Abstract
Purpose
Recent work has suggested that insulin-like growth factor 1 (IGF-1) gene polymorphisms are genetically linked with high-grade myopia (HM), which is a complex-trait eye disorder in which numerous candidate loci and genes are thought to play a role. We investigated whether the IGF-1 single nucleotide polymorphisms (SNPs) rs6214, rs10860860, and rs2946834 are associated with HM (≤-6.0 diopters [D]) and any myopia (≤-0.5 D) phenotype in Polish families.
Methods
Forty-two multiplex HM Polish families, of whom 127 had HM, participated in the study. All of the family members (n=306) underwent a detailed ophthalmic examination, including axial length measurements. The IGF-1 SNPs rs6214, rs10860860, and rs2946834 were evaluated by PCR-RFLP and direct sequencing methods. Both Family-Based Association Test (FBAT) and family-based Pedigree Disequilibrium Test (PDT) were used to examine the potential association of the IGF-1 SNPs rs6214, rs10860860, and rs2946834 with HM or any myopia. To determine the distribution of the HM-associated SNPs rs6214 and rs10860860, 543 unrelated individuals from the general Polish population were also analyzed.
Results
We found no significant association between the IGF-1 SNPs rs6214, rs10860860, and rs2946834 and HM or any myopia phenotype in Polish HM families. In the general Polish population, the minor allele frequencies of the SNPs rs6214 and rs10860860 did not deviate significantly from the distribution reported for European populations (p=0.629). In the FBAT analysis under the dominant model, the haplotype consisted of T allele of rs10860860, with C allele of rs2946834 of IGF-1 was found less frequently transmitted to HM individuals (p=0.0065), pointing to a nonassociated or protective haplotype.
Conclusions
Our results do not support recent studies reporting an association of the SNPs rs6214, rs10860860, and rs2946834 in the IGF-1 gene with HM and any myopia phenotypes. Further replication studies involving other populations are needed to investigate the possible role of IGF-1 as a potential myopia candidate gene.
Introduction
Myopia affects 25% of the Western world, making this condition the most common eye disorder in the West and constituting a significant public health and economic problem [1,2]. The cost of optical correction to provide clear distinct vision is considerable. Moreover, the development of high-grade myopia (HM; ≤-6.0 diopters [D]) [3] is a significant risk factor for other ocular diseases, including chorioretinal degeneration, glaucoma, retinal detachment, premature cataracts, and finally blindness [4-6]. Consequently, great efforts have been undertaken to identify and understand the mechanisms underlying the development and progression of myopia.
Myopia has a diverse etiology, with both environmental and genetic factors believed to be involved in the condition’s development and progression. The environmental factors implicated in myopia include near work, light exposure, lack of physical activity, diet, a higher level of education, and urbanization [7-10]. However, HM is highly heritable and often appears as familial ocular disorder, where genetic predisposition seems to be a dominant factor of its development and progression [11-13]. Each type of Mendelian inheritance for familial HM has been described [14,15]. To date, several genetic loci for nonsyndromic myopia (MYP) have been mapped, including 12 loci linked to HM: MYP1, chromosome Xq28 (OMIM 310460) [16,17]; MYP2 18p11.31 (OMIM 160700) [18,19]; MYP3 12q21-q23 (OMIM 603221) [20-22]; MYP4 7q36 (OMIM 608367) [23]; MYP5 17q21-q22 (OMIM 608474) [24]; MYP11 4q22-q27 (OMIM 609994) [25]; MYP12 2q37.1 (OMIM 609995) [26]; MYP13 Xq23-q25 (OMIM 300613) [27]; MYP15 10q21.1 (OMIM 612717) [28]; MYP16 5p15.33-p15.2 (OMIM 612554) [29]; MYP18 14q22.1-q24.2 (OMIM 255500) [30], and MYP19 5p15.1-p13.3 (OMIM 613969) [31]. Moreover, two recent independent genome-wide association studies involving large cohorts of refractive error patients identified loci at chromosome 15q14 and 15q25 [32,33].
Candidate gene association studies have revealed several HM susceptibility genes, including: collagen, type I, alpha 1 (COL1A1) [34,35], transforming growth factor, beta 1 (TGFB1) [36,37], transforming growth beta-induced factor (TGIF) [38,39], lumican (LUM) [40,41], hepatocyte growth factor (HGF) [42,43], myocilin (MYOC) [44,45], paired box 6 (PAX6) [46,47], and uromodulin-like 1 (UMODL1) [48]. However, positive results have not been replicated, and inconsistent data have been published. Thus, the causative mutation(s) has not yet been found, suggesting genetic heterogeneity among studied populations.
Recently, Metlapally et al. [49] reported a genetic association between the three single nucleotide polymorphism (SNP)s rs6214, rs10860860, and rs2946834 and familial myopia in a large, international cohort of myopia pedigrees of Caucasian origin, suggesting that insulin-like growth factor 1 (IGF-1) may be a candidate gene for HM. These three SNPs are located within the MYP3 locus (OMIM 603221) mapped to chromosomal region 12q21-q23. This locus was previously reported to be associated with autosomal dominant HM [20,21]. The SNP rs6214 (reference allele G) lies in the 3′-untranslated region (UTR) of IGF-1 (OMIM 147440), whereas the SNPs rs10860860 (reference allele A) and rs2946834 (reference allele C) are located in the noncoding sequence in close proximity to IGF-1.
The IGF-1 gene encodes insulin-like growth factor (pIGF-1), which is a member of the signaling system involved in development, cellular growth, differentiation, protein translation, metabolism, apoptosis, and aging [50,51]. The association of IGF-1 with numerous human diseases, such as diabetes [52], cancer [53], and growth failure [54] has been reported. IGF-1 has been also implicated in ocular diseases, including retinopathy of prematurity [55,56], age-related macular degeneration [57], and diabetic retinopathy [58,59]. However, for IGF-1 to be considered as a candidate gene for HM, previously published findings need to be replicated.
In the present study, we tested the association of rs6214, rs10860860, and rs2946834 in the IGF-1 gene with HM and any myopia phenotype in 42 Polish families. Our findings do not confirm the results reported previously for another myopic Caucasian cohort, however which was different from the Polish population [49]. To our knowledge, this is the first replication study to screen genetic variants in IGF-1, which previous work has suggested may be associated with any myopia and HM phenotypes.
Methods
Subjects
Forty-two multigenerational Polish HM families were enrolled in the study. The subjects were classified into three groups, including: 1) affected individuals (HM), 2) individuals with an unknown status, and 3) unaffected persons. All of the affected individuals had: A) bilateral axial HM in excess of or equal to −6.0 D (≤-6.0 D) in at least one eye and in excess of or equal to −5.0 D (≤-5.0 D) in the second eye, B) a history of onset of myopia at age ≤15 years, and C) a multiplex family with affected relatives in different generations. Individuals who were classified as unknown were: A) all children ≤15 years unless they fulfilled criteria for affected status as specified above, or B) individuals who have myopia with −6.0 D< X ≤-4.0 D, or C) individuals with a refractive error of ≤-6.0 D for one eye and a refractive error >-5.0 D for the second eye, or D) individuals with late age of onset (>15 years). All of the remaining individuals were considered unaffected, including hyperopic, normal seeing, and myopic subjects with a spherical refractive error (SPH) in the range from ≤-0.5 D to >-4.0 D.
The SNPs rs6214, rs10860860, and rs2946834 were examined in 306 subjects, including 127 with HM, 148 unaffected, and 31 individuals with an unknown status. In addition, to determine the distribution of the genotypes possibly associated with HM (rs6214 and rs10860860) [49] in the general Polish population, 543 unrelated white Caucasian individuals were examined. The population samples were collected randomly and anonymously, and the myopia status was not determined [60].
All of the individuals (affected, unaffected, and unknown) who participated in this study underwent a complete ophthalmic assessment, including a visual acuity testing, best-corrected visual acuity testing, a slit lamp evaluation, intraocular pressure examination, fundoscopy, axial length determination, keratometry, and refractometry. The detailed clinical evaluation and pedigrees of Polish HM families have been previously described [61]. The clinical characteristics of all of the individuals examined are shown in brief in Table 1. The SPH was used to assign HM status.
