SYNOPSIS
Objective
We examined gender differences in the incidence of acute myocardial infarction (AMI) after the passage of a smoke-free law in Lexington, Kentucky. The initial legislation had exemptions not covering manufacturing facilities and government buildings, which may have put men at greater risk for AMI.
Methods
We examined the effect of Lexington's smoke-free public places law on hospitalizations for AMI (i.e., heart attack) among men and women 40 months prior to and 32 months after enactment of the law. We used the statewide administrative database (Comp Data) for all hospital billing records for the four health-care systems in Lexington-Fayette County. Cases were included in the analysis if (1) the patient was $35 years of age; (2) the patient had a primary discharge diagnosis of AMI, with an International Classification of Diseases, Ninth Revision code in the range of 410.00 to 410.99; and (3) the date of service was between January 1, 2001, and December 31, 2006.
Results
Among women, AMI hospitalizations declined 23% after the law took effect. The rate of AMI events among men did not change significantly. There was an overrepresentation of women in the hospitality industry and a disproportionate number of men working in manufacturing facilities and government worksites not mandated by the law.
Conclusions
We found gender differences in the reduction of AMI hospitalizations following implementation of a smoke-free law that covered only some sectors of the workforce. Enacting smoke-free laws that cover all places of employment and strengthening existing partial laws may extend protection against AMIs to female and male workers.
Despite the U.S. trend to enact state and local smoke-free legislation, exposure to secondhand smoke (SHS) continues to present a significant public health and occupational hazard. As of April 1, 2011, only 48% of Americans were protected by 100% smoke-free legislation covering all workplaces, restaurants, and bars.1 Lexington-Fayette (Kentucky) Urban County Government implemented a smoke-free enclosed public places law on April 27, 2004, prohibiting smoking in most enclosed public places, including, but not limited to, restaurants, bars, bowling alleys, bingo halls, convenience stores, laundry facilities, and other businesses open to the public.2 Workers in buildings not open to the public—including facilities operated by private organizations, rooms used for private social functions and those in retail tobacco stores, government office buildings or workplaces (pursuant to Kentucky Revised Statute 61.165), and tobacco warehouses—remained exposed to SHS. The ordinance did not cover manufacturing facilities or government worksites, which have a preponderance of male workers,3,4 thus putting men at greater risk for poor health outcomes related to SHS exposure. Kentucky has a rich tobacco-growing tradition and weak tobacco-control policies,5,6 and its adult smoking rates for men and women are among the highest in the nation.7 Tobacco-producing states such as Kentucky fall behind other states in enacting progressive tobacco-control policies,6 in part due to a long tradition of pro-tobacco influence.8
Exposure to SHS has immediate, substantial, and sustained adverse effects on the cardiovascular system and is a cause of coronary heart disease among adults,9–15 resulting in an estimated 46,000 coronary heart disease deaths annually among nonsmokers.13 Nonsmokers exposed to SHS have a 25%–30% higher risk of coronary heart disease compared with those who are not exposed to SHS. Exposure to SHS alters both platelet and endothelial function, increasing the risk for acute myocardial infarction (AMI).9 Even brief exposure to SHS affects both the number and function of endothelial progenitor cells and leads to sustained vascular injury.16
An estimated 1.2 million Americans are diagnosed with a new or recurrent AMI every year. Gender disparities in the incidence and mortality from AMI and in the influence of modifiable risk factors and medical therapies exist. Men are more likely than women to be diagnosed and hospitalized for AMI.17 Further, in a study by Berger et al., 30-day crude mortality rates were higher among women than men; however, gender differences disappeared after controlling for relevant clinical factors.18 Gender disparities have also been found in response to medical therapies designed to reduce the risk of AMI (e.g., women may be less responsive to aspirin therapy than men).19 Modifiable risk factors such as cigarette smoking, SHS exposure, high blood lipid levels, and obesity account for more than 90% of the risk for an initial AMI.20 Young male current smokers have the highest population-attributable risk for AMI, and they are at particular risk as a result of exposure to SHS.21 However, middle-aged women who smoke cigarettes are more likely to have AMIs than their male counterparts.22 Women may be more sensitive than men to the harmful effects of smoking and more likely to develop ischemic heart disease due to exposure to tobacco smoke.23
While there is a preponderance of scientific evidence supporting the protective effect of smoke-free legislation on the heart,24–27 there is emerging literature to suggest that gender may be an important consideration in studying the outcomes of this legislation. A study of New York City's comprehensive tobacco-control efforts reported a differential effect on smoking prevalence by gender.28 Young adult women were more likely to quit smoking compared with young adult men following smoke-free legislation and smoking cessation assistance. One study in Rome found that a smoke-free public places law was associated with reductions in acute coronary events among middle-aged men but not women.29 Indeed, studies suggest that smoke-free legislation may have greater effects on AMIs experienced by men, regardless of smoking status.30 Low-income women may remain exposed to SHS at work in smoke-free communities.31 Greaves and Hemsing called for a framework that is sensitive to gender when developing and evaluating smoke-free policies.32
We examined the effects of a non-comprehensive smoke-free law in Lexington, Kentucky, on hospitalizations for AMI among men and women. Given that a substantial number of men, who comprise the majority of the manufacturing and government workforce, were not protected by the smoke-free law, we hypothesized that females would be more likely than males to experience a decline in AMIs after the law took effect (hereafter, “post-law”).
