Abstract
Objectives
Dignity Therapy is a unique, individualized, brief psychotherapy, developed for patients (and their families) living with life threatening or life limiting illness. The purpose of this study was to determine if Dignity Therapy could mitigate distress and/or bolster end-of-life experience for patients nearing death.
Trial Design
Multi-site randomized controlled trial, with patients assigned to Dignity Therapy, Client Centred Care or Standard Palliative Care. Study arm assignment was based on a computer-generated table of random numbers. Blinding was achieved using opaque sealed envelopes, containing allocations that were only opened once consent had been obtained.
Participants
Patients receiving hospital or community (hospice or home) based palliative care, in Winnipeg, New York, or Perth, randomly assigned to, Dignity Therapy [n=108], Client Centered Care [n=107] and Standard Palliative Care (n=111).
Main Outcome Measures
The primary outcome measures included the FACIT Spiritual Well-Being Scale, the Patient Dignity Inventory, the Hospital Anxiety and Depression Scale; items from the Structured Interview for Symptoms and Concerns, the Quality of Life Scale and a modified Edmonton Symptom Assessment Scale. Mean changes between baseline and end of intervention ratings were determined. Secondary outcomes, examining self-report end-of-life experience, consisted of a post-study survey administered across all study arms.
Intervention
Dignity Therapy, a novel, brief psychotherapy, provides patients with life threatening and life limiting illnesses an opportunity to speak about things that matter most to them. These recorded conversations form the basis of a generativity document, which patients can bequeath to individuals of their choosing. Client Centred Care is a supportive psychotherapeutic approach, in which research nurse/therapists guide patients through discussions focusing on here and now issues.
Findings
No significant differences across study arms, between the primary study outcome measures of pre and post distress, were found. However, on the secondary outcomes, comprised of the post study survey, patients reported that Dignity Therapy was significantly more likely to be experienced as helpful (χ2=35.501; p<0.001), improve quality of life (χ2 =14.520; p<0.001), sense of dignity (χ2 =12.655; p=0.002); change how their family sees and appreciates them (χ2 =33.811; p<0.001) and be helpful to their family (χ2=33.864; p<0.001).
Interpretation
Despite the beneficial effects of Dignity Therapy, its ability to mitigate outright distress, such as depression, desire for death or suicidality, has yet to be proven. However, there is currently ample evidence supporting its clinical application for patients nearing death, as a means of enhancing their end-of-life experience.
INTRODUCTION
There is a growing literature exploring ways of understanding and supporting patients facing end-of-life.1–3 Dignity Therapy, a unique, individualized, brief psychotherapy, was developed for the purpose of relieving distress and enhancing end-of-life experience for patients nearing death. While the intervention itself has been previously described, in brief, Dignity Therapy provides patients near the end-of-life an opportunity to reflect on things that matter most to them or that they would most want remembered.4 A framework of questions (Table 1), based on an empirical model of dignity in the terminally ill, informs the basic content of the therapeutic process.5,6 These conversations, guided by a trained therapist, are flexible so as to accommodate the patient's needs and choices regarding what they specifically wish to address. Dignity Therapy is audio-recorded and transcribed, with an edited version of the transcript returned to patients to share or bequeath to individuals of their choice.
Table 1.
Dignity Therapy Question Protocol
| Tell me a little about your life history; particularly the parts that you either remember most or think are the most important? When did you feel most alive? |
| Are there specific things that you would want your family to know about you, and are there particular things you would want them to remember? |
| What are the most important roles you have played in life (family roles, vocational roles, community-service roles, etc)? Why were they so important to you and what do you think you accomplished in those roles? |
| What are your most important accomplishments, and what do you feel most proud of? |
| Are there particular things that you feel still need to be said to your loved ones or things that you would want to take the time to say once again? |
| What are your hopes and dreams for your loved ones? |
| What have you learned about life that you would want to pass along to others? What advice or words of guidance would you wish to pass along to your (son, daughter, husband, wife, parents, other[s])? |
| Are there words or perhaps even instructions that you would like to offer your family to help prepare them for the future? |
| In creating this permanent record, are there other things that you would like included? |
A previous Phase I trial of Dignity Therapy, with of a sample of one-hundred terminally ill patients, reported 91% percent being satisfied with the therapy; 76% reported a heightened sense of dignity; 68%, an increased sense of purpose; 67%, a heightened sense of meaning; 47%, an increased will to live; and 81% indicated that it had been or would be of help to their family. Post-intervention measures of suffering and depressive symptoms showed modest, albeit significant improvement.4 Family members of patients also found dignity therapy helpful: 78% found that it enhanced patient dignity, 72% reported that it heightened the meaning of life for the patient, 78% said the document produced from the therapy session was a comfort to them in their time of grief, and 95% stated they would recommend Dignity Therapy for other patients and families.7
In view of the initial promise of Dignity Therapy, this study was conducted in order to examine its performance under randomized controlled conditions. Our primary objective was to determine if Dignity Therapy could lessen various dimensions of distress (e.g. depression, suffering), while our secondary objective was to determine if Dignity Therapy could enhance the quality of the dying experience, such as improving quality of life and sense of dignity, compared to two other conditions; standard palliative care and client centred care, as described below.
METHODS
Participants
Participants were recruited between April 2005 and October 2008, and eligible if they had a terminal prognosis with a life expectancy of six months or less, as determined by their treating physician; if they were receiving palliative care services through an affiliated recruitment site; if they were 18 years of age or greater; if they were willing to commit to 3 to 4 contacts over approximately 7 to 10 days; and if they were able and willing to provide written informed consent. Participants were excluded if they were delirious or otherwise cognitively impaired (based on clinical consensus and post randomization Blessed Orientation Memory Concentration test [BOMC]),8 if they were too unwell to complete the requirements of the protocol; or if they were unable to speak and read English.
Ethics Committee Approval: This trial was coordinated by the Manitoba Palliative Care Research Unit at CancerCare Manitoba, Winnipeg, Canada. Other participating centres included Curtin University, Perth, Australia and Memorial Sloan Kettering Cancer Centre, New York, USA. Approval was obtained from the ethics committees of all participating centres.
The funders played no role in the study design, data collection, analysis or interpretation of the data; nor in the writing of the final report. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
Study Arm Descriptions
After providing written informed consent, all participants were randomly assigned to one of three study arms; Dignity Therapy, Client Centred Care or Standard Palliative Care and asked to complete base-line psychosocial questionnaires.
Dignity Therapy
Patients randomized to Dignity Therapy were assigned a dignity therapist, comprised of a psychologist, psychiatrist or experienced palliative care nurse. All therapists took part in a three day training workshop, led by the PI (HMC). Ongoing Dignity Therapy supervision was provided by each site PI (HMC, LK, WB), initially on every case and than at varying degrees of frequency, until individual therapist competence was achieved. Group supervision, led by the PI, took place every six to eight weeks throughout the study, using videoconferencing to connect all three study sites. The PI also reviewed a random sample (about one in six) of Dignity Therapy transcripts from all study sites, in order to identify any problems or opportunities for therapeutic improvements. Feedback from this review was offered, either individually, or when more broadly applicable, within group supervision.