Table 1. Clinical characteristic of genotyped individuals.
| Clinical characteristic | Affected | Unaffected | Unknown | General population group | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of individuals | 127 | 148 | 31 | 543 | ||||||
| Age at Examination (year) | ||||||||||
| Range | 5–87 | 3–86 | 3–81 | 3–83 | ||||||
| Mean age (±SD) | 40.2 (±20.43) | 38.6 (±18.54) | 27.1 (±22.63) | 41.8 (±16.1) | ||||||
| Age of Onset (year) | ||||||||||
| Range | 2–15 | … | … | … | ||||||
| Mean age (±SD) | 8.21 (±3.40) | |||||||||
| Gender | ||||||||||
| Female | 77 (60.6%) | 79 (53.4%) | 13 (41.9%) | 285 (52.5%) | ||||||
| Male | 50 (39.4%) | 69 (46.6%) | 18 (58.1%) | 258 (47.5%) | ||||||
| Spherical Refractive Error [D] | OD | OS | OD+OS | OD | OS | OD+OS | OD | OS | OD+OS | not determined |
| Mean | −9.34 | −9.29 | −9.32 | −0.05 | 0.00 | −0.03 | −2.74 | −2.77 | −2.75 | |
| (±SD) | (±3.95) | (±3.84) | (±3.89) | (±1.24) | (±1.28) | (±1.26) | (±1.95) | (±2.09) | (±2.00) | |
| Cylindrical Refractive Error [D] | OD | OS | OD+OS | OD | OS | OD+OS | OD | OS | OD+OS | not determined |
| Mean | −0.90 | −0.84 | −0.87 | −0.39 | −0.36 | −0.38 | −0.29 | −0.19 | −0.25 | |
| (±SD) | (±1.34) | (±1.15) | (±1.24) | (±0.56) | (±0.65) | (±0.60) | (±0.38) | (±0.46) | (±0.42) | |
| Spherical Equivalent [D] | OD | OS | OD+OS | OD | OS | OD+OS | OD | OS | OD+OS | not determined |
| Mean | −9.72 | −9.63 | −9.69 | −0.26 | −0.17 | −0.22 | −2.88 | −2.87 | −2.87 | |
| (±SD) | (±4.09) | (±3.91) | (±4.00) | (±1.19) | (±1.24) | (±1.21) | (±1.95) | (±2.12) | (±2.00) | |
| Axial Length [mm] | OD | OS | OD+OS | OD | OS | OD+OS | OD | OS | OD+OS | not determined |
| Mean | 27.26 | 27.27 | 27.27 | 23.38 | 23.40 | 23.39 | 24.34 | 23.56 | 23.95 | |
| (±SD) | (±2.09) | (±1.96) | (±2.03) | (±0.79) | (±0.84) | (±0.82) | (±1.16) | (±4.16) | (±3.05) | |
In addition, any myopia phenotype status was established in reference to the criteria published by Metlapally et al. [49], who defined any myopia phenotype as ≤-0.5 D based on SPH. The clinical information data for this category are shown in Appendix 1.
The research protocol was approved by the Institutional Review Board at Poznan University of Medical Sciences in Poland. In accordance with the Declaration of Helsinki, written informed consent was obtained for the genetic studies from all of the participating family members and individuals from the general Polish population group.
Genotyping of IGF-1 SNPs rs6214, rs10860860, and rs2946834
The SNPs rs6214 and rs10860860 were analyzed by PCR-RFLP and direct sequencing methods. Two pairs of primers were used to amplify DNA harboring the analyzed SNPs. The amplicons were digested by the restriction enzymes TaiI and NdeI, respectively, according to the manufacturer’s instructions (Fermentas, Vilnius, Lithuania). The detailed PCR-RFLP protocols used in this study are provided in Appendix 2. In addition, all homozygous rs6214 AA and rs10860860 TT samples were verified by direct sequencing using the BigDye® Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems [ABI], Foster City, CA) and an ABI 3730xl analyzer. The results were analyzed by Sequencher® Software 4.10.1 (Gene Codes Corporation, Ann. Arbor, MI). Due to a lack of a restriction site for SNP rs2946834, we analyzed this polymorphism by direct sequencing as described above. The detailed PCR protocol, as well as the primer sequences, are given in Appendix 2.
All of the primer pairs used in this study were designed with the Primer3 v.0.4.0 tool and synthesized by Genomed Co. (Warsaw, Poland).
Statistical analyses
PEDCHECK version 1.1 [62] was used to determine Mendelian inconsistencies within families. Plink software [63] was used to examine the genotype distribution of the SNPs tested for departures from expectations of the Hardy–Weinberg equilibrium (HWE).
Haploview [64] was used to estimate the linkage disequilibrium (LD) pattern of the analyzed SNPs in the Polish HM families and compare with data pertaining to the CEU population (HapMap Public Release #27).
We tested for an association between the rs6214, rs10860860, and rs2946834 polymorphisms of the IGF-1 gene and HM and any myopia using the Family-Based Association Test (FBAT, version 1.7.2). FBAT is a generalized approach derived from the transmission/disequilibrium test (TDT) [65], which allows the genotype distribution observed in the affected offspring and the expected distribution to be evaluated. The models of inheritance examined by FBAT included the additive, dominant, and recessive models [66,67]. The FBAT analysis was performed based on the compound null hypothesis of no linkage and no association between the phenotype and the genetic variant. To analyze the haplotype using FBAT, 42 multiplex Polish families were divided into 122 nuclear families (two parents and their offspring), and they were tested using a two-stage procedure. First, the SNPs rs6214, rs10860860, and rs2946834 were examined separately. Testing was then undertaken for possible haplotypes of the specific alleles of rs6214, rs10860860, and rs2946834. Analyses in which there were less than ten informative families for a particular marker were excluded from consideration. Unaffected individuals were included in the study to increase the statistical power of the FBAT analysis.
In addition, to verify the FBAT results, the genetic association between the three selected polymorphisms of the IGF-1 gene and HM and any myopia phenotypes were tested using the family-based Pedigree Disequilibrium Test (PDT, version 5.1) [68] as described by Metlapally et al. [49]. The PDT analysis program evaluates evidence of LD in general pedigree data.
Results
The genotype distribution and allele frequencies in affected, unaffected, and individuals with unknown status, as well as in the general Polish population group, are shown in Table 2. All genotypes of examined SNPs were tested for HWE, and no significant deviations were found.
Table 2. Genotype distribution and allele frequency of IGF-1 gene SNPs rs6214, rs10860860, and rs2946834.
| High-grade myopia | Any myopia | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Affected | Unaffected | Unknown | Affected | Unaffected | Unknown | Population group | |||||||||
| SNP | SNP genotype/allele | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| rs6214 | GG | 51 | 40.1 | 54 | 36.5 | 13 | 41.9 | 82 | 39.6 | 27 | 34.6 | 9 | 42.9 | 209 | 38.5 |
| GA | 59 | 46.5 | 78 | 52.7 | 13 | 41.9 | 98 | 47.3 | 43 | 55.1 | 9 | 42.9 | 264 | 48.6 | |
| AA | 17 | 13.4 | 16 | 10.2 | 5 | 16.2 | 27 | 13.1 | 8 | 10.3 | 3 | 14.2 | 70 | 12.9 | |
