Abstract
Background
The optimal strategy for promoting self-care for heart failure (HF) is unclear.
Methods and Results
We conducted a randomized trial to determine whether a “teach to goal” (TTG) educational and behavioral support program provided incremental benefits to a brief (one hour) educational intervention (BEI) for knowledge, self-care behaviors, and HF-related quality of life (HFQOL). The TTG program taught use of adjusted-dose diuretics and then reinforced learning goals and behaviors with 5-8 telephone counseling sessions over one month. Participants’ (N=605) mean age was 61 years; 37% had marginal or inadequate literacy; 69% had ejection fraction < 0.45; and 31% had class III or IV symptoms. The TTG group had greater improvements in general and salt knowledge (p < 0.001) and greater increases in self-care behaviors (from mean 4.8 to 7.6 for TTG vs. 5.2 to 6.7 for BEI; p<0.001). HFQOL improved from 58.5 to 64.6 for the TTG group but did not change for the BEI group (64.7 to 63.9; p < 0.001 for the difference in change scores). Improvements were similar regardless of participants’ literacy level.
Conclusions
Telephone reinforcement of learning goals and self-care behaviors improved knowledge, health behaviors, and HF-related QOL compared to a single education session.
Keywords: heart failure, patient education, counseling, self-care
Heart failure (HF) affects 5.8 million people in the US, causing 283,000 deaths and costing 39.2 billion dollars annually.1 Self-care training teaches key skills and reinforces behaviors associated with better outcomes, including symptom recognition, weight monitoring, dietary salt restriction, exercise, medication adherence, and a plan for what to do in the event of exacerbation of symptoms.2
Several studies have examined the effect of self-care training interventions on HF outcomes, including knowledge, self-efficacy, self-care behaviors, hospitalization, quality of life, and mortality.3-7 These studies were very heterogeneous in the frequency and duration of the self-management interventions, ranging from a single one-hour session to phone calls weekly for one month, biweekly for 8 weeks, and monthly for the remainder of the study year.4 The optimal dose and duration of training remain unclear.
Because self-care training can reduce readmissions, Medicare has adopted discharge education as a core quality measure that assesses whether patients admitted for HF are discharged home with written instructions or educational material about their recommended activity level, diet, medications, follow-up appointment, weight monitoring, and what to do if symptoms worsen.8 However, this requires only that some evidence of training be documented while the patient is hospitalized, and it does not distinguish between minimal or more intensive training, including reinforcement of self-care education and behaviors after hospitalization (as was typically done in the interventions cited above). Studies have found weak or no association between achievement of high scores for this measure and subsequent rates of hospital readmission, suggesting that current self-care education does not reach the level needed to improve HF outcomes.9
The apparent lack of effectiveness of current self-care education may be due in part to the lack of reinforcement of key learning goals and behaviors. A single teaching session may be insufficient to ensure that patients are adequately prepared to meet the challenges of this complex condition. This may be compounded by the fact that many patients have low health literacy.2 Both written and oral patient education materials and instructions may contain unfamiliar words and concepts, resulting in low comprehension and failure of patients to adequately perform self-care behaviors. Low health literacy is especially common among the elderly,10 who also have the highest prevalence of heart failure.1 Despite the fact that low health literacy has been shown to be a risk factor for low knowledge and poor health outcomes,11, 12 most previous studies of self-care education programs have not examined whether their interventions were also effective for patients with low health literacy; one small single-center trial has shown that a literacy-sensitive intervention could improve self-care behaviors and health outcomes for patients with both high and low literacy.13
We conducted a multi-site randomized trial to examine the effect of two different levels of self-care training on the adoption of key self-care behaviors and on HF-related quality of life: a single educational session delivered by a health educator vs. a combination of a single educational session and a series of follow-up phone calls. The interventions were designed to minimize the number of learning goals and to communicate essential concepts clearly to patients regardless of their literacy level. We therefore also examined whether the benefits of the interventions differed by literacy level.
Methods
Overview
We conducted a randomized trial (ClinicalTrials.gov NCT00378950) of heart failure self-care education comparing a single in-person education session versus a more intensive goal-based education program that included the same single in-person education session plus a series of follow-up education phone calls. Details regarding study participant eligibility, recruitment procedures, and data collection processes have been previously described14 and are summarized here. The study protocol was approved by the Institutional Review Board Human Subjects Committee at all sites. The trial’s main outcomes of effect of the intervention on the incidence of hospitalizations and death at 6 and 12 months will be reported in future publications.