METHODS
We measured AMI events 40 months prior to and 32 months after the enforcement of Lexington-Fayette County's smoke-free law on April 27, 2004. The statewide administrative database (Comp Data) was the data source for all Lexington-Fayette County hospital billing records for the four health-care systems serving the area. Records included hospital discharge diagnosis by International Classification of Diseases, Ninth -Revision (ICD-9) billing code, dates of service, gender, age, and county of residence. Tobacco use information was not available. While some residents of Fayette work outside the county, most who live in the county also work there.33 We excluded from the analysis patients treated in Fayette County who lived outside the area.
Cases were included in the analysis if (1) the patient was $35 years of age; (2) the patient had a primary discharge diagnosis of AMI, with an ICD-9 code in the range of 410.00 to 410.99; and (3) the date of service was between January 1, 2001, and December 31, 2006. We omitted patients younger than 35 years of age because approximately 10% of the cases were younger than this cutoff, which would have led to very small cell sizes after further considering the 10 relevant age-by-gender categories; omitting patients younger than this cutoff is consistent with a prior study by Juster et al.34 We chose discharge diagnosis as the criterion for inclusion, as it is a more accurate reflection of the true condition than the diagnosis at admission (e.g., chest pain due to gall bladder disease vs. heart attack).35
Data analysis
We summarized the pre- and post-law demographic characteristics of patient populations using descriptive statistics; we compared pre- and post-law events using a two-sample t-test or the Chi-square test of association. We combined the yearly number of cases for residents of Lexington-Fayette County with the corresponding population estimate to obtain crude annual rates.36 We then age-adjusted these crude rates, with standardization to the 2000 U.S. Census population estimates for each corresponding age cohort. We determined annual age-adjusted rates for the entire group of patients, as well as for women and men separately. While we recognize the gender gap in smoking prevalence, especially among Latinos in the U.S.,37 we were unable to control for race/ethnicity in this study due to relatively few minority cases in the state (and county), whose population is predominantly non-Hispanic white.
We modeled the monthly rates for AMI hospitalizations during the six-year period using Poisson regression; we specified the negative binomial distribution to allow for over- or under-dispersion. We based the model on crude (unadjusted) rates, given that age was included as a covariate in the model. The initial regression model included the effects of law status (pre-law vs. post-law), gender, age (with seven categories corresponding to Census data cohorts $35 years of age), and the two- and three-way interactions of these effects. We used the log of the estimated population size as an offset variable in the model, with population estimates specific to the year, gender, and age category of the cases. The regression model also contained annual Fayette County weighted estimates for adult smoking rates, obtained from the Behavioral Risk Factor Surveillance System; an indicator for time (month of event, ranging from one to 72) to assess secular trends unrelated to law implementation; a law status by time interaction term to estimate whether AMI hospitalization rates continued to change over time; and first- and second-order harmonics to account for seasonal variation. We sequentially removed the interaction terms not significant in the initial model for ease of interpretation, with little change in model fit. We determined goodness of fit of the models using Pearson's Chi-square statistic and corresponding degrees of freedom.