| G | 161 | 63.4 | 186 | 62.8 | 39 | 62.9 | 262 | 63.3 | 97 | 62.2 | 27 | 64.3 | 682 | 62.8 | |
| A | 93 | 36.6 | 110 | 37.2 | 23 | 37.1 | 152 | 36.7 | 59 | 37.8 | 15 | 35.7 | 404 | 37.2 | |
| rs10860860 | AA | 57 | 44.9 | 60 | 40.5 | 15 | 48.4 | 96 | 46.4 | 23 | 29.5 | 13 | 61.9 | 248 | 45.7 |
| AT | 54 | 42.5 | 75 | 50.7 | 14 | 45.2 | 88 | 42.5 | 48 | 61.5 | 7 | 33.3 | 251 | 46.2 | |
| TT | 16 | 12.6 | 13 | 8.8 | 2 | 6.4 | 23 | 11.1 | 7 | 9.0 | 1 | 4.8 | 44 | 8.1 | |
| A | 168 | 66.1 | 195 | 65.9 | 44 | 71.0 | 280 | 67.6 | 94 | 60.3 | 33 | 78.6 | 747 | 68.8 | |
| T | 86 | 33.9 | 101 | 34.1 | 18 | 29.0 | 134 | 32.4 | 62 | 39.7 | 9 | 21.4 | 339 | 31.2 | |
| rs2946834 | CC | 61 | 48.8 | 72 | 49.0 | 14 | 45.2 | 109 | 53.4 | 29 | 37.2 | 9 | 42.9 | - | - |
| CT | 48 | 38.4 | 61 | 41.5 | 14 | 45.2 | 78 | 38.2 | 37 | 47.4 | 8 | 38.1 | - | - | |
| TT | 16 | 12.8 | 14 | 9.5 | 3 | 9.7 | 17 | 8.3 | 12 | 15.4 | 4 | 19.0 | - | - | |
| C | 170 | 68 | 205 | 69.7 | 42 | 67.7 | 296 | 72.5 | 95 | 60.9 | 26 | 61.9 | - | - | |
| T | 80 | 32 | 89 | 30.3 | 20 | 32.3 | 112 | 27.5 | 61 | 39.1 | 16 | 38.1 | - | - | |
| rs6214/ rs10860860 | GG / AA | 35 | 27.6 | 40 | 27.0 | 9 | 29.0 | 61 | 29.5 | 15 | 19.2 | 8 | 38.1 | 154 | 28.4 |
| GG / AT | 13 | 10.2 | 13 | 8.8 | 4 | 12.9 | 18 | 8.7 | 11 | 14.1 | 1 | 4.8 | 53 | 9.8 | |
| GG / TT | 3 | 2.4 | 1 | 0.7 | 0 | 0.0 | 3 | 1.4 | 1 | 1.3 | 0 | 0 | 2 | 0.4 | |
| GA / AA | 19 | 14.9 | 19 | 12.8 | 5 | 16.1 | 31 | 15.0 | 7 | 9.0 | 5 | 23.8 | 81 | 14.9 | |
| GA / AT | 34 | 26.8 | 55 | 37.2 | 8 | 25.8 | 60 | 29.0 | 33 | 42.3 | 4 | 19.0 | 158 | 29.0 | |
| GA / TT | 6 | 4.7 | 4 | 2.7 | 0 | 0.0 | 7 | 3.4 | 3 | 3.8 | 0 | 0 | 25 | 4.6 | |
| AA / AA | 3 | 2.4 | 1 | 0.7 | 1 | 3.2 | 4 | 1.9 | 1 | 1.3 | 0 | 0 | 13 | 2.4 | |
| AA / AT | 7 | 5.5 | 7 | 4.7 | 2 | 6.5 | 10 | 4.8 | 4 | 5.2 | 2 | 9.5 | 40 | 7.4 | |
| AA / TT | 7 | 5.5 | 8 | 5.4 | 2 | 6.5 | 13 | 6.3 | 3 | 3.8 | 1 | 4.8 | 17 | 3.1 | |
| rs2946834/ rs6214 | CT / GG | 18 | 14.4 | 18 | 12.2 | 6 | 19.4 | 28 | 13.7 | 12 | 15.4 | 2 | 9.5 | - | - |
| CT / GA | 24 | 19.2 | 32 | 21.8 | 7 | 22.6 | 41 | 20.1 | 18 | 23.1 | 4 | 19.0 | - | - | |
| CC / AA | 9 | 7.2 | 5 | 3.4 | 4 | 12.9 | 16 | 7.8 | 1 | 1.3 | 1 | 4.8 | - | - | |
| TT / AA | 2 | 1.6 | 0 | 0.0 | 0 | 0.0 | 2 | 1.0 | 0 | 0.0 | 0 | 0.0 | - | - | |
| CT / AA | 6 | 4.8 | 11 | 7.5 | 1 | 3.2 | 9 | 4.4 | 7 | 9.0 | 2 | 9.5 | - | - | |
| CC / GA | 27 | 21.6 | 37 | 25.2 | 5 | 16.1 | 48 | 23.5 | 18 | 23.1 | 3 | 14.3 | - | - | |
| CC / GG | 25 | 20 | 30 | 20.4 | 5 | 16.1 | 45 | 22.1 | 10 | 12.8 | 5 | 23.8 | - | - | |
| TT / GA | 7 | 5.6 | 9 | 6.1 | 1 | 3.2 | 8 | 3.9 | 7 | 9.0 | 2 | 9.5 | - | - | |
| TT / GG | 7 | 5.6 | 5 | 3.4 | 2 | 6.5 | 7 | 3.4 | 5 | 6.4 | 2 | 9.5 | - | - | |
| rs10860860/ rs2946834 | AT / CT | 29 | 23.2 | 42 | 28.6 | 5 | 16.1 | 43 | 21.1 | 29 | 37.2 | 4 | 19.0 | - | - |
| TT / TT | 8 | 6.4 | 3 | 2.0 | 0 | 0.0 | 8 | 3.9 | 3 | 3.8 | 0 | 0.0 | - | - | |
| TT / CT | 5 | 4 | 7 | 4.8 | 1 | 3.2 | 9 | 4.4 | 4 | 5.1 | 0 | 0.0 | - | - | |
| AT / TT | 7 | 5.6 | 6 | 4.1 | 3 | 9.7 | 8 | 3.9 | 6 | 7.7 | 2 | 9.5 | - | - | |
| AA / CC | 42 | 33.6 | 42 | 28.6 | 7 | 22.6 | 68 | 33.3 | 16 | 20.5 | 7 | 33.3 | - | - | |
| AA / TT | 1 | 0.8 | 5 | 3.4 | 0 | 0.0 | 1 | 0.5 | 3 | 3.8 | 2 | 9.5 | - | - | |
| AA / CT | 14 | 11.2 | 12 | 8.2 | 8 | 25.8 | 26 | 12.7 | 4 | 5.1 | 4 | 19.0 | - | - | |
| AT / CC | 16 | 12.8 | 27 | 18.4 | 6 | 19.4 | 35 | 17.2 | 13 | 16.7 | 1 | 4.8 | - | - | |
| TT / CC | 3 | 2.4 | 3 | 2.0 | 1 | 3.2 | 6 | 2.9 | 0 | 0.0 | 1 | 4.8 | - | - | |
| rs10860860/ rs2946834/ rs6214 | AA / CC / AA | 3 | 2.4 | 1 | 0.7 | 1 | 3.2 | 4 | 2.0 | 1 | 1.3 | 0 | 0.0 | - | - |
| AA / CC / GA | 15 | 12.0 | 13 | 8.8 | 1 | 3.2 | 21 | 10.3 | 6 | 7.7 | 2 | 9.5 | - | - | |
| AA / CC / GG | 24 | 19.2 | 28 | 19.0 | 5 | 16.1 | 43 | 21.1 | 9 | 11.5 | 5 | 23.8 | - | - | |
| AA / CT / GA | 4 | 3.2 | 4 | 2.7 | 4 | 12.9 | 10 | 4.9 | 0 | 0.0 | 2 | 9.5 | - | - | |
| AA / CT / GG | 10 | 8.0 | 8 | 5.4 | 4 | 12.9 | 16 | 7.8 | 4 | 5.1 | 2 | 9.5 | - | - | |
| AA / TT / GA | 0 | 0.0 | 2 | 1.4 | 0 | 0.0 | 0 | 0.0 | 1 | 1.3 | 1 | 4.8 | - | - | |
| AA / TT / GG | 1 | 0.8 | 3 | 2.0 | 0 | 0.0 | 1 | 0.5 | 2 | 2.6 | 1 | 4.8 | - | - | |
| AT / CC / AA | 3 | 2.4 | 1 | 0.7 | 2 | 6.5 | 6 | 2.9 | 0 | 0.0 | 0 | 0.0 | - | - | |
| AT / CC / GA | 12 | 9.6 | 24 | 16.3 | 4 | 12.9 | 27 | 13.2 | 12 | 15.4 | 1 | 4.8 | - | - | |
| AT / CC / GG | 1 | 0.8 | 2 | 1.4 | 0 | 0.0 | 2 | 1.0 | 1 | 1.3 | 0 | 0.0 | - | - | |
| AT / CT / AA | 3 | 2.4 | 6 | 4.1 | 0 | 0.0 | 3 | 1.5 | 4 | 5.1 | 2 | 9.5 | - | - | |
| AT / CT / GA | 18 | 14.4 | 26 | 17.7 | 3 | 9.7 | 28 | 13.7 | 17 | 21.8 | 2 | 9.5 | - | - | |
| AT / CT / GG | 8 | 6.4 | 10 | 6.8 | 2 | 6.5 | 12 | 5.9 | 8 | 10.3 | 0 | 0.0 | - | - | |
| AT / TT / AA | 1 | 0.8 | 0 | 0.0 | 0 | 0.0 | 1 | 0.5 | 0 | 0.0 | 0 | 0.0 | - | - | |
| AT / TT / GA | 3 | 2.4 | 5 | 3.4 | 1 | 3.2 | 4 | 2.0 | 4 | 5.1 | 1 | 4.8 | - | - | |
| AT / TT / GG | 3 | 2.4 | 1 | 0.7 | 2 | 6.5 | 3 | 1.5 | 2 | 2.6 | 1 | 4.8 | - | - | |
| TT / CC / AA | 3 | 2.4 | 3 | 2.0 | 1 | 3.2 | 6 | 2.9 | 0 | 0.0 | 0 | 0.0 | - | - | |
| TT / CT / AA | 3 | 2.4 | 5 | 3.4 | 1 | 3.2 | 6 | 2.9 | 3 | 3.8 | 0 | 0.0 | - | - | |
| TT / CT / GA | 2 | 1.6 | 2 | 1.4 | 0 | 0.0 | 3 | 1.5 | 1 | 1.3 | 0 | 0.0 | - | - | |
| TT / TT / AA | 1 | 0.8 | 0 | 0.0 | 0 | 0.0 | 1 | 0.5 | 0 | 0.0 | 1 | 4.8 | - | - | |
| TT / TT / GA | 4 | 3.2 | 2 | 1.4 | 0 | 0.0 | 4 | 2.0 | 2 | 2.6 | 0 | 0.0 | - | - | |
| TT / TT / GG | 3 | 2.4 | 1 | 0.7 | 0 | 0.0 | 3 | 1.5 | 1 | 1.3 | 0 | 0.0 | - | - | |
The minor allele frequencies estimated for the general Polish population group were 0.372 and 0.312 for rs6214 A and rs10860860 T, respectively. The coexistence of two minor homozygous genotypes of rs6214 AA and rs10860860 TT was observed in 3.1% of individuals (Table 2). In HM families, the minor allele frequencies for the SNPs analyzed were 0.366, 0.339, and 0.320 for rs6214 A, rs10860860 T, and rs2946834 T, respectively, for HM and 0.367, 0.324, and 0.275, respectively, for any myopia phenotype (Table 2). In the HM category, the coexistence of two minor homozygous genotypes of the SNPs rs6214 AA and rs10860860 TT was observed in 5.5% and 5.4% of affected and unaffected subjects, respectively. The coexistence of two minor homozygous genotypes of rs6214 AA and rs2946834 TT was 1.6% and 0%, whereas, the coexistence of rs10860860 TT and rs2946834 TT, was observed in 6.4% of affected and 2.0% of unaffected subjects, respectively (Table 2). The coexistence of three minor genotypes of the SNPs rs6214 AA, rs10860860 TT, and rs2946834 TT analyzed was found in 0.8% of affected individuals and was absent in unaffected subjects (Table 2).