Patients were shown the Dignity Therapy question framework (Table 1) and asked to consider what they might wish to speak about during their Dignity Therapy session(s); this initial introduction to, and explanation of, Dignity Therapy took about 30 minutes. Within a few days, or as soon as a second meeting could be arranged, the therapist used the question framework to help elicit the patient's recollections, hopes, wishes for loved ones; lessons learned and things they wanted remembered by those they were about to leave behind. Dignity Therapy is flexible enough to accommodate participant preferences and choices regarding content, but the ethos of questioning targets those things that might enhance a sense of meaning, purpose, continued sense of self, and overall sense of dignity. All Dignity Therapy sessions were audio-taped; these sessions usually took about 60 minutes. Upon completion, the audio-recording was transcribed verbatim and the transcript edited, to provide a clear and readable narrative. This transcript or `generativity document' was returned to the patient within approximately four business days from their prior session, read to them in its entirety to ensure that no errors of omission or commission needed to be addressed (this final session usually took about 30 minutes). (Generativity, or the ability to guide the next generation, encompasses how patients might find strength or comfort in knowing that they will leave behind something lasting and transcendent of death)5. The final version of the generativity document was then given to the patient, to be passed along to a designated recipient of their choosing, from whom follow-up data were later obtained (the influence of Dignity Therapy on family recipients of generativity documents will be reported separately). At the conclusion of this session, participants were asked to complete a psychometric follow-up battery (as described below).
Client Centred Care
Client Centred Care is a supportive psychotherapeutic approach, in which the research nurse-therapist guided the patient through discussions focusing on `here and now' issues i.e. participants were asked about their illness, associated symptoms, and what was being done to address their distress. As such, the content of Client Centred Care was kept as distinct from Dignity Therapy as much as possible and did not focus on issues of generativity, meaning or purpose. If these issues were raised, the therapist did not probe for additional detail, allowing the interview to gently return to illness related inquiry. Although these sessions were audio-recorded for purposes of auditing protocol adherence, no permanent record of these conversations was provided to the patient or to his or her family. The number of contacts for Client Centred Care and Dignity Therapy were identical; with the initial, middle and final meetings designed to occupy about the same time interval across both arms. During the final meeting, seven to ten days later, the participants completed the psychometric battery.
Standard Palliative Care
Participants assigned to Standard Palliative Care had access to the full range of palliative care support services available to all study patients, including specialist palliative care physicians and nurses (i.e. experts in pain and symptom management), social workers, chaplains, and psychologists and/or psychiatrists. No participating site provided a formal approach to addressing generativity issues; as such, a program comparable to Dignity Therapy was not available to patients who were not randomized to the Dignity Therapy arm of this trial. Once patients were randomized to standard palliative care, they were asked to complete a battery of baseline psychometric questionnaires; seven to ten days later—a time frame corresponding to the approximate interval between the first and last contact in the other two study arms—they were asked to complete a battery of psychometric measures.
Baseline and Outcome Measures
The primary baseline measures consisted of the Palliative Performance Scale (PPS) (a measure of physical performance) [100%=healthy; 0%=death],9 the FACIT Spiritual Well-Being Scale (a measure of spiritual well-being with 2 subscales measuring Meaning/Peace and Faith),10 the Patient Dignity Inventory,11 and the Hospital Anxiety and Depression Scale (HADS).12 We also administered items from the Structured Interview for Symptoms and Concerns (SISC),13 including dignity, desire for death, suffering, hopelessness, depression, suicidal ideation and sense of burden to others. Additional measures included a two-item Quality of Life Scale14 and an Edmonton Symptom Assessment Scale (ESAS), modified to include a `will-to-life' visual analogue scale.15 All measures were re-administered immediately upon study completion. Secondary outcomes, addressing to what extent the intervention might have influenced their end-of-life experience, were measured by way of a post-study survey, asking detailed questions about their experience of the study and how it had affected them and their family.
Randomization and Masking
The study statistician did the randomization (1:1:1) in blocks of 30. Study arm assignment was based on a computer-generated table of random numbers. Blinding was achieved using opaque sealed envelopes containing allocations from a computer-generated table of random numbers. In order to determine trial arm designation, the envelopes were sent to each site and opened by study staff, in sequence, once participant consent had been obtained. To avoid any possible response bias or contamination, research staff with whom the participant had no prior contact administered the final psychometric battery. Recordings from the Dignity Therapy and Client Centered Care study arms were reviewed by the study coordinator to ensure protocol adherence and prevent cross arm contamination.
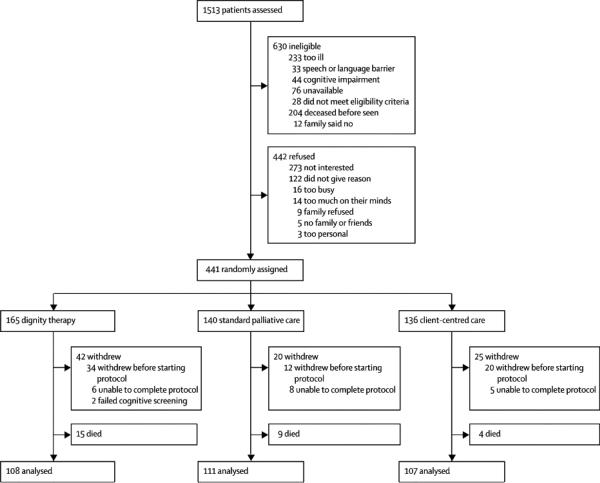
Recruitment (Figure I)
One-thousand five-hundred thirteen patients were assessed for eligibility utilizing a consecutive sampling approach. Of those, 630 were deemed ineligible and 442 refused (Figure 1). A total of 441 participants were randomized; following randomization, 28 patients died, 85 withdrew because of declining health and 2 failed BOMC screening. Given that there was either no, or only very partial data for these individuals, they were excluded from the analysis. As such, 326 participants completed the study. Recruitment was relatively even across the three study sites (Winnipeg, 119; Perth, 99 and New York, 108), with each site balanced across each study arm.
Figure 1.