In addition to Poisson regression, we considered a first-order autoregressive time-series model. Consistent with a study comparing these two strategies when quantifying time trends for relatively rare outcomes38 (e.g., hospitalizations for AMI), there were no appreciable differences for the present study in the level of significance between these two methods for any of the predictors. We reported the Poisson regression results in this article, as this method estimates the relative risk (RR) of an event post-law compared with pre-law, adjusting for county-level smoking rate and demographic, time-trend series, and seasonal main effects and significant interactions in the model.
Due to the significant interaction between law status and gender in the Poisson model, we plotted the actual monthly gender-specific rates per 100,000 population, weighted by age distribution, on a graph of the predicted rates based on the Poisson regression model, with separate curves for men and women. We conducted data analyses and graphing using SAS® version 9.1,39 with α=0.05.
RESULTS
During the six-year study period, there were a total of 2,692 AMI hospitalizations among Lexington-Fayette County residents, including 1,564 before the smoke-free law (i.e., through April 2004) and 1,128 post-law. The average age for pre-law AMI cases (67.3 years) was older than the average age for the post-law period (65.5 years) (t=3.2, p=0.001). The percentage of female AMI cases was lower in the post-law period (38%) than in the pre-law period (47%) (χ2=24.0, p,0.0001).
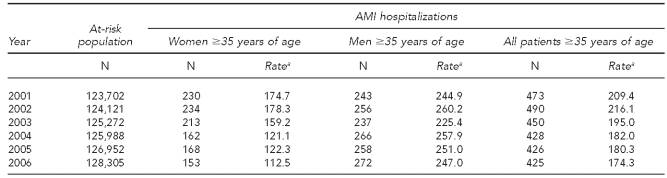
As shown in Table 1, the age-adjusted rates for men did not exhibit a directional trend over time, but there was a decrease in these rates for females from 2003 to 2004 (the year when the smoke-free law was implemented), which was maintained during the subsequent two years. As there was no systematic change in age-adjusted rates for men, the decline over time was less pronounced in the combined group of men and women.
Table 1.
Size of the population aged >35 years at risk for AMI hospitalization, with number of cases and age-adjusted rates, by gender and overall: Lexington-Fayette County, Kentucky, 2001–2006
aAge-adjusted rate per 100,000 at-risk population, adjusted to the 2000 U.S. Census
AMI = acute myocardial infarction
The final Poisson regression model fit the data well; the ratio of Pearson's Chi-square statistic to the degrees of freedom was 0.98, close to the null value of 1.0. In addition to the main effects of law, gender, and age, as well as the time-trend series and harmonic terms, the final model contained the two-way interactions of gender with law and age. Other interaction terms, including the interaction between law status and time, were not significant and were removed from the final model. We used the main effect of law and the gender-by-law interaction effect to determine the post- and pre-law RRs for women and men within the Poisson model, adjusting for county-level adult smoking rate, demographics, time trends, and seasonality.
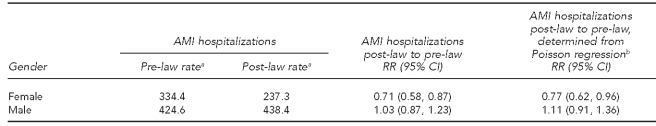
As displayed in Table 2, the rate of AMI hospitalizations declined by 97.1 per 100,000 person-years from pre- to post-law for women, but men demonstrated an increase of 13.8 per 100,000 person-years for this pre- to post-law comparison. Considering only the number of cases for each gender pre- and post-law, along with the corresponding size of the at-risk population for each gender and time frame, the RR of an AMI hospitalization was 0.71 for women and 1.03 for men; the decline in AMI hospitalizations was significant for women (p,0.05) but not for men.
Table 2.
Rate of AMI hospitalizations among people >35 years of age before and after implementation of a public places smoke-free law in 2004, by gender: Lexington-Fayette County, Kentucky, 2001–2006
aPer 100,000 person-years
bAdjusted for county-level adult smoking rate, demographics, time, and seasonality. The two significant interaction terms retained in the regression were law status by gender and gender by age.
