens M, Vandenvelde C, et al. Direct detection and identification of Pseudomonas aeruginosa in clinical samples such as skin biopsy specimens and expectorations by multiplex PCR based on two outer membrane lipoprotein genes, oprI and oprL. J Clin Microbiol. 1997;35:1295–1299. doi: 10.1128/jcm.35.6.1295-1299.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Giske CG, Libisch B, Colinon C, Scoulica E, Pagani L, et al. Establishing clonal relationships between VIM-1-like metallo-beta-lactamase-producing Pseudomonas aeruginosa strains from four European countries by multilocus sequence typing. J Clin Microbiol. 2006;44:4309–4315. doi: 10.1128/JCM.00817-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, et al. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995;33:2233–2239. doi: 10.1128/jcm.33.9.2233-2239.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu PVM, Kusama H, H. Bergan T. Survey of heat-stable, major somatic antigens of Pseudomonas aeruginosa. Int J Syst Bacteriol. 1983;33:256–264. [Google Scholar]
- 50.Feltman H, Schulert G, Khan S, Jain M, Peterson L, et al. Prevalence of type III secretion genes in clinical and environmental isolates of Pseudomonas aeruginosa. Microbiology. 2001;147:2659–2669. doi: 10.1099/00221287-147-10-2659. [DOI] [PubMed] [Google Scholar]
- 51.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2011. [DOI] [PubMed]
- 52.Schouls LM, van der Heide HG, Vauterin L, Vauterin P, Mooi FR. Multiple-locus variable-number tandem repeat analysis of Dutch Bordetella pertussis strains reveals rapid genetic changes with clonal expansion during the late 1990s. J Bacteriol. 2004;186:5496–5505. doi: 10.1128/JB.186.16.5496-5505.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Librado P, Rozas J. DnaSP v5: a software for comprehensive analysis of DNA polymorphism data. Bioinformatics. 2009;25:1451–1452. doi: 10.1093/bioinformatics/btp187. [DOI] [PubMed] [Google Scholar]
- 54.Kumar S, Tamura K, Jakobsen IB, Nei M. MEGA2: molecular evolutionary genetics analysis software. Bioinformatics. 2001;17:1244–1245. doi: 10.1093/bioinformatics/17.12.1244. [DOI] [PubMed] [Google Scholar]
- 55.Feil EJ, Li BC, Aanensen DM, Hanage WP, Spratt BG. eBURST: inferring patterns of evolutionary descent among clusters of related bacterial genotypes from multilocus sequence typing data. J Bacteriol. 2004;186:1518–1530. doi: 10.1128/JB.186.5.1518-1530.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jolley KA, Feil EJ, Chan MS, Maiden MC. Sequence type analysis and recombinational tests (START). Bioinformatics. 2001;17:1230–1231. doi: 10.1093/bioinformatics/17.12.1230. [DOI] [PubMed] [Google Scholar]
- 57.Huson DH, Bryant D. Application of phylogenetic networks in evolutionary studies. Mol Biol Evol. 2006;23:254–267. doi: 10.1093/molbev/msj030. [DOI] [PubMed] [Google Scholar]
- 58.Bruen TC, Philippe H, Bryant D. A simple and robust statistical test for detecting the presence of recombination. Genetics. 2006;172:2665–2681. doi: 10.1534/genetics.105.048975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Didelot X, Falush D. Inference of bacterial microevolution using multilocus sequence data. Genetics. 2007;175:1251–1266. doi: 10.1534/genetics.106.063305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martin DP, Williamson C, Posada D. RDP2: recombination detection and analysis from sequence alignments. Bioinformatics. 2005;21:260–262. doi: 10.1093/bioinformatics/bth490. [DOI] [PubMed] [Google Scholar]
