Abstract
Objective
To evaluate the effectiveness of Safe Thinking and Affect Regulation (STAR), a 14-session HIV-prevention program for adolescents at alternative/therapeutic schools. Because these youth frequently have difficulties with emotions and cognitions, it was designed to improve sexuality specific affect management and cognitive monitoring, as well as HIV-related knowledge and attitudes. It was hypothesized that STAR would lead to a decrease in sexual risk and improved HIV knowledge and attitudes.
Method
Fourteen schools were randomly assigned by year either to the STAR intervention or a brief educational program. Schools received the alternate intervention the following year. 185 adolescents in 29 cohorts (groups) participated in the interventions. Assessment of sexual behavior, knowledge and attitudes with audio computer-assisted self-interviews occurred at three, six and nine months post intervention.
Results
Hierarchical Linear Model (HLM) analyses found that adolescents in the STAR intervention reported a significantly greater decrease (p < .05) in the Sexual Risk Index than youth in the control group over the six months post intervention and similar improvements in the HIV Knowledge Scale and the Condom Use Self Efficacy Scale. There were no group differences between six and nine months post intervention.
Conclusions
This STAR intervention for youth in alternative schools was associated with decreased sexual risk for six months after the intervention. These data suggest that intervention strategies that target cognitions and affect within a sexual context might be usefully applied to improving sexual behavior but may need to be reinforced over time.
Keywords: sexual risk, adolescents, HIV prevention, alternative schools
Each year, approximately half of all new sexually transmitted infections (STIs), and one third of new cases of Human Immunodeficiency Virus infection (HIV), occur in youth 13 to 29 years of age.1-3 These data underscore the fact that adolescents are at risk for HIV and that effective prevention programs need to reach young people. Alternative or therapeutic schools enroll those who function poorly in traditional academic settings, often due to behavioral or emotional difficulties, and have specialized programs to address these needs. Youth in these schools are at greater risk for HIV and other sexually transmitted diseases than their peers and thus are a critical target for prevention. For example 86% of adolescents in alternative high schools report having engaged in sexual intercourse, as compared with 48% of those attending regular schools. Importantly, less than half (47%) of youth attending alternative schools reported using a condom at most recent sex.4
Effective programs to reduce sexual risk among youth exist and their impact has been demonstrated in diverse groups such as African American community adolescents5,6 homeless youth7,8 and in traditional schools.9-11 Four studies have reported on programs specifically for youth in psychiatric treatment, a population that shares many similarities with youth in alternative schools.12-16 All programs were acceptable to students and appeared to improve attitudes for safer sex, consistent with effective programs in other populations. However, none identified emotional or cognitive factors specific to these youth as intervention targets. In addition, the projects were limited by small sample sizes and lack of behavioral data following the intervention. Most effective programs have been based on some variation of Social Learning Theory.16 Generally such programs increase personal motivation to stay safe from HIV, improve social norms about sex and teach safer sex skills.
Alternative schools are a unique setting comprised of high-risk youth who have not been able to succeed in traditional school environments. Youth attending alternative school settings evidence higher rates of psychiatric disorders, substance abuse, learning disorders, and academic difficulties as well as more frequent histories of sexual abuse.17,18 Thus, consistent with evidence that a range of psychiatric and behavioral concerns tend to cluster with HIV-risk behaviors19, youth attending alternative schools frequently experience numerous concerns that place them at elevated risk for contracting HIV or other sexually transmitted infections. Alternative and therapeutic schools have not been targeted for prevention. It is possible that the factors associated with increased sex risk for certain youth, such as academic, emotional and behavioral difficulties, may interfere with their ability to benefit from programs based on traditional prevention models (such as basic education, social learning, or social inoculation models)20-22. Although there are many merits to universal prevention programs, efforts aimed at youth at greater risk, such as interventions in alternative school settings, may be more successful than universal programs if they address risk factors that are especially applicable for the at-risk adolescents.
Safe Thinking and Affect Regulation (STAR) is a 14-session HIV-prevention intervention that was tailored to provide a range of skills that influence successful engagement in safe-sex behaviors specifically for youth attending alternative schools.23 The STAR intervention was developed to address skills deficits, such as difficulties with affect regulation and poor cognitive monitoring, that are associated with maladaptive behaviors among these at-risk youth. As summarized in Table 1, the STAR intervention applied principles of Dialectical Behavior Therapy (DBT)24 adapted to the unique developmental and learning needs of youth attending alternative schools, to address these deficits specifically in the context of sexual situations. Dysfunctional thinking was explained as “safe vs. unsafe” thoughts that influence behavior and the examples and practice pertained to sex behaviors. Several strategies improved affect management so that adolescents could use safer sex behaviors effectively. For example youth practiced recognizing and labeling feelings, developed skills to quantify feelings, discussed the negative outcomes of poor affect management, and practiced distress tolerance skills. The intervention also provided basic skills about communication, abstinence and condom use as well as information about HIV/AIDS, sexuality, and healthy relationships.