AMI = acute myocardial infarction
RR = relative risk
CI = confidence interval
The results of the Poisson regression adjusting for county-level smoking rate, demographic factors, time trends, and seasonality were similar to the unadjusted RRs. For women, the RR of post- to pre-law AMI hospitalizations was 0.77 (p=0.02), while the RR for men was 1.11 (p=0.3); these adjusted comparisons also demonstrated a significant decline for women and a nonsignificant change for men (Table 2). Among women, AMI hospitalizations declined 23% post-law, while the rate of these AMI events among men did not change significantly between the two time periods.
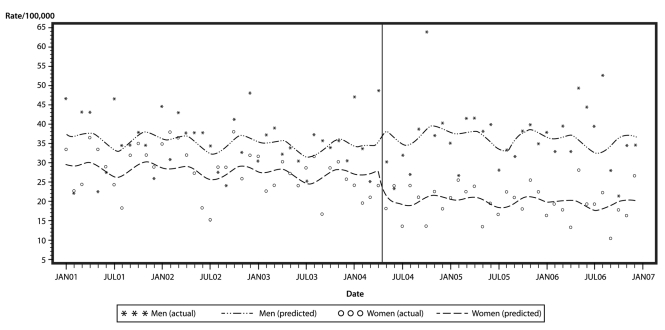
The Figure shows the actual rates of AMI hospitalizations per month for women and men relative to the size of the population at risk, weighted by age -distribution. The Poisson regression pre- and post-law curves predicted from the model described previously are also shown with separate curves by gender. Consistent with the age-adjusted rates presented in Table 1 and the significant decline among women in RR post-law (Table 2), the Figure illustrates that while the pre- and post-law curves for men were relatively stable over time, there was a notable post-law decline for women that was maintained during the 32-month post-law period.
Figure.
Actual and predicted monthly rates of AMI hospitalizations per 100,000 population before and after implementation of a smoke-free public places law in 2004: Lexington-Fayette County, Kentucky, 2001–2006a
aThe vertical line represents the date the smoke-free law went into effect (April 2004). The Poisson regression model used to determine the predicted rates demonstrated a 23% decrease in AMI hospitalizations for women after the law went into effect, while the change in rates for men was not significant.
AMI = acute myocardial infarction
DISCUSSION
Following implementation of a smoke-free enclosed public places law in Lexington-Fayette County, there was a 23% decline in AMIs among women, adjusting for time trends, county-level smoking rate, seasonality, and the demographics of the at-risk population. The post-law rates for women were relatively stable during the 32-month post-law period, indicating that the protective effect of the smoke-free law was maintained for women. This 23% decline in AMIs was slightly higher than the estimate from one meta-analysis that reported a decline of 15% for each year after implementation.26,40
The fact that we did not see a beneficial effect of the law on AMIs among men may have been because the smoke-free legislation did not cover all workplaces at the time. Our findings are inconsistent with two studies of smoke-free legislation and AMI in Italy. One study in Piedmont found a significant decline in admissions for AMIs among both men and women younger than 60 years of age following implementation of a smoke-free law that covered all indoor public places but not all workplaces.41 Another study in Rome showed a significant reduction in acute coronary events (including, but not limited to, AMI) among Roman men but not women following implementation of the smoke-free public places law.29 Our dissimilar findings may have been due to Kentucky's pro-tobacco heritage, coupled with higher-than-average adult smoking7 and cardiovascular disease42 rates.
Both AMI prevalence and rate of hospitalizations for cardiovascular disease showed a steady upward trend from 2001 to 2006 in Kentucky. The prevalence of AMIs increased from 5.0% to 6.6% from 2003 to 2006 (prevalence data not available for 2001–2002).43 Among men, AMI prevalence during this time period changed from 6.6% to 8.3%, representing a 26% increase; among women, there was a 39% increase in AMI hospitalizations, from 3.6% to 5.0%. The rate of cardiovascular hospitalizations among Kentuckians also increased from 210.3 per 10,000 population to 232.9 per 10,000 population during the six-year period;42 gender-specific rates were not available. While AMI prevalence and cardiovascular disease were trending upward in the state during the study period, AMI events for women in Lexington, the second-largest metropolitan area of Kentucky, showed a decline during this time period that coincided with implementation of the smoke-free law. Further research is needed to determine the differential effects of smoke-free legislation on AMIs among men and women.
