SUMMARY
Obstructive sleep apnoea syndrome in a child is characterized by prolonged episodes of obstructive hypopnoea and/or apnoea of upper airway leading to morbidity. The most common risk factor is adeno-tonsillar hypertrophy. Obstructive sleep apnoea syndrome diagnosis is based on clinical ENT evaluation and an instrumental approach, such as pulse oximetry or the gold standard overnight polysomnography. The aim is to establish, in a population of children with suspected obstructive sleep apnoea syndrome, the frequency of this disorder, the effect of adenotonsillectomy and the risk of post-operative complications. A total of 481 patients (297 male, 184 female) with suspected obstructive sleep apnoea syndrome (aged 2-14 years) were evaluated between March 2007 and April 2010 and divided into 3 morphological phenotypes: classic, adult and congenital. All patients underwent ENT assessment and a pulse oximetry with 4 channels cardiopulmonary monitoring. The examination following the Brouillette criteria was defined as negative, positive or inconclusive; when positive, adenotonsillectomy was the first therapeutic approach. At 6 months after surgery, all patients underwent check-up pulse oximetry. Of the overall sample, 96% of the patients had a classical phenotype, 3% an adult type and 1% a congenital type. The monitoring resulted pathological in 19% (17% of them were at increased post-operative risk), negative in 61% and inconclusive in 20%. All 5 patients with congenital phenotype were positive. Of the positive patients, 86% underwent adenotonsillectomy and a control pulse oximetry 6 months thereafter, 96% resulted negative. Pulse oximetry was efficient in order to avoid incorrect surgery indications, improving appropriateness and safety of adenotonsillectomy in children with obstructive sleep apnoea syndrome. Adenotonsillectomy showed a success rate of 96% and there were no episodes of post-surgery complications in particular in those patients at increased risk.
KEY WORDS: OSAS, Pulse oximetry, Adenotonsillectomy, Sleep disorder breathing, Brouillette criteria
RIASSUNTO
La sindrome delle apnee ostruttive nel sonno (OSAS) pediatrica è caratterizzata da prolungati episodi di ostruzione delle alte vie aeree, ipopnea e/o apnea, che possono condurre a complicanze. Il fattore di rischio più comune è l'ipertrofia adenotonsillare. Il percorso diagnostico include sia una valutazione clinica ORL sia un approccio strumentale, come la pulsiossimetria o l'indagine polisonnografica notturna (gold standard). L'obiettivo è determinare, in una popolazione di bambini con sospetta OSAS, la frequenza di tale disturbo, l'efficacia dell'adenotonsillectomia ed il rischio di complicanze post-operatorie. 481 pazienti (297 maschi e 184 femmine) con sospetta OSAS (di età 2-14 anni) sono stati valutati tra marzo 2007 e aprile 2010 e suddivisi in 3 fenotipi morfologici: "classic", "adult" e "congenital". Tutti i pazienti sono stati sottoposti a valutazione ORL e a pulsiossimetria 4 canali con monitoraggio cardiorespiratorio. L'esame seguendo i criteri di Brouillette ha dato risultato negativo, positivo o non conclusivo; quando positivo, l'adenotonsillectomia è stato il primo approccio terapeutico. Dopo 6 mesi dall'intervento i pazienti sono stati sottoposti ad una pulsiossimetria di controllo. Del campione totale il 96% dei pazienti mostrava un fenotipo "classic", il 3% fenotipo "adult" e l'1% "congenital". Il monitoraggio è risultato patologico nel 19% (il cui 17% erano soggetti ad aumentato rischio di complicanze post-operatorie), negativo nel 61% dei casi e non conclusivo nel 20%. L'86% dei pazienti positivi sono stati sottoposti ad adenotonsillectomia e a una pulsiossimetria di controllo 6 mesi dopo, negativa nel 96% dei casi. La pulsiossimetria risulta efficace nel migliorare l'appropriatezza e la sicurezza dell'adenotonsillectomia nei bambini affetti da OSAS al fine di evitare un'indicazione chirurgica non corretta. L'adenotonsillectomia ha risolto la sintomatologia nel 96% dei casi senza episodi di complicanze post-operatorie, in particolare tra i pazienti ad aumentato rischio.