- 61.Lomholt JA, Poulsen K, Kilian M. Epidemic population structure of Pseudomonas aeruginosa: evidence for a clone that is pathogenic to the eye and that has a distinct combination of virulence factors. Infect Immun. 2001;69:6284–6295. doi: 10.1128/IAI.69.10.6284-6295.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kiewitz C, Tummler B. Sequence diversity of Pseudomonas aeruginosa: impact on population structure and genome evolution. J Bacteriol. 2000;182:3125–3135. doi: 10.1128/jb.182.11.3125-3135.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morales G, Wiehlmann L, Gudowius P, van Delden C, Tummler B, et al. Structure of Pseudomonas aeruginosa populations analyzed by single nucleotide polymorphism and pulsed-field gel electrophoresis genotyping. J Bacteriol. 2004;186:4228–4237. doi: 10.1128/JB.186.13.4228-4237.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pirnay JP, Bilocq F, Pot B, Cornelis P, Zizi M, et al. Pseudomonas aeruginosa population structure revisited. PLoS One. 2009;4:e7740. doi: 10.1371/journal.pone.0007740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pirnay JP, De Vos D, Cochez C, Bilocq F, Vanderkelen A, et al. Pseudomonas aeruginosa displays an epidemic population structure. Environ Microbiol. 2002;4:898–911. doi: 10.1046/j.1462-2920.2002.00321.x. [DOI] [PubMed] [Google Scholar]
- 66.Wiehlmann L, Wagner G, Cramer N, Siebert B, Gudowius P, et al. Population structure of Pseudomonas aeruginosa. Proc Natl Acad Sci U S A. 2007;104:8101–8106. doi: 10.1073/pnas.0609213104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Denamur E, Picard B, Decoux G, Denis JB, Elion J. The absence of correlation between allozyme and rrn RFLP analysis indicates a high gene flow rate within human clinical Pseudomonas aeruginosa isolates. FEMS Microbiol Lett. 1993;110:275–280. doi: 10.1111/j.1574-6968.1993.tb06334.x. [DOI] [PubMed] [Google Scholar]
- 68.Picard B, Denamur E, Barakat A, Elion J, Goullet P. Genetic heterogeneity of Pseudomonas aeruginosa clinical isolates revealed by esterase electrophoretic polymorphism and restriction fragment length polymorphism of the ribosomal RNA gene region. J Med Microbiol. 1994;40:313–322. doi: 10.1099/00222615-40-5-313. [DOI] [PubMed] [Google Scholar]
- 69.Fonseca EL, Freitas Fdos S, Vicente AC. The colistin-only-sensitive Brazilian Pseudomonas aeruginosa clone SP (sequence type 277) is spread worldwide. Antimicrob Agents Chemother. 54:2743. doi: 10.1128/AAC.00012-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Posada D. Evaluation of methods for detecting recombination from DNA sequences: empirical data. Mol Biol Evol. 2002;19:708–717. doi: 10.1093/oxfordjournals.molbev.a004129. [DOI] [PubMed] [Google Scholar]
- 71.Stumpf MP, McVean GA. Estimating recombination rates from population-genetic data. Nat Rev Genet. 2003;4:959–968. doi: 10.1038/nrg1227. [DOI] [PubMed] [Google Scholar]
- 72.Spratt BG, Hanage WP, Li B, Aanensen DM, Feil EJ. Displaying the relatedness among isolates of bacterial species -- the eBURST approach. FEMS Microbiol Lett. 2004;241:129–134. doi: 10.1016/j.femsle.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 73.Perez-Losada M, Browne EB, Madsen A, Wirth T, Viscidi RP, et al. Population genetics of microbial pathogens estimated from multilocus sequence typing (MLST) data. Infect Genet Evol. 2006;6:97–112. doi: 10.1016/j.meegid.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mathee K, Narasimhan G, Valdes C, Qiu X, Matewish JM, et al. Dynamics of Pseudomonas aeruginosa genome evolution. Proc Natl Acad Sci U S A. 2008;105:3100–3105. doi: 10.1073/pnas.0711982105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Romling U, Fiedler B, Bosshammer J, Grothues D, Greipel J, et al. Epidemiology of chronic Pseudomonas aeruginosa infections in cystic fibrosis. J Infect Dis. 1994;170:1616–1621. doi: 10.1093/infdis/170.6.1616. [DOI] [PubMed] [Google Scholar]
- 76.Foght JM, Westlake DW, Johnson WM, Ridgway HF. Environmental gasoline-utilizing isolates and clinical isolates of Pseudomonas aeruginosa are taxonomically indistinguishable by chemotaxonomic and molecular techniques. Microbiology. 1996;142(Pt 9):2333–2340. doi: 10.1099/00221287-142-9-2333. [DOI] [PubMed] [Google Scholar]