Statistical Methods
Analyses were done on all patients with available data at baseline and at the end of the study intervention. The data was summarised using standard descriptive measures. The primary outcomes consisted of mean changes between baseline and end of intervention, on measures of psychosocial, spiritual and existential distress (see Baseline and Outcome Measures). Two group comparisons were carried out, using t-tests where the data approximated a normal distribution and Mann Whitney U tests when the data was ordinal. Three group comparisons were carried out using analysis of variance (ANOVA) when a normal distribution was reasonably approximated and Kruskal-Wallis tests when it was not. With an alpha set at .05, a desired power set at .80, and a small to medium effect size using Cohen's value for such an effect size of 0.15, the estimated recruitment target was 120 patients per arm.16 The effect size here refers to the standard deviation of the group means divided by the hypothesized common standard deviation. With three groups, an effect size of 0.15 would imply that at least one group mean is at least one third of a standard deviation away from the other two. SPSS-Version 18 was the software package used for statistical analysis.
When a significant result was obtained in a multi-group comparison, the precise nature of the group differences were explored using Tukey's test (if analysis of variance had been used) or a series of Mann-Whitney U tests (if the Kruskal Wallis test had been used). Pre-therapy versus post-therapy comparisons were carried out using the paired t test if the data was approximately normal or the Wilcox signed-rank test if it was not. All comparisons were carried out on a two-tailed basis. In view of the large number of comparisons being carried out and the resulting increased risk of type 1 errors, a probability of p<0.01 was used as the minimum acceptable designation of significance.
Results
Of the 326 participants who completed the study, 161 (49.4%) were male (table 2). The average age was 65.1 years (SD 14.4) [range: 22 – 102]. One-hundred ninety two (58.9%) were married or living common-law, with the remainder widowed, divorced or not married. 183 (56.1%) were living with their spouse/partner, 86 (26.4%) alone, 70 (21.5%) were living with children and the remainder living with others, such as friends or other relatives. Home based palliative care accounted for 196 (60.1%) of patients; 72 (22.1%) patients were receiving inpatient unit palliative care; 31 (22.1%) acute care inpatient (followed by palliative care on non-palliative care unit); and 27 (8.3%) freestanding hospice. Regarding religious affiliation, 119 (36.6%) were Protestant, 86 (26.4%) Catholic, 43 (13.2%) Jewish, 43 (13.2%) other, 33 (10.1%) none, and one person was unable to answer. Thirty participants (9.2%) had less than high school education, 107 (32.8%) had completed high school, and 188 (57.7%) college or post-graduate training (one person was unable to answer). Cancer disease site distribution included gastrointestinal (37.7%), genitourinary (17.2%), lung (14.7%), breast (8.9%), miscellaneous solid tumors (7.7%), hematological (4.6%), brain (2.8%), head and neck (2.2%) and non-malignant terminal condition (i.e. end-stage organ failure, ALS) [4.3%]. The average Palliative Performance Scale (PPS) rating for all participants was 44.30% (SD 15.13). As expected for a trial of this size, there was good balance at baseline in patient characteristics between the three randomised groups'.
Table 2.
Demographic Characteristics of RCT Sample by Study Arm
| RCT Study Arm | |||
|---|---|---|---|
| Demographics | Dignity Therapy | Client Centred Care | Standard Care Palliative |
| N per group | 108 | 107 | 111 |
| Age yrs M (SD) | 64.2 (14.6) | 64.3 (14.3) | 66.7 (14.2) |
| PPS score (SD) | 44.2 (15.2) | 44.4 (14.4) | 44.2 (15.9) |
|
| |||
| n (%) | n (%) | n (%) | |
|
| |||
| Male | 56 (52) | 55 (51) | 50 (45) |
|
| |||
| Marital status | |||
| Married | 60 (56) | 67 (63) | 65 (59) |
| Other | 48 (44) | 40 (37) | 46 (41) |
|
| |||
| Religion | |||
| Catholic | 31 (29) | 29 (28) | 26 (24) |
| Protestant | 22 (21) | 16 (15) | 30 (27) |
| Jewish | 17 (16) | 15 (14) | 11 (10) |
| Anglican | 17 (16) | 18 (17) | 16 (14) |
| Other | 11 (10) | 14 (13) | 18 (16) |
| None | 9 (8) | 14 (13) | 10 (9) |
|
| |||
| Living with arrangements | |||
| Alone | 30 (28) | 27 (25) | 29 (26) |
| Spouse | 37 (34) | 51 (48) | 50 (45) |
| Others | 18 (17) | 13 (12) | 21 (19) |
| Combination | 23 (21) | 16 (15) | 11 (10) |
|
| |||
| Education completed | |||
| None-primary | 11 (10) | 8 (8) | 11 (10) |
| High school | 38 (35) | 33 (31) | 36 (32) |
| College | 43 (40) | 45 (42) | 47 (42) |
| Post graduate | 16 (15) | 20 (19) | 17 (16) |
|
| |||
| Cancer site (primary) | |||
| Lung | 15 (15) | 18 (18) | 15 (14) |
| Breast | 10 (10) | 11 (10) | 8 (7) |
| GastroIntestinal | 30 (29) | 30 (30) | 48 (44) |
| Genitourinary | 15 (15) | 13 (13) | 9 (8) |
| Other | 32 (31) | 29 (29) | 29 (27) |
|
| |||
| Race | |||
| Caucasian | 98 (91) | 94 (88) | 99 (91) |
| Other | 10 (9) | 13 (12) | 10 (9) |
|
| |||
| Care setting | |||
| Palliative care unit | 25 (23) | 24 (22) | 21 (22) |
| In-pt pall service | 7 (6) | 13 (12) | 10 (9) |
| Out-patient/home | 64 (59) | 61 (57) | 69 (60) |
| Hospice | 12 (11) | 9 (8) | 11 (9) |
One hundred thirty four (41.1%) participants reported that they had lived with their life limiting condition less than one year; 104 (31.9%) 1 to 3 years; and the remainder for more than three years. One hundred eleven (34.1%) participants were assigned to Standard Palliative Care, 107 (32.8%) to Client Centred Care and 108 (33.1%) to Dignity Therapy. The median survival time was 110 days (25% ≤ 56 days; 75% ≤ 235 days) (65.3% of patients had died by the time the study concluded; the proportion of patients surviving across the study arms was not significantly different between groups (χ2=4.58; 2 df; p=0.1). There was no difference in post study survival time between the three study arms (F=0.675, p=0.51). Age and sex distribution, PPS ratings, as well as drop-out rate (death and withdrawal due to declining health), across all three study arms showed no significant differences.