Participants
Study participants were enrolled from 2007 to 2009 from university-affiliated General Internal Medicine and Cardiology clinics at four sites: University of North Carolina (UNC); Northwestern University; University of California, San Francisco- San Francisco General Hospital; and Olive View-UCLA Medical Center. To be included in the study, each participant required a diagnosis of HF, New York Heart Association (NYHA) class II-IV symptoms in the past 6 months, current use of a loop diuretic, fluency in English or Spanish, and adequate cognitive functioning (based on the Mini-Cog screening tool).15
Recruitment, Baseline Interview, Initial Education, and Randomization
Potential participants were approached at regular outpatient appointments. Those agreeing to participate provided informed consent. Subsequently, the research assistant (RA) administered baseline questionnaires as described below. At the end of the baseline assessment, all participants received the initial educational session from the site’s health educator. Each site employed only one Masters’ level health educator; we ensured quality and consistency across sites through rigorous initial training and regular conference calls. The initial education session was approximately 40 minutes long and included review of daily self-assessment and action planning in case of exacerbation, salt avoidance, exercise, and medication adherence. Participants also received the Caring for Your Heart: Living Well with Heart Failure educational manual (http://www.nchealthliteracy.org/hfselfmanage.html) and a new digital scale for weighing themselves. After the initial education session, participants were randomized to either the intervention or control group, stratified by literacy.
Intervention Description
Those assigned to the control group (BEI) completed their session and continued with their usual care. Those assigned to the intervention group (TTG) received our more intensive education and self-care training intervention based on social cognitive theory and adult learning theory.14 The intervention included more specific instruction using daily weights to guide diuretic self-adjustment, including an individualized plan developed with the patient clinician.
Over the next 4 weeks, the intervention participant was scheduled to receive 5-8 follow-up phone calls from the educator to reinforce the education and to guide the patient toward better self-care skills, with each call lasting about 10 minutes. We chose this frequency based on our past research,13 our theoretical framework based on Social Cognitive Theory, and concerns about not overwhelming participants with too many calls. 14 During the first 2 calls, the health educator focused on reviewing the key behavior components of the program: performing daily weights, recording that weight, assessing for symptoms, taking the proper dose of diuretic according to their weight, and calling the doctor when appropriate. This information continued to be reviewed at every call to assess adherence. Calls 3 through 8 focused on the other three elements of HF self-care, including medication adherence, limiting salt, and exercise. The calls focused on reviewing the initial educational content, assessing the patient’s knowledge and behaviors, and providing additional information and encouragement.
Study Measures
During baseline interviews, we obtained race/ethnicity, insurance status, income, subjective socioeconomic status, years of education, and medication use. We abstracted age, gender, co-morbid conditions, prescribed medications, and diagnostic lab test and echocardiogram results from the medical chart. HF severity was assessed by interview and categorized by NYHA class. All interviews were conducted verbally in the language of choice (English or Spanish) by a trained research assistant fluent in the language. All items that had not previously been administered in Spanish were translated by native Spanish speakers by forward and back translation.
Literacy was measured with the Short-Test of Functional Health Literacy in Adults (S-TOFHLA) in either English or Spanish. The S-TOFHLA is a 36-item, 7-minute timed test of reading comprehension, and is a reliable, validated measure of literacy in the health care context.16, 17 Each participant’s literacy level was categorized (using standard cut-points) as either inadequate/marginal (0-22 correct answers), which we refer to as “low literacy,” or adequate literacy (23–36 correct).
Heart failure-related Quality of Life (HFQOL) was assessed at baseline using the Improving Chronic Illness Care Evaluation (ICICE) Heart Failure Symptom Scale (HFSS), a validated instrument that was adapted for phone interview from the Minnesota Living with Heart Failure Questionnaire and other HF health status scales.18 The HFSS consists of 7 questions with a 5-point response scale; scores were transformed to a 100-point scale with 100 representing the least possible symptoms/best health. The frame of reference for all items was the past 4 weeks. In prior work, a difference of 14 points on the 0-100 scale is roughly equivalent to a change in one level of NYHA classification.19
HF knowledge and self-care behaviors were assessed using an adapted version of the ICICE telephone survey.18 All knowledge questions were taken from specific learning goals in the education programs. The eight general HF knowledge questions included the definition of HF, how often someone with HF should weigh himself/herself, and identification of symptoms that were signs of worsening HF. The 10 salt knowledge questions included identification of foods with high salt content, knowledge of the “safe” amount of salt on a nutrition label, and why salt is bad for someone with HF. The ten-item self-care behavior scale included items related to weight monitoring, knowledge of target weight, knowing the appropriate responses to deal with a weight increase, efforts to decrease salt intake, and exercise frequency. Self-efficacy, a person’s perceived ability to do the things required to manage his/her HF or perform HF-related behaviors (e.g., tell whether their HF is getting worse, eat foods low in salt, explain symptoms to their doctor) was measured with a 10-item scale developed for this trial (Cronbach’s alpha = 0.81). Respondents rated each of the 10 self-efficacy questions using a 10-point response scale ranging from 1 (not sure) to 10 (absolutely sure). Participants’ responses were highly skewed with a modal response of 10; therefore, we dichotomized each item as a response of 10 (“absolutely sure,” which was assigned a 1) vs. 9 or less (“not absolutely sure’” assigned a 0).
