Abstract
Laparoscopic surgery has become the gold standard for the surgical treatment of benign disorders of bile ducts, for example, symptomatic cholelithiasis. Nowadays, laparoscopic surgery is becoming less invasive by means of the advanced technologic capabilities. In this article, the authors present a 65-year-old patient with situs inversus totalis who was examined because of abdominal pain and dyspeptic symptoms. Ultrasonography and tomography revealed cholecystitis with gallstones (calculous cholecystitis), besides, it was observed that the liver and the gall bladder were on the left side and the heart, the stomach and the spleen were located on the right side of the patient. The patient was performed single incision laparoscopic cholecystectomy. The patient was discharged on the postoperative day 1. In the present article, the authors described how easily the single incision laparoscopic cholecystectomy could resolve the technical difficulties encountered in the patients with situs inversus totalis during the conventional laparoscopic surgery.
Background
Situs inversus totalis (SIT), which was first described by Fabricius in 1600, is a very rare clinical entity.1 The incidence of SIT that is characterised by the transposition of thoracoabdominal organs is thought to be in the range of 1:10 000–1:20 000.2 Although the incidence of cholelithiasis is not increased with SIT, it is known that there are approximately 30 cases who underwent laparoscopic cholecystectomy surgery to date. The laparoscopic cholecystectomy that was introduced by Moretin in 1987 has become the gold standard for the surgical treatment of benign disorders of bile ducts, for example, symptomatic cholelithiasis.3–6 The laparoscopic surgery is becoming less invasive by means of the advanced technologic capabilities. The main goal of minimally invasive techniques called the single incision laparoscopic surgery (SILS), the terms transumblical endoscopic surgery, laparoendoscopic single site surgery, natural orifice transumblical surgery and single laparoscopic incision transabdominal surgery is to provide a safe surgical treatment as well as the best cosmetic outcome.7 In this article, we present our minimally invasive surgical treatment procedure in a patient with SIT and cholelithiasis.
Case presentation
A 65-year-old woman was examined because of abdominal pain and dyspeptic symptoms lasting for 2 years. There was no specific event on her own and family medical history; on physical examination of the patient, peritoneal tenderness was found on the left upper quadrant. Laboratory tests were found to be within reference ranges, except leukocytosis (14000/mm3). On the chest postero-anterior x-ray, it was observed that the heart was located on the right side; (figure 1) abdominal ultrasonography revealed that the liver and the gallbladder were located on the left side of the patient (figure 2A). Besides, there were multiple millimetric gallstones in the gallbladder, thickness in the gallbladder wall and reactive fluid accumulation around the gallbladder. The patient was hospitalised with the presumed diagnosis of acute cholecystitis and was given medical treatment. On the abdominal tomography, it was found that the liver and the gallbladder were located on the left side and that the heart, stomach and the spleen were settled on the right side; therefore, the diagnosis of situs inversus totalis was made (figure 2B). After the medical treatment, an informed consent form was signed by the patient and she was prepared for the surgery. The patient was performed single incision laparoscopic cholecystectomy surgery (figure 3). The patient was allowed to eat and drink orally on the same day of surgery and was discharged on the first postoperative day.
Figure 1.

Chest x-ray point out dextrocardia.
Figure 2.