Baseline measures for all pre-study psychometrics were calculated. (See Table 3A and 4A). Because no initial threshold level of distress was stipulated as an entry criterion, the sample was most noteworthy for its paucity of distress. In most instances, patients were not markedly distressed, as indicated by the average Patient Dignity Inventory (PDI) item scores, along with other baseline psychometric measures. Differences between pre and post study measures were calculated for all PDI and SISC items, along with modified ESAS individual sub-scale scores, the Quality of Life Scale, FACIT and HADS, comparing changes across all three study arms. No significant differences were found (see Table 3B and 4B). The post study survey, however, disclosed various differences between the three study conditions (Table 5). Patients receiving Dignity Therapy were significantly more likely to report having found the study helpful (χ2=35.501, 2 df; p<0.001), that it improved their quality of life (χ2=14.520, 2 df; p<0.001), and sense of dignity (χ2=12.655, 2 df; p=0.002). Dignity Therapy patients, compared to the other study arms, were also significantly more likely to report that being in the study changed how their family sees and appreciates them (χ2=33.811, 2 df; p<0.001) and that it has or will be of help to their family (χ2=33.864, 2 df; p<0.001). Dignity Therapy significantly outperformed one of the two other study arms on improving spiritual well being (χ2=10.354, 2 df; p=0.006), lessening sadness or depression (χ2=9.379, 2 df; p=0.009), and feeling satisfied with the study arm assignment (χ2=29.583, 2 df; p<0.001).
Table 3A.
Baseline distress across all three arms as measured by the Patient Dignity Inventory6 at t1
| PDI Item* | Standard Palliative Care (SC) Mean/standard deviation | Client Centered Care (CCC) Mean/standard deviation | Dignity Therapy (DT) Mean/standard deviation |
|---|---|---|---|
| Not able to continue usual routines | 2.70 (1.317) | 2.51 (1.140) | 2.47 (1.284) |
| Physically distressing symptoms | 2.28 (1.209) | 2.57 (1.331) | 2.32 (1.289) |
| Not able to carry out important roles | 2.11 (1.222) | 2.02 (1.173) | 1.88 (1.150) |
| Feeling no longer who I was | 2.00 (1.265) | 2.21 (1.335) | 2.20 (1.288) |
| Not able to perform tasks of daily living | 1.74 (1.150) | 1.84 (1.109) | 1.79 (1.077) |
| Feeling of not having control | 2.08 (1.121) | 2.15 (1.231) | 2.15 (1.287) |
| Feeling uncertain | 2.08 (1.237) | 2.05 (1.158) | 2.10 (1.184) |
| Not able to attend to bodily functions | 1.40 (0.947) | 1.56 (1.057) | 1.42 (0.929) |
| Feeling anxious | 1.73 (1.009) | 1.93 (1.113) | 1.93 (1.091) |
| Feeling of reduced privacy | 1.87 (1.134) | 1.66 (1.037) | 1.82 (1.126) |
| Feeling a burden to others | 1.99 (1.083) | 2.07 (1.127) | 1.90 (1.076) |
| Feeling how you look has changed | 1.79 (1.105) | 1.64 (1.041) | 1.83 (1.120) |
| Feeling depressed | 1.69 (0.951) | 1.76 (1.000) | 1.84 (1.120) |
| Worried about future | 2.13 (1.222) | 2.15 (1.241) | 2.08 (1.298) |
| Not being able to think clearly | 1.66 (1.043) | 1.92 (1.119) | 1.74 (0.931) |
| Feeling of unfinished business | 1.95 (1.102) | 2.03 (1.145) | 1.91 (1.107) |
| Feeling life no longer has meaning or purpose | 1.56 (1.050) | 1.54 (1.012) | 1.58 (0.981) |
| Not feeling worthwhile of valued | 1.42 (0.859) | 1.61 (1.088) | 1.50 (0.932) |
| Feeling have not made meaningful contribution | 1.30 (0.736) | 1.39 (0.798) | 1.33 (0.710) |
| Not feeling able to mentally fight illness | 1.40 (0.789) | 1.56 (0.898) | 1.43 (0.837) |
| Not being able to accept things as they are | 1.48 (0.862) | 1.55 (0.914) | 1.57 (1.020) |
| Concerns regarding spiritual life | 1.18 (0.508) | 1.36 (0.758) | 1.30 (0.727) |
| Not being treated with respect | 1.12 (0.400) | 1.18 (0.529) | 1.19 (0.587) |
| Not feeling supported by health care providers | 1.18 (0.490) | 1.45 (0.954) | 1.20 (0.679) |
| Not feeling supported by friends or family | 1.07 (0.293) | 1.18 (0.642) | 1.23 (0.731) |
1=Not a problem, 2=a slight problem; 3=a problem; 4=a major problem; 5=an overwhelming problem
Table 4A.
| INSTRUMENT | Standard Palliative Care (SC) Mean/standard deviation | Client Centered Care (CCC) Mean/standard deviation | Dignity Therapy (DT) Mean/standard deviation |
|---|---|---|---|
| SISC* | |||
| Loss of Dignity | 0.35 (0.805) | 0.68 (1.087) | 0.58 (0.996) |
| Desire for Death | 0.60 (1.193) | 0.64 (1.176) | 0.44 (0.868) |
| Sense of Suffering | 1.46 (1.530) | 1.52 (1.348) | 1.63 (1.574) |
| Hopelessness | 0.78 (1.082) | 0.87 (1.235) | 0.90 (1.168) |
| Depression | 1.14 (1.311) | 1.25 (1.186) | 1.22 (1.263) |
| Suicidality | 0.21 (0.662) | 0.38 (0.856) | 0.29 (0.724) |
| Burden to Others | 1.54 (1.445) | 1.53 (1.562) | 1.47 (1.550) |
| ESAS** | |||
| Pain | 2.76 (2.802) | 3.13 (2.835) | 2.72 (2.788) |
| Nausea | 1.62 (2.438) | 1.30 (2.336) | 1.52 (2.181) |
| Drowsiness | 2.89 (2.710) | 3.31 (2.916) | 3.61 (2.960) |
| Shortness of Breath | 1.70 (2.327) | 2.35 (2.917) | 1.98 (2.594) |
| Will to Live± | 9.05 (2.017) | 9.00 (2.000) | 9.08 (1.939) |
| Appetite | 5.91 (3.031) | 6.93 (2.645) | 6.59 (3.127) |
| Level of Activity | 4.59 (2.662) | 4.80 (2.686) | 4.59 (2.969) |
| Sense of Well Being± | 6.65 (2.642) | 6.74 (2.618) | 6.67 (2.670) |
| Quality of Life | |||
| Quality of Life rating+ | 6.27 (2.695) | 6.29 (2.503) | 6.48 (2.693) |
| Quality of Life satisfaction+ | 6.10 (3.089) | 5.83 (3.163) | 6.34 (3.055) |
| FACIT*** (48) | |||
| Total | 33.818 (9.56) | 32.861 (9.607) | 34.700 (9.586) |
| • FACIT-Secular (32) | 23.65 (6.30) | 23.050 (6.260) | 24.500 (5.852) |
| • FACIT-Faith (16) | 10.0 (5.07) | 9.811 (5.098) | 10.200 (5.215) |
| HADS**** (42) | |||
| Total | 11.363 (6.755) | 12.058 (7.277) | 11.075 (6.757) |
| • HADS-Depression (21) | 6.027 (4.017) | 6.301 (4.043) | 5.859 (3.856) |
| • HADS-Anxiety (21) | 5.336 (3.786) | 5.757 (4.255) | 5.217 (4.204) |
0=none; 1 =minimal; 2=mild; 3=moderate; 4=strong; 5=severe; 6=extreme
1='no' or `poor'; 10= `worst'
reverse scoring
1=poor/not satisfied; 10=excellent/very satisfied
high score reflects better spiritual wellbeing
high score reflects more intense depression
Table 3B.