Introduction
Obstructive sleep apnoea syndrome (OSAS) in children is a respiratory disorder characterized by prolonged episodes of partial obstruction (obstructive hypopnoea) and/ or complete obstruction (obstructive apnoea) of the upper airway that disrupt normal ventilation and nocturnal sleep architecture.
The first modern description of OSAS is attributed to William Osler, who in 1901 in The Principles and Practice of Medicine 1 described a child with adenoidal facies, chest deformity, nasal voice, hearing, taste and smell compromised due to the large amount of nasopharyngeal secretions, enuresis, mental retardation and oral breathing, which results in a look he referred to as "stupid". If untreated, the paediatric OSAS can lead to morbidity frameworks involving many organs and systems. The immediate consequences of OSAS in children are behavioural problems, hyperactivity, learning and concentration difficulties, systemic and pulmonary hypertension, cardiac hypertrophy, impairment in body height and weight 2-7. Recognizing and early treatment of OSAS in children prevents the occurrence of its more serious complications. Paediatric OSAS affects children of all ages, from newborn to adolescence, with a higher prevalence in preschool age (2-6 years). Currently, however, epidemiological data are very few and conflicting. The prevalence of sleep-disordered breathing in pre-school and school age children varies considerably: from 3.2% to 27% for snoring (in most studies, 1/3 of the children aged 2-6 years have been claimed to snore occasionally and 10-14% to snore frequently) and from 0.5% to 3% due to OSAS 8. Clinically, patients with respiratory disease present a set of symptoms which can be divided into daytime and nighttime. Among the main nocturnal symptoms, are: mouth breathing, noisy breathing or snoring during most nights, sleep apnoea, restless sleep, particular positions during sleep (hyperextension of the head, sitting on the bed), profuse sweating, forced breathing, parasomnia such as the presence of pavor nocturnus, enuresis and somniloquio. The daytime symptoms, instead, consist in: hyperactivity, presence of attention deficits resulting in poor school performance, irritability 3 5-7.
Targets of diagnosis of OSAS are: differentiating primary snoring from OSAS, identifying patients at risk of complications, avoiding unnecessary operations in patients without risk of complications, recognizing patients at high risk of post-operative complications so that appropriate precautions can be taken before and after surgery.
Diagnostic workup in paediatric OSAS combines history and clinical examination and instrumental evaluation and refer to children aged 6 months to 16 years. The diagnostic gold standard of OSAS is the standard overnight polysomnography 9 10. However, given the scarcity of centres with polysomnograph equipment and the costs involved, simplified and less expensive screening techniques are now available. We used as a screening test, namely, the home pulse oximetry, because it is an easy technique to use, which requires a limited number of channels and maintains an excellent standard of reliability 11. Pulse oximetry, as reported in the literature, reaches a positive predictive value of 97% and a negative predictive value of 47%. These data show that this examination is able to distinguish primary snoring from obstructive syndrome only when the test result is positive 11. When the result is negative, or inconclusive, patients undergo a second level exam, such as polysomnography, which can be performed at home, recording cardio-respiratory parameters and body position, distinguishing obstructive apnoea, neurological apnoea and/or hypopnoea, and establishing the presence and severity of SDB (sleep-disordered breathing) in children 12 13.
Adenotonsillar hypertrophy is the most common risk factor in the genesis of sleep respiratory disorders and literature data show that adenotonsillectomy allows a reduction in symptoms as well as normalization of the polysomnographic framework in most cases. In fact, if adenotonsillar hypertrophy is the predominant factor contributing to OSAS in children, removal of tonsils and adenoids should lead to immediate resolution of airway obstruction during sleep 14. Other causes of OSAS are nasal obstruction (caused by allergic rhinitis, sinusitis etc.), obesity, laryngeal masses, laryngomalacia, tracheomalacia, cranium-facial anomalies, neurological or neuromuscular disorders. The aim of this study was to determine, in a population of children with suspected OSAS, the frequency of this disorder, the effect of adenotonsillectomy and the risk of post-operative complications.