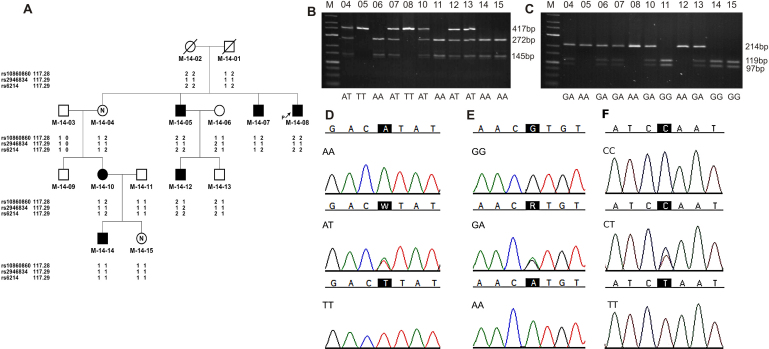
The FBAT and PDT analyses revealed no significant association between the rs6214, rs10860860, and rs2946834 SNPs analyzed and HM, as well as no significant association with any myopia phenotype. The haplotype consisted of alleles T of rs10860860, and alleles C of rs2946834 of IGF-1 was found less frequently in HM individuals than expected (p=0.0065). Table 3 presents the Z scores and p values for the tested IGF-1 polymorphisms and the haplotypes. Moreover, we found a random distribution of genotypes and alleles of the SNPs examined in the Polish HM families (Figure 1 and Appendix 3).
Table 3. Family-based association test analyses (FBAT) and pedigree disequilibrium test (PDT) analyses of the IGF-1 gene SNPs rs6214, rs2946834, and rs10860860.
| High-Grade Myopia | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| FBAT | |||||||||
| additive | dominant | recesive | PDT | ||||||
| SNP | Allele | Z | p | Z | p | Z | p | Z | p |
| rs10860860 | T | −0.781 | 0.434947 | −0.946 | 0.344327 | −0.137 | 0.890758 | −1.068 | 0.2855 |
| A | 0.781 | 0.434947 | 0.137 | 0.890758 | 0.946 | 0.344327 | 1.068 | 0.2855 | |
| rs2946834 | T | 0.899 | 0.368809 | 0.454 | 0.649731 | 1.044 | 0.296272 | 0.697 | 0.4855 |
| C | −0.899 | 0.368809 | −1.044 | 0.296272 | −0.454 | 0.649731 | −0.697 | 0.4855 | |
| rs6214 | A | −0.052 | 0.958800 | 0.234 | 0.815084 | −0.412 | 0.680280 | −0.688 | 0.4913 |
| G | 0.052 | 0.958800 | 0.412 | 0.680280 | −0.234 | 0.815084 | 0.688 | 0.4913 | |
| rs10860860/ rs6214 | AG | −0.347 | 0.728871 | 0.340 | 0.733820 | −0.807 | 0.419469 | - | - |
| TA | −0.964 | 0.335015 | −0.812 | 0.416977 | - | - | - | - | |
| AA | 1.345 | 0.178669 | 1.606 | 0.108337 | - | - | - | - | |
| TG | −0.003 | 0.997942 | 0.308 | 0.758358 | - | - | - | - | |
| rs10860860/ rs2946834 | AC | −0.016 | 0.987072 | −0.886 | 0.375848 | 0.760 | 0.447395 | - | - |
| TT | 0.667 | 0.504478 | 0.695 | 0.487210 | - | - | - | - | |
| TC | −2.331 | 0.019747 | −2.723 | 0.006470 | - | - | - | - | |
| AT | 1.898 | 0.057721 | 1.898 | 0.057721 | - | - | - | - | |
| rs2946834/ rs6214 | CG | −1.472 | 0.141034 | −1.464 | 0.143106 | −0.662 | 0.508095 | - | - |
| CA | −0.364 | 0.715703 | −0.906 | 0.364933 | - | - | - | - | |
| TG | 1.172 | 0.241160 | 1.358 | 0.174527 | - | - | - | - | |
| TA | 1.433 | 0.151778 | 1.433 | 0.151778 | - | - | - | - | |
| rs10860860/ rs2946834/ rs6214 | ACG | −1.467 | 0.142408 | −1.425 | 0.154041 | −0.698 | 0.484867 | - | - |
| TCA | −2.145 | 0.031928 | −2.528 | 0.011472 | - | - | - | - | |
| ACA | 1.743 | 0.081412 | 1.781 | 0.074903 | - | - | - | - | |
| ATG | 1.449 | 0.147280 | 1.449 | 0.147280 | - | - | - | - | |
| TTA | 0.830 | 0.406764 | 0.830 | 0.406764 | - | - | - | - | |
| TTG | 0.438 | 0.661696 | 0.826 | 0.409048 | - | - | - | - | |
| ATA | - | - | - | - | - | - | - | - | |
| TCG | - | - | - | - | - | - | - | - | |
| Any Myopia | |||||||||
| FBAT | |||||||||
| additive | dominant | recesive | PDT | ||||||
| SNP | Allele | Z | p | Z | p | Z | p | Z | p |
| rs10860860 | T | −1.243 | 0.213893 | −0.636 | 0.525020 | −1.423 | 0.154872 | −1.572 | 0.1159 |
| A | 1.243 | 0.213893 | 1.423 | 0.154872 | 0.636 | 0.525020 | 1.572 | 0.1159 | |
| rs2946834 | T | −0.757 | 0.449004 | −0.850 | 0.395113 | −0.199 | 0.842542 | −0.983 | 0.3258 |
| C | 0.757 | 0.449004 | 0.199 | 0.842542 | 0.850 | 0.395113 | 0.983 | 0.3258 | |
| rs6214 | A | −0.346 | 0.729034 | 0.407 | 0.684086 | −1.063 | 0.287596 | −0.567 | 0.5708 |
| G | 0.346 | 0.729034 | 1.063 | 0.287596 | −0.407 | 0.684086 | 0.567 | 0.5708 | |
| rs10860860/ rs6214 | AG | 0.618 | 0.536845 | 1.353 | 0.176003 | −0.393 | 0.694038 | - | - |
| TA | −0.769 | 0.441736 | −0.362 | 0.717451 | - | - | - | - | |
| AA | 0.794 | 0.427175 | 1.252 | 0.210729 | - | - | - | - | |
| TG | −1.093 | 0.274437 | −0.829 | 0.407052 | - | - | - | - | |
| rs10860860/ rs2946834 | AC | 0.801 | 0.423129 | 0.813 | 0.416233 | 0.471 | 0.637682 | - | - |
| TT | −0.737 | 0.460854 | −0.432 | 0.665463 | - | - | - | - | |
| TC | −0.973 | 0.330541 | −1.256 | 0.209270 | - | - | - | - | |
| AT | 1.211 | 0.226036 | 1.405 | 0.160003 | - | - | - | - | |
| rs2946834/ rs6214 | CG | −0.672 | 0.501768 | −0.81 | 0.417700 | −0.201 | 0.840646 | - | - |
| TG | 0.276 | 0.782902 | −0.421 | 0.673876 | - | - | - | - | |
| CA | 0.526 | 0.59913 | 0.88 | 0.379065 | - | - | - | - | |
| TA | 0.1 | 0.920244 | 0.325 | 0.745094 | - | - | - | - | |
| rs10860860/ rs2946834/ rs6214 | ACG | −0.270 | 0.786807 | −0.552 | 0.580836 | 0.162 | 0.871179 | - | - |
| TCA | −0.539 | 0.590146 | −0.902 | 0.367010 | - | - | - | - | |
| ACA | 1.245 | 0.213008 | 1.122 | 0.261914 | - | - | - | - | |
| ATG | 1.027 | 0.304204 | 1.251 | 0.211033 | - | - | - | - | |
| TTA | −0.385 | 0.700077 | −0.179 | 0.857572 | - | - | - | - | |
| TTG | −0.474 | 0.635663 | −0.111 | 0.911560 | - | - | - | - | |
| ATA | - | - | - | - | - | - | - | - | |
| TCG | - | - | - | - | - | - | - | - | |
Figure 1.