Distress across all three arms as measured by the Patient Dignity Inventory6 at t2
| PDI Item* | Standard Palliative Care (SC) Mean/standard deviation | Client Centered Care (CCC) Mean/standard deviation | Dignity Therapy (DT) Mean/standard deviation |
|---|---|---|---|
| Not able to continue usual routines | 2.42 (1.254) | 2.28 (1.136) | 2.33 (1.250) |
| Physically distressing symptoms | 2.22 (1.139) | 2.35 (1.204) | 2.37 (1.242) |
| Not able to carry out important roles | 2.05 (1.166) | 2.02 (1.173) | 1.88 (1.240) |
| Feeling no longer who I was | 2.02 (1.152) | 2.06 (1.258) | 2.09 (1.270) |
| Not able to perform tasks of daily living | 1.84 (1.148) | 1.88 (1.211) | 2.11 (1.248) |
| Feeling of not having control | 2.00 (1.053) | 2.22 (1.216) | 2.00 (1.124) |
| Feeling uncertain | 1.88 (1.093) | 2.07 (1.229) | 2.21 (1.221) |
| Not able to attend to bodily functions | 1.64 (1.118) | 1.61 (1.016) | 1.82 (1.564) |
| Feeling anxious | 1.80 (1.016) | 1.92 (1.084) | 1.90 (1.090) |
| Feeling of reduced privacy | 1.73 (1.009) | 1.83 (1.077) | 1.84 (1.180) |
| Feeling a burden to others | 1.92 (1.113) | 2.11 (1.144) | 1.91 (1.024) |
| Feeling how you look has changed | 1.69 (1.077) | 1.71 (0.991) | 1.72 (1.084) |
| Feeling depressed | 1.74 (0.992) | 1.79 (1.064) | 1.81 (1.065) |
| Worried about future | 1.76 (1.029) | 1.94 (1.172) | 2.03 (1.261) |
| Not being able to think clearly | 1.69 (0.980) | 1.85 (1.102) | 1.79 (1.116) |
| Feeling of unfinished business | 1.86 (1.151) | 1.91 (1.069) | 1.79 (1.016) |
| Feeling life no longer has meaning or purpose | 1.48 (0.923) | 1.64 (1.032) | 1.46 (0.850) |
| Not feeling worthwhile of valued | 1.44 (0.914) | 1.58 (1.055) | 1.57 (1.150) |
| Feeling have not made meaningful contribution | 1.23 (0.674) | 1.44 (0.892) | 1.36 (0.862) |
| Not feeling able to mentally fight illness | 1.44 (0.931) | 1.58 (0.945) | 1.46 (0.883) |
| Not being able to accept things as they are | 1.48 (0.952) | 1.50 (0.851) | 1.54 (0.938) |
| Concerns regarding spiritual life | 1.23 (0.670) | 1.24 (0.612) | 1.37 (1.260) |
| Not being treated with respect | 1.20 (0.585) | 1.23 (0.667) | 1.20 (0.621) |
| Not feeling supported by health care providers | 1.13 (0.488) | 1.26 (0.757) | 1.11 (0.421) |
| Not feeling supported by friends or family | 1.14 (0.553) | 1.23 (0.708) | 1.08 (0.391) |
1=Not a problem, 2=a slight problem; 3=a problem; 4=a major problem; 5=an overwhelming problem
Table 4B.
| INSTRUMENT | Standard Palliative Care (SC) Mean/standard deviation | Client Centered Care (CCC) Mean/standard deviation | Dignity Therapy (DT) Mean/standard deviation |
|---|---|---|---|
| SISC* | |||
| Loss of Dignity | 0.51 (0.943) | 0.47 (0.955) | 0.67 (1.192) |
| Desire for Death | 0.65 (1.285) | 0.68 (1.176) | 0.53 (0.880) |
| Sense of Suffering | 1.41 (1.384) | 1.46 (1.348) | 1.34 (1.402) |
| Hopelessness | 0.68 (1.306) | 0.80 (1.169) | 0.86 (1.271) |
| Depression | 1.06 (1.377) | 1.06 (1.250) | 1.23 (1.227) |
| Suicidality | 0.30 (1.023) | 0.32 (0.958) | 0.27 (0.731) |
| Burden to Others | 1.24 (1.497) | 1.43 (1.381) | 1.33 (1.399) |
| ESAS** | |||
| Pain | 2.87 (2.800) | 3.18 (2.942) | 2.79 (2.609) |
| Nausea | 1.59 (2.612) | 1.55 (2.423) | 1.57 (2.423) |
| Drowsiness | 3.07 (2.837) | 3.54 (2.963) | 3.65 (2.908) |
| Shortness of Breath | 1.75 (2.503) | 2.51 (3.109) | 2.52 (2.846) |
| Will to Live± | 8.84 (2.403) | 9.00 (2.194) | 8.99 (1.615) |
| Appetite | 6.05 (3.175) | 7.05 (2.995) | 6.24 (3.040) |
| Level of Activity | 4.45 (2.814) | 4.42 (2.784) | 4.24 (2.916) |
| Sense of Well Being± | 6.44 (2.891) | 6.50 (2.883) | 6.62 (2.659) |
| Quality of Life | |||
| Quality of Life rating+ | 6.34 (2.473) | 6.64 (2.549) | 6.39 (2.542) |
| Quality of Life satisfaction+ | 6.05 (2.986) | 6.05 (2.876) | 6.04 (2.938) |
| FACIT (48) | |||
| Total | 34.438 (10.133) | 32.430 (10.373) | 33.969 (10.290) |
| • FACIT-Secular (32) | 24.038 (6.758) | 22.800 (7.186) | 23.878 (6.269) |
| • FACIT-Faith (16) | 10.400 (4.724) | 9.630 (5.054) | 10.091 (5.133) |
| HADS (56) | |||
| Total | 11.387 (7.431) | 11.760 (7.803) | 11.452 (6.844) |
| • HADS-Depression (28) | 6.189 (4.209) | 6.384 (4.304) | 5.642 (4.073) |
| • HADS-Anxiety (28) | 5.198 (4.049) | 5.376 (4.395) | 5.810 (3.802) |
0=none; 1 =minimal; 2=mild; 3=moderate; 4=strong; 5=severe; 6=extreme
1='no' or `poor'; 10= `worst'
reverse scoring; higher scores represent better outcomes
1=poor/not satisfied; 10=excellent/very satisfied
high score reflects better spiritual wellbeing
high score reflects more intense depression
Table 5.
