Abstract
Formation of cystic artery pseudo aneurysm is a rare complication of a common problem that is, acute cholecystitis. Here the authors present a case of 58-year-man with history of upper abdominal pain and fever. Ultrasound initially showed huge subhepatic collection and distended gall bladder with gall stones. Later on, CT scan showed the cystic artery pseudo aneurysm in the wall of gall bladder. Selective angioembolisation of cystic artery followed by elective open cholecystectomy was done and patient recovered well postprocedure. Pathology report later on showed xanthogranulomatous cholecystitis. Case emphasises the need of high index of suspicion to diagnose this rare entity, which in this case was successfully treated with two staged approach that is, angioembolisation of aneurismal vessel and then interval open cholecystectomy.
Background
Acute cholecystitis is a very common condition in our day to day practice but underlying pseudoaneurysm may be life threatening if not treated urgently. This report will help the physician to have high index of suspicion in haemodynamically unstable patients presenting as acute cholecystitis especially with unusual radiological findings.
Haemobilia is a rare condition1 and is defined as bleeding from biliary tree which may remain asymptomatic or present as malena or hemetamesis. Most common cause of haemobilia is liver trauma.2 Other less frequent causes may be post cholecystitis, postpancreatitis,3 postlaparoscopic cholecystectomy, hepatic and biliary neoplasm or bleeding problems (polyarteritis nodosa and haemophilia).3 Cystic artery pseudo aneurysm is a very rare cause of haemobilia and only 16 cases are reported in literature to date. Here we present case of cystic artery pseudo aneurysm as a result of acute cholecystitis.
Case presentation
Our patient is a 58-year-old gentleman who presented in emergency room with a 10 day history of right upper quadrant pain followed by high-grade fever and vomiting. He was initially evaluated in local hospital and then referred to us. He had hypertension and history of ischemic heart disease for which he had been in follow-up with cardiologist. History was unremarkable for any surgery and abdominal/hepatic trauma. On examination, he had tachycardia, he was febrile, dehydrated and jaundiced. Abdominal examination revealed localised tenderness in right hypochondrium and hepatomegaly 3 cm below right costal margin.
Lab results showed haemoglobin of 8.5 gm%, leukocyte counts were 23000/mm3 with neutrophilia and platelets were 457000/mm3, total bilirubin was 3.1 mg% (0.6–1 mg%) with direct of 1.9 mg%, γ glutamytransferase of 442 IU/l (normal 3–50 IU/l), alanine aminotransferase of 46 IU/l (normal 0–55 IU/l), alkaline phosphatase of 623 IU/l (normal 28–124 IU/l), lactate dehydrogenase of 543 IU/l (normal 253–58 IU/l).Lipase, amylase and coagulation profile were within normal range.
Ultrasonography (US) initially revealed a huge collection(141×146×93 mm) in left sub hepatic area along with swollen pancreatic head and sonographic evidence of acute calculus cholecystitis (figure 1). To further delineate the situation, CT was done which revealed well-defined enhancing lesion in the wall of gall bladder along with high density signal (blood) within gall bladder and redemonstration of left sub hepatic collection (figure 2). So diagnosis of acute cholecystitis leading to aneurysm formation was made. Collection was attributed to rupture of gall bladder into sub hepatic area. He was resuscitated, intravenous antimicrobials were started. US guided percutaneous drain was placed in sub hepatic collection which drained 420 ml of reddish brown pus mimicking altered blood. Subsequently, culture of this pus grew Staphylococcus aureus. Selective cystic artery angiography was done which confirmed the presence of cystic artery pseudo aneurysm. This aneurysm was angioembolised using coils (figure 3). Patient responded well to these measures. Because of ongoing sub clinical sepsis and evaluation by cardiologist for his previous cardiac history, interval cholecystectomy was planned. He underwent open cholecystectomy after 4 weeks of angioembolisation. Peroperatively gall bladder was found shrunken and necrosed with multiple small calculi. Histopathology later came out to be xanthogranulomatous cholecystitis. Postoperatively, patient recovered well and was doing well after 4 months of surgery (lost to follow-up for 3 months).
Figure 1.

Coronal view of CT scan demonstrating aneurysm (arrow) and collection.
Figure 2.

Axial view of CT scan demonstrating subhepatic collection in relation to the cystic artery aneurysm and adjacent structures (arrow).
Figure 3.
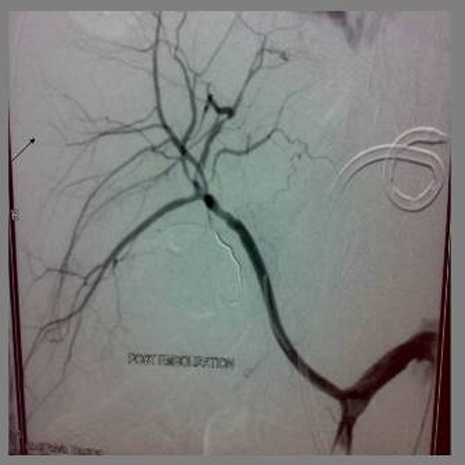
Picture after embolisation of aneurysm with micro coils (arrow).