Assessment at One Month
Patients were called by the UNC Survey Research Unit (SRU) on day 30 of the study (with Day 1 defined as the day of the initial in-person educational session) and a blinded interview conducted. If the first call was unsuccessful, the SRU would try every 3-7 days for up to 60 days, and the site research assistants would also attempt to contact the patient to either direct them to call the SRU or to conduct the interview themselves. After 60 days without contact, the patient was considered lost to follow-up.
Data Analysis
Data analyses were conducted using SAS (version 9.2; Cary, NC). We first assessed whether randomization achieved adequate balance between the study groups (BEI vs. TTG) for baseline demographic and clinical characteristics and whether there were differences between patients who completed or failed to complete the one-month follow-up survey (i.e., response bias). Independent sample t-tests were conducted for continuous variables and Chi-square tests for categorical variables. To assess changes in knowledge, self-efficacy, self-care behaviors, and HFSS scores between baseline and one-month follow-up for each study group (i.e., separately), we used paired t-tests. To assess differences in the change between the groups, we used an independent sample t-test (i.e., difference-in-differences). Despite randomization, we did find some significant differences in baseline characteristics between the TTG and BEI groups; therefore, we conducted linear regression analyses modeling the one month score as the dependent variable and adjusting for differences in baseline characteristics as independent variables.20 The results were similar and are not presented here. To test for heterogeneous treatment effects, we repeated analyses stratified by health literacy level. Secondary analyses were conducted to examine differences in the proportion of participants who responded correctly to individual items in the scales at each point in time (BEI vs. TTG).
Results
We identified 2848 patients who were potentially eligible for the study based on medical record review (Figure 1). A total of 1006 were never approached, 555 patients either refused (N=413) or had their physician refuse (N=142), and 682 were but found to be ineligible. The remaining 605 patients agreed to participate and were enrolled; 302 were randomized to the BEI group and 303 to the TTG group. The characteristics of the group are shown in Table 1. Mean age 60.7, 52% were male, and over 50% were non-White; 37% had low literacy skills. HFSS score also differed somewhat at baseline(63.0 ± 22.2 for the BEI group vs. 58.6 ±21.8 for the TTG group; p = 0.02).
Figure 1.
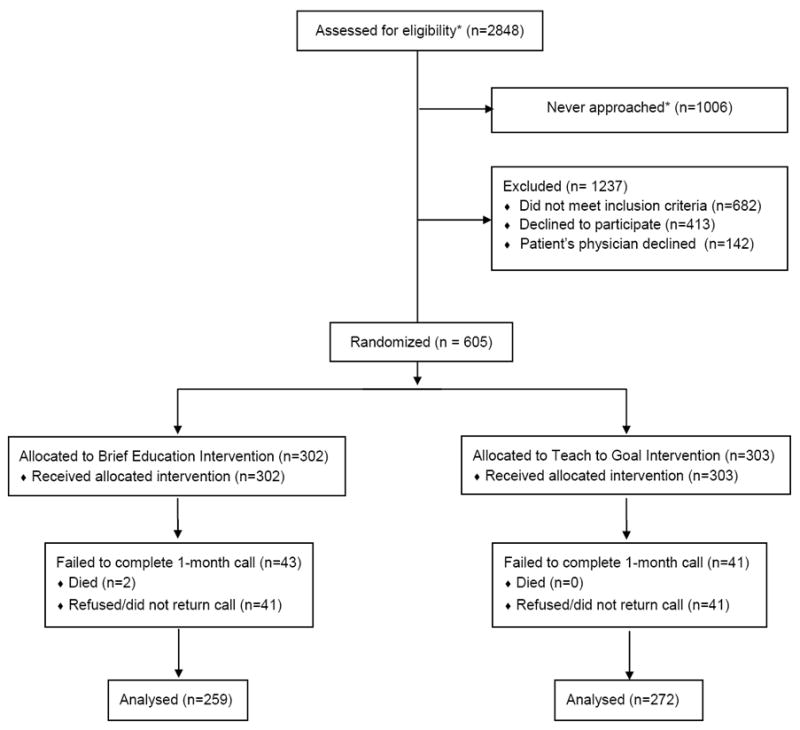
CONSORT Diagram Showing Participant Study Flow
*Some sites were able to identify potentially eligible patients using administrative and electronic health records. Not all patients were approached.
Table 1.
