Abstract
A 70-year-old male was admitted with a 2-week progressive course of severe cognitive impairment, scoring three on the Mini Mental State Examination. MRI of the brain showed confluent hyperintense areas in T2/FLAIR in the periventricular and subcortical white matter, extending to right parietal cortex and basal ganglia. Intra-arterial angiography was unremarkable. A targeted stereotactic brain biopsy disclosed a leukocytoclastic vasculitis. The patient improved on steroids. Leukocytoclastic vasculitis adds to the spectrum of histopathologic subtypes of primary angiitis of the central nervous system.
Background
Rapidly progressive dementia may be due to multiple causes and often presents a diagnostic challenge. Primary angiitis of the central nervous system (PACNS) is a form of vasculitis limited to the central nervous system (CNS), with protean and non-specific clinical manifestations, which must be considered in this setting.
In 1988, Calabrese and Malek proposed diagnostic criteria for PACNS that included development of an acquired otherwise unexplained neurological deficit, an angiogram with characteristic features of vasculitis, or a CNS biopsy specimen showing vasculitis.1 The most common histopathologic patterns of PACNS are granulomatous and lymphocytic.2
We present a rare case of rapidly progressive dementia due to a primary leukocytoclastic vasculitis of the CNS.
Case presentation
A 70-year-old male with history of depression was admitted with a 2-week progressive course of cognitive impairment. On neurological examination he was disoriented, had difficulties in naming and severe memory deficits, scoring three on the Mini Mental State Examination (MMSE).
Investigations
Brain MRI showed confluent hyperintense areas in T2/FLAIR in the periventricular and subcortical white matter, extending to the right parietal cortex and basal ganglia (figure 1A). Laboratory investigation disclosed a raised erythrocyte sedimentation rate (ESR) (80 mm/h). Cerebrospinal fluid findings included 121 inflammatory cells/mm3, raised protein level (154.2 mg/dl), negative serologies and cultures. Intra-arterial angiography was unremarkable.
Figure 1.
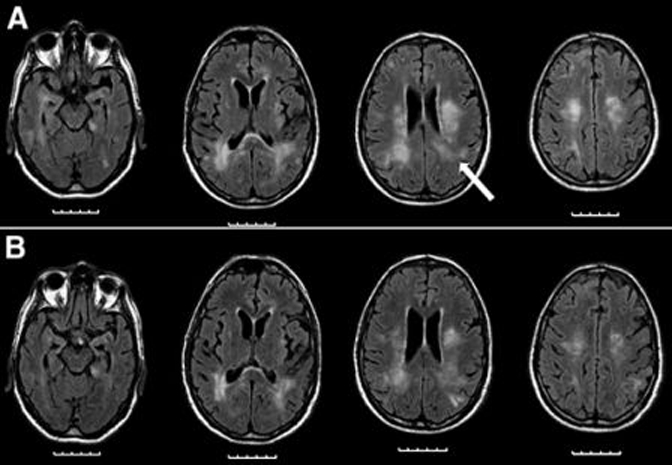
MRI, FLAIR: (A) At admission. Confluent hyperintense areas in T2/FLAIR in the periventricular and subcortical white matter, extending to the right parietal cortex and basal ganglia. The lesions were mildly hypointense in T1 and showed discrete gadolinium enhancement. Stereotactic biopsy site (arrow). (B) Two weeks after treatment.
A targeted stereotactic brain biopsy was performed, which disclosed a perivascular and transmural small vessel inflammatory infiltrate composed mainly of neutrophils, compatible with a leukocytoclastic vasculitis. There was also microglia activation, gliosis and sparse lymphocytes and neutrophils in the brain parenchyma. No fibrinoid necrosis, granulomas or giant cells were found (figure 2). Further laboratory investigation and body imaging excluded associated systemic inflammatory disease, vasculitis, infection or neoplasm.
Figure 2.
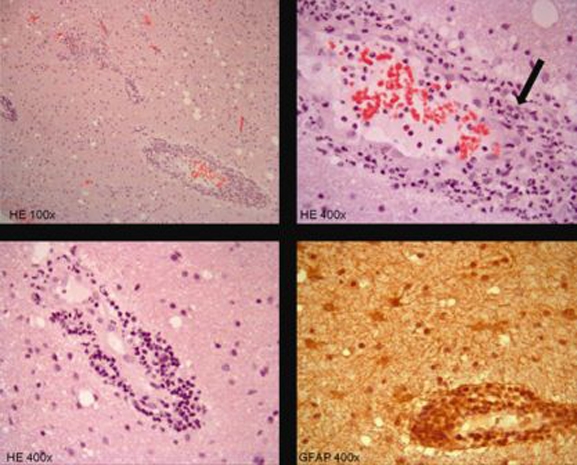
Brain biopsy: Transmural and perivascular small vessel inflammatory infiltrate. Fragmented neutrophils are seen (arrow). Microglia activation, gliosis, sparse lymphocytes and neutrophils in the brain parenchyma are also observed.
Differential diagnosis
Leukocytoclastic vasculitis with CNS involvement is occasionally described in sytemic vasculitis, such as in hypersensitivity vasculitis, microscopic polyangiitis, Behçet disease, Sjogrën syndrome, systemic lupus erythematosus and Mycoplasma pneumoniae infection.