This is the first study to report an association between smoke-free laws and AMIs among women but not men. At the time of this study, Lexington's law covered all venues open to the public; however, not all workers were protected. Lexington's ordinance at the time was not a 100% smoke-free workplace law; rather, it covered all buildings open to the public. Manufacturing facilities that were not open to the public were not mandated to be smoke-free. Of the civilian employed population aged 16 years and older in Fayette County, 9.5% work in manufacturing. While men comprise 53.7% of the civilian workforce in Fayette County, 77.5% of manufacturing workers are male.3 Further, government office buildings or workplaces were not covered by the ordinance. Of the civilian employed population aged 16 years and older in Fayette County, 18.1% work for the government (including local, state, and federal). While men comprise 53.7% of the civilian workforce in Fayette County, 48.5% of government workers are male.4 Combining these two work sectors, 27.5% of the civilian workforce $16 years of age work in manufacturing and government. While men comprise 53.7% of the workforce in the county, they comprise 58.5% of workers in these two sectors not protected by the smoke-free ordinance. The gender distribution of workers in other workplaces not covered by the smoke-free policy, including workers in tobacco retail stores, is not known.
A plausible explanation for the lack of effect of the legislation on AMIs among men, and one possible contributing factor to our findings, was that men are overrepresented in the manufacturing and government sectors and that those workers were not covered by Lexington's smoke-free ordinance. Another factor that could have contributed to the decrease in AMI hospitalizations was the decline in adult smoking prevalence in Fayette County after the law went into effect.44 However, the rate of decrease did not differ by gender.
One possible explanation for the protective effect of the smoke-free law among women was that women are overrepresented in the food service/hospitality industry in Fayette County. Although 54.4% of food preparation and serving-related workers in Fayette County are female, women comprise only 46.3% of the civilian workforce.3 It is well-known that workers in the food service industry are disproportionately affected by SHS on the job.45 The protective effect of the smoke-free law for hospitality workers is evident from other studies in Lexington. There was a dramatic improvement in air quality in hospitality venues46 and an immediate reduction in hair nicotine among bar and restaurant workers following implementation of Lexington's smoke-free law.47 While more research is needed, at least two studies suggest that women may be more sensitive to tobacco smoke,22,23 perhaps putting them at higher risk for AMIs when exposed to SHS. The exact mechanism is unclear, but there is speculation that tobacco smoke may have an anti-estrogenic effect, particularly in young, premenopausal women who would otherwise benefit from estrogen's cardio-protective role.22 Smoke-free laws may be more protective for women, given the possibility that they may be more sensitive than men to tobacco smoke.
Limitations
This study had several limitations. One limitation was the absence of a control or comparison group. We cannot infer causation, but we can say that there was an association between smoke-free laws and AMIs based on the pre-post, no-control-group design. We also were unable to examine differences by race/ethnicity, given the small subgroup sizes for racial/ethnic minority group categories in Lexington-Fayette County. Another limitation was the potential for underestimation of AMI cases, given the migration of workers both in and out of Lexington. Lexington-Fayette County is a growing metropolitan area in which some residents commute outside the county to work. Similarly, there are people who live in surrounding counties who commute to Lexington-Fayette County to work. Health outcomes of those who work in the county but live elsewhere were not investigated because their place of work was unavailable. Likewise, Fayette County residents who work elsewhere may have been hospitalized in a non-county hospital during work hours, and they were not included in the analysis. The limited number of personal characteristics for each case was another limitation, as data on tobacco use and SHS exposure were not available. Many in our sample may have been current smokers, but we did not have access to these data.
CONCLUSIONS
There was a 23% decline in AMIs among women after implementation of Lexington's smoke-free public places ordinance in 2004. We found this decline despite the fact that AMI prevalence and hospitalizations for cardiovascular disease were on an upward trend in Kentucky during the study period. We did not find an effect of the law on AMIs among men. The overrepresentation of women in the hospitality industry in Fayette County, combined with the disproportionate number of men working in manufacturing facilities and government worksites not mandated by the smoke-free law, may partially explain why women may have been more protected by this law than men. Another explanation is that women may be more sensitive to tobacco smoke and, thus, more likely to be protected by smoke-free legislation. Further research is needed to examine the differential effects of smoke-free laws by strength of law, gender, and worker subgroup.