Material and methods
A total of 481 patients (297 male, 184 female), age range 2 to 14 years, all with suspected OSAS, were evaluated in the period between March 2007 and April 2010. In this study, the diagnostic and therapeutic iter applied to patients follows the National Guidelines of 2008 14. During ENT evaluation, children were divided into three phenotypes: the classic type (with adenoidal facies characterized by elongated face, eyes, halos, loss of seal lips with hypotonic lip, arched and narrow palate and adenotonsillar hypertrophy) 7 16; the adult type (with obesity, short and stubby neck, and reduced vertical dimension of the lower third of face); the congenital type (mostly characterized by micrognathia, mandibular hypoplasia, macroglossia, retrognathism, complex cranium-facial abnormalities). In the overall sample, 4 patients presented Down syndrome and one had a polymalformative syndrome.
All patients assigned for the study of sleep were selected during an ENT assessment based on the physical examination and the type of daytime and nocturnal symptoms observed. The examination was completed with a detailed ENT evaluation. The nasal and rhino-pharyngeal regions were assessed with a flexible paediatric endoscope. Adenoidal hypertrophy depending on the rhino-pharyngeal space occupied, was graded from 1 to 4, as follows: Grade 1, from 0 to 25% of the rhino-pharynx, Grade 2, from 25 to 50%, Grade 3, from 50 to 75% and Grade 4 > 75%. The nose was assessed for septal deviation, mucosal thickening and polyps. The oral cavity was examined for tonsillar enlargement, tongue and soft palate size and appearance. The size of the tonsils was graded through a scale from 0 to a maximum of 4 when the tonsils meet the midline. The clinical examination was completed with an orthodontic examination to evaluate the morphology of the dental arch and the dental occlusion. All data, for each patient, were recorded on a dedicated evaluation form.
After ENT examination, all patients considered in the study underwent a pulse oximetry with 4-channel cardiopulmonary monitoring. The equipment as well as performing pulse oximetry, also provides heart-rate monitoring with continuous recording of a 3-lead electrocardiogram (ECG) and recording of chest movement. Therefore, with this instrument, it is possible to record: impedance respiratory chest curve, ECG, blood oxygen saturation and plethysmography. Plethysmography is essential for proper reporting, which must be scrupulously carried out manually by the scorer, as it offers the possibility to control signal quality and to eliminate desaturations related to artefacts. Artefacts can be technical (loss of contact between the power supply and equipment or between equipment and saturation sensor or loss of contact between the sensor and the patient's skin) or physiological (patient movement or hypoperfusion). Pulse oximetry, in all cases, was placed, in our ward, by trained medical staff. The doctor also had the responsibility of informing the parents about the basic operation of the monitor, on alarms, and the connection of electrodes placed, by the physician, to the monitor before bedtime. During installing of the equipment, the patient's parents were given a diary in which to note down the events occurring during the night and were requested to answer the Brouillette questionnaire to be completed at home. All recordings were made at the patients' home. The total recording time required was at least 8 hours.
The evaluation was performed according to Brouillette's criteria 11 under which desaturation is defined as a drop in oxygen saturation above 4% and clusters of desaturation as the presence of five or more desaturations collected in a time between 10 and 30 minutes. An examination is defined as negative, when there is an absence of clusters of desaturation and lack of desaturation below 90%; positive when there are 3 or more clusters of desaturation and at least three desaturations below 90% and inconclusive when it does not match previous criteria. Patients who have a nadir SpO2 less than 80% may be considered at an increased post-operative risk 9-11. In patients with positive pulse oximetry adenotonsillectomy was indicated. Patients at increased risk of post-operative respiratory compromise were observed at strict follow-up for 24 hours after the adenotonsillectomy with pulse oximetry, monitoring the cardio-respiratory parameters and saturation. All patients who underwent surgery were observed at follow-up with systematic ambulatory monitoring for 7 to 15 days after surgery. At 6 months after surgery, all patients were again submitted to a check-up with pulse oximetry.