The present investigation is a randomized controlled longitudinal investigation of sex risk behaviors in youth attending alternative schools, comparing the STAR intervention to a brief educational control intervention. We hypothesized that youth participating in the STAR intervention, compared to youth participating in the control intervention, would report decreased sexual risk, improved HIV knowledge, and more positive attitudes about the use of condoms. Since HIV prevention programs have not targeted alternative or therapeutic schools, a brief educational comparison condition was chosen and was designed to deliver factual HIV/AIDS information in an engaging format in order to ensure that all youth were exposed to relevant facts. It was hypothesized that the positive impact would last for as long as six months after the conclusion of the intervention, similar to other efficacious prevention programs.5,25-29 The impact of prevention programs among adolescents is not always sustained30 so a 9 month post intervention assessment was designed to test the longer term impact.
Method
Randomization and Schedule of Activities
Fourteen schools were randomized to either the STAR intervention or control groups during their initial school year of participation in the program. In subsequent school years, schools received the alternate intervention. In this way, each school received both interventions, controlling for potential school-related differences. In addition, administering only one intervention condition during the school year minimized potential crosstalk between classmates receiving alternate interventions since the average length of time for students in the schools was one year. Typically, the first STAR intervention session began in September of the first school year and was completed in December. Three, six and nine month post intervention assessments then occurred the following March, June and September. The alternate intervention was not begun in the second year until the final first year assessment had been completed but few adolescents from the first year were still in the alternative school during the second intervention year. The second year intervention was conducted with new youth assessments at similar intervals.
Study Procedures
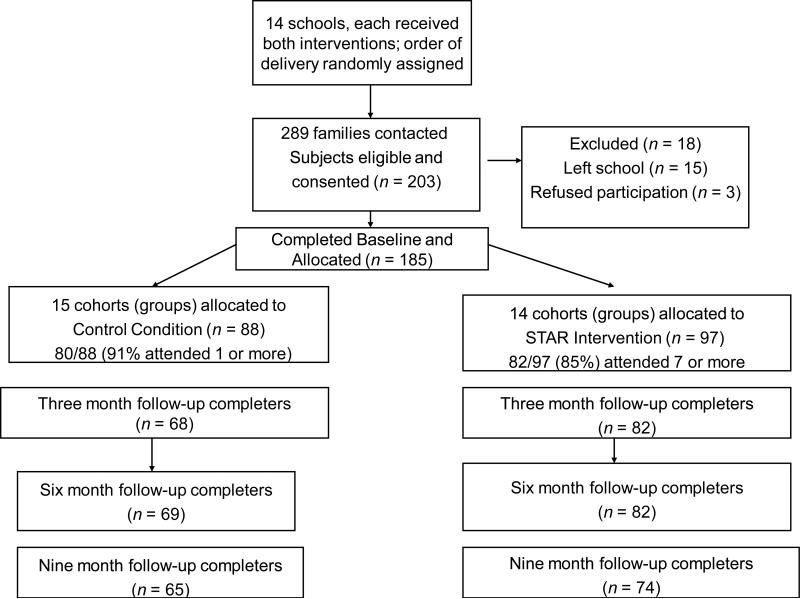
The hospital institutional review board approved all study protocols. Informed consent was obtained from all participants 18 years or older and assent from youth less than 18 and consent from minors’ parents or guardians. Potentially eligible youth between 12 and 19 years of age were identified by school staff who contacted youth or their families, as appropriate, for permission to provide contact information to study staff. Two hundred eighty-nine families (approximately 85% of the youth in available classes) with children in the eligible age range agreed to initial contact with researchers to learn about the project. Of those 289 families, 203 families (70%) were eligible and were consented for participation (resulting in approximately 60% of youth in the classes enrolled). Many were excluded because of an anticipated discharge or transfer. See Figure 1 for the Consolidated Standards of Reporting Trials (CONSORT)31 flowchart of the numbers of cohorts (groups), participant consent, randomization, and retention throughout the study.
Figure 1.
Participant consent, randomization, and retention (CONSORT flowchart) for Project STAR (Safe Thinking and Affect Regulation).
Participants
As shown in Figure 1, 29 cohorts of adolescents from the fourteen schools participated in the interventions, with each school receiving both interventions but in different years and with different youth. 203 adolescents were consented for the study and 18 did not participate, primarily because they left the school prior to the start of the interventions. The 185 participants consisted of 185 youth ages 12-19 recruited from 2004 to 2008. Exclusion criteria included current pregnancy, recent childbirth, self-reported HIV infection, cognitive limitation preventing group participation or assessment, history of sexual aggression, or likelihood of being discharged prior to the conclusion of the intervention period. Participants were primarily female (61%) and White (57%), similar to the majority of youth in the participating schools. The STAR intervention condition was comprised of 97 students in 14 cohorts and control participants were 88 youth in 15 cohorts. All cohorts were followed up to 9 months after the intervention.
Assessments
Audio computer-assisted self-interviews (ACASI) were administered on laptop computers to ensure privacy to students at baseline and at follow-up assessments that occurred at 3 months, 6 months, and 9 months after the final intervention session. Participants were asked about the previous 90 days and were provided a standard script instructing them to consider significant events of the last three months to assist in recall. Trained research staff supervised completion of the measures and answered participant questions as they arose; school staff did not participate in study procedures. Adolescents were compensated ($20) at each time point for their time related to completing questionnaires.
