Abstract
Hypertrophy refers to an enlargement caused by an increase in the size but not in the number of cells. Generalised masticatory muscle hypertrophy may affect the temporalis muscle, masseters and medial pterygoids in a variety of combinations. Masseteric hypertrophy may present as either unilateral or bilateral painless swelling of unknown origin in the region of angle of mandible. It is a relatively rare condition and presents a diagnostic dilemma. While the history and clinical examination are important in differentiating this benign condition from parotid or dental pathology, they cannot necessarily exclude rare malignant lesion within the muscle. Advanced imaging modalities like CT and MRI are essential to confirm the diagnosis. Here the authors are reporting a unique case of masseter muscle hypertrophy along with medial pterygoid hypertrophy which was missed clinically but confirmed using CT and MRI.
Background
Hypertrophy of muscle refers to an increase in size of individual muscle fibres.1 Masticatory muscle hypertrophy can affect all the muscles of mastication, several muscles or just one muscle. It can occur either bilaterally or unilaterally, and most commonly the masseter muscles alone are affected. The involved muscles, which are variably enlarged and can be up to three times the normal size, are otherwise normal on all imaging studies.2 Several case reports on combined hypertrophy of temporalis and masseter muscles were published3–5 but concurrent occurrence of hypertrophy of masseter and medial pterygoid muscles is very rare.
Masseter muscle hypertrophy (MMH) may present as unilateral or bilateral, benign increase in size of masseter muscle. Its aetiology remains unexplained. It is most commonly seen in late adolescence and early adulthood, affects both males and females but has slight male predominance.6
Very little information concerning this entity has appeared in dental literature because MMH in itself is only occasionally associated with dental problems such as attrition, periodontal breakdown or temperomandibular joint problem. Unilateral or bilateral hypertrophy of the masseter muscle is characterised by an increase in the volume of the muscle mass.7
Clinically, patient may present with the complaint of unaesthetic appearance due to facial asymmetry or ‘square’ face appearance. Some patients complain of pain, headache, muscle stress, trismus and intermittent masticatory claudication.8 The radiographic findings associated with MMH are the bone spurs at the angle of mandible6 or flaring of mandibular angle2 and hyperostosis of mandibular ramus.9 CT and MRI scans provide useful diagnostic information regarding this condition.2 8 10
This entity must be carefully differentiated from unilateral compensatory hypertrophy (due to hypertrophy or hyperplasia in the contralateral side), masseter tumour, salivary gland disease, parotid tumour, parotid inflammatory disease, masseter muscle intrinsic myopathy,8 lipoma, vascular tumours, benign and malignant mandible tumours6 and metabolic disorders.1
Case presentation
A 19-year-old male patient reported with a chief complaint of asymmetry of face due to swelling on lower left back tooth region since 4 years.
History revealed that initially the swelling was smaller in size and became prominent over a period of 4 years. No history of any trauma, pain, discomfort, altered sensation and increase or decrease in salivary flow was elicited. There was no relevant family and medical history. However, there was a history of emotional stress, unilateral chewing and bruxism was elicited. Diet history revealed that the patient consumed mixed diet predominantly of fibrous nature.
Extra oral examination revealed a square faced patient with gross asymmetry on left side of face (figure 1). Inspection revealed a single, large swelling measuring around 6 cm in maximum diameter in anterior-posterior direction present on left angle to ramus area of mandible with no distension of overlying tissue. Palpation of swelling confirmed a contractile mass which yielded no fluctuation, no reducibility, no pulsation and no tenderness. It was firm in consistency all over when teeth were clenched together. Auscultation yielded no bruit. Mouth opening was normal. Temporomandibular joint (TMJ) showed well-coordinated and symmetrical movements with no clicking, crepitus or deviation to any side. Muscles of mastication were non-tender on palpation.
Figure 1.

Asymmetry of left side of face.
Intraoral examination revealed mild generalised attrition with no other significant findings (figure 2).
Figure 2.

Intraoral picture shows mild attrition.
Based on history and clinical examination, a provisional diagnosis of unilateral masseter muscle hypertrophy was made.
Investigations
All haematological and serological reports were within normal range. Orthopantomography and posteroanterior view of skull revealed prominence of mandibular angle and spur development on left side and increased soft tissue shadow bilaterally which was more marked on left side (figures 3 and 4).
Figure 3.