Post Study Survey Results (mean survey score comparisons across three study arms)
| Post Study Survey Questions The study arm has… | Standard Palliative Care (SC)/Standard Deviation | Client Centered Care (CCC)/Standard Deviation | Dignity Therapy (DT)/Standard Deviation | χ2 2 df | p-value | ArmsDT Significantly Outperforme d |
|---|---|---|---|---|---|---|
| …been helpful to me | 3.50 (1.011) | 3.72 (0.888) | 4.23 (0.635) | 35.501 | <0.0001 | CCC, SC |
| …been as helpful as any other aspect of my health care | 3.27 (1.041) | 3.12 (1.041) | 3.63 (1.044) | 6.386 | 0.041 | NA |
| …improved my quality of life | 2.96 (0.958) | 2.84 (1.045) | 3.54 (0.947) | 14.520 | 0.001 | CCC, SC |
| …given me a sense of looking after unfinished business | 2.86 (1.059) | 2.93 (1.156) | 3.35 (1.010) | 6.874 | 0.032 | NA |
| …improved my spiritual well being | 3.00 (1.114) | 2.56 (0.983) | 3.27 (1.087) | 10.354 | 0.006 | CCC |
| …lessened my sense of sadness and depression | 2.57 (0.922) | 2.65 (1.044) | 3.11 (1.018) | 9.379 | 0.009 | SC |
| …lessened my sense of feeling a burden to others | 2.58 (0.950) | 2.53 (0.960) | 2.81 (0.981) | 2.707 | >0.10 | NA |
| …made me feel more worthwhile or valued | 3.35 (0.996) | 3.02 (1.012) | 3.38 (0.934) | 3.751 | >0.10 | NA |
| …made me feel like I am still me | 3.59 (0.920) | 3.40 (0.979) | 3.81 (0.852) | 5.906 | 0.052 | NA |
| …given me a greater sense of having control over my life | 3.16 (0.997) | 2.81 (1.052) | 3.02 (1.016) | 2.737 | >0.10 | NA |
| …helped me to accept the way things are | 3.31 (1.010) | 3.19 (1.118) | 3.39 (1.063) | 0.924 | >0.10 | NA |
| …made me feel more respected and understood by others | 3.04 (0.979) | 2.79 (0.976) | 3.16 (0.895) | 3.849 | >0.10 | NA |
| …made me feel that I am still able to carry out important tasks or fill an important role | 3.48 (0.995) | 3.02 (1.047) | 3.62 (0.974) | 8.963 | 0.011 | NA |
| …been satisfactory | 3.80 (0.743) | 4.17 (0.563) | 4.26 (0.634) | 29.583 | <0.0001 | SC |
| …made me feel that life was more meaningful | 3.19 (1.069) | 3.31 (1.022) | 3.55 (1.054) | 6.731 | 0.035 | NA |
| …given me a heightened sense of purpose | 3.20 (0.984) | 3.15 (1.026) | 3.49 (1.037) | 6.858 | 0.032 | NA |
| …increased my sense of dignity | 3.09 (1.019) | 3.11 (0.974) | 3.52 (1.039) | 12.655 | 0.002 | CCC, SC |
| …lessened my sense of suffering | 2.70 (1.016) | 2.77 (0.979) | 2.86 (1.037) | 1.062 | >0.10 | NA |
| …increased my will to live | 2.76 (1.035) | 2.92 (0.972) | 2.94 (1.113) | 1.725 | >0.10 | NA |
| …or will be of help to my family | 3.20 (1.002) | 3.29 (0.992) | 3.93 (0.797) | 33.864 | <0.0001 | CCC, SC |
| …or could change way my family sees or appreciates me | 2.85 (1.003) | 2.85 (1.040) | 3.58 (1.006) | 33.811 | <0.0001 | CCC, SC |
| In general, I am satisfied with my psychosocial care | 4.14 (0.648) | 3.99 (0.893) | 4.25 (0.773) | 5.969 | 0.051 | NA |
(Strongly disagree=1; Disagree=2; Neither agree nor disagree=3; Agree=4; Strongly agree=5) Bolded p-values significant at p<0.01;
NA = not applicable (detailed group comparisons only carried out if p significant at less than 0.01)
Discussion
This study represents the first randomized control trial of Dignity Therapy. We set out to determine if this novel psychotherapeutic approach would significantly outperform standard care, or Client Centered Care (which focused on non-generativity, here and now issues) on various measures of psychological, existential and spiritual distress. While floor effects precluded our ability to demonstrate significant differences across study arms, our secondary outcomes revealed substantive benefits of Dignity Therapy. Using a post-study survey, patients who received Dignity Therapy were significantly more likely to report benefits, in terms of finding it helpful, improving their quality of life, their sense of dignity; changing how their family might see or appreciate them, and deeming it helpful to their family, compared to the other study arms.
Comprehensive palliative care requires that careful attention be paid to the physical, psychosocial, existential and spiritual sources of end-of-life distress. Restricting ones' focus on any of these domains to the exclusion of others, fails to meet standards of palliative care as specified by the World Health Organization17 and the Institutes of Medicine (IOM).18 In describing factors associated with a good death, the IOM includes preparation for death and opportunities for closure or `sense of completion' of the life.18 Yet, while significant inroads have been made in our ability to achieve physical comfort for dying patients, there are few novel interventions designed to address the psychosocial, existential and spiritual dimensions of end-of-life care.
Dignity Therapy was developed for the purpose of lessening distress and enhancing end-of-life experience for patients approaching death. In our phase I trial, nearly all patients found Dignity Therapy helpful, whether they had disclosed substantial initial distress or not.4 On the basis of that finding, baseline distress was not specified as an entry criteria for this current randomized controlled trial. Given that base rates of distress within our sample were quite low, it is perhaps not surprising that we were unable to measure any significant changes in distress across the three study arms. Showing improvement of measures of depression, will to live and quality of life, presupposes that patients' experience those areas as initially being problematic. In the absence of such initial distress, there is simply little room for improvement.
It is also possible that the instruments we used for our primary outcomes were less responsive and less sensitive to changes than the secondary outcome measures, whereby patients reported their experiences in a post-study survey. The difficulty of demonstrating psychosocial change at end of life by way of using self-report measures has been well documented. Unlike a chemotherapy trial, where survival interval, tumor load, and overall mortality provide readily measurable and objective outcomes, defining outcomes for Dignity Therapy is far more challenging. Dignity Therapy was designed to favorably influence the experience of people moving towards death. As such, measures of overt distress, along with indicators of psychosocial, existential and spiritual impact, were incorporated into the study protocol. A recent review of quality of life measures suitable for use in palliative care was unable to identify any with established responsiveness to change.19 A recent meta-analysis concluded that pre-intervention distress is a critical moderator of efficacy for psychosocial interventions for cancer patients.20 Scott et al have suggested that a more successful approach may be applying serial qualitative interviews.21 This approach, however, would not be well suited to a design comprised of an RCT.