STAR Intervention
Participants in the intervention condition participated in 14 sessions (45 minutes each) conducted during the school day. The first 13 sessions were conducted weekly, followed by a booster session one month later. The theoretical framework was based on Social Learning Theory and Dialectical Behavior Therapy. A more complete rationale for the intervention elements of Project STAR have been described elsewhere.23,32 Table 1 provides a summary of each session. Briefly, the scripted intervention sessions employed an interactive psycho-educational format using didactic instruction, games, role plays, and group discussion. Sessions focused on basic skills relevant to communication, abstinence and condom use, as well as information about HIV/AIDS, sexuality, and healthy relationships. Affect management skills (e.g., identifying and labeling emotions) and distress tolerance skills (e.g., breathing, imagery) were taught to reduce distress that might occur during sexual situations. To enhance cognitivemonitoring skills, youth were taught to challenge dysfunctional thinking related to sexual behaviors and to replace these thoughts with more healthy cognitions. Finally, youth practiced affect management and cognitive monitoring skills while learning sex-specific skills (e.g., condom application) and while role-playing key sex-related communication scenarios (e.g., condom negotiation, sexual refusal).
Control Intervention
Since HIV prevention programs have not targeted alternative or therapeutic schools, a brief educational comparison condition was chosen. It delivered recent factual HIV/AIDS information in an engaging format in order to ensure that all youth were exposed to relevant facts and to be compatible with state guidelines for HIV/AIDS education. The educational content related information about HIV/AIDS, including sexual anatomy, sexually transmitted diseases, and methods of transmission (see Table 1).
Intervention Dose
Ninety-one percent of control participants and 85% of treatment participants attended at least 50% of the sessions (1 out of 2 sessions for control and 7 out of 14 sessions for treatment).
Intervention Fidelity
Fidelity was enhanced by methods recommended for health change interventions to standardize training, minimize “drift” in provider skills, and increase adherence to intervention protocol33. Sessions were conducted using a scripted treatment manual. Groups of four to eight students were led by two research staff facilitators, including a clinician with at least a master's degree in psychology and a Bachelor-level research assistant. Training consisted of role plays of each session in which research team members acted as participants. Investigators observed facilitators delivering each session before they were deemed competent. To ensure adherence to the scripted intervention and to reduce “drift,” investigators observed at least 20% of intervention sessions. Adherence to protocol was rated on a 5-point scale (1 = very well to 5 = not very well) that assessed each of the six to seven major session activities (e.g. “Safe Thoughts Game”, “Living with AIDS”), 90% of which were rated as having been done “very well.” Facilitators were also rated on general performance (e.g. “Listened well,” “Had an active and engaging style”) across activities on the same five point scale and over 90% of items were rated as “well” or “very well.”
Measures
Sexual behaviors
Sexual behaviors were assessed via ACASI using a skip pattern in which respondents were first asked whether they had ever engaged in anal or vaginal intercourse. Oral sex was not assessed since few adolescents report only oral without vaginal or anal sex experience.34 Participants who endorsed having engaged in any penetrative sexual activities were subsequently asked to indicate the number of times they had engaged in vaginal or anal sex in the last 90 days, reporting separately on number of occasions of protected and unprotected sex acts. To include the level of sexual risk of subjects who were not sexually active or who had sex infrequently, an alternative to the count of unprotected sex acts, which tends to be highly skewed at both ends of the distribution35, was used. A composite index of sexual risk was created (Sexual Risk Index), with participants reporting: no lifetime history of sex assigned a risk score of 0, prior experience with sex but no sex during the past 90 days assigned a score of 1, 100% condom use during sex over the last 90 days assigned 2, inconsistent condom use during sex over the last 90 days assigned 3, and no condom use during sexual encounters in last 90 days assigned 4.
HIV Knowledge
This scale assessed adolescent knowledge of HIV/AIDS and condom use behavior. Adolescents responded “true,” “false,” or “I don't know” (which was coded as incorrect) to 20 statements, such as “A birth control pill will protect you against AIDS.” Cronbach's alpha for the current sample was 69. Higher scores indicate greater knowledge.36
Condom Use Self-Efficacy
Adolescents completed 13 items measuring perceived abilities to use condoms in specific contexts (e.g., “How sure are you that you could use a condom when.... you are depressed ...your partner doesn't want to use one.”). Participants responded on a 4-point scale (“very sure I could” to “very sure I couldn't”); alpha for the sample was .94. Higher scores indicate greater self-efficacy.37
Advantages of Condom Use
This 13-item scale measured adolescents’ perceived benefits and drawbacks to condom use. Items such as “I would feel safer” or “My partner would be angry” were rated on a 5-point scale (“not at all important” to “very important”). Cronbach's alpha for the sample was .78. Higher scores indicate greater perceived advantage to using condoms.37
Negative Condom Use Expectations
Six items assessed adolescents’ expectations around condom use (e.g., “Condoms ruin the mood”) on a 5-point scale (“strongly disagree” to “strongly agree”). Alpha for this sample was .79. Higher scores indicate more negative expectations regarding the use of condoms.38
Symptoms of distress and a history of childhood trauma were assessed because these factors have been shown to be associated with sexual risk.39 The Global Severity Index (GSI) of the Brief Symptom Inventory-18 (BSI) is an abbreviated measure of distress including self-reported symptoms of depression, anxiety, and somatization.40 It has been used previously with adolescents41,42. Participants endorse one of five Likert-type responses (ranging from 1 = not at all to 5 = extremely) to indicate the extent to which they have been “distressed or bothered” by each symptom in the past 7 days. In this study, it demonstrated a Cronbach's α = .91. The Childhood Trauma Questionnaire (CTQ) is a widely-used 28-item retrospective self-report measure of trauma with subscales for sexual abuse, emotional abuse, physical abuse, emotional neglect, and physical neglect.43 Prior research supports the use of the measure as a reliable and valid index of childhood traumatic experiences44,45. Internal consistency of the subscale: Sexual abuse α = .93; Emotional abuse α = .87; Physical abuse α = .92 ; Emotional neglect α = .85 ; and Physical neglect α = .79 .