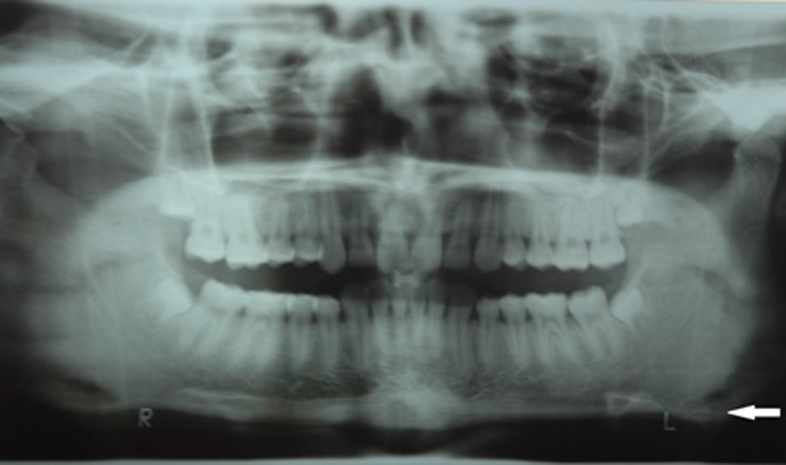
OPG shows bone spurs at angle of mandible (white arrow).
Figure 4.

PA skull view shows bone spurs at angle of mandible (white arrow).
CT scan with contrast with 5×5 spiral sections of that particular area of face reported the hypertrophy of left masseter. Another significant finding was the hypertrophy of left medial pterygoid muscle. Early enlargement of right masseter muscle was also revealed (figure 5). Parotid and submandibular glands were normal and symmetrical in position. Nasopharyngeal and oropharyngeal air columns were normal in course.
Figure 5.
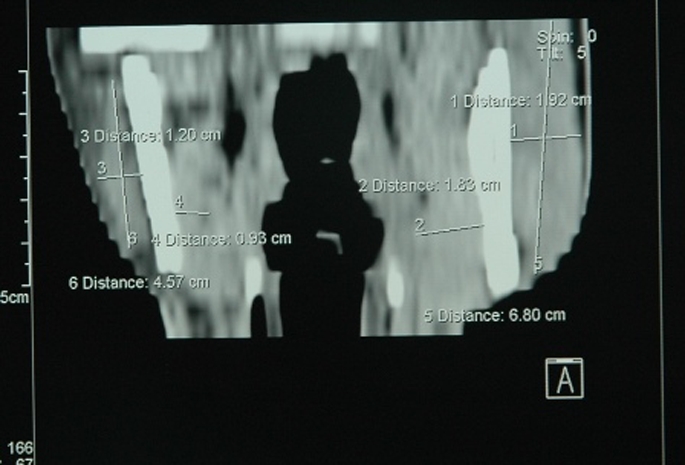
CT scan shows masseter and medial pterygoid hypertrophy on left side.
MRI scan taken in transaxial and coronal sections showed enlargement of left masseter and medial pterygoid muscle as compared to contra-lateral side. Medial pterygoid muscle was enlarged up to 85% in some planes on left side as compared to right side but muscle margins were preserved with well-defined surrounding fascial planes (figure 6).
Figure 6.

MRI shows masseter and medial pterygoid hypertrophy on left side.
Differential diagnosis
Parotid gland swellings, inflammatory myopathy, proliferative myositis, muscular dystrophy, lipomatosis, haemangioma, liposarcoma, lymphoma, lipoma, benign and malignant tumours of mandible.
Treatment
Surgical de-bulking of left masseter and medial pterygoid was performed under general anesthesia.
Outcome and follow-up
The patient was lost to follow-up and could not be contacted following discharge.
Discussion
In 1880, Legg reported a case of bilateral hypertrophy of the masseter and temporal muscle in a 10-year-old girl.6 Since its first description approximately 130 cases have been reported in literature.6 MMH is relatively a rare entity reported more frequently in people of Asiatic origin. According to one review, the average age of patients was 30 years, 57% were males, 60% had bilateral involvement and only 5% had concurrent temporalis muscle hypertrophy.6 This disease is uncommon in old people because it is possible that the swellings recede spontaneously over the years.3
Aetiology of MMH is still unclear. It can occasionally occur as a congenital form but mostly it presents as an acquired condition. It is generally considered to be functional hypertrophy initiated by number of condition such as bruxism, clenching, unilateral chewing, TMJ disorders, malocclusion and psychological factors.8 Some authors say that the most common cause MMH is bruxism because the muscle still works when the patient is asleep.11 In our case, the patient had emotional stress, unilateral chewing and bruxism.