- 77.Ajayi T, Allmond LR, Sawa T, Wiener-Kronish JP. Single-nucleotide-polymorphism mapping of the Pseudomonas aeruginosa type III secretion toxins for development of a diagnostic multiplex PCR system. J Clin Microbiol. 2003;41:3526–3531. doi: 10.1128/JCM.41.8.3526-3531.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kulasekara BR, Kulasekara HD, Wolfgang MC, Stevens L, Frank DW, et al. Acquisition and evolution of the exoU locus in Pseudomonas aeruginosa. J Bacteriol. 2006;188:4037–4050. doi: 10.1128/JB.02000-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lanotte P, Watt S, Mereghetti L, Dartiguelongue N, Rastegar-Lari A, et al. Genetic features of Pseudomonas aeruginosa isolates from cystic fibrosis patients compared with those of isolates from other origins. J Med Microbiol. 2004;53:73–81. doi: 10.1099/jmm.0.05324-0. [DOI] [PubMed] [Google Scholar]
- 80.Hauser AR, Cobb E, Bodi M, Mariscal D, Valles J, et al. Type III protein secretion is associated with poor clinical outcomes in patients with ventilator-associated pneumonia caused by Pseudomonas aeruginosa. Crit Care Med. 2002;30:521–528. doi: 10.1097/00003246-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 81.Shaver CM, Hauser AR. Relative contributions of Pseudomonas aeruginosa ExoU, ExoS, and ExoT to virulence in the lung. Infect Immun. 2004;72:6969–6977. doi: 10.1128/IAI.72.12.6969-6977.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lee VT, Smith RS, Tummler B, Lory S. Activities of Pseudomonas aeruginosa effectors secreted by the Type III secretion system in vitro and during infection. Infect Immun. 2005;73:1695–1705. doi: 10.1128/IAI.73.3.1695-1705.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Faure K, Shimabukuro D, Ajayi T, Allmond LR, Sawa T, et al. O-antigen serotypes and type III secretory toxins in clinical isolates of Pseudomonas aeruginosa. J Clin Microbiol. 2003;41:2158–2160. doi: 10.1128/JCM.41.5.2158-2160.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Berthelot P, Attree I, Plesiat P, Chabert J, de Bentzmann S, et al. Genotypic and phenotypic analysis of type III secretion system in a cohort of Pseudomonas aeruginosa bacteremia isolates: evidence for a possible association between O serotypes and exo genes. J Infect Dis. 2003;188:512–518. doi: 10.1086/377000. [DOI] [PubMed] [Google Scholar]
- 85.Finck-Barbancon V, Goranson J, Zhu L, Sawa T, Wiener-Kronish JP, et al. ExoU expression by Pseudomonas aeruginosa correlates with acute cytotoxicity and epithelial injury. Mol Microbiol. 1997;25:547–557. doi: 10.1046/j.1365-2958.1997.4891851.x. [DOI] [PubMed] [Google Scholar]
- 86.Brolund A, Haeggman S, Edquist PJ, Gezelius L, Olsson-Liljequist B, et al. The DiversiLab system versus pulsed-field gel electrophoresis: characterisation of extended spectrum beta-lactamase producing Escherichia coli and Klebsiella pneumoniae. J Microbiol Methods. 2010;83:224–230. doi: 10.1016/j.mimet.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 87.Viedma E, Juan C, Acosta J, Zamorano L, Otero JR, et al. Nosocomial spread of colistin-only-sensitive sequence type 235 Pseudomonas aeruginosa isolates producing the extended-spectrum beta-lactamases GES-1 and GES-5 in Spain. Antimicrob Agents Chemother. 2009;53:4930–4933. doi: 10.1128/AAC.00900-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Samuelsen O, Toleman MA, Sundsfjord A, Rydberg J, Leegaard TM, et al. Molecular epidemiology of metallo-beta-lactamase-producing Pseudomonas aeruginosa isolates from Norway and Sweden shows import of international clones and local clonal expansion. Antimicrob Agents Chemother. 