Given the lack of significant difference across study arms for the primary outcome measures, we also considered whether the trial might have been underpowered. Our post-hoc power calculation, based on the actual number of trial participants determined that with 326 patients, this study had a power of 0.72 – 0.95 to detect an effect size of 0.15 – 0.30, respectively. It is also noteworthy that most non-significant differences had large p-values and significant differences had very small p-values, so the issue of power may be moot.
That said, patients receiving Dignity Therapy were significantly more likely than those assigned to other study arms, to report that this approach was helpful, that it improved their quality of life, enhanced their sense of dignity and provided benefits to their family. It would appear that although they reported their initial state of psychosocial or existential well-being as satisfactory, patients receiving Dignity Therapy often encountered an enhanced quality of end-of-life experience that they simply could not have anticipated. While difficult to measure, the impact was often poignant and profound. For instance, one 72-year-old woman with bowel cancer stated, “[Dignity therapy] brought to the forefront that I have to prepare my family to the best of my ability.” A 56-year-old woman said, “Mostly I want my family to know that I'm okay with dying and they must move on.” She went on to say that “the therapy showed me I am not the cancer, I am still in here. I am so grateful for that because I lost myself….it really helped me remember who I am.”
In hindsight, one might argue that this randomized controlled trial should have screened for patients reporting some baseline critical level of distress. That might have enhanced the likelihood of demonstrating differences across the three study arms, based on changes in the pre and post intervention questionnaires. Our disinclination to do so, however, was based on prior findings, illustrating the salutary effects of Dignity Therapy for nearly all patients nearing death, whether overtly distressed or not. Introducing critical thresholds of distress for study inclusion would have eliminated the vast majority of patients, who are most likely to partake of this novel therapeutic approach. Another consideration may have been a cross over design, in which patients could experience and thus compare Dignity therapy with other possible study conditions. However, given how ill these patients were, such a design would not have been feasible, with many patients either deteriorating or dying prior to a head to head comparison being possible.
It is also notable that of the 1513 patients who were accessed for eligibility, 42% were ineligible, primarily because they were too ill to take part in the study. Of those who met eligibility criteria, half consented to participate, nearly three-quarters of whom completed the protocol. For palliative care protocols that require cognitively intact participants, this recruitment pattern is not at all atypical.22 The nature of Dignity Therapy is such that only patients who are mentally capable of providing personally meaningful responses, are those who will be approached to take part. Therefore, generalizability should be framed in terms of those who maintain their cognitive capacity in proximity to death. Although this particular trial primarily involved patients with cancer, other studies have begun to explore its application in non-cancer populations23
We are not aware of any instance where patients withdrew from Dignity Therapy because of feeling upset or distressed. Many patients, however, indicated moments during Dignity Therapy that were emotionally evocative; for example, talking about hopes or wishes for family members in anticipation of a time beyond their death. By and large, however, patients appreciated the opportunity to articulate these issues. The only safety issue, which will be reported more fully in a separate paper describing family experiences of Dignity Therapy, concerned a few occasions where family members were dissatisfied with the generativity document. In those instances, they felt the patient had become too ill to give fulsome responses, or that the answers provided a distorted image of the participant. As such, it is important that patients who are delirious or otherwise cognitively impaired be excluded from Dignity Therapy.
Several studies have recently been published, reporting on the performance of Dignity therapy under various circumstances. A Phase I Danish study of ten health care professionals and twenty patients concluded that, with minor cultural adaptations, Dignity Therapy was “a manageable, acceptable and relevant intervention for Danish patients admitted to palliative care”.24 A pilot study of eight end stage patients in rural Kentucky with end stage cancer showed that Dignity Therapy could be delivered by videophone, and achieve overall benefit and high levels of patient satisfaction.25 A phase I study conducted in French Canada reported that amongst a cohort of 33 dying patients, relevance and satisfaction were found to be high, for patients and families alike.26
Despite the beneficial effects elicited by Dignity Therapy, its ability to mitigate outright distress, such as depression, desire for death or suicidality, remains unproven. Future research amongst more severely distressed patients may indeed establish its role in those particular circumstances. However, while “symptomatic relief of distress is an important goal of psychotherapeutic treatment, it is too limited a framework from which to consider the purpose and potential benefit of individual psychotherapy for patients with advanced or terminal disease.”27 In these circumstances, psychotherapy is not only offered to alleviate distress, but also as a means of preventing distress, promoting well being and establishing a sense of personal meaning and life purpose. Psychotherapeutic support can help patients face disappointments, process the reality of leaving behind loved ones; deal with feelings of sadness, loss, isolation and a damaged sense of identity and personal value. It can also help patients consider personal priorities regarding relationships, religious and spiritual beliefs, and deal with the urgency of resolving conflicts or achieve personally meaningful goals.27–30 Palliative care must offer patients opportunities to engage in this myriad of issues, and Dignity Therapy is one means by which it might do so. Future research exploring the salutary effects of Dignity Therapy will no doubt help to unravel the psychological, spiritual and existential complexities of facing death, and how to best support patients and families confronting advanced and terminal illness.
Research in Context
The systematic review that accompanied the application for funding of the Dignity Therapy RCT was incorporated into two publications; Chochinov HM, Hack T, Hassard T, et al. Dignity and Psychotherapeutic Considerations in End of Life Care. Journal of Palliative Care. 2004;20:142–143, and later updated, appearing in, Chochinov HM. Dying, Dignity and new Horizons in Palliative End-of-Life care. CA: A Cancer Journal for Clinicians. 2006;56(2):84–103. This is the first randomized trial of Dignity Therapy. Based on the findings of this study, clinicians should consider Dignity Therapy a viable therapeutic approach, which can enhance end-of-life experience for patients and families confronting death.
Supplementary Material
Acknowledgements
We thank our research staff, including Sheila Lander, Kathy Cullihall, Beverley Cann (Winnipeg); Joanne Hale, Jenny Clarke, Sky Dawson, and Lynn Oldham (Perth); Shannon Poppito, Wendy Lichtenthal, Amy Berg, Kimberly Pitrelli (New York). Dr. Chochinov is a Canada Research Chair in Palliative Care, funded by the Canadian Institutes for Health Research.
Source of Funding: National Cancer Institute, NIH
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statements: None of the authors have any conflict of interest to declare.