Data Analysis
Data screening was conducted for all time-points. There were no significant concerns with skewness or kurtosis and no significant outlying cases. Baseline demographics were compared between the treatment and control group using t-tests for continuous variables and χ2 tests for categorical variables. We also compared dropout rates between the treatment and control groups. All data screening and baseline analyses were performed using SPSS 17.0 for Windows.
Three-level mixed models were used to account for the nested nature of these data. Assessments were nested within participants who were nested within 29 groups ranging in size from four to nine. To match group-level randomization procedures, intervention effects were tested at the third- or group-level. Mixed models not only address nesting but also address missing data through the application of full information maximum likelihood estimation, an approach that tests an intent-to-treat model (e.g., includes all participants who were randomized to a treatment condition) and produces less biased estimates than approaches such as last observation carried forward46. Tests of both initial intervention effects and maintenance of effects were simultaneously conducted using piecewise mixed effects modeling in HLM 6.08 software47. To guard against misspecifications in the random components of the model, Huber-corrected standard errors were used when testing the fixed components of the model.48
Piecewise models were used to test the treatment effect from baseline through 6 months post intervention, and the maintenance effect from six months to nine months post intervention. The first segment of the model tested for the treatment effect and placed a linear constraint on the pre-treatment, three month and six month post treatment assessments. The model tested if the slope of the trajectory defined by these three time-points differed between treatment conditions. The second segment of the model tested the maintenance effect by testing treatment differences in the change from six months to nine months post intervention. Both segments of the model were simultaneously estimated using HLM 6.08.
Results
Table 2 lists the baseline demographics for both the treatment and the control conditions. There was a significant difference for gender, with more females in the STAR intervention group than in the control group and the STAR group reported greater emotional abuse (11.32 vs. 9.58, t (167) = 2.09, p < .05). There were no significant differences on age, race, ethnicity, sexual risk score, global emotional distress, or other trauma history.
Table 2.
Baseline Demographic and Behavior Data of Adolescents in Alternative and Therapeutic Schools
| Total Sample N = 185 | Intervention n = 97 | Control n = 88 | |||
|---|---|---|---|---|---|
| Count (%) | Count (%) | Count (%) | Test Statistic | P | |
| Gender (Female) | 112 (61%) | 68 (70%) | 44 (50%) | χ2 (1) = 7.81 | .005 |
| Ethnicity | |||||
| Hispanic | 50 (27%) | 31 (32%) | 19 (22%) | χ2 (1) = 2.51 | .11 |
| Race | χ2 (5) = 5.19 | .39 | |||
| White | 93 (57%) | 42 (51%) | 51 (63%) | ||
| African American or Haitian | 31 (19%) | 17 (21%) | 14 (17%) | ||
| Native Hawaiian/Pacific Islander | 5 (3%) | 4 (5%) | 1 (1%) | ||
| American Indian/Alaska Native | 5 (3%) | 3 (4%) | 2 (3%) | ||
| Asian | 2 (1%) | 2 (2%) | 0 (0%) | ||
| Multiple Endorsements | 27 (17%) | 14 (17%) | 13 (16%) | ||
| Age | |||||
| Mean (SD) | 15.28 (1.26) | 15.30 (1.25) | 15.38 (1.40) | t (165.5)=.95 | .34 |
| Sex Behaviors | |||||
| Ever Sexually Active | 100 (55%) | 53 (55%) | 47 (54%) | χ2 (1) = .03 | .87 |
| Sexual Risk Index | |||||
| Mean (SD) | 1.19 (1.37) | 1.32 (1.46) | 1.05 (1.25) | t(178.6) = -1.36 | .18 |
| Global Distress (GSI) | |||||
| Mean (SD) | 33.43(14.61) | 33.07 (13.46) | 33.8 (15.81) | t (177) = .34 | .73 |
| Childhood Trauma Total (CTQ) | |||||
| Mean (SD) | 53.58(19.07) | 55.22(19.88) | 51.82(18.13) | t (162) = 1.14 | .26 |
Each piecewise model intercept provides additional information regarding baseline differences accounting for cohort. No intercept differences were found for sex risk, HIV knowledge, condom use self-efficacy, or negative condom use expectations. However, there was a significant baseline difference between treatment conditions for levels of condom use advantages (t (27) = 2.21, p < .05), with STAR intervention participants reporting more advantages to condom use than control participants.