Baseline Demographic and Clinical Characteristics of Study Participants
| All Patients (N=605) | Brief Educational Intervention (N=302) | Teach to Goal (N=303) | P | |
|---|---|---|---|---|
|
| ||||
| Demographics
| ||||
| Site, N (%) | 1.00 | |||
| UNC | 216 (36) | 108 (36) | 108 (36) | |
| NU | 166 (27) | 83 (27) | 83 (27) | |
| UCSF | 148 (24) | 74 (25) | 74 (24) | |
| UCLA | 75 (12) | 37 (12) | 38 (13) | |
|
| ||||
| Age, mean ± SD | 60.7 ± 13.1 | 60.3 ± 12.3 | 61.1 ± 13.8 | 0.49 |
|
| ||||
| Race/Ethnicity, N (%) | 0.73 | |||
| White, non-Hispanic | 233 (39) | 122 (40) | 111 (37) | |
| Hispanic | 97 (16) | 43 (14) | 54 (18) | |
| African American | 232 (38) | 114 (38) | 118 (39) | |
| Other/ Missing | 43 (7) | 23 (7) | 19 (6) | |
|
| ||||
| Male, N (%) | 314 (52) | 156 (52) | 158 (52) | 0.90 |
|
| ||||
| Language: English, N (%) | 522 (87) | 261 (88) | 261 (87) | 0.67 |
|
| ||||
| Low Literacy by TOFHLA, N (%) | 225 (37) | 112 (37) | 113 (37) | 0.96 |
|
| ||||
| Annual Income, $, N (%) | 0.91 | |||
| <$15,000 | 305 (52) | 153 (52) | 152 (52) | |
| $15,000-40,000 | 159 (27) | 78 (27) | 82 (28) | |
| >40,000 | 125 (21) | 63 (21) | 62 (21) | |
|
| ||||
| Education Level, N(%) | 0.22 | |||
| <12th grade | 160 (26) | 78 (26) | 82 (27) | |
| High School | 177 (29) | 86 (28) | 91 (30) | |
| Some college | 140 (23) | 64 (21) | 76 (25) | |
| College graduate or greater | 128 (21) | 74 (25) | 54 (18) | |
|
| ||||
| Insurance, N(%) | 0.76 | |||
| Medicare | 298 (49) | 148 (49) | 150 (49) | |
| Medicaid | 151 (25) | 77 (25) | 74 (24) | |
| Private | 77 (13) | 35 (12) | 42 (14) | |
| Uninsured | 79 (13) | 42 (14) | 37 (12) | |
|
| ||||
| Clinical Characteristics
| ||||
| NYHA Class, N (%) | 0.89 | |||
| I | 114 (19) | 60 (20) | 54 (18) | |
| II | 304 (50) | 152 (50) | 152 (50) | |
| III | 118 (20) | 56 (19) | 62 (20) | |
| IV | 69 (11) | 34 (11) | 35 (12) | |
|
| ||||
| Heart Failure Symptom Score, Mean (SD) | 60.8 ± 22.1 | 63.0 ± 22.2 | 58.6 ± 21.8 | 0.02 |
|
| ||||
| Systolic Dysfunction: | 0.16 | |||
| LVEF < 45, N (%) | 355 (60) | 186 (62) | 169 (57) | |
|
| ||||
| Systolic blood pressure (mm/Hg), mean (SD) | 124.8 ± 22.7 | 124.2 ± 21.7 | 125.3 ±23.7 | 0.58 |
|
| ||||
| Diastolic blood pressure (mm/Hg), mean (SD) | 71.3 ± 12.9 | 71.8 ± 13.5 | 70.8 ±12.3 | 0.34 |
|
| ||||
| Body Mass index (kg/m2), mean (SD) | 33.1 ± 8.9 | 33.8 ± 9.0 | 32.5 ± 8.7 | 0.09 |
|
| ||||
| Creatinine level (mg/dl), mean (SD) | 1.3 ± .5 | 1.2 ± .5 | 1.3 ± .6 | 0.19 |
|
| ||||
| Diabetes, N (%) | 290 (48) | 140 (46) | 150 (50) | 0.44 |
|
| ||||
| Hypertension, N (%) | 513 (85) | 257 (85) | 256 (84) | 0.83 |
|
| ||||
| Previous MI or angina, N (%) | 230 (38) | 112 (37) | 118 (39) | 0.64 |
|
| ||||
| Current smoker, N (%) | 96 (16) | 50 (17) | 46 (15) | 0.64 |
|
| ||||
| Medication Hx | ||||
| ACE-I, N (%) | 391 (66) | 200 (67) | 191 (64) | 0.37 |
| ARB, N (%) | 120 (20) | 64 (21) | 56 (18) | 0.39 |
| ACE-I or ARB, N (%) | 497 (82) | 258 (85) | 239 (79) | 0.04 |
| Beta blocker, N (%) | 492 (82) | 251 (84) | 241 (80) | 0.16 |
| Spironolactone, N (%) | 166 (27) | 90 (30) | 76 (25) | 0.20 |
SD - Standard Deviation; UNC- University of North Carolina; NU – Northwestern University; UCSF – University of California San Francisco, San Francisco General Hospital; University of California Los Angeles; TOFHLA - Test of Functional Health Literacy in Adults, short version; NYHA-New York Heart Association; LVEF – left ventricular ejection fraction; MI – myocardial infarction; ACE-I – angiotensin converting enzyme inhibitor; ARB – angiotensin receptor blocker
Individuals with Medicare are included in this category regardless of whether they had supplemental or private insurance.