Results
Observation of the objective data collected during the ENT evaluation showed that 460 out of 481 patients (96%) had a classical phenotype. In 16 out of 481 patients (3%), the child presented an adult type phenotype and in 5 patients out of 481 (1%) this was found to be a congenital type phenotype. In particular, among these 5 patients, 4 had Down's syndrome and one had a polymalformative syndrome characterized by micrognathia and mandibular hypoplasia. Two patients with Down's syndrome presented severe adenotonsillar hypertrophy (Grade IV ) whereas the other two patients had Grade I adenotonsillar hypertrophy. The nocturnal cardio-respiratory monitoring was
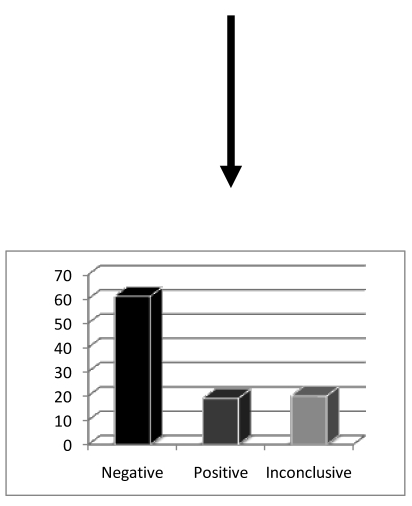
The nocturnal cardio-respiratory monitoring was found to be pathological in 92 patients (19%), negative in 295 patients (61%) and inconclusive in 94 patients (20%). Sixteen patients among those with positive pulse oximetry (17%) were considered potentially at increased post-operative risk. All 5 patients with congenital type phenotype were positive for pulse oximetry (Fig. 1).
Fig. 1.
Outcome of nocturnal cardio-respiratory monitoring.
A total of 79 out of the 92 (86%) patients positive at the pulse oximetry test underwent adenotonsillectomy. In five cases (5%), the parents refused surgery despite being fully aware of the consequences and risks associated with such a decision. Two patients with Down's syndrome were subjected to continuous positive airway pressure (CPAP) ventilation as there was no significant obstruction of the upper airways (low degree of tonsillar hypertrophy and absence of adenoidal hypertrophy). Phase II surgery (maxillo-mandibular advancement, tongue base resection) was not performed as this was considered too complex and invasive for this particular patient population. Currently, 6 patients are still on the waiting list for adenotonsillectomy. Among the positive patients, who were indicated to undergo adenotonsillectomy, in 16 cases (17%) the pulse oximetry SpO2 nadir was less than 80% and, therefore, it was necessary to use the pulse oximeter, for 24 hours after surgery, in order to monitor saturation and cardio-respiratory parameters as these were patients at increased post-operative risk. The average hospitalization time related to all the patients considered in the study was 24 hours. In the 79 children submitted to surgery, control pulse oximetry was carried out 6 months later; 76 of them (96%) were negative for OSAS while 3 (4%) patients were still positive (Fig. 2); 2 were Down's syndrome and one was affected by a polymalformative syndrome where other functional and anatomical factors besides adenotonsillar hypertrophy, caused the disorder; all 3 patients were started on a cycle of adaptation with CPAP.
Fig. 2.
Patients' evaluation 6 months after adenotonsillectomy.
In our series, no complications were recorded during or after surgery. Moreover, in none of the 16 patients with a higher post-operative risk was desaturation below 80% or cardio-respiratory compromise observed that might require medical attention in the 24 hours post-operative monitoring 17. Patients with negative or inconclusive pulse oximetry were retested after 12 and 6 months, respectively, and underwent a second level examination (polysomnography) if signs and symptoms were still present. Our study is still on-going and data will be presented in future reports.