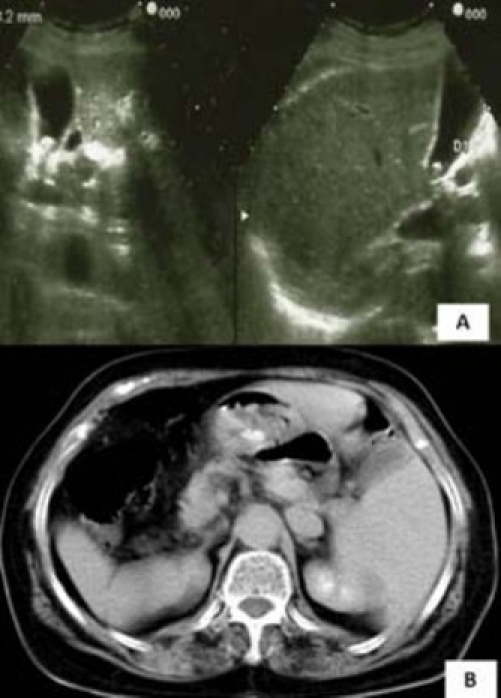
(A) Abdominal ultrasonography showed stones in gallbladder. (B) CT showed a right-sided spleen and stomach with a left-sided liver and a gallbladder containing stones.
Figure 3.
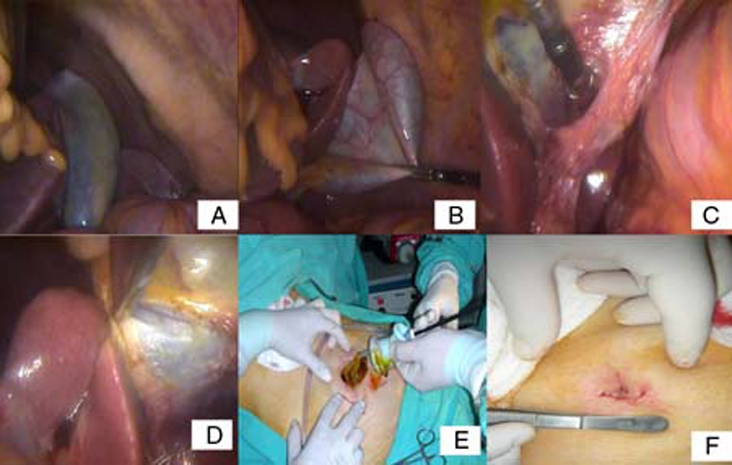
(A) The liver and the gallbladder are seen in the left upper quadrant of the abdomen. (B) The gallbladder was suspended from the fundus to the anterior wall of the abdomen. (C) The cystic duct and artery were identified dissecting Calot’s triangle above Rouviere’s sulcus. The cystic duct and artery were clipped and divided. (D) The gallbladder was excised retrogradely from the liver bed. (E) The gallbladder was extracted from the umbilical incision. (F) The skin was closed subcutaneously.
Treatment
The patient was operated under general anaesthesia and in the reverse Trendelenburg position. In contrast to the conventional laparoscopic cholecystectomy, the video monitor was positioned on the right side of the operating table, while the surgeon and other equipment were standing on the left side. The surgery was begun with the insertion of the SILS port through a 2 cm subumbilical incision. For optic camera, a 12 mm trocar site on the port was used; a flat-angle camera was used. Carbon dioxide (CO2) insufflation was started for achieving an intraabdominal pressure of 12 mm Hg. On the intraabdominal inspection, it was observed that the liver and the gallbladder were located on the left side of the patient, whereas the spleen and the stomach were on the right. The operative technique is similar to the procedure described by Tacchino et al. (figure 3). The fundus of the gallbladder was suspended to the anterior abdominal wall without emptying its content. Thus, Calot’s triangle was exposed allowing the dissection in a safe manner. With the help of two articulating instruments (roticulator endo grasp and roticulator endo dissect, 5 mm; Covidien), Calot’s triangle was dissected above the plane of Rouviere’s sulcus. The cystic artery and duct were clipped and then divided. The gallbladder was excised retrogradely. After haemostasis control, the gallbladder was extracted through umbilical incision together with the surgical instruments. The trocar entrance site was closed. The skin was closed subcutaneously.