Hypertrophy of medial pterygoid muscle has hardly been reported in literature. A compensatory adjustment to keep the mandible in centric position in case of a patient with hemifacial microsomia and unilateral condylar hypoplasia has been reported with medial pterygoid hypertrophy.12 Distraction osteogenesis of mandible can not only lengthen a deficient bone but may increase muscle mass.13
Clinically these patients are usually asymptomatic although some complain of discomfort over the posterior part of jaw and TMJ. Usually patients seek advice for the facial swellings, which is more commonly seen in late adolescence and early adulthood. The swelling is present over the ramus of mandible and becomes firm on clenching the teeth, when the coarse bundles of hypertrophied muscle can be palpated.11 The bony spurs at angle of mandible are a common finding and it can be observed in the anteroposterior radiograph of skull. They are caused by periosteal irritation and new bone deposition responding to increased forces exerted by muscle bundle. However, according to Bloem and Hoof, 20% of normal people have this finding and it cannot be considered a diagnostic aid.6
Diagnosis is based on history, clinical findings and findings of imaging modalities. Electro-myogram and neurological tests are of little importance in the diagnosis.8 Image modalities of MMH are CT and MRI. In our case, CT and MRI provided useful information about MMH and medial pterygoid hypertrophy.
Management of muscle hypertrophy is multifaceted. Para functional habits must be corrected. Dental restorations and occlusal adjustments to correct premature contacts are important. Non-surgical modalities of treatment include reassurance, tranquilisers or muscle relaxants, injection of Botulinum toxin type A 40–60 IU per muscle administered by intramuscular route. Surgical modality includes cosmetic surgery to reduce the bone prominence from mandibular angle.6 Extraoral approach was widely used earlier to manage MMH. Intraoral approach is now considered a better option with the availability of better tools and techniques.14 Removal of internal vertical band of the masseter muscle equivalent to approximately 2/3 of its thickness has been advocated.8
Learning points.
-
▶
Masseter muscle hypertrophy is a benign condition that can cause facial asymmetry and aesthetic concern in young individuals.
-
▶
Concurrent occurrence of masseter muscle hypertrophy along with medial pterygoid muscle makes it a rare entity which is difficult to diagnose clinically specially in the absence of oral manifestations.
-
▶
It may pose a diagnostic dilemma because it may be confused for various parotid gland disorders, orodental infections, vascular malformations and benign and malignant tumours of mandible.
-
▶
Advanced imaging modalities like CT and MRI scans are required for diagnosis of masseter muscle and medial pterygoid muscle.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology; Diseases of the Nerve and Muscles. Fourth edition Noida: Saunders; 2003:875 [Google Scholar]
- 2.Som PM, Curtin HD. Head and Neck Imaging, Fourth edition Vol. 2; St Louis: Mosby; 2003:1991 [Google Scholar]
- 3.Chrispal A, Boorugu HK. Benign masticatory muscle hypertrophy. J Assoc Physicians India 2009;57:764. [PubMed] [Google Scholar]
- 4.Lambert CD, Young JR. Hypertrophy of the branchial muscles. A case with unusual features. J Neurol Neurosurg Psychiatr 1976;39:810–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rokadiya S, Malden NJ. Variable presentation of temporalis hypertrophy–A case report with literature review. Br Dent J 2006;201:153–5 [DOI] [PubMed] [Google Scholar]
- 6.Sannomya EK, Gonçalves M, Cavalcanti MP. Masseter muscle hypertrophy: case report. Braz Dent J 2006;17:347–50 [DOI] [PubMed] [Google Scholar]
- 7.Peretta R, Melison M, Meneghello R, et al. Unilateral masseter muscle hypertrophy: morphofunctional analysis of the relapse after treatment with botulinum toxin. Cranio 2009;27:200–10 [DOI] [PubMed] [Google Scholar]
- 8.Rispoli DZ, Camargo PM, Pires JL, Jr, et al. Benign masseter muscle hypertrophy. Braz J Otorhinolaryngol 2008;74:790–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daramola OO, Sabino ML, Flanary VA. Unilateral muscle hypertrophy with mandibular ramus hyperostosis. Int J Pediatr Otorhinolaryngol Extra 2011. doi:10.1016/j.pedex.2011.06.001 [Google Scholar]
- 10.Schellhas KP. MR imaging of muscles of mastication. AJR Am J Roentgenol 1989;153:847–55 [DOI] [PubMed] [Google Scholar]
- 11.Da Silva K, Mandel L. Bilateral temporalis muscle hypertrophy: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:e1–3 [DOI] [PubMed] [Google Scholar]
- 12.Nakata S, Mizuno M, Koyano K, et al. Functional masticatory evaluation in hemifacial microsomia. Eur J Orthod 1995;17:273–80 [DOI] [PubMed] [Google Scholar]
- 13.Mackool RJ, Hopper RA, Grayson BH, et al. Volumetric change of the medial pterygoid following distraction osteogenesis of the mandible: an example of the associated soft-tissue changes. Plast Reconstr Surg 2003;111:1804–7 [DOI] [PubMed] [Google Scholar]
- 14.de Holanda Vasconcellos RJ, de Oliveira DM, do Egito Vasconcelos BC, et al. Modified intraoral approach to removal of mandibular angle for correction of masseteric hypertrophy: a technical note. J Oral Maxillofac Surg 2005;63:1057–60 [DOI] [PubMed] [Google Scholar]