To date, most of the published smoke-free law and AMI studies have evaluated the impact of comprehensive 100% smoke-free workplace and public places legislation.34,48–50 While 23 U.S. states and 454 communities have adopted laws requiring all workplaces, restaurants, and bars to be smoke-free, the majority of states and municipalities in the U.S. have been slow to protect all workers from exposure to SHS.51 We found gender differences in the reduction of AMI hospitalizations following implementation of a smoke-free law that covered only some sectors of the workforce. Enacting comprehensive smoke-free laws that cover all places of employment and strengthening existing partial laws may extend protection against AMIs to both male and female workers. However, smoke-free legislation is greatly influenced by the corporate tobacco lobby and anti-government groups, and progress toward protecting all workers from SHS requires adequate resources and commitment to pro-health advocacy.8
Footnotes
This work was supported by the Flight Attendant Medical Research Institute. The University of Kentucky Medical Institutional Review Board approved the study. The authors thank the University of Kentucky HealthCare Office of Business Development and Decision Support for providing the database (Comp Data) for this study.
REFERENCES
- 1.American Nonsmokers' Rights Foundation. Percent of U.S. state populations covered by 100% smokefree air laws. 2011. [cited 2011 Apr 1]. Available from: URL: http://www.no-smoke.org/pdf/percentstatepops.pdf.
- 2.Clean Indoor Air Ordinance. Lexington-Fayette Urban County Government Code, Ch. 14, §§97-104 (July 1, 2003)
- 3.Census Bureau (US) Occupation by sex and median earnings in the past 12 months (in 2006 inflation-adjusted dollars) for the civilian employed population 16 years and over. 2006. [cited 2010 Jul 23]. Available from: URL: http://www.factfinder.census.gov/servlet/STTable?_bm=y&-qr_name=ACS_2006_EST_G00_S2401&-geo_id=01000US&-ds_name=ACS_2006_EST_G00_&-_lang=en&-redoLog=false.
- 4.Census Bureau (US) Class of worker by sex and median earnings in the past 12 months (in 2006 inflation-adjusted dollars) for the civilian employed population 16 years and over. 2006. [cited 2010 Jul 23]. Available from: URL: http://factfinder.census.gov/servlet/STTable?_bm=y&-state=st&-context=st&-qr_name=ACS_2006_EST_G00_S2408&-ds_name=ACS_2006_EST_G00_&-CONTEXT=st&-tree_id=306&-redoLog=false&-geo_id=05000US21067&-format=&-_lang=en.
- 5.Chaloupka FJ, Hahn EJ, Emery SL. Policy levers for the control of tobacco consumption. Kentucky Law J. 2002;90:1009–42. [Google Scholar]
- 6.Polednak AP. Smoke-free laws and cigarette excise taxes in U.S. states with highest vs. lowest adult smoking rates in 2007. Prev Med. 2009;49:558–9. doi: 10.1016/j.ypmed.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 7.State-specific prevalence of cigarette smoking and smokeless tobacco use among adults—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(43):1400–6. [PubMed] [Google Scholar]
- 8.Givel M. Limited state progress in regulating secondhand tobacco smoke. Int J Health Serv. 2007;37:469–76. doi: 10.2190/L187-PWL4-24H1-N448. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services (US) The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta: HHS, Centers for Disease Control and Prevention (US), Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [PubMed] [Google Scholar]
- 10.Whincup PH, Gilg JA, Emberson JR, Jarvis MJ, Feyerabend C, Bryant A, et al. Passive smoking and risk of coronary heart disease and stroke: prospective study with cotinine measurement. BMJ. 2004;329:200–5. doi: 10.1136/bmj.38146.427188.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Annual smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 1997–2001. MMWR Morb Mortal Wkly Rep. 2005;54(25):625–8. [PubMed] [Google Scholar]
- 12.He J, Vupputuri S, Allen K, Prerost MR, Hughes J, Whelton PK. Passive smoking and the risk of coronary heart disease—a meta-analysis of epidemiologic studies. N Engl J Med. 1999;340:920–6. doi: 10.1056/NEJM199903253401204. [DOI] [PubMed] [Google Scholar]