Discussion
Aim of the study is to establish, in a population of children with suspected OSAS, the frequency of this disorder, the effect of adenotonsillectomy and the risk of post-operative complications. As previously mentioned, all children undergoing sleep studies, using pulse oximetry, showed clinical signs and symptoms, in various combinations, sufficient to lead to the suspicion of obstructive sleep apnoea. Results of the present investigation, have clearly demonstrated the effectiveness of the study of sleep in improving appropriateness and safety of adenotonsillectomy in patients with OSAS. In particular, it was found that of about 481 patients studied, presenting signs and symptoms of paediatric OSAS, only 19% were actually suffering from disease, at nocturnal pulse oximetry, and, therefore, were eligible for surgery 18 19.
In the surgical approach of paediatric OSAS, the primary purpose is to resolve or, at least, improve the clinical situation. From the literature, it is clear that adenotonsillecadenotonsillectomy is the gold standard of care in children with OSAS since it eliminates the clinical symptoms and leads to normalization of polysomnography in a large percentage of cases 17. In fact, adenotonsillectomy is considered the first and most effective therapeutic procedure in cases of OSAS in children, even in those children with associated syndromes 17. This evidence was confirmed in the present study as in the 79 patients undergoing adenotonsillectomy a success rate of 96% was achieved. However, the 3 failures concerning two patients with Down's syndrome and one patient with polymalformative syndrome, were not suffering from adenotonsillar hypertrophy but other factors, such as the genesis of an anatomical and functional disorder, took place. These patients were treated by ventilatory support with CPAP. As for patients with an increased risk of post-operative complications, a percentage of 17% of patients with positive pulse oximetry was achieved, these data are consistent with the literature 19. As shown in our study, patients with OSAS and, in particular, in the 16 patients at increased risk of postoperative respiratory distress, there were no episodes of post-operative complications. In this respect, it should not be forgotten that the literature shows how post-operative complications, especially among patients considered at risk, can cause respiratory disorders due to post-operative obstruction as a result of oedema, laryngeal spasm and nasal secretions. Children with OSAS are more sensitive to the depressant effect of anaesthetics and analgesics, in respiratory centres, and also show altered neuromuscular control in the upper airways 20. This demonstrates, despite reports in the literature 21, the possibility to operate these patients in hospitals not equipped with paediatric resuscitation, without endangering patients' lives, through the application of protected intervention methods (careful evaluation in the presence of specialists in the immediate peri-operative anaesthesia, cardiopulmonary monitoring for 24 hours after surgery) and availability of resuscitation structure, if needed.
Finally, we wish to point out as the mere clinical history, even if essential in the diagnostic procedure of paediatric OSAS, it is not enough to make a correct diagnosis of OSAS. In fact, we demonstrated a great difference between patients with suspected OSAS and those actually affected by this disease. Without correct application of the diagnostic procedure by means of pulse oximetry, most patients with suspected OSAS would have undergone unnecessary adenotonsillectomy which can be considered an overtreatment for these patients who presented merely primary snoring and not an evident OSAS.
Pulse oximetry is an essential examination in the diagnosis of OSAS above all for children suffering from this disease in order to avoid an incorrect indication to surgery. For this reason, pulse oximetry should be performed in all surgical units dealing with paediatric adenotonsillectomy.