Example of genotype distribution of SNPs rs10860860, rs2946834, and rs6214 in the IGF-1 gene. A: Pedigree of HM-14 family. Filled symbols: individuals with high myopia; open symbols: unaffected individuals; symbols with a question mark: individuals with an unknown disease status; an arrow indicates a proband. Detailed clinical findings in family HM-14 are shown in Appendix 3. B: RFLP analysis of SNP rs10860860 and C: RFLP analysis of SNP rs6214. Line M: DNA ladder 25–700 bp, remaining lines: numbers of genotyped individuals according to the pedigree HM-14. Below, genotypes are shown. D: Partial sequence chromatograms showing rs10860860, E: rs6214, and F: rs2946834 genotypes, respectively. Black squares indicate SNP alleles.
The analysis of LD between rs6214, rs2946834, and rs10860860 did not reveal high LD between SNP pairs in the Polish HM families. Moreover, the r2 values for pairs of markers were similar in Polish HM families and the CEU population (p=0.629).
Discussion
Genetic association studies, including case-control and family-base studies, have been widely used to search for genetic factors involved in human diseases, including HM [69,70]. Recently, Metlapally et al. [49] suggested that IGF-1 may be a candidate gene for familial myopia based on a positive association between the SNPs rs6214 and rs10860860 and the HM phenotype and the SNPs rs6214, rs10860860, and rs2946834 and any myopia phenotype.
The SNP rs6214 is considered to be a functional polymorphism due to its location in the 3′-UTR of the IGF-1 gene. The 3′-UTR, a noncoding sequence, contains regulatory motifs crucial for gene expression, mRNA stability, and cellular location of mRNA or the binding of microRNA [71,72]. Previous work has suggested that sequence changes in this region may alter mRNA stability and lead to altered binding activity to microRNAs, which might downregulate gene expression by mRNA cleavage or translational repression [73,74].
The chick model of experimental myopia suggests a possible role for IGF-1 in eye growth and elongation; and therefore, in myopia development and progression. Insulin and IGF-1 injected into chick eyes resulted in an increase in the rate of axial length, ocular elongation, and the anterior chamber depth [75,76]. However, these findings do not entirely correspond with published data for the mammal model, with IGF-1 reported to be a weak factor for mouse lens epithelial cell differentiation and proliferation [77,78].
Cordian et al. [9] stated that myopia may be related to impaired metabolic control. They observed that enhanced scleral growth may result from increased levels of insulin and insulin-like growth hormones. Compared with untreated patients with Laron syndrome (LS), susceptibility to mild myopia has been observed in patients with LS (OMIM 262500) who received treatment with IGF-1. However, there was no difference in axial length between IGF-1 treated LS patients and healthy controls [79].
In the present study, we investigated the previously reported association of the SNPs rs6214, rs10860860, and rs2946834 in the IGF-1 gene with familial HM or any myopia phenotypes. The SNPs selected for the analysis were not in LD in the Polish families; the r2 values for pairs of markers were similar in the CEU population and in the Polish HM families. Simultaneously, we estimated the allele distributions of the selected SNPs (rs6214 and rs10860860) in the general Polish population group. We found no significant differences in minor allele frequencies observed in the general Polish population (rs6214 A and rs10860860 T, 0.372 and 0.312, respectively) and the data provided by HapMap Public Release #28 for CEU: Utah residents with Northern and Western European ancestry from the Centre d”Etude du Polymorphisme Humain (CEPH) collection (rs6214 A and rs10860860 T, 0.425 and 0.350, respectively). In our family-based study, we found no evidence of an association between the SNPs rs6214, rs10860860, and rs2946834 in the IGF-1 gene and any myopia and HM. In contrast to previously published data [49], random distribution of genotypes and alleles were observed in the Polish HM families that we examined. However, the haplotype consisted of allele T of rs10860860, and allele C of rs2946834 of IGF-1 was found less frequently in HM individuals than expected (p=0.0065), pointing to a protective effect of the haplotype. These and other allele haplotypes were not examined in the Metlapally et al. [49] study.
Over the years, various studies have reported associations between numerous nucleotide variants in several genes and HM [30,42,44,80]. However, subsequent studies have failed to confirm and replicate these associations [40,45,81,82]. Possible reasons for the observed discrepancies in the published HM data, especially in relation to complex genetic traits, include (i) ethnic differences, (ii) sample size, (iii) subject misclassification, (iv) power of association analyses, and (v) criteria for statistical significance [83-85].
We analyzed a homogenous ethnic group. All of the participants were Polish, white Caucasian, and of European origin. Metlapally et al. [49] examined IGF-1 polymorphisms in a large cohort of Caucasian HM families, but the subjects were derived from different countries, and the majority of families in their study were from the US (60%). European-Americans are often treated as a homogeneous group; however, due to historical immigration, this cohort is formed of diverse source populations [86].
Unlike the study by Metlapally et al. [49], we employed distinct criteria to determine subjects’ HM status. Metlapally et al. [49] based the HM state on SPH, as well as on spherical equivalent (SE) error of −5.00 D or more in at least one eye. We used more stringent criteria in our study. Subjects were classified as affected based on SPH only and a −6.00 D or more in at least one eye and −5.00 D in the second eye in accordance with HM criteria described elsewhere [3]. In some cases, subjects classified as having an unknown myopia status in our study would be classified as having HM data published by Metlapally et al. [49]. Moreover, in our study, individuals with any myopia who did fulfill the criteria for HM or unknown status were treated as unaffected individuals. Metlapally et al. [49] found a significant association between HM and the SNPs rs6214 and rs10860860, as well as any myopia (including low and medium myopia) and the SNPs rs6214, rs10860860, and rs2946834, out of 13 tested SNPs in IGF-1. Therefore, we performed an additional analysis using the any myopia phenotype criteria described by Metlapally et al. [49]. Again, the FBAT and PDT analyses showed no positive association between the IGF-1 SNPs rs6214, rs10860860, and rs2946834 and any myopia phenotype.
Metlapally et al. [49] defined the statistical significance as p≤0.0038, which is in the range where false-positive results are common [84]. Another study has proposed that p≤5×10−5 or even p≤2×10−7 provides a ratio of a truly positive, reproducible association for candidate genes [87]. Although association studies have identified many putative disease genes, these have often been difficult to confirm. According to Manly [87], irreproducibility might be a consequence of weak statistical power of the original work. Manley’s Better Association for Disease and Gene (BADGE) classification suggests that first-class (p≤2×10−7) and second-class (5×10−6) associations provide some assurance of reproducibility. However, the reliability of second-class associations depends on assumptions. As these criteria are not fulfilled in the Metlapally et al. [49] study, theoretically, their results will be difficult to replicate in subsequent studies. It is possible that the use of more stringent statistic criteria for positive genetic association [88,89] might yield different study findings.
In conclusion, our study revealed no evidence to support the previously reported genetic association of the IGF-1 gene polymorphisms rs6214, rs10860860, and rs2946834 with HM and any myopia phenotypes in Polish families.
Acknowledgments
This work was supported by The Polish Ministry of Science and Higher Education Grant 2 P05A 095 29. Sequencing was in part supported by DNA Sequencing and Oligonucleotides Synthesis Laboratory (oligo.pl) of the Institute of Biochemistry and Biophysics PAS: MiniGrant G28.
Appendix
Appendix 1. Clinical information data for any myopia state. To access the data, click or select the words “Appendix 1.” This will initiate the download of a compressed (pdf) archive that contains the file.
Appendix 2. The PCR and PCR-RFLP conditions for SNPs rs6214, rs10860860, and rs2946834 analyses. *The SNP rs2946834 genotypes were determined by direct sequencing. Due to a lack of a restriction site for rs2946834, the PCR-RFLP assay was not performed. To access the data, click or select the words “Appendix 2.” This will initiate the download of a compressed (pdf) archive that contains the file.