- 13.California Environmental Protection Agency. Proposed identification of environmental tobacco smoke as a toxic air contaminant. Sacramento (CA): California Environmental Protection Agency, Air Resources Board, Office of Environmental Health Hazard Assessment; 2005. [Google Scholar]
- 14.Barnoya J, Glantz SA. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation. 2005;111:2684–98. doi: 10.1161/CIRCULATIONAHA.104.492215. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health and Human Services (US) Rockville (MD): HHS, Public Health Service, Office of the Surgeon General (US); 2010. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the Surgeon General. [PubMed] [Google Scholar]
- 16.Heiss C, Amabile N, Lee AC, Real WM, Schick SF, Lao D, et al. Brief secondhand smoke exposure depresses endothelial progenitor cells activity and endothelial function: sustained vascular injury and blunted nitric oxide production. J Am Coll Cardiol. 2008;51:1760–71. doi: 10.1016/j.jacc.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 17.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 18.Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–82. doi: 10.1001/jama.2009.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yerman T, Gan WQ, Sin DD. The influence of gender on the effects of aspirin in preventing myocardial infarction. BMC Med. 2007;5:29. doi: 10.1186/1741-7015-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 21.Teo KK, Ounpuu S, Hawken S, Pandey MR, Valentin V, Hunt D, et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet. 2006;368:647–58. doi: 10.1016/S0140-6736(06)69249-0. [DOI] [PubMed] [Google Scholar]
- 22.Njølstad I, Arnesen E, Lund-Larsen PG. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction. A 12-year follow-up of the Finmark Study. Circulation. 1996;93:450–6. doi: 10.1161/01.cir.93.3.450. [DOI] [PubMed] [Google Scholar]
- 23.Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ. 1998;316:1043–7. doi: 10.1136/bmj.316.7137.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schroeder SA. Public smoking bans are good for the heart. J Am Coll Cardiol. 2009;54:1256–7. doi: 10.1016/j.jacc.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Institute of Medicine, Committee on Secondhand Smoke Exposure and Acute Coronary Events. Secondhand smoke exposure and cardiovascular effects: making sense of the evidence. Washington: National Academies Press; 2010. [PubMed] [Google Scholar]
- 26.Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. J Am Coll Cardiol. 2009;54:1249–55. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 27.Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation. 2009;120:1373–9. doi: 10.1161/CIRCULATIONAHA.109.870691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ellis JA, Perl SB, Davis K, Vichinsky L. Gender differences in smoking and cessation behaviors among young adults after implementation of local comprehensive tobacco control. Am J Public Health. 2008;98:310–6. doi: 10.2105/AJPH.2006.101758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cesaroni G, Forastiere F, Agabiti N, Valente P, Zuccaro P, Perucci CA. Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117:1183–8. doi: 10.1161/CIRCULATIONAHA.107.729889. [DOI] [PubMed] [Google Scholar]
- 30.Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med. 2008;359:482–91. doi: 10.1056/NEJMsa0706740. [DOI] [PubMed] [Google Scholar]
- 31.Moore RS, Annechino RM, Lee JP. Unintended consequences of smoke-free bar policies for low-SES women in three California counties. Am J Prev Med. 2009;37(2 Suppl):S138–43. doi: 10.1016/j.amepre.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greaves LJ, Hemsing NJ. Sex, gender, and secondhand smoke policies: implications for disadvantaged women. Am J Prev Med. 2009;37(2 Suppl):S131–7. doi: 10.1016/j.amepre.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 33.Census Bureau (US) State and county quick facts: Lexington-Fayette, Kentucky. [cited 2011 Mar 3]. Available from: URL: http://quickfacts.census.gov/qfd/states/21/2146027.html.