References
- 1.Steinhauser KE, Christakis NA, Clipp EC, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22:727–37. doi: 10.1016/s0885-3924(01)00334-7. [DOI] [PubMed] [Google Scholar]
- 2.Lynn J. Perspectives on care at the close of life. Serving patients who may die soon and their families: the role of hospice and other services. Jama. 2001;285:925–32. doi: 10.1001/jama.285.7.925. [DOI] [PubMed] [Google Scholar]
- 3.Emanuel L, Bennett K, Richardson VE. The dying role. J Palliat Med. 2007;10:159–68. doi: 10.1089/jpm.2006.0134. [DOI] [PubMed] [Google Scholar]
- 4.Chochinov HM, Hack T, Hassard T, Kristjanson L, McClement S, Harlos M. Dignity Therapy: A Novel Psychotherapeutic Intervention for Patients Nearing Death. Journal of Clinical Oncology. 2005;23:5520–5525. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 5.Chochinov HM, Hack T, McClement S, Harlos M, Kristjanson L. Dignity in the Terminally Ill: A Developing Empirical Model. Social Science and Medicine. 2002;54:433–443. doi: 10.1016/s0277-9536(01)00084-3. [DOI] [PubMed] [Google Scholar]
- 6.Chochinov HM. Dignity Conserving Care: A New Model for Palliative Care. JAMA. 2002;287:2253–2260. doi: 10.1001/jama.287.17.2253. [DOI] [PubMed] [Google Scholar]
- 7.McClement S, Hack T, Chochinov HM, Hassard T, Kristjanson L, Harlos M. Dignity Therapy: Family Member Perspectives. Journal of Palliative Medicine. 2007;10:1076–82. doi: 10.1089/jpm.2007.0002. [DOI] [PubMed] [Google Scholar]
- 8.Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry. 1999;14:936–40. [PubMed] [Google Scholar]
- 9.Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative Performance Scale (PPS): A new tool. Journal of Palliative Care. 1996;12:5–11. [PubMed] [Google Scholar]
- 10.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy--spiritual well-being scale (FACIT-sp) Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. 2002. [DOI] [PubMed] [Google Scholar]
- 11.Chochinov HM, Hassard T, McClement S, Hack T, Kristjanson L, Harlos M, Sinclair S, Murray A. The Patient Dignity Inventory: A novel way of measuring dignity related distress in Palliative Care. Journal of Pain and Symptom Management. 2008 doi: 10.1016/j.jpainsymman.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Moorey S, Greer S, Watson M, et al. The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. Br J Psychiatry. 1991;158:2555–259. doi: 10.1192/bjp.158.2.255. [DOI] [PubMed] [Google Scholar]
- 13.Wilson KG, Graham ID, Viola RA, Chater S, de Faye BJ, Weaver LA, Lachance JA. Structured interview assessment of symptoms and concerns in palliative care. Can J Psychiatry. 2004;49:350–8. doi: 10.1177/070674370404900603. [DOI] [PubMed] [Google Scholar]
- 14.Graham KY, Longman AJ. Quality of life in persons with melanoma: Preliminary model testing. Cancer Nursing. 1987;10:338–346. [PubMed] [Google Scholar]
- 15.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 16.Cohen J. Statistical power analysis for the behavioral sciences. revised edition Academic Press; New York: 1977. [Google Scholar]
- 17.World Health Organization . Cancer Pain Relief and Palliative Care: Report of a WHO Expert Committee (Technical Bulletin 804) World Health Organization; Geneva, Switzerland: 1990. [PubMed] [Google Scholar]
- 18.Field MJ, Cassel CK. For the Institute of Medicine. National Academy Press; Washington DC: 1997. Approaching death: Improving care at the end of life. [PubMed] [Google Scholar]
- 19.Gwenda Albers, Echteld Michael A, de Vet Henrica CW, Onwuteaka-Philipsen Bregje D, van der Linden Mecheline HM, Luc Deliens Evaluation of quality-of-life measures for use in palliative care: a systematic review. Palliat Med. 2010;24:17. doi: 10.1177/0269216309346593. [DOI] [PubMed] [Google Scholar]
- 20.Schneider S, Moyer A, Knapp-Oliver, Sohl S, Cannella D, Targhella V. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med. 2010;33:1–14. doi: 10.1007/s10865-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murray SA, Kendall M, Carduff E, Worth A, Harris FM, Lloyd A, Cavers D, Grant L, Sheikh A. Use of serial qualitative interviews to understand patients' evolving experiences and needs. BMJ. 2009;339:b3702. doi: 10.1136/bmj.b3702. [DOI] [PubMed] [Google Scholar]
- 22.Wilson KG, Chochinov HM, McPherson CJ, Skirko MG, Allard P, Chary S, Gagnon PR, Macmillan K, De Luca M, O'Shea F, Kuhl D, Fainsinger RL, Karam AM, Clinch JJ. Desire for euthanasia or physician-assisted suicide in palliative cancer care. Health Psychol. 2007;26:314–23. doi: 10.1037/0278-6133.26.3.314. [DOI] [PubMed] [Google Scholar]
- 23.Chochinov HM, Cann B, Cullihall K, Kristjanson L, Harlos M, McClement SE, Hack TF, Hassard T. Dignity Therapy: A Feasibility Study of Elders in Long-term Care. Journal of Palliative and Supportive Care. doi: 10.1017/S1478951511000538. In Press. [DOI] [PubMed] [Google Scholar]
- 24.Houmann LJ, Rydahl-Hansen S, Chochinov HM, Kristjanson LJ, Groenvold M. Testing the feasibility of the Dignity Therapy interview: adaptation for the Danish culture. BMC Palliat Care. 2010;9:21. doi: 10.1186/1472-684X-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Passik SD, Kirsh KL, Leibee S, Kaplan LS, Love C, Napier E, Burton D, Sprang R. A feasibility study of dignity psychotherapy delivered via telemedicine. Palliat Support Care. 2004;2:149–55. doi: 10.1017/s1478951504040209. [DOI] [PubMed] [Google Scholar]
- 26.Gagnon P, Chochinov HM, Cochrane J, Le Moignan Moreau J, Fontaine R, Croteau L. Psychothérapie de la Dignité : Une intervention pour réduire la détresse psychologique chez les personnes en soins palliatifs. Psycho-Oncologie. 2010;4:169–175. [Google Scholar]
- 27.Rodin G. Individual Psychotherapy for the Patient with Advanced Disease Individual Psychotherapy for the Patient with Advanced Disease. In: Chochinov HM, Breitbart, editors. Handbook of Psychiatry and Palliative Medicine. Second Edition Oxford University Press; 2006. [Google Scholar]
- 28.Cordova MJ, Cunningham LL, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychol. 2001;20:176–185. [PubMed] [Google Scholar]
- 29.Block SD. Perspectives on care at the close of life. Psychological considerations, growth, and transcendence at the end of life: the art of the possible. JAMA. 2001;285:2898–905. doi: 10.1001/jama.285.22.2898. [DOI] [PubMed] [Google Scholar]
- 30.Tedeschi RG, Calhoun LG. Trauma and the Transformation of Suffering. Sage Publications; Thousand Oaks, CA: 1995. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.