Appendix 3. Detailed clinical findings in family HM-14. *SPH- spherical refractive error, †CYL - cylindrical refractive error. To access the data, click or select the words “Appendix 3.” This will initiate the download of a compressed (pdf) archive that contains the file.
References
- 1.Pararajasegaram R. VISION 2020-the right to sight: from strategies to action. Am J Ophthalmol. 1999;128:359–60. doi: 10.1016/s0002-9394(99)00251-2. [DOI] [PubMed] [Google Scholar]
- 2.Vitale S, Cotch MF, Sperduto R, Ellwein L. Costs of refractive correction of distance vision impairment in the United States, 1999–2002. Ophthalmology. 2006;113:2163–70. doi: 10.1016/j.ophtha.2006.06.033. [DOI] [PubMed] [Google Scholar]
- 3.Cline D, Hofstetter HW, Griffin JR. Dictionary of Visual Science. 4th ed. Boston: Butterworth-Heinemann; 1997. [Google Scholar]
- 4.Burton TC. The influence of refractive error and lattice degeneration on the incidence of retinal detachment. Trans Am Ophthalmol Soc. 1989;87:143–55. [PMC free article] [PubMed] [Google Scholar]
- 5.Brown NA, Hill AR. Cataract: the relation between myopia and cataract morphology. Br J Ophthalmol. 1987;71:405–14. doi: 10.1136/bjo.71.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106:2010–5. doi: 10.1016/s0161-6420(99)90416-5. [DOI] [PubMed] [Google Scholar]
- 7.Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children's refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40. [PubMed] [Google Scholar]
- 8.Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–32. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cordain L, Eaton SB, Brand MJ, Lindeberg S, Jensen C. An evolutionary analysis of the aetiology and pathogenesis of juvenile-onset myopia. Acta Ophthalmol Scand. 2002;80:125–35. doi: 10.1034/j.1600-0420.2002.800203.x. [DOI] [PubMed] [Google Scholar]
- 10.Czepita D, Goslawski W, Mojsa A, Muszyñska-Lachota I. Role of light emitted by incandescent or fluorescent lamps in the development of myopia and astigmatism. Med Sci Monit. 2004;10:168–71. [PubMed] [Google Scholar]
- 11.Hammond CJ, Snieder H, Gilbert CE, Spector TD. Genes and environment in refractive error: the twin eye study. Invest Ophthalmol Vis Sci. 2001;42:1232–6. [PubMed] [Google Scholar]
- 12.Dirani M, Chamberlain M, Shekar SN, Islam AF, Garoufalis P, Chen CY, Guymer RH, Baird PN. Heritability of refractive error and ocular biometrics: the Genes in Myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2006;47:4756–61. doi: 10.1167/iovs.06-0270. [DOI] [PubMed] [Google Scholar]
- 13.Liang CL, Yen E, Su JY, Liu C, Chang TY, Park N, Wu MJ, Lee S, Flynn JT, Juo SH. Impact of family history of high myopia on level and onset of myopia. Invest Ophthalmol Vis Sci. 2004;45:3446–52. doi: 10.1167/iovs.03-1058. [DOI] [PubMed] [Google Scholar]
- 14.Sorsby A, Benjamin B. Modes of inheritance of errors of refraction. J Med Genet. 1973;10:161–4. doi: 10.1136/jmg.10.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Young TL, Metlapally R, Shay AE. Complex trait genetics of refractive error. Arch Ophthalmol. 2007;125:38–48. doi: 10.1001/archopht.125.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz M, Haim M, Skarsholm D. X-linked myopia: Bornholm eye disease–linkage to DNA markers on the distal part of Xq. Clin Genet. 1990;38:281–6. [PubMed] [Google Scholar]
- 17.Young TL, Deeb SS, Ronan SM, Dewan AT, Alvear AB, Scavello GS, Paluru PC, Brott MS, Hayashi T, Holleschau AM, Benegas N, Schwartz M, Atwood LD, Oetting WS, Rosenberg T, Motulsky AG, King RA. X-linked high myopia associated with cone dysfunction. Arch Ophthalmol. 2004;122:897–908. doi: 10.1001/archopht.122.6.897. [DOI] [PubMed] [Google Scholar]
- 18.Young TL, Ronan SM, Drahozal LA, Wildenberg SC, Alvear AB, Oetting WS, Atwood LD, Wilkin DJ, King RA. Evidence that a locus for familial high myopia maps to chromosome 18p. Am J Hum Genet. 1998;63:109–19. doi: 10.1086/301907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lam DS, Tam PO, Fan DS, Baum L, Leung YF, Pang CP. Familial high myopia linkage to chromosome 18p. Ophthalmologica. 2003;217:115–8. doi: 10.1159/000068554. [DOI] [PubMed] [Google Scholar]
- 20.Young TL, Ronan SM, Alvear AB, Wildenberg SC, Oetting WS, Atwood LD, Wilkin DJ, King RA. A second locus for familial high myopia maps to chromosome 12q. Am J Hum Genet. 1998;63:1419–24. doi: 10.1086/302111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nürnberg G, Jacobi FK, Broghammer M, Becker C, Blin N, Nürnberg P, Stephani U, Pusch CM. Refinement of the MYP3 locus on human chromosome 12 in a German family with Mendelian autosomal dominant high-grade myopia by SNP array mapping. Int J Mol Med. 2008;21:429–38. [PubMed] [Google Scholar]
- 22.Farbrother JE, Kirov G, Owen MJ, Pong-Wong R, Haley CS, Guggenheim JA. Linkage analysis of the genetic loci for high myopia on 18p, 12q, and 17q in 51 U.K. families. Invest Ophthalmol Vis Sci. 2004;45:2879–85. doi: 10.1167/iovs.03-1156. [DOI] [PubMed] [Google Scholar]
- 23.Naiglin L, Gazagne C, Dallongeville F, Thalamas C, Idder A, Rascol O, Malecaze F, Calvas P. A genome wide scan for familial high myopia suggests a novel locus on chromosome 7q36. J Med Genet. 2002;39:118–24. doi: 10.1136/jmg.39.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paluru P, Ronan SM, Heon E, Devoto M, Wildenberg SC, Scavello G, Holleschau A, Mäkitie O, Cole WG, King RA, Young TL. New locus for autosomal dominant high myopia maps to the long arm of chromosome 17. Invest Ophthalmol Vis Sci. 2003;44:1830–6. doi: 10.1167/iovs.02-0697. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Q, Guo X, Xiao X, Jia X, Li S, Hejtmancik JF. A new locus for autosomal dominant high myopia maps to 4q22-q27 between D4S1578 and D4S1612. Mol Vis. 2005;11:554–60. [PubMed] [Google Scholar]
- 26.Paluru PC, Nallasamy S, Devoto M, Rappaport EF, Young TL. Identification of a novel locus on 2q for autosomal dominant high-grade myopia. Invest Ophthalmol Vis Sci. 2005;46:2300–7. doi: 10.1167/iovs.04-1423. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Q, Guo X, Xiao X, Jia X, Li S, Hejtmancik JF. Novel locus for X linked recessive high myopia maps to Xq23-q25 but outside MYP1. J Med Genet. 2006;43:e20. doi: 10.1136/jmg.2005.037853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nallasamy S, Paluru PC, Devoto M, Wasserman NF, Zhou J, Young TL. Genetic linkage study of high-grade myopia in a Hutterite population from South Dakota. Mol Vis. 2007;13:229–36. [PMC free article] [PubMed] [Google Scholar]
- 29.Lam CY, Tam PO, Fan DS, Fan BJ, Wang DY, Lee CW, Pang CP, Lam DS. A genome-wide scan maps a novel high myopia locus to 5p15. Invest Ophthalmol Vis Sci. 2008;49:3768–78. doi: 10.1167/iovs.07-1126. [DOI] [PubMed] [Google Scholar]
- 30.Yang Z, Xiao X, Li S, Zhan Q. Clinical and linkage study on a consanguineous Chinese family with autosomal recessive high myopia. Mol Vis. 2009;15:312–8. [PMC free article] [PubMed] [Google Scholar]
- 31.Ma JH, Shen SH, Zhang GW, Zhao DS, Xu C, Pan CM, Jiang H, Wang ZQ, Song HD. Identification of a locus for autosomal dominant high myopia on chromosome 5p13.3-p15.1 in a Chinese family. Mol Vis. 2010;16:2043–54. [PMC free article] [PubMed] [Google Scholar]