Discussion
The SIT, an autosomal recessive disease, is encountered in 0.01% of the population.2 8 9 It is characterised by the transposition of thoracoabdominal visceral organs, however, central nervous system transposition does not occur.10 For this reason, clinical examination can be misleading in SIT patients. The SIT patients with symptomatic cholelithiasis feel the pain in the left upper quadrant only when peritoneal irritation occurs due to the events such as acute cholecystitis. When peritoneal irritation is absent, they describe the right upper quadrant or only epigastrium region.11–14 In contrast to what are expected, minor variations in intra- and extra-hepatic biliary, venous and arterial systems are found. However, although rare, it can be associated with some severe syndromes, for example, Kartagener syndrome.15 16 The hepatoduodenal ligament does not differ from that of orthotopic patients.17 18 Although there are many reports about SIT, as far as is known, there is no evidence that the incidence of cholelithiasis is greater in SIT.19 In the literature, there are 30 cases who were performed laparoscopic cholecystectomy because of symptomatic cholelithiasis.20 All case reports, except one, stated conventional laparoscopic surgical technique. The conventional laparoscopic surgery possesses certain technical problems in the patients with SIT. Because, the majority of the persons who invent the surgical instruments and two-thirds of the surgeons are right handed,21 the right handed surgeons experience dissection errors and loss of orientation.22 Therefore, in every case reports, each author describes his/her own technique to overcome that challenge of orientation and dissection. Nowadays, laparoscopic surgery, which is the gold standard for the surgical treatment of benign disorders of bile ducts, is becoming less invasive. The SILS having primary advantages on cosmetic outcomes and postoperative pain is introduced as a result of this evolution. However, right handed surgeons have to use their non-dominant hands in SILS in orthotopic symptomatic cholelithiasis cases and in conventional laparoscopic surgery in SIT patients.23 Therefore, the rates of iatrogenic bile duct injuries are becoming higher. In a study, it was proved that in laparoscopic surgery performed because of acute cholecystitis, the incidence of bile tree injury was three times higher in comparison with open surgery. But, this technical problem disappears when SIT patients are performed SILS because of symptomatic cholelithiasis, because, right handed surgeons can use their right hands for the dissection and their left hands for the traction. The antegrade dissection beginning from the fundus, which was proposed by Thomas B Hugh21 for open surgery and by Hyung Joon Han20 for laparoscopic surgery, is not a surgical technique widely applicable for all patients. In all SILS patients, Rouviere’s sulcus that is located lateral to the hepatoduodenal ligament must be identified as a reference point. Although Rouviere’s sulcus is open in 78% of the patients, it can be recognised in 90% of the cases. With a dissection performed above this sulcus, iatrogenic injuries can be minimalised.24 The only possibility increasing the risk of bile duct injury is the loss of orientation. This challenge can be resolved by educational courses about advanced laparoscopic procedures targeted for healthcare staff as well as surgeons.7
In conclusion, laparoscopic surgery is the gold standard for benign bile tree diseases in the patients with SIT. The difficulties brought by conventional laparoscopic surgical techniques can easily be overcome with SILS, as we described in our patient. The only disadvantage of SILS is that it requires much experience in practice.
Learning points.