In this case, the diagnosis of small vessel PACNS was considered as there were no additional features of systemic vasculitis.
Treatment
The patient was treated with oral prednisolone (1 mg/kg).
Outcome and follow-up
After 12 days on treatment, cognitive function improved, with a MMSE score of 14. ESR decreased to 38 mm/h. Lumbar puncture revealed 28 lymphocytes/mm3 and a protein level of 121.4 mg/dl. MRI images also improved, showing less extensive signal changes (figure 1B). Due to frequent urinary tract infections it was not possible to start cyclophosphamide. The patient was continued on oral prednisolone, showing no cognitive decline after a 6 months follow-up period.
Discussion
The diagnosis of small vessel PACNS was based on a CNS biopsy specimen showing vasculitis, normal cerebral angiography and exclusion of systemic involvement.
In this case the ESR was increased. Although acute-phase reactants are usually reported as normal in PACNS, Hankey found a moderate increase in ESR in about 30% of biopsy-confirmated PACNS patients.3
Miller et al reported three histopathologic patterns observed in PACNS. Granulomatous inflammation was the most common (58%) with nearly half of the cases associated with deposition of β-A4 amyloid in the vessel wall. Pure lymphocytic infiltration was described in 28% of the cases, and acute necrotising was seen in 14% of cases. No statistically significant differences in outcome were noted among the three histopathologic groups.2
In our case, the histopathologic features were compatible with a leukocytoclastic vasculitis and do not fit into any of these three categories. Leukocytoclastic vasculitis with CNS involvement is occasionally described in sytemic vasculitis, such as in hypersensitivity vasculitis, microscopic polyangiitis, Behçet disease, Sjogrën syndrome, systemic lupus erythematosus and M pneumoniae infection.4–8 However, isolated leukocytoclastic vasculitis of the CNS was only reported once, in a 70-year-old female with a similar clinical presentation.9
This case also emphasises the importance of brain biopsy in cases where cerebrovascular imaging is inconclusive. Notably, in the case of small vessel PACNS, intra-arterial angiography may be unremarkable. The role of brain biopsy is not limited to proving the diagnosis as it is also important for identification of PACNS mimics, especially infections and malignancy.10
No randomised studies on treatment of PACNS have been done, but most case series suggest a good outcome when patients are treated with glucocorticoids alone or in combination with cyclophosphamide.10 In this patient, treatment with steroids led to a partial cognitive improvement, showing no cognitive decline after a 6 months follow-up period.
Learning points.
-
▶
The differential diagnosis of rapidly progressive dementia is broad and presents a particular challenge, requiring a thorough investigation. Moreover, many of the rapidly progressive dementias may be treatable and PACNS must be considered in this setting.
-
▶
In the case of small vessel PACNS, intra-arterial angiography may be unremarkable.
-
▶
This case emphasises the importance of brain biopsy in cases where cerebrovascular imaging is inconclusive, such as in the case of small vessel vasculitis.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Calabrese LH, Mallek JA. Primary angiitis of the central nervous system. Report of 8 new cases, review of the literature, and proposal for diagnostic criteria. Medicine (Baltimore) 1988;67:20–39 [DOI] [PubMed] [Google Scholar]
- 2.Miller DV, Salvarani C, Hunder GG, et al. Biopsy findings in primary angiitis of the central nervous system. Am J Surg Pathol 2009;33:35–43 [DOI] [PubMed] [Google Scholar]
- 3.Hankey GJ. Isolated angiitis/angiopathy of the central nervous system. Cerebrovasc Dis 1991;1:2–15 [Google Scholar]
- 4.Younger DS. Vasculitis of the nervous system. Curr Opin Neurol 2004;17:317–36 [DOI] [PubMed] [Google Scholar]
- 5.Tang CW, Wang PN, Lin KP, et al. Microscopic polyangiitis presenting with capsular warning syndrome and subsequent stroke. J Neurol Sci 2009;277:174–5 [DOI] [PubMed] [Google Scholar]
- 6.Kleinig TJ, Koszyca B, Blumbergs PC, et al. Fulminant leucocytoclastic brainstem vasculitis in a patient with otherwise indolent systemic lupus erythematosus. Lupus 2009;18:486–90 [DOI] [PubMed] [Google Scholar]
- 7.Soylu A, Kavukçu S, Erdur B, et al. Multisystemic leukocytoclastic vasculitis affecting the central nervous system. Pediatr Neurol 2005;33:289–91 [DOI] [PubMed] [Google Scholar]
- 8.Guleria R, Nisar N, Chawla TC, et al. Mycoplasma pneumoniae and central nervous system complications: a review. J Lab Clin Med 2005;146:55–63 [DOI] [PubMed] [Google Scholar]
- 9.Castelnovo G, Bouly S, Vladut M, et al. [Rapidly progressive dementia disclosing primary angiitis of the central nervous system]. Ann Med Interne (Paris) 2001;152:273–5 [PubMed] [Google Scholar]
- 10.Hajj-Ali RA, Singhal AB, Benseler S, et al. Primary angiitis of the CNS. Lancet Neurol 2011;10:561–72 [DOI] [PubMed] [Google Scholar]