During the 30 day study period, 2 patients died (both in the BEI group), and 72 (11.7%) patients did not complete the one-month assessment call (41 in the BEI group and 31 in the TTG group), leaving 259 patients in the BEI group and 272 in the TTG group. Response rates were similar for the BEI (86%) and the TTG (90%) groups. Non-responders had lower literacy, less education, lower annual income, and worse heart failure symptoms, and were more likely to have been enrolled at UCSF/San Francisco General Hospital (p < 0.05 for all). Among the intervention group, the median number of calls completed was 4.0 (interquartile range 3 – 5).
Changes in General Heart Failure and Salt Knowledge
The TTG group had a significantly greater increase in general knowledge compared to the BEI group (0.70 vs. 0.30, p = 0.008; Table 2). The amount of net improvement was similar for individuals with inadequate/marginal literacy and those with adequate literacy (Table 2).
Table 2.
Mean (± SD) General Knowledge, Salt Knowledge, and Self-Efficacy Scores at Baseline and the One-Month Follow-up Telephone Interview for Patients in the Brief Educational Intervention (BEI) and the Teach to Goal (TTG) Groups, Including Stratified Analyses According to Functional Health Literacy.*
| Baseline | Follow Up | Absolute Change: Baseline to Follow-Up | Net Difference in Change Between Groups | |||||
|---|---|---|---|---|---|---|---|---|
| BEI | TTG | BEI | TTG | BEI | TTG | Difference (95% CI) | P | |
| General Knowledge (8 items)
| ||||||||
| Overall | 6.3 ±1.8 | 6.1 ±1.8 | 6.6 ±1.6 | 6.8 ±1.5 | +0.30 | +0.70 | 0.40 (0.11, 0.69) | 0.008 |
| Inadequate/ Marginal | 5.5 ±1.9 | 5.4 ±2.0 | 5.9 ±1.9 | 6.2 ±1.7 | +0.32 | +0.80 | 0.48 (-0.13, 1.09) | 0.12 |
| Adequate | 6.6 ±1.6 | 6.5 ±1.6 | 6.9 ±1.3 | 7.1 ±1.2 | +0.29 | +0.65 | 0.35 (0.04, 0.67) | 0.03 |
|
| ||||||||
| Salt Knowledge (10 items)
| ||||||||
| Overall | 7.7 ±1.4 | 7.4 ±1.5 | 8.1 ±1.6 | 8.3 ±1.5 | +0.37 | +0.90 | 0.52 (0.26, 0.79) | <0.001 |
| Inadequate/ Marginal | 7.3 ±1.6 | 6.8 ±1.7 | 7.4 ±1.9 | 7.5 ±1.6 | +0.12 | +0.71 | 0.59 (0.04, 1.15) | 0.04 |
| Adequate | 7.9 ±1.2 | 7.7 ±1.3 | 8.4 ±1.4 | 8.7 ±1.2 | +0.50 | +0.99 | 0.50 (0.21, 0.78) | 0.001 |
|
| ||||||||
| Self-Efficacy (10 items)
| ||||||||
| Overall | 5.0 ±2.8 | 4.8 ±2.8 | 5.4 ±3.2 | 5.8 ±3.0 | +0.38 | +1.01 | 0.63 (0.16, 1.10) | 0.009 |
| Inadequate/Marginal | 4.8 ±2.8 | 4.3 ±2.7 | 5.0 ±3.4 | 5.2 ±3.1 | +0.19 | +0.90 | 0.71 (-0.20, 1.63) | 0.13 |
| Adequate | 5.1 ±2.8 | 5.0 ±2.8 | 5.6 ±3.1 | 6.1 ±2.9 | +0.47 | +1.06 | 0.59 (0.05, 1.14) | 0.03 |
Health Literacy was measured with the short version of the Test of Functional Health Literacy in Adults.
SD indicated standard deviation and CI indicates confidence interval.
The proportion of people who said that weight gain is a sign of worsening heart failure increased from 67.4% to 74.0% in the BEI group and from 66.2% to 81.6% in the TTG group (change 6.5% vs. 15.4%, respectively), and the proportion of people who said that someone with heart failure should weigh himself several times per week or more increased from 59.4% to 79.7% in the BEI group and from 58.7% to 87.6% in the TTG group (change 20.3% vs. 29.0%, respectively). (See Appendix 1 for other individual knowledge items). Several items had high baseline knowledge, making it difficult to achieve improvement. For example, approximately 80% of all patients knew that shortness of breath, swelling of the legs or ankles, and waking up short of breath were signs of heart failure. The TTG group also had a significantly greater increase in salt knowledge compared to the BEI group (0.90 vs. 0.37, p < 0.001; Table 2). Knowledge of the “safe” amount of sodium per serving on a nutrition label increased from 9% to 37% in the BEI group and from 10% to 55% in the TTG group (p=0.001). The magnitude of improvement with TTG compared to BEI was similar for both literacy strata (Table 2).