-
▶
Situs inversus totalis is very rare disease and also conventional laparoscopic surgery for benign bile tree diseases includes technique difficulty. SILS can overcome these odds.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech A 2001;11:233–7 [DOI] [PubMed] [Google Scholar]
- 2.Al-Jumaily M, Hoche F. Laparoscopic cholecystectomy in situs inversus totalis: is it safe? J Laparoendosc Adv Surg Tech A 2001;11:229–31 [DOI] [PubMed] [Google Scholar]
- 3.Jaffray B. Minimally invasive surgery. Arch Dis Child 2005;90:537–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mosimann F. Laparoscopic cholecystectomy has become the new gold standard for the management of symptomatic gallbladder stones. Hepatogastroenterology 2006;53:1. [PubMed] [Google Scholar]
- 5.Bittner R. Laparoscopic surgery–15 years after clinical introduction. World J Surg 2006;30:1190–203 [DOI] [PubMed] [Google Scholar]
- 6.Sauerland S, Agresta F, Bergamaschi R, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc 2006;20:14–29 [DOI] [PubMed] [Google Scholar]
- 7.Ersin S, Firat O, Sozbilen M. Single-incision laparoscopic cholecystectomy: is it more than a challenge? Surg Endosc 2010;24:68–71 [DOI] [PubMed] [Google Scholar]
- 8.D’Agata A, Boncompagni G. [Video laparoscopic cholecystectomy in situ viscerum inversus totalis]. Minerva Chir 1997;52:271–5 [PubMed] [Google Scholar]
- 9.Demetriades H, Botsios D, Dervenis C, et al. Laparoscopic cholecystectomy in two patients with symptomatic cholelithiasis and situs inversus totalis. Dig Surg 1999;16:519–21 [DOI] [PubMed] [Google Scholar]
- 10.Aydin U, Unalp O, Yazici P, et al. Laparoscopic cholecystectomy in a patient with situs inversus totalis. World J Gastroenterol 2006;12:7717–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Southam JA. Left-sided gallbladder:: calculous cholecystitis with situs inversus. Ann Surg 1975;182:135–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heimann T, Sicular A. Acute cholecystitis with situs inversus. N Y State J Med 1979;79:253–4 [PubMed] [Google Scholar]
- 13.Drover JW, Nguyen KT, Pace RF. Laparoscopic cholecystectomy in a patient with situs inversus viscerum: a case report. Can J Surg 1992;35:65–6 [PubMed] [Google Scholar]
- 14.Goh P, Tekant Y, Shang NS, et al. Laparoscopic cholecystectomy in a patient with empyema of the gallbladder and situs inversus. Endoscopy 1992;24:799–800 [DOI] [PubMed] [Google Scholar]
- 15.Varano NR, Merklin RJ. Situs inversus: review of the literature, report of four cases and analysis of the clinical implications. J Int Coll Surg 1960;33:131–48 [PubMed] [Google Scholar]
- 16.Schiffino L, Mouro J, Levard H, et al. [Cholecystectomy via laparoscopy in situs inversus totalis. A case report and review of the literature]. Minerva Chir 1993;48:1019–23 [PubMed] [Google Scholar]
- 17.McDermott JP, Caushaj PF. ERCP and laparoscopic cholecystectomy for cholangitis in a 66-year-old male with situs inversus. Surg Endosc 1994;8:1227–9 [DOI] [PubMed] [Google Scholar]
- 18.Kamitani S, Tsutamoto Y, Hanasawa K, et al. Laparoscopic cholecystectomy in situs inversus totalis with “inferior” cystic artery: a case report. World J Gastroenterol 2005;11:5232–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McKay D, Blake G. Laparoscopic cholecystectomy in situs inversus totalis: a case report. BMC Surg 2005;5:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han HJ, Choi SB, Kim CY, et al. Single-incision multiport laparoscopic cholecystectomy for a patient with situs inversus totalis: report of a case. Surg Today 2011;41:877–80 [DOI] [PubMed] [Google Scholar]
- 21.Hugh TB. New strategies to prevent laparoscopic bile duct injury–surgeons can learn from pilots. Surgery 2002;132:826–35 [DOI] [PubMed] [Google Scholar]
- 22.Park SS, Min BW, Kim WB, et al. Double cancer of the stomach and oesophagus with situs ambiguus with polysplenia: the importance of preoperative evaluation. Dig Liver Dis 2005;37:799–802 [DOI] [PubMed] [Google Scholar]
- 23.Machado NO, Chopra P. Laparoscopic cholecystectomy in a patient with situs inversus totalis: feasibility and technical difficulties. JSLS 2006;10:386–91 [PMC free article] [PubMed] [Google Scholar]
- 24.Strasberg SM. Avoidance of biliary injury during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg 2002;9:543–7 [DOI] [PubMed] [Google Scholar]