2010;54:346–352. doi: 10.1128/AAC.00824-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Libisch B, Watine J, Balogh B, Gacs M, Muzslay M, et al. Molecular typing indicates an important role for two international clonal complexes in dissemination of VIM-producing Pseudomonas aeruginosa clinical isolates in Hungary. Res Microbiol. 2008;159:162–168. doi: 10.1016/j.resmic.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 90.Lepsanovic Z, Libisch B, Tomanovic B, Nonkovici Z, Balogh B, et al. Characterisation of the first VIM metallo-beta-lactamase-producing Pseudomonas aeruginosa clinical isolate in Serbia. Acta Microbiol Immunol Hung. 2008;55:447–454. doi: 10.1556/AMicr.55.2008.4.9. [DOI] [PubMed] [Google Scholar]
- 91.Juan C, Zamorano L, Mena A, Alberti S, Perez JL, et al. Metallo-beta-lactamase-producing Pseudomonas putida as a reservoir of multidrug resistance elements that can be transferred to successful Pseudomonas aeruginosa clones. J Antimicrob Chemother. 2010;65:474–478. doi: 10.1093/jac/dkp491. [DOI] [PubMed] [Google Scholar]
- 92.Johnson JK, Arduino SM, Stine OC, Johnson JA, Harris AD. Multilocus sequence typing compared to pulsed-field gel electrophoresis for molecular typing of Pseudomonas aeruginosa. J Clin Microbiol. 2007;45:3707–3712. doi: 10.1128/JCM.00560-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Empel J, Filczak K, Mrowka A, Hryniewicz W, Livermore DM, et al. Outbreak of Pseudomonas aeruginosa infections with PER-1 extended-spectrum beta-lactamase in Warsaw, Poland: further evidence for an international clonal complex. J Clin Microbiol. 2007;45:2829–2834. doi: 10.1128/JCM.00997-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Duljasz W, Gniadkowski M, Sitter S, Wojna A, Jebelean C. First organisms with acquired metallo-beta-lactamases (IMP-13, IMP-22, and VIM-2) reported in Austria. Antimicrob Agents Chemother. 2009;53:2221–2222. doi: 10.1128/AAC.01573-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cholley P, Thouverez M, Hocquet D, van der Mee-Marquet N, Talon D, et al. The majority of multi-drug resistant Pseudomonas aeruginosa isolates from hospitals in eastern France belongs to a few clonal types. J Clin Microbiol. 2011;49:2578–2583. doi: 10.1128/JCM.00102-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Silva FM, Carmo MS, Silbert S, Gales AC. SPM-1-Producing Pseudomonas aeruginosa: Analysis of the Ancestor Relationship Using Multilocus Sequence Typing, Pulsed-Field Gel Electrophoresis, and Automated Ribotyping. Microb Drug Resist. 2011;17:215–220. doi: 10.1089/mdr.2010.0140. [DOI] [PubMed] [Google Scholar]
- 97.Koh TH, Khoo CT, Tan TT, Arshad MA, Ang LP, et al. Multilocus sequence types of carbapenem-resistant Pseudomonas aeruginosa in Singapore carrying metallo-beta-lactamase genes, including the novel bla(IMP-26) gene. J Clin Microbiol. 2010;48:2563–2564. doi: 10.1128/JCM.01905-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Edalucci E, Spinelli R, Dolzani L, Riccio ML, Dubois V, et al. Acquisition of different carbapenem resistance mechanisms by an epidemic clonal lineage of Pseudomonas aeruginosa. Clin Microbiol Infect. 2008;14:88–90. doi: 10.1111/j.1469-0691.2007.01874.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Neighbor-joining tree constructed using MEGA 4, showing relationships between the concatenated sequences of all P. aeruginosa STs (n = 70). Bootstrap values are indicated at corresponding nodes and STs at end of branches. Bar is 0.002 substitutions per site.
(TIFF)
SplitsTree networks for each individual locus of Pseudomonas aeruginosa housekeeping gene.
(TIFF)
Database displaying the phenotypic and genotypic features of the studied strains: strains, sources, countries, allelic profiles, STs, serotypes, virulence genes, presence of multidrug-resistance, PFGE patterns, PFGE groups, clonal complexes. Representative isolates for PFGE-clusters that were subjected to MLST are highlighted in column 1.
(XLS)