- 32.Solouki AM, Verhoeven VJ, van Duijn CM, Verkerk AJ, Ikram MK, Hysi PG, Despriet DD, van Koolwijk LM, Ho L, Ramdas WD, Czudowska M, Kuijpers RW, Amin N, Struchalin M, Aulchenko YS, van Rij G, Riemslag FC, Young TL, Mackey DA, Spector TD, Gorgels TG, Willemse-Assink JJ, Isaacs A, Kramer R, Swagemakers SM, Bergen AA, van Oosterhout AA, Oostra BA, Rivadeneira F, Uitterlinden AG, Hofman A, de Jong PT, Hammond CJ, Vingerling JR, Klaver CC. A genome-wide association study identifies a susceptibility locus for refractive errors and myopia at 15q14. Nat Genet. 2010;42:897–901. doi: 10.1038/ng.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hysi PG, Young TL, Mackey DA, Andrew T, Fernández-Medarde A, Solouki AM, Hewitt AW, Macgregor S, Vingerling JR, Li YJ, Ikram MK, Fai LY, Sham PC, Manyes L, Porteros A, Lopes MC, Carbonaro F, Fahy SJ, Martin NG, van Duijn CM, Spector TD, Rahi JS, Santos E, Klaver CC, Hammond CJ. A genome-wide association study for myopia and refractive error identifies a susceptibility locus at 15q25. Nat Genet. 2010;42:902–5. doi: 10.1038/ng.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Inamori Y, Ota M, Inoko H, Okada E, Nishizaki R, Shiota T, Mok J, Oka A, Ohno S, Mizuki N. The COL1A1 gene and high myopia susceptibility in Japanese. Hum Genet. 2007;122:151–7. doi: 10.1007/s00439-007-0388-1. [DOI] [PubMed] [Google Scholar]
- 35.Metlapally R, Li YJ, Tran-Viet KN, Abbott D, Czaja GR, Malecaze F, Calvas P, Mackey D, Rosenberg T, Paget S, Zayats T, Owen MJ, Guggenheim JA, Young TL. COL1A1 and COL2A1 genes and myopia susceptibility: evidence of association and suggestive linkage to the COL2A1 locus. Invest Ophthalmol Vis Sci. 2009;50:4080–6. doi: 10.1167/iovs.08-3346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hayashi T, Inoko H, Nishizaki R, Ohno S, Mizuki N. Exclusion of transforming growth factor-beta1 as a candidate gene for myopia in the Japanese. Jpn J Ophthalmol. 2007;51:96–9. doi: 10.1007/s10384-006-0417-y. [DOI] [PubMed] [Google Scholar]
- 37.Zha Y, Leung KH, Lo KK, Fung WY, Ng PW, Shi MG, Yap MK, Yip SP. TGFB1 as a susceptibility gene for high myopia: a replication study with new findings. Arch Ophthalmol. 2009;127:541–8. doi: 10.1001/archophthalmol.2008.623. [DOI] [PubMed] [Google Scholar]
- 38.Scavello GS, Paluru PC, Ganter WR, Young TL. Sequence variants in the transforming growth beta-induced factor (TGIF) gene are not associated with high myopia. Invest Ophthalmol Vis Sci. 2004;45:2091–7. doi: 10.1167/iovs.03-0933. [DOI] [PubMed] [Google Scholar]
- 39.Pertile KK, Schäche M, Islam FM, Chen CY, Dirani M, Mitchell P, Baird PN. Assessment of TGIF as a candidate gene for myopia. Invest Ophthalmol Vis Sci. 2008;49:49–54. doi: 10.1167/iovs.07-0896. [DOI] [PubMed] [Google Scholar]
- 40.Wang P, Li S, Xiao X, Jia X, Jiao X, Guo X, Zhang Q. High myopia is not associated with the SNPs in the TGIF, lumican, TGFB1, and HGF genes. Invest Ophthalmol Vis Sci. 2009;50:1546–51. doi: 10.1167/iovs.08-2537. [DOI] [PubMed] [Google Scholar]
- 41.Lin HJ, Wan L, Tsai Y, Chen WC, Tsai SW, Tsai FJ. The association between lumican gene polymorphisms and high myopia. Eye (Lond) 2010;24:1093–101. doi: 10.1038/eye.2009.254. [DOI] [PubMed] [Google Scholar]
- 42.Han W, Yap MK, Wang J, Yip SP. Family-based association analysis of hepatocyte growth factor (HGF) gene polymorphisms in high myopia. Invest Ophthalmol Vis Sci. 2006;47:2291–9. doi: 10.1167/iovs.05-1344. [DOI] [PubMed] [Google Scholar]
- 43.Yanovitch T, Li YJ, Metlapally R, Abbott D, Viet KN, Young TL. Hepatocyte growth factor and myopia: genetic association analyses in a Caucasian population. Mol Vis. 2009;15:1028–35. [PMC free article] [PubMed] [Google Scholar]
- 44.Tang WC, Yip SP, Lo KK, Ng PW, Choi PS, Lee SY, Yap MK. Linkage and association of myocilin (MYOC) polymorphisms with high myopia in a Chinese population. Mol Vis. 2007;13:534–44. [PMC free article] [PubMed] [Google Scholar]
- 45.Zayats T, Yanovitch T, Creer RC, McMahon G, Li YJ, Young TL, Guggenheim JA. Myocilin polymorphisms and high myopia in subjects of European origin. Mol Vis. 2009;15:213–22. [PMC free article] [PubMed] [Google Scholar]
- 46.Hewitt AW, Kearns LS, Jamieson RV, Williamson KA, van Heyningen V, Mackey DA. PAX6 mutations may be associated with high myopia. Ophthalmic Genet. 2007;28:179–82. doi: 10.1080/13816810701356676. [DOI] [PubMed] [Google Scholar]
- 47.Ng TK, Lam CY, Lam DS, Chiang SW, Tam PO, Wang DY, Fan BJ, Yam GH, Fan DS, Pang CP. AC and AG dinucleotide repeats in the PAX6 P1 promoter are associated with high myopia. Mol Vis. 2009;15:2239–48. [PMC free article] [PubMed] [Google Scholar]
- 48.Nishizaki R, Ota M, Inoko H, Meguro A, Shiota T, Okada E, Mok J, Oka A, Ohno S, Mizuki N. New susceptibility locus for high myopia is linked to the uromodulin-like 1 (UMODL1) gene region on chromosome 21q22.3. Eye (Lond) 2009;23:222–9. doi: 10.1038/eye.2008.152. [DOI] [PubMed] [Google Scholar]
- 49.Metlapally R, Ki CS, Li YJ, Tran-Viet KN, Abbott D, Malecaze F, Calvas P, Mackey DA, Rosenberg T, Paget S, Guggenheim JA, Young TL. Genetic association of insulin-like growth factor-1 polymorphisms with high-grade myopia in an international family cohort. Invest Ophthalmol Vis Sci. 2010;51:4476–9. doi: 10.1167/iovs.09-4912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Werner H, Leroith D. New concepts in regulation and function of the insulin-like growth factors: implications for understanding normal growth and neoplasia. Cell Mol Life Sci. 2000;57:932–42. doi: 10.1007/PL00000735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bartke A. The somatotropic axis and aging: Mechanisms and persistent questions about practical implications. Exp Gerontol. 2009;44:372–4. doi: 10.1016/j.exger.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dunger DB, Ong KK, Sandhu MS. Serum insulin-like growth factor-I levels and potential risk of type 2 diabetes. Horm Res. 2003;60:131–5. doi: 10.1159/000074514. [DOI] [PubMed] [Google Scholar]
- 53.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–28. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 54.Netchine I, Azzi S, Houang M, Seurin D, Perin L, Ricort JM, Daubas C, Legay C, Mester J, Herich R, Godeau F, Le Bouc Y. Partial primary deficiency of insulin-like growth factor (IGF)-I activity associated with IGF1 mutation demonstrates its critical role in growth and brain development. J Clin Endocrinol Metab. 2009;94:3913–21. doi: 10.1210/jc.2009-0452. [DOI] [PubMed] [Google Scholar]
- 55.Hellström A, Engström E, Hard AL, Albertsson-Wikland K, Carlsson B, Niklasson A, Löfqvist C, Svensson E, Holm S, Ewald U, Holmström G, Smith LE. Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth. Pediatrics. 2003;112:1016–20. doi: 10.1542/peds.112.5.1016. [DOI] [PubMed] [Google Scholar]
- 56.Pérez-Muñuzuri A, Fernández-Lorenzo JR, Couce-Pico ML, Blanco-Teijeiro MJ, Fraga-Bermúdez JM. Serum levels of IGF1 are a useful predictor of retinopathy of prematurity. Acta Paediatr. 2010;99:519–25. doi: 10.1111/j.1651-2227.2009.01677.x. [DOI] [PubMed] [Google Scholar]
- 57.Rosenthal R, Wohlleben H, Malek G, Schlichting L, Thieme H, Bowes Rickman C, Strauss O. Insulin-like growth factor-1 contributes to neovascularization in age-related macular degeneration. Biochem Biophys Res Commun. 2004;323:1203–8. doi: 10.1016/j.bbrc.2004.08.219. [DOI] [PubMed] [Google Scholar]