- 34.Juster HR, Loomis BR, Hinman TM, Farrelly MC, Highland A, Bauer UE, et al. Declines in hospital admissions for acute myocardial infarction in New York State after implementation of a comprehensive smoking ban. Am J Public Health. 2007;97:2035–9. doi: 10.2105/AJPH.2006.099994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown F, Leon-Chisen N, editors. 2010 revised edition. Chicago: American Hospital Association; 2010. International Classification of Diseases, Ninth Revision 2011 coding handbook, with answers. [Google Scholar]
- 36.Census Bureau (US) County total population, population change and estimated components of population change. 2006. [cited 2010 Jul 23]. Available from: URL: http://www.census.gov/popest/datasets.html.
- 37.Pérez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, et al. Cigarette smoking behavior among U.S. Latino men and women from different countries of origin. Am J Public Health. 2001;91:1424–30. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kuhn L, Davidson LL, Durkin MS. Use of Poisson regression and time series analysis for detecting changes over time in rates of child injury following a prevention program. Am J Epidemiol. 1994;140:943–55. doi: 10.1093/oxfordjournals.aje.a117183. [DOI] [PubMed] [Google Scholar]
- 39.SAS Institute, Inc. SAS®: Version 9.1 for Windows. Cary (NC): SAS Institute, Inc.; 2003. [Google Scholar]
- 40.Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis [published erratum appears in J Am Coll Cardiol 2009;54:1902] J Am Coll Cardiol. 2009;54:1249–55. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 41.Barone-Adesi F, Vizzini L, Merletti F, Richiardi L. Short-term effects of Italian smoking regulation on rates of hospital admission for acute myocardial infarction. Eur Heart J. 2006;27:2468–72. doi: 10.1093/eurheartj/ehl201. [DOI] [PubMed] [Google Scholar]
- 42.Kentucky Cabinet for Health and Family Services. Kentucky cardiovascular disease fact sheet. 2008. [cited 2010 Jul 22]. Available from: URL: http://chfs.ky.gov/NR/rdonlyres/738A1FCB-4F89-4C25-A6E1-548D3E36BE29/0/KyCVDFactSheet_Aug081.pdf.
- 43.Kentucky Cabinet for Health and Family Services, Department for Public Health. Kentucky Behavioral Risk Factor Surveillance System annual reports. [cited 2010 Jul 22]. Available from: URL: http://chfs.ky.gov/dph/info/dpqi/hp/brfss.htm.
- 44.Hahn EJ, Rayens MK, Butler KM, Zhang M, Durbin E, Steinke D. Smoke-free laws and adult smoking prevalence. Prev Med. 2008;47:206–9. doi: 10.1016/j.ypmed.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 45.Shopland DR, Anderson CM, Burns DM, Gerlach KK. Disparities in smoke-free workplace policies among food service workers. J Occup Environ Med. 2004;46:347–56. doi: 10.1097/01.jom.0000121129.78510.be. [DOI] [PubMed] [Google Scholar]
- 46.Lee K, Hahn EJ, Okoli CT, Repace J, Troutman A. Differential impacts of smoke-free laws on indoor air quality. J Environ Health. 2008;70(24-30):54. [PubMed] [Google Scholar]
- 47.Hahn EJ, Rayens MK, York N, Okoli CT, Zhang M, Dignan M, et al. Effects of a smoke-free law on hair nicotine and respiratory symptoms in restaurant and bar workers. J Occup Environ Med. 2006;48:906–13. doi: 10.1097/01.jom.0000215709.09305.01. [DOI] [PubMed] [Google Scholar]
- 48.Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328:977–80. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bartecchi C, Alsever RN, Nevin-Woods C, Thomas WM, Estacio RO, Bartelson BB, et al. Reduction in the incidence of acute myocardial infarction associated with a citywide smoking ordinance. Circulation. 2006;114:1490–6. doi: 10.1161/CIRCULATIONAHA.106.615245. [DOI] [PubMed] [Google Scholar]
- 50.Seo DC, Torabi MR. Reduced admissions for acute myocardial infarction associated with a public smoking ban: matched controlled study. J Drug Educ. 2007;37:217–26. doi: 10.2190/DE.37.3.a. [DOI] [PubMed] [Google Scholar]
- 51.American Nonsmokers' Rights Foundation. Overview list—how many smokefree laws? 2011. [cited 2011 Apr 1]. Available from: URL: http://www.no-smoke.org/pdf/mediaordlist.pdf.