Response to intervention
Piecewise models were fit to each outcome in order to simultaneously test the intervention and maintenance effects of the treatment on that outcome. Unadjusted means for Sex Risk Index at each assessment are presented in Table 3, as well as tests of group differences in change of the outcomes observed in the mixed models. Relative to control participants, participants in the STAR intervention showed a significant decrease in the Sex Risk Index across the three and six month follow-up assessments (t (27) = -2.60, p < .05). They also showed greater increases in HIV-related Knowledge scores (t (27) = 2.81, p < .05), and greater increases in Condom Use Self-efficacy scores (t (27) = 2.28, p < .05). There were no significant differences between treatment conditions for scores on Negative Condom Use Expectations or Advantages of Condom Use.
Table 3.
Project STAR (Safe Thinking and Affect Regulation) Intervention Effects among 185 Adolescents in Therapeutic and Alternative Schools
| Unadjusted Means | Test of Intervention Effects | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Three Months Post Intervention | Six Months Post Intervention | |||||
| Control | STAR | Control | STAR | Control | STAR | test statistics from HLMa | |
| Sexual Risk Index | 1.04 | 1.32 | 1.21 | 1.11 | 1.25 | 1.09 | t = -2.60; p = 0.02 |
| HIV Knowledge | 13.20 | 13.32 | 13.75 | 15.39 | 14.02 | 15.70 | t = 2.81; p = 0.01 |
| Condom Use Self-Efficacy | 44.40 | 43.46 | 41.46 | 46.20 | 43.80 | 45.49 | t = 2.28; p = 0.03 |
| Advantages of Condom Use | 48.72 | 51.27 | 49.17 | 51.27 | 52.01 | 54.06 | t = -0.17; p = 0.87 |
| Negative Condom Use Expectations | 13.74 | 13.08 | 14.17 | 13.37 | 12.99 | 11.93 | t = 0.15; p = 0.89 |
Note: There were no statistically significant difference between groups at the baseline assessment; HIV = Human Immunodeficiency Virus.
test statistics were derived from piecewise Hierarchical Linear Models (HLM).
Maintenance of intervention effects after 9 months
The second segments of the piecewise models were the maintenance of effects from six to nine months post intervention. Table 4 presents unadjusted mean scores for both groups and each outcome at the nine month assessment, as well as tests of group differences in maintenance observed in the mixed models. Although the direction of most effects was consistent with waning influence of intervention at nine months post intervention (see Table 4) none of these trends reached statistical significance.
Table 4.
Maintenance of Project STAR (Safe Thinking and Affect Regulation) Intervention Effects among 185 Adolescents in Therapeutic and Alternative Schools
| Unadjusted Means Nine Month Post Intervention | Test of Intervention Effects | ||
|---|---|---|---|
| Control | STAR | test statistics from HLMa | |
| Sexual Risk Index | 1.37 | 1.38 | t = 0.22; p = 0.83 |
| HIV Knowledge | 15.00 | 15.74 | t = -1.71; p = 0.20 |
| Condom Use Self-Efficacy | 44.94 | 45.79 | t = -1.84; p = 0.08 |
| Advantages of Condom Use | 50.94 | 54.34 | t = 0.25; p = 0.82 |
| Negative Condom Use Expectations | 13.55 | 11.92 | t = -1.52; p = 0.14 |
Note: HIV = Human Immunodeficiency Virus.
test statistics were derived from piecewise Hierarchical Linear Models (HLM).
Discussion
This project found that an intervention for youth in therapeutic and alternative schools that was based on empirically supported HIV prevention techniques, and also included sexuality-specific affect management and cognitive monitoring components, was associated with less sexual risk over a six month follow-up period and improvements in HIV knowledge and self efficacy for condom use after the intervention than a brief, knowledge-based comparison condition. This study is the first HIV prevention intervention to document a decrease in sexual risk by self-report over six months for adolescents in alternative schools. These findings are significant since youth in alternative schools have greater rates of risk behavior than their community peers and their ability to respond to standard HIV prevention programs may be compromised due to the frequent occurrence of emotional, behavioral and learning disorders. Importantly, the present study had good retention of a population that is often transient. Furthermore, numerous methodological strengths enhance the study's validity such as a highly scripted intervention, intensive facilitator training, monitoring of the intervention's delivery, and confidential adolescent self-report via laptop computers. Despite the potential for sexual risk to increase over time, the intervention was associated with a decrease in risk for up to six months after the intervention.
Consistent with the design of the STAR intervention, improvement in HIV knowledge and in self efficacy for condom use was associated with the intervention. After the STAR intervention, adolescents knew more about HIV and felt more confident in their ability to use condoms. Although the perceived more advantages and negative outcomes to their use (e.g., “condoms ruin the mood”) did not diminish. These findings might suggest that if confidence is improved, then condoms are more likely to be used, even if the negative perceptions of their use are not eliminated. Additionally, it is possible that the unique elements of the intervention, such as the focus on sexuality-specific affect management and cognitive monitoring, were crucial in providing the intervention's impact. Many of the items assessing condom use self efficacy appear related to affect management (e.g. “I could use a condom if I was upset”). Unfortunately, no specific and valid assessment occurred of the use of affect management and cognitive monitoring, so mediational analyses are not possible. Dismantling studies in the future will be able to address this issue.