Changes in Self-Efficacy
Patients in the TTG group had a significantly greater increase in self-efficacy than those in the BEI group. Self-efficacy increased from 5.0 (± 2.8) to 5.4 (± 3.2) in the BEI group and from 4.8 (± 2.8) to 5.8 (± 3.0) in the TTG group (change 0.4 vs. 1.0, respectively; p = 0.006 for comparison of the change between groups; Table 2). The results were similar regardless of literacy level (Table 2). Almost all of the self-efficacy items improved more in the TTG group (see Appendix 2).
Changes in Self-Care Behaviors
Both the TTG and the BEI groups showed substantial, statistically significant increases in self-care behaviors (Figure 2). On the 10-point self-care behavior scale, the score increased from 4.9 (± 2.0) to 6.6 (± 1.8) in the BEI group (p < 0.001) and from 4.4 (± 2.0) to 7.6 (± 1.8) in the TTG group (p < 0.001. However, the improvement was significantly greater for the TTG group (change 1.8 vs. 3.2, respectively; p < 0.001 for the difference in the change between groups). The magnitude of the improvements in self-care behaviors and the differences between the BEI and TTG groups were very similar regardless of literacy level (Figure 2). For the BEI group, individuals with marginal/inadequate literacy improved by 1.6 points and those with adequate literacy improved by 1.5. Among those in the TTG group, the improvements were 2.7 and 2.8 for those with inadequate/marginal and adequate literacy, respectively. These trends were similar for all for all self-care behavior items except for exercising ten or more minutes three or more days per week (see Appendix 3).
Figure 2.
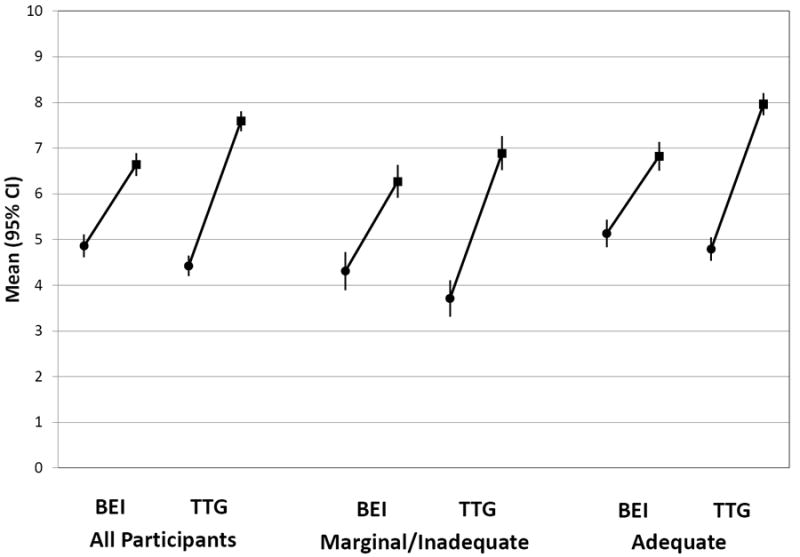
Mean Self-Care Scores (95% CI) at Baseline (●) and One-Month Follow-Up (■) for the Brief Educational Intervention (BEI) and the Teach to Goal (TTG) Groups, Stratified by Health Literacy Level (Adequate and Marginal/Inadequate).
CI indicates confidence intervals
Changes in Heart Failure-related Quality of Life
Among patients in the BEI group, the HFSS (our measure of heart failure-related quality of life) at baseline was 64.8 (± 22.4), and at the one-month outcome assessment it was unchanged at 64.1 (± 22.8). In contrast, the HFSS for patients in the TTG group improved from 58.6 (± 22.2) at baseline to 65.3 (± 22.4) at the one-month assessment. The change was -0.6 vs. 6.7, respectively, for the BEI and the TTG groups (p < 0.001 for comparison of the change between the two groups; Figure 3). The greater improvement with TTG was present for participants with both low and adequate literacy, although among patients in the TTG group, those with inadequate/marginal literacy improved somewhat more than those with adequate literacy (9.4 vs. 5.3 point increase, respectively).
Figure 3.
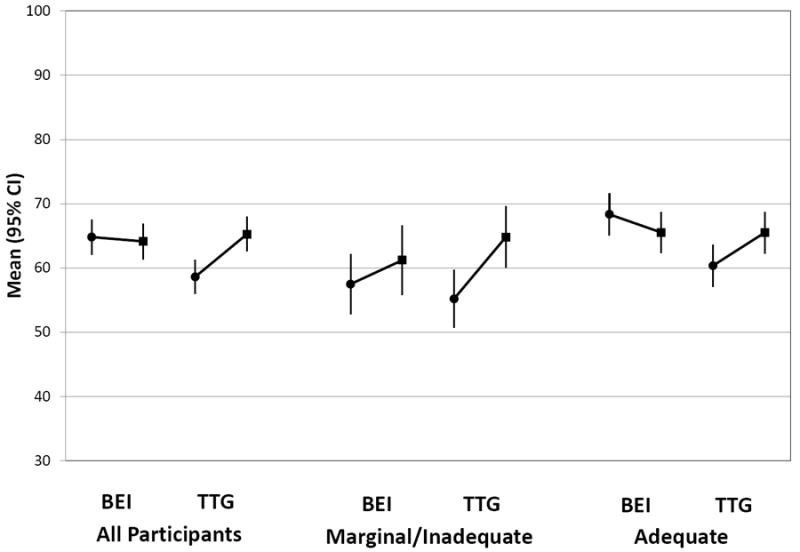
Mean Heart Failure Symptom Score (95% CI) at Baseline (●) and One-Month Follow-Up (■) for the Brief Educational Intervention (BEI) and the Teach to Goal (TTG) Groups, Stratified by Health Literacy Level (Adequate and Marginal/Inadequate).