References
- 1.Osler W. The Principle and Practice of medicine. New York: D. Appleton and Company; 1901. [Google Scholar]
- 2.Montgomery-Downs HE, Crabtree VM, Gozal D, et al. Cognition, sleep and respiration in at-risk children treated for obstructive sleep apnoea. Eur Respir J. 2005;25:336–342. doi: 10.1183/09031936.05.00082904. [DOI] [PubMed] [Google Scholar]
- 3.Gozal D, Pope DW., Jr Snoring during early childhood and academic performance at ages thirteen to fourteen years. Pediatrics. 2001;107:1394–1399. doi: 10.1542/peds.107.6.1394. [DOI] [PubMed] [Google Scholar]
- 4.Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4-5 year olds. Arch Dis Child. 1993;68:360–366. doi: 10.1136/adc.68.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barkley RA. Attention-deficit/hyperactivity disorder. In: Mash EJ, Barkley RA, editors. Child Psychopathology. New York: Guilford Press; 1996. [Google Scholar]
- 6.Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102(3 Pt 1):616–620. doi: 10.1542/peds.102.3.616. [DOI] [PubMed] [Google Scholar]
- 7.Guilleminault C, Partinen M, Praud JP, et al. Morphometric facial changes and obstructive sleep apnea in adolescents. J Pediatr. 1989;114:997–999. doi: 10.1016/s0022-3476(89)80447-0. [DOI] [PubMed] [Google Scholar]
- 8.Brunetti L, Rana S, Lospalluti ML, et al. Prevalence of obstructive sleep-apnea syndrome in a cohort of 1207 children of southern Italy. Chest. 2001;120:1930–1935. doi: 10.1378/chest.120.6.1930. [DOI] [PubMed] [Google Scholar]
- 9.Villa MP, Brunetti L, Bruni O, et al. Guidelines for the diagnosis of childhood obstructive sleep apnea syndrome. Minerva Pediatr. 2004;56:239–253. Gruppo di studio interdisciplinare disturbi respiratori nel sonno. [PubMed] [Google Scholar]
- 10.Muzumdar H, Arens R. Diagnostic issues in pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:263–273. doi: 10.1513/pats.200707-113MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brouillette RT, Morielli A, Leimanis A, et al. Nocturnal pulse oximetry as an abbreviated testing modality for pediatric obstructive sleep apnea. Pediatrics. 2000;105:405–412. doi: 10.1542/peds.105.2.405. [DOI] [PubMed] [Google Scholar]
- 12.Zucconi M, Calori G, Castronovo V, et al. Respiratory monitoring by means of an unattended device in children with suspected uncomplicated sleep apnea. Chest. 2003;124:602–607. doi: 10.1378/chest.124.2.602. [DOI] [PubMed] [Google Scholar]
- 13.Moss D, Urschitz MS, Bodman A, et al. Reference values for nocturnal home polysomnography in primary schoolchildren. Pediatric Res. 2005;58:958–965. doi: 10.1203/01.PDR.0000181372.34213.13. [DOI] [PubMed] [Google Scholar]
- 14. SNLG "Sistema Nazionale per le linee guida". Documento 15 Marzo 2008: Appropriatezza e sicurezza degli interventi di Tonsillectomia e di Adenoidectomia.
- 15.Marcus CL. Sleep-disordered breathing in children. Am J Respir Crit Care Med. 2001;164:16–30. doi: 10.1164/ajrccm.164.1.2008171. [DOI] [PubMed] [Google Scholar]
- 16.Cassano P, Gelardi M. Fibroendoscopia dell�ostruzione del cavo rinofaringeo da ipertrofia adenoidea. Medico e Bambino. 2000;4:239–243. [Google Scholar]
- 17.Nixon GM, Kermack AS, McGregor CD, et al. Sleep and breathing on the first night after adenotonsillectomy for obstructive sleep apnea. Pediatr Pulmonol. 2005;39:332–338. doi: 10.1002/ppul.20195. [DOI] [PubMed] [Google Scholar]
- 18.Schechter MS Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome, author Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics;2002:109–e69. doi: 10.1542/peds.109.4.e69. [DOI] [PubMed] [Google Scholar]
- 19.Nixon GM, Kermack AS, Davis GM, et al. Planning adenotonsillectomy in children with obstructive sleep apnea: the role of overnight oximetry. Pediatrics. 2004;113:e19–e25. doi: 10.1542/peds.113.1.e19. [DOI] [PubMed] [Google Scholar]
- 20.Waters KA, McBrien F, Stewart P, et al. Effects of OSA, inhalational anesthesia, and fentanyl on the airway and ventilation of children. J Appl Physiol. 2002;92:1987–1994. doi: 10.1152/japplphysiol.00619.2001. [DOI] [PubMed] [Google Scholar]
- 21.Schwengel DA, Sterni LM, Tunkel DE, et al. Perioperative management of children with obstructive sleep apnea. Anesth Analg. 2009;109:60–75. doi: 10.1213/ane.0b013e3181a19e21. [DOI] [PubMed] [Google Scholar]