There was not a statistically significant difference between groups in the change in sex risk, HIV knowledge or attitudes between six and nine months after the intervention but both groups appeared to experience an increase in risk and comparable decreases in knowledge and attitudes. Perhaps due to continued influence of substantial psychosocial and contextual risk factors, the intervention's impact did not increase over the final three months of the study follow up. These data suggest the need for booster sessions to reinforce skills and perhaps interventions that target other factors, such as family and peer networks, in order to maintain safe health behaviors.
Despite its strengths, limitations to the study should be noted. In order to reduce the potential for contamination between conditions, randomization was not done by subjects but rather by the order of the delivery of the conditions in schools. Since all schools received both interventions, site differences and potential for contamination between conditions were minimized. Randomization by individual could provide more equivalent groups and a stronger test of intervention efficacy. Maintaining the internal validity of research, while balancing the logistical concerns of small organizations, is a challenge of such research. Additionally, the only measure of sexual behavior was by self-report. Although assessments were completed confidentially on laptop computers (a methodology that improves the report of sensitive behaviors), larger samples are needed for collection of biological markers of sexually transmitted infections to verify the efficacy of this intervention. Also, the comparison condition provided sexual health information in an appealing format but was of briefer duration than the STAR intervention. It is possible that the length of the STAR intervention accounted for its impact, however several attention-matched health promotion conditions have not been associated with improvement in sexual behavior5-7. Lastly, enrollment occurred in alternative schools in one geographic location and, although there was racial and ethnic diversity in the sample, the results may not generalize to other locations. The youth were in facilities designed to improve their emotional and behavioral health and the influence of such treatment on study outcomes was not examined in this study, although each school participated in both conditions, reducing the potential confound of school specific treatment programs on outcome.
This project tested a group intervention for adolescents in alternative schools but may have broader clinical implications. This study found that an intervention that was based on standard approaches to improve knowledge, attitudes and skills about safer sex, in conjunction with skills to apply affect management and cognitive monitoring in sexual situations, was associated with safer sexual behavior up to six months post intervention. These data suggest that common clinical techniques and approaches that target impaired cognitions and emotional dysregulation can be usefully applied to improving sexual behavior among youth with emotional and behavioral difficulties. It is possible that clinicians will be able to use these principles and techniques to target and enhance healthy behaviors for youth with a wide range of emotional, behavioral, and learning difficulties and within a range of settings.
Table 1a.
Topics in Project STAR (Safe Thinking and Affect Regulation)
| Session 1. Problem Solving and Sexuality | Introduction of discussion of sexuality in adolescence, introduction of STAR model, introduction of good communication, and role-play. |
| Session 2. STD/AIDS and Birth Control | Overview of reproductive systems, review of STD, review of common sex myths, and presentation of basic concepts regarding protecting self and partner from STDs and pregnancy. |
| Session 3. HIV-Risk Evaluation | Provision of information related to HIVirus and AIDS, categorization of HIV risk-levels across a variety of behaviors, and personalization of risk. |
| Session 4. Personal Vulnerability | Review of HIV/AIDS, game and video aimed at illustrating personal risks in unsafe sex, and video promoting empathy and outlining challenges for individuals with HIV. |
| Session 5. Assertiveness I | Overview of assertive communication, particularly as related to negotiation of sex behaviors. |
| Session 6. Healthy Thinking | Dysfunctional thinking concepts pertaining to sex behaviors. |
| Session 7. Affect Management | Practice recognizing and labeling feelings, discussion of negative outcomes of poor affect management, and education and practice related to distress tolerance skills. |
| Session 8. People with AIDS | Review of a video regarding life before and with HIV/AIDS. |
| Session 9. Assertiveness II | Training in assertiveness skills and role-plays in assertive communication with video taping. |
| Session 10. Assertiveness III | Applying assertive communication to discussion of sex-related behaviors, highlighting applications of earlier skills (i.e., affect regulation, dysfunctional thinking). |
| Session 11. Condom Use | Discussion of feelings about condom use, condom use skills training and practice. |
| Session 12. Condom Negotiation Skills and Substance Use | Assertiveness skills in sexual and drug contexts, discussion of factors that may make it difficult to implement assertiveness skills (i.e., strong feelings, unsafe thoughts, and substance use). |
| Session 13. HIV Testing | Provision of information regarding HIV testing, challenge of myths about HIV testing. |
| Session 14. Review Session | Review of information and skills learned during initial sessions. |
Table 1b.
Topics in Human Immunodeficiency Virus (HIV) Knowledge Comparison Condition
| Session 1. STD/AIDS and Birth Control | Overview of reproductive systems, review of STDs, review of common sex myths, and presentation of basic concepts regarding protecting self and partner from STDs and pregnancy. |
| Session 2. HIV-Risk Evaluation | Provision of information related to HIV and AIDS, categorization of HIV risk-levels across a variety of behaviors, and personalization of risk. |
Note: AIDS = Acquired Immune Deficiency Syndrome; STDs = Sexually Transmitted Diseases;
Acknowledgments
Research supported by National Institute of Mental Health grants R01 61149 and R01 66641 (LKB) and the Lifespan/Tufts/Brown Centers For Acquired Immune Deficiency Syndrome (AIDS) Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Brown, Nugent, Houck, Lescano, Whitely, Barker, and Zlotnick, and Ms. Viau report no biomedical financial interests or potential conflicts of interest.
Clinical trial registration information -- HIV, Abuse, and Psychiatric Disorders Among Youth; NCT00603369; clinicaltrials.gov.