Investigations
Lab results showed haemoglobin of 8.5 gm%, leukocyte counts were 23000/mm3 with neutrophilia and platelets were 457000/mm3, total bilirubin was 3.1 mg% (0.6–1 mg%) with direct of 1.9 mg%, γ glutamytransferase of 442 IU/l (normal 3–50 IU/l), alanine aminotransferase of 46 IU/l (normal 0–55 IU/l), alkaline phosphatase of 623 IU/l (normal 28–124 IU/l), lactate dehydrogenase of 543 IU/l (normal 253–58 IU/l). Lipase, amylase and coagulation profile were within normal range.
Outcome and follow-up
Postoperatively patient recovered well and was doing well after 4 months of surgery (lost to follow-up for 3 months).
Discussion
The present case reflects the very rare complication of a very common entity of acute cholecystitis. In this case, acute inflammation secondary to gall stones has led to formation of cystic artery pseudo aneurysm. Although the precise mechanism of aneurysm formation is not well understood, it is hypothesised that it is a constant inflammatory process that lead to erosion in elastic and muscular components of arterial wall ultimately resulting in aneurysm formation. But the rarity of aneurysm formation also hypothesised the possibility of early thrombosis of cystic artery secondary to inflammation.4
In literature, only 16 cases have been reported, of which 11 were males and five were females with median age of presentation at 65 years. Classically patients presents with Quinke’s triad (upper quadrant pain, obstructive jaundice, gastrointestinal haemorrhage). Of all reported cases, 56% presents with this typical triad and same number of patients had aneurysm in wall of gall bladder (as compared to those having aneurysm outside the wall before entering of vessel in gall bladder wall). Our patient also presented with Quinke’s triad and had aneurysm within gall bladder wall.
In all reported cases, US was used as initial tool of investigation but is not accurate modality to diagnose cystic artery pseudo aneurysm. CT scan is a better option to diagnose and to retrieve the location and relations of aneurysm to surrounding viscera. In our patient, US was not able to pick up cystic artery pseudo aneurysm which was subsequently seen on CT scan. But still the gold standard to diagnose cystic artery pseudo aneurysm especially smaller ones is the selective hepatic angiography. Angiography being superior in way, that beside diagnosis of disease it also offers therapeutic advantage for aneurysms.5 Other less commonly used tests are Doppler US, dynamic MRI and endoscopic retrograde cholangiography.5 None of these investigations was used in our patient.
Different treatment strategies were used to treat disease in all reported cases. In our patient, we used two stepped approach that is, angioembolisation of aneurysm and then cholecystectomy. Only two out of 16 reported cases have used this approach and were found successful.3 5 Other methods of treatment which were used are external biliary drainage followed by cholecystectomy. In one patient only angioembolisation of aneurysm was done without cholecystectomy because of medical illness of that patient. It is important to mention that the definitive treatment for cystic artery pseudoaneurysm is cholecystectomy, external biliary drainage or angioembolisation are time buying temporising measures. To conclude, the present case emphasises the need of early disease suspicion and good outcome with this two step approach especially when the condition of patient does not allow early operative intervention.
Learning points.
-
▶
Interventional radiology has a promising role in managing unstable patients.
-
▶
For complete recovery, patient must undergo interval cholecystectomy.
-
▶
High index of suspicion is one of the most important factors for good outcome in this fatal condition.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery 1948;24:571–86 [PubMed] [Google Scholar]
- 2.Croce MA, Fabian TC, Spiers JP, et al. Traumatic hepatic artery pseudoaneurysm with hemobilia. Am J Surg 1994;168:235–8 [DOI] [PubMed] [Google Scholar]
- 3.de Perrot M, Berney T, Bühler L, et al. Management of bleeding pseudoaneurysms in patients with pancreatitis. Br J Surg 1999;86:29–32 [DOI] [PubMed] [Google Scholar]
- 4.Barba CA, Bret PM, Hinchey EJ. Pseudoaneurysm of the cystic artery: a rare cause of hemobilia. Can J Surg 1994;37:64–6 [PubMed] [Google Scholar]
- 5.Maeda A, Kunou T, Saeki S, et al. Pseudoaneurysm of the cystic artery with hemobilia treated by arterial embolization and elective cholecystectomy. J Hepatobiliary Pancreat Surg 2002;9:755–8 [DOI] [PubMed] [Google Scholar]