CI indicates confidence intervals
Discussion
Our results show that compared to a single education session (BEI group), the TTG program that reinforced learning goals and behaviors with 5-8 telephone counseling sessions over the next month (including teaching adjusted-dose diuretics to maintain a target weight) resulted in slightly greater knowledge, substantially better achievement of self-care goals, higher self-efficacy, and greater improvement in heart failure symptoms. Teaching persons with HF proper self-care skills is important for achieving optimal health outcomes and minimizing preventable hospitalizations.2 In the four trials investigating patient self-care education (as distinct from a complete disease management program), HF-specific hospitalizations were reduced by 34%.3 However, the educational methods, intensity, duration, and reinforcement needed to achieve optimal outcomes are unclear,2 and few studies have examined these issues. A one-hour teaching session at the time of hospital discharge increased self-care practices and decreased the combined outcome of death or re-hospitalization compared to the standard discharge process.21
The TTG program was equally efficacious for patients with inadequate/marginal literacy as for those with adequate literacy. Both subgroups showed improvement in knowledge, self-care behaviors, self-efficacy, and HF symptom scores, and the TTG intervention was better than the BEI intervention for both subgroups. An American Heart Association Scientific Statement on Promoting Self-Care in Persons with Heart Failure identified poor health literacy as a factor that impedes self-care management.2 Previous studies of self-care education and skills training have either not measured health literacy or not been adequately powered to determine whether interventions are similarly efficacious for patients with poor health literacy. The TTG intervention was specifically designed to overcome the factors that impede learning and behavior change for persons with poor health literacy. Our results provide encouraging evidence that these impediments can be overcome with interventions that are designed according to theoretical principles of instructional design and behavior change and that provide more intensive education and skills training with repetition and reinforcement over time. However, participants with poor health literacy had worse baseline knowledge, behaviors, and self-efficacy compared to those with adequate literacy, and our intervention did not significantly reduce the difference between them. Thus, further research is needed to find ways to overcome the barriers to learning and behavior change posed by poor health literacy and to eliminate the disparities that result from these.
Despite the limited learning goals, structured curriculum design, and reinforcement with telephone calls, the gains in knowledge for the TTG intervention were modest. Some of this may be explained by the high baseline knowledge of study participants. Most of the patients we enrolled had HF for many years. However, 24% of patients did not know that shortness of breath was a sign of heart failure, and there was no improvement in this among either group.
Similarly, 16% did not know that leg or ankle swelling was a sign of heart failure, and even among the TTG group, only half learned this over the one-month follow-up. Future studies should explore alternative ways of teaching these fundamental self-monitoring concepts to patients, such as video instead of static images. It may be easier to teach this to patients when they are in the midst of an exacerbation rather than the stable outpatients that we enrolled. Knowledge of high-salt foods was also high at baseline, and improvement was likely limited by ceiling effects.
Self-care behaviors and self-efficacy improved much more than knowledge, which suggests that knowledge and behaviors (and changes in the two) are not tightly linked. While theoretical models and practical experience say that knowledge is necessary but not sufficient for behavior change, it remains unclear how much knowledge and what particular learning goals are essential. When designing our intervention, we worked hard to eliminate non-essential information, but our findings suggest that even less educational content and greater emphasis on self-care behaviors may be more effective.
There are several important issues to consider when interpreting our findings. We mostly enrolled established patients who already had high knowledge, and many had advanced skills in HF self- management (e.g., knew about adjusting their diuretic dose to maintain a target weight). It is likely that the benefits of the TTG intervention compared to the BEI would have been even greater among patients hearing this information for the first time. In addition, we believe that the baseline education session received by the BEI group is probably more intensive than what many patients receive. Because we had an active comparison group that is often better than usual care, the benefits achieved by implementation of the TTG intervention could be substantially greater in actual practice than what we report here. It is also possible that our study overestimated the effect size of the TTG intervention. Patients with adequate literacy who were randomized to the TTG group had worse baseline HF symptom scores than those randomized to the BEI group (Figure 3). If by chance those with adequate literacy randomized to the TTG group had worse baseline HFSS scores on the day of the baseline interview, regression to the mean could lead to an overestimate of their improvement in HF symptoms scores at the follow-up interview and an overestimate of the difference in improvement between the TTG and BEI groups. We found no evidence of unblinding or measurement bias, and the results did not change when we conducted a multivariate analysis that adjusted for differences in baseline HFSS scores. Finally, the intervention was multifaceted, and we cannot determine whether the greater improvement in HFQOL in the TTG group was due to greater improvements in knowledge, self-efficacy, self-care behaviors, or some other direct effect of the intervention.