Reference List
- 1.CDC HIV Incidence. Statistics and Surveillance – United States, 2008. [April 25, 2011]; http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/pdf/incidence.pdfAugust,2008.
- 2.Hall H, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: Incidence and prevalence estimates 2000. Perspectives on Sexual and Reproductive Health. 2004;36:6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 4.Grunbaum J, Lowry R, Kann L. Prevalence of health-related behaviors among alternative high school students as compared with students attending regular high schools. Journal of Adolescent Health. 2001;29:337–343. doi: 10.1016/s1054-139x(01)00304-4. [DOI] [PubMed] [Google Scholar]
- 5.Jemmott JB, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among black male adolescents. Effects of an AIDS prevention intervention. American Journal of Public Health. 1992;82:372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanton B, Li X, Ricardo J, Galbrath J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youth. Archives of Pediatrics and Adolescent Medicine. 1996;150:363–372. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- 7.DiClemente RJ, Wingood GM, Harrington K, et al. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of the American Medical Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- 8.Rotherm-Borus MJ, Song J, Gwadz M, et al. Reductions in HIV risk among runaway youths. Prevention Science. 2003;4:173–87. doi: 10.1023/a:1024697706033. [DOI] [PubMed] [Google Scholar]
- 9.Alford S, et al. Advocates for Youth. Washington, DC: Science and success: Sex education and other programs that work to prevent teen pregnancy, HIV & sexually transmitted infections. p. 2008. 2003. [Google Scholar]
- 10.Kohler, et al. Abstinence-only and comprehensive sex education and the initiation of sexual activity and teen pregnancy. Journal of Adolescent Health. 42(4):344–351. doi: 10.1016/j.jadohealth.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 11.Kirby D. School-based interventions to prevent unprotected sex and HIV among adolescents. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. Plenum; New York: 2000. pp. 83–101. [Google Scholar]
- 12.Brown L, Reynolds L, Lourie K. A pilot HIV prevention program for adolescents in a psychiatric hospital. Psychiatric Services. 1997;48:531–533. doi: 10.1176/ps.48.4.531. [DOI] [PubMed] [Google Scholar]
- 13.Hubbard B, Giese M, Raney J. A replication study of reducing the risk, a theory-based sexuality curriculum for adolescents. Journal of School Health. 1998;68:243–47. doi: 10.1111/j.1746-1561.1998.tb06347.x. [DOI] [PubMed] [Google Scholar]
- 14.Slonim-Nevo V, Auslander WF, Ozawa MN. Education options and AIDS-related behaviors among troubled adolescents. J Pediatr Psychol. 1995;20:41–60. doi: 10.1093/jpepsy/20.1.41. [DOI] [PubMed] [Google Scholar]
- 15.Gottlieb A, Aruffo J, Webb R, Hardin B. Impact of peer-led AIDS eduction with adolescent medical and psychiatric inpatients. Clinical Research. 1991;39:820A. [Google Scholar]
- 16.Pedlow CT, Carey MP. HIV sexual risk-reduction interventions for youth: A review and methodological critique of randomized controlled trials. Behav Modif. 2003 April;27:135–190. doi: 10.1177/0145445503251562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buzi R, Tortolero S, Roberts R, Ross M, Addy R, Markham C. The impact of a history of sexual abuse on high-risk sexual behaviors among females attending alternative schools. Adolescence. 2003;38:595–605. [PubMed] [Google Scholar]
- 18.Houck C, Nugent N, Lescano C, Peters A, Brown L. Impact of sexual abuse on sexual behaviors, sexual attitudes, and psychological adjustment in alternative schools. J Pediatr Psychol. 2010;35:473–83. doi: 10.1093/jpepsy/jsp111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Houck C, Lescano C, Brown L, Tolou-Shams M, Thompson J, Project SHIELD Study Group “Islands of risk”: Identifying subtypes of adolescents at risk for HIV. J Pediatr Psychol. 2006;31:619–629. doi: 10.1093/jpepsy/jsj067. [DOI] [PubMed] [Google Scholar]
- 20.Watson DW, McCuller J, Bisesi L, Tanamly S, Sim T, Kavich J. Preparing adolescents for success in school: A school-based model for adolescents in the alternative high school setting. Journal of HIV/AIDS Prevention in Children and Youth. 2006;6(2):7–31. [Google Scholar]
- 21.Pentz MA. Target populations and interventions in prevention research. 1994. [PubMed]
- 22.Eggert LL, Seyl CD, Nicholas LJ. Effects of a school-based prevention program for potential high school dropouts and drug abusers. International Journal of Addictions. 1990;25(7):773–801. doi: 10.3109/10826089009056218. [DOI] [PubMed] [Google Scholar]
- 23.Lescano CM, Brown LK, Puster K, Miller P. Sexual abuse and adolescent HIV risk: A group intervention framework. Journal of HIV/AIDS Prevention in Children and Youth. 2004;6:43–57. [Google Scholar]
- 24.Linehan MM. Skills training manual for treating borderline personality disorder. Guilford Press; New York, NY US: 1993. [Google Scholar]