- 58.Bergman PB, Moravski CJ, Edmondson SR, Russo VC, Bach LA, Wilkinson-Berka JL, Werther GA. Expression of the IGF system in normal and diabetic transgenic (mRen-2)27 rat eye. Invest Ophthalmol Vis Sci. 2005;46:2708–15. doi: 10.1167/iovs.04-0921. [DOI] [PubMed] [Google Scholar]
- 59.Wilkinson-Berka JL, Wraight C, Werther G. The role of growth hormone, insulin-like growth factor and somatostatin in diabetic retinopathy. Curr Med Chem. 2006;13:3307–17. doi: 10.2174/092986706778773086. [DOI] [PubMed] [Google Scholar]
- 60.Rydzanicz M, Wróbel M, Cywińska K, Froehlich D, Gawecki W, Szyfter W, Szyfter K. Screening of the general Polish population for deafness-associated mutations in mitochondrial 12S rRNA and tRNA Ser(UCN) genes. Genet Test Mol Biomarkers. 2009;13:167–72. doi: 10.1089/gtmb.2008.0098. [DOI] [PubMed] [Google Scholar]
- 61.Rydzanicz M, Nath SK, Sun C, Podfigurna-Musielak M, Frajdenberg A, Mrugacz M, Winters D, Ratnamala U, Radhakrishna U, Bejjani BA, Gajecka M. Identification of novel suggestive loci for high-grade myopia in Polish families. Mol Vis. 2011;17:2028–39. [PMC free article] [PubMed] [Google Scholar]
- 62.O'Connell JR, Weeks DE. PedCheck: a program for identification of genotype incompatibilities in linkage analysis. Am J Hum Genet. 1998;63:259–66. doi: 10.1086/301904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81:559–75. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–5. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 65.Spielman RS, Ewens WJ. The TDT and other family-based tests for linkage disequilibrium and association. Am J Hum Genet. 1996;59:983–9. [PMC free article] [PubMed] [Google Scholar]
- 66.Laird NM, Horvath S, Xu X. Implementing a unified approach to family-based tests of association. Genet Epidemiol. 2000;19:S36–42. doi: 10.1002/1098-2272(2000)19:1+<::AID-GEPI6>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 67.Rabinowitz D, Laird N. A unified approach to adjusting association tests for population admixture with arbitrary pedigree structure and arbitrary missing marker information. Hum Hered. 2000;50:211–23. doi: 10.1159/000022918. [DOI] [PubMed] [Google Scholar]
- 68.Martin ER, Monks SA, Warren LL, Kaplan NL. A test for linkage and association in general pedigrees: the pedigree disequilibrium test. Am J Hum Genet. 2000;67:146–54. doi: 10.1086/302957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tang WC, Yap MK, Yip SP. A review of current approaches to identifying human genes involved in myopia. Clin Exp Optom. 2008;91:4–22. doi: 10.1111/j.1444-0938.2007.00181.x. [DOI] [PubMed] [Google Scholar]
- 70.Hornbeak DM, Young TL. Myopia genetics: a review of current research and emerging trends. Curr Opin Ophthalmol. 2009;20:356–62. doi: 10.1097/ICU.0b013e32832f8040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mazumder B, Seshadri V, Fox PL. Translational control by the 3?-UTR: the ends specify the means. Trends Biochem Sci. 2003;28:91–8. doi: 10.1016/S0968-0004(03)00002-1. [DOI] [PubMed] [Google Scholar]
- 72.Lee EK, Gorospe M. Minireview: posttranscriptional regulation of the insulin and insulin-like growth factor systems. Endocrinology. 2010;151:1403–8. doi: 10.1210/en.2009-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–97. doi: 10.1016/s0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 74.Chen JM, Férec C, Cooper DN. A systematic analysis of disease-associated variants in the 3′ regulatory regions of human protein-coding genes I: general principles and overview. Hum Genet. 2006;120:1–21. doi: 10.1007/s00439-006-0180-7. [DOI] [PubMed] [Google Scholar]
- 75.Zhu X, Wallman J. Opposite effects of glucagon and insulin on compensation for spectacle lenses in chicks. Invest Ophthalmol Vis Sci. 2009;50:24–36. doi: 10.1167/iovs.08-1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Feldkaemper MP, Neacsu I, Schaeffel F. Insulin acts as a powerful stimulator of axial myopia in chicks. Invest Ophthalmol Vis Sci. 2009;50:13–23. doi: 10.1167/iovs.08-1702. [DOI] [PubMed] [Google Scholar]
- 77.Shirke S, Faber SC, Hallem E, Makarenkova HP, Robinson ML, Overbeek PA, Lang RA. Misexpression of IGF-I in the mouse lens expands the transitional zone and perturbs lens polarization. Mech Dev. 2001;101:167–74. doi: 10.1016/s0925-4773(00)00584-0. [DOI] [PubMed] [Google Scholar]
- 78.Xie L, Chen H, Overbeek PA, Reneker LW. Elevated insulin signaling disrupts the growth and differentiation pattern of the mouse lens. Mol Vis. 2007;13:397–407. [PMC free article] [PubMed] [Google Scholar]
- 79.Bourla DH, Laron Z, Snir M, Lilos P, Weinberger D, Axer-Siegel R. Insulinlike growth factor I affects ocular development: a study of untreated and treated patients with Laron syndrome. Ophthalmology. 2006;113:1197.e1–5. doi: 10.1016/j.ophtha.2005.12.023. [DOI] [PubMed] [Google Scholar]
- 80.Lam DS, Lee WS, Leung YF, Tam PO, Fan DS, Fan BJ, Pang CP. TGFbeta-induced factor: a candidate gene for high myopia. Invest Ophthalmol Vis Sci. 2003;44:1012–5. doi: 10.1167/iovs.02-0058. [DOI] [PubMed] [Google Scholar]
- 81.Nakanishi H, Yamada R, Gotoh N, Hayashi H, Otani A, Tsujikawa A, Yamashiro K, Shimada N, Ohno-Matsui K, Mochizuki M, Saito M, Saito K, Iida T, Matsuda F, Yoshimura N. Absence of association between COL1A1 polymorphisms and high myopia in the Japanese population. Invest Ophthalmol Vis Sci. 2009;50:544–50. doi: 10.1167/iovs.08-2425. [DOI] [PubMed] [Google Scholar]
- 82.Hayashi T, Inoko H, Nishizaki R, Ohno S, Mizuki N. Exclusion of transforming growth factor-beta1 as a candidate gene for myopia in the Japanese. Jpn J Ophthalmol. 2007;51:96–9. doi: 10.1007/s10384-006-0417-y. [DOI] [PubMed] [Google Scholar]
- 83.Colhoun HM, McKeigue PM, Davey Smith G. Problems of reporting genetic associations with complex outcomes. Lancet. 2003;361:865–72. doi: 10.1016/s0140-6736(03)12715-8. [DOI] [PubMed] [Google Scholar]
- 84.Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Newton-Cheh C, Hirschhorn JN. Genetic association studies of complex traits: design and analysis issues. Mutat Res. 2005;573:54–69. doi: 10.1016/j.mrfmmm.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 86.Price AL, Butler J, Patterson N, Capelli C, Pascali VL, Scarnicci F, Ruiz-Linares A, Groop L, Saetta AA, Korkolopoulou P, Seligsohn U, Waliszewska A, Schirmer C, Ardlie K, Ramos A, Nemesh J, Arbeitman L, Goldstein DB, Reich D, Hirschhorn JN. Discerning the ancestry of European Americans in genetic association studies. PLoS Genet. 2008;4:e236. doi: 10.1371/journal.pgen.0030236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Manly KF. Reliability of statistical associations between genes and disease. Immunogenetics. 2005;57:549–58. doi: 10.1007/s00251-005-0025-x. [DOI] [PubMed] [Google Scholar]
- 88.Dahlman I, Eaves IA, Kosoy R, Morrison VA, Heward J, Gough SC, Allahabadia A, Franklyn JA, Tuomilehto J, Tuomilehto-Wolf E, Cucca F, Guja C, Ionescu-Tirgoviste C, Stevens H, Carr P, Nutland S, McKinney P, Shield JP, Wang W, Cordell HJ, Walker N, Todd JA, Concannon P. Parameters for reliable results in genetic association studies in common disease. Nat Genet. 2002;30:149–50. doi: 10.1038/ng825. [DOI] [PubMed] [Google Scholar]
- 89.Hirschhorn JN, Daly MJ. Genome-wide association studies for common diseases and complex traits. Nat Rev Genet. 2005;6:95–108. doi: 10.1038/nrg1521. [DOI] [PubMed] [Google Scholar]