This study has important implications for health care providers and policy-makers. Disease management programs can improve health outcomes and reduce costs.3 However, it remains unclear what the marginal benefits are for single session education, structured follow-up telephone calls to reinforce teaching goals and self-care behaviors, and more intensive remote monitoring by health professionals. Our findings show that follow-up telephone calls (without remote monitoring of signs and symptoms) incrementally improve knowledge, self-care, and HF symptoms beyond a single, intensive face-to-face teaching session; this incremental benefit can be achieved even for patients with low literacy who may struggle to master critical self-care behaviors. Longer follow-up of this study population is needed to understand what proportion of patients can sustain high-level mastery and regular performance of self-care behaviors and whether this results in sustained improvements in symptoms and reductions in hospitalizations and death. Patients who master and regularly perform self-care behaviors may not need more intensive and expensive remote monitoring, while others who fail to achieve self-care goals may greatly benefit from this extra support. Additional studies will be needed to elucidate the health benefits and incremental cost-effectiveness of these strategies.
Supplementary Material
Acknowledgments
This study was supported by the National Heart Lung and Blood Institute (grant number R01 HL081257).
Footnotes
Disclosures
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trial Registration - URL: http://www.clinicaltrials.gov/. Unique identifier: NCT00378950
References
- 1.Lloyd-Jones D, A R, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2010 Update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Riegel B, M D, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 3.McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–9. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 4.Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord. 2006;6:43. doi: 10.1186/1471-2261-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yehle KS, Plake KS. Self-efficacy and educational interventions in heart failure: a review of the literature. J Cardiovasc Nurs. 2010 May-Jun;25(3):175–88. doi: 10.1097/JCN.0b013e3181c71e8e. [DOI] [PubMed] [Google Scholar]
- 6.Cameron J, Worrall-Carter L, Driscoll A, Stewart S. Measuring self-care in chronic heart failure: a review of the psychometric properties of clinical instruments. J Cardiovasc Nurs. 2009 Nov-Dec;24(6):E10–22. doi: 10.1097/JCN.0b013e3181b5660f. [DOI] [PubMed] [Google Scholar]
- 7.Fredericks S, Beanlands H, Spalding K, Da Silva M. Effects of the characteristics of teaching on the outcomes of heart failure patient education interventions: a systematic review. Eur J Cardiovasc Nurs. 2010 Mar;9(1):30–7. doi: 10.1016/j.ejcnurse.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Overview of Specifications of Measures Displayed on Hospital Compare as of December 14, 2006. [Sept. 7, 2010]; Available from: http://www.cms.gov/HospitalQualityInits/downloads/HospitalOverviewOfSpecs200512.pdf.
- 9.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361:2637–45. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 10.Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–82. [PubMed] [Google Scholar]
- 11.Nielson-Bohlman L, Panzer A, Kindig D, editors. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 12.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006 Mar 13;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeWalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes M, Weinberger M, Macabasco-O’Connell A, Pignone M. Comparison of a one-time educational intervention to a teach-to-goal educational intervention for self-management of heart failure: design of a randomized controlled trial. BMC Health Serv Res. 2009;9:99. doi: 10.1186/1472-6963-9-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borson S, Scanlan JM, Brush M, Vitallano P, Dokmak A. The Mini-Cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. International Journal of Geriatric Psychiatry. 2000;15(11):1021–1027. doi: 10.1002/1099-1166(200011)15:11<1021::aid-gps234>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 16.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 17.Kandula NR, Nsiah-Kumi PA, Makoul G, Sager J, Zei CP, Glass S, Stephens Q, Baker DW. The relationship between health literacy and knowledge improvement after a multimedia type 2 diabetes education program. Patient Educ Couns. 2009;75:321–7. doi: 10.1016/j.pec.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Baker DW, Brown J, Chan KS, Dracup KA, Keeler EB. A telephone survey to measure communication, education, self-management, and health status for patients with heart failure: the Improving Chronic Illness Care Evaluation (ICICE) J Card Fail. 2005;11:36–42. doi: 10.1016/j.cardfail.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Macabasco-O’Connell A, Dewalt DA, Broucksou KA, Hawk V, Baker DW, Schillinger D, Ruo B, Bibbins-Domingo K, Holmes GM, Erman B, Weinberger M, Pignone M. Relationship Between Literacy, Knowledge, Self-Care Behaviors, and Heart Failure-Related Quality of Life Among Patients With Heart Failure. J Gen Intern Med. 2011 Mar 3; doi: 10.1007/s11606-011-1668-y. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vickers AJ, Altman DG. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–4. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111:179–85. doi: 10.1161/01.CIR.0000151811.53450.B8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