- 25.Stanton B. Adolescent Human Immunodeficiency Virus prevention what we have accomplished and what still needs to be done. Arch Pediatrics and Adolescence. 2009;163(12):1162–1163. doi: 10.1001/archpediatrics.2009.226. [DOI] [PubMed] [Google Scholar]
- 26.Ingram BL, Flannery D, Elkavich A, Rotheram-Borus MJ. Common processes in evidence-based adolescent HIV prevention programs. AIDS and Behavior. 2008;12(3):374–383. doi: 10.1007/s10461-008-9369-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Education and Prevention. 2006;18(Suppl A):59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 28.Lyles CM, Kay LS, Crepaz N, Herbst JM, Passin WF, Kim AS, et al. Best-evidence Interventions: Findings from a systematic review of HIV behavioral interventions for U.S. populations at high risk 2000-2004. American Journal of Public Health. 2007;97(1):133–143. doi: 10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eke AN, Mezoff JS, Duncan T, Sogolow ED. Reputationally strong HIV prevention programs: Lessons from the front line. AIDS Education and Prevention. 2006;18(2):163–175. doi: 10.1521/aeap.2006.18.2.163. [DOI] [PubMed] [Google Scholar]
- 30.Sales et al. A decade in review: Building on the experiences of past adolescent STI/HIV interventions to optimize future prevention efforts. Sexually Transmitted Infections. 2006;82:431–436. doi: 10.1136/sti.2005.018002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cambell MK, Elbourne DR, Altman DG. Consort Statement: Extension to cluster rondomised trials. BMJ. 2004;328(7441):702–708. doi: 10.1136/bmj.328.7441.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lescano C, Brown L, Miller P, Puster K. Unsafe sex: Do feelings matter? Journal of Prevention & Intervention in the Community. 2007;33:51–62. doi: 10.1300/J005v33n01_05. [DOI] [PubMed] [Google Scholar]
- 33.Bellg A, Resnick B, Minicucci D, Ogedegbe G, Ernst D, Borrelli B, et al. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH behavior change consortium. Health Psychology. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 34.Boekeloo BO, Howard DE. Oral sex experience among young adolescents receiving general examinations. American Journal of Health Behavior. 2002 Jul-Aug;26(4):306–314. doi: 10.5993/ajhb.26.4.7. [DOI] [PubMed] [Google Scholar]
- 35.Schroder K, Carey M, Vanable P. Methodological challenges in research on sexual risk behavior: I. item content, scaling, and data analytical options. Annals of Behavioral Medicine. 2003;26(2):76–103. doi: 10.1207/s15324796abm2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown L, Fritz G. Children's knowledge and attitudes about AIDS. Journal of American Academy of Child and Adolescent Psychiatry. 1988;27:504–508. doi: 10.1097/00004583-198807000-00022. [DOI] [PubMed] [Google Scholar]
- 37.Prochaska JO, Redding CA, Harlow LL, Rossi JS, Velicer WF. The transtheoretical model of change and HIV prevention: A review. Health Education Quarterly. 1994;21:471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- 38.NIMH Multisite HIV Prevention Trial Group The NIMH multisite HIV prevention trial: Reducing HIV sexual risk behavior. Science. 1998;280:1889–1894. doi: 10.1126/science.280.5371.1889. [DOI] [PubMed] [Google Scholar]
- 39.Brown L, Lourie K, Zlotnick C, Cohn J. The impact of sexual abuse on the IV-risk related behavior of adolescents in intensive psychiatric treatment. American Journal of Psychiatry. 2000;157:1413–1415. doi: 10.1176/appi.ajp.157.9.1413. [DOI] [PubMed] [Google Scholar]
- 40.Derogatis LR, Savitz KL. Handbook of Psychological Assessment in Primary Care Settings. Lawrence Erlbaum Associates; Mawah: 2000. The SCL-90-R and brief symptom inventory (BSI) in primary care. pp. 297–334. [Google Scholar]
- 41.Ickovics JR, Meade CS, Kershaw TS, Milan S, Lewis JB, Ethier KA. Urban teens: Trauma, posttraumatic growth, and emotional distress among female adolescents. Journal of Consulting and Clinical Psychology. 2006 Oct;74(5):841–850. doi: 10.1037/0022-006X.74.5.841. Special issue: Benefit-Finding. [DOI] [PubMed] [Google Scholar]
- 42.Handal PJ, DeWitt G, Gilner FH, Searight HR. Preliminary validity for the Langner Symptoms Survey and Brief. Symptom Inventory as mass-screening instruments for adolescent adjustment. Journal of Clinical Child Psychology. 1993;22:382–386. [Google Scholar]
- 43.Bernstein DFL. Manual for the childhood trauma questionnaire: A retrospective self-report. The psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- 44.Bernstein D, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Scher C, Stein MAG, McCreary D, Forde D. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14:843–57. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- 46.Molenberghs G, Thijs H, Jansen I, Beunekens C, Kenward MG, Mallinckrodt C, Carroll RJ. Analyzing incomplete longitudinal clinical trial data. Biostatistics. 2004;5:445–464. doi: 10.1093/biostatistics/5.3.445. [DOI] [PubMed] [Google Scholar]
- 47.Raudenbush SW, Bryk AS, Congdon R. HLM6 for Windows 2004 (Computer software) Scientific Software International, Inc.; Lincolnwood, IL: [Google Scholar]
- 48.Liang L, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]