Abstract
Background and Objectives
Increasing numbers of women are surviving breast cancer, and survivorship care is becoming more complex. Primary care physicians provide care for most survivors of breast cancer in the Canadian province of British Columbia. The present study offers insight into the confidence of primary care physicians in their abilities to provide such care. It also explores potential ways to assist those providers in enhancing this aspect of their practice.
Methods
A questionnaire was mailed to 1000 primary care physicians caring for survivors of breast cancer. The questionnaire explored the perspectives of the responding physicians on their ability to manage various aspects of survivorship care for breast cancer patients, identified preferences for the content and format of communication from oncologists at the time of transition from active oncology treatment to survivorship, and determined the means most commonly used to obtain knowledge about breast cancer. This 1-page, 31-item checkbox and open-answer questionnaire assessed the perceptions of primary care physicians about the care of breast cancer survivors after completion of active treatment and their personal preferences for resources providing information about breast cancer.
Results
The questionnaire response rate was 59%. Primary care physicians reported being most confident in screening for recurrence and managing patient anxiety; they were least confident in managing lymphedema and providing psychosocial counselling. Compared with physicians following fewer survivors of breast cancer, those who followed more breast cancer survivors had higher confidence in managing the biomedical aspects of follow-up and in providing counselling about nutrition and exercise. Most physicians found discharge letters from oncologists to be useful. Point-form discharge information was preferred by 43%; detailed description, by 19%; and both formats, by 38%. The most useful information items identified for inclusion in a discharge letter were a diagnosis and treatment summary and the recommended surveillance and endocrine therapy. Continuing medical education events and online resources were the means most commonly used to obtain knowledge about breast cancer.
Conclusions
Primary care physicians who provide follow-up for survivors of breast cancer report that they are confident in managing care and satisfied with discharge letters containing a diagnosis and treatment summary, and recommendations for surveillance and endocrine treatment. At the time of patient discharge, additional information about common medical and psychosocial issues in this patient population would be useful to primary care physicians. Preferred means to access current breast cancer information include continuing medical education events and online resources.
Keywords: Breast cancer survivors, primary care physician perspective, follow-up cancer care, survivorship care plans
1. INTRODUCTION
Breast cancer is the most common cancer and the second-highest cause of cancer death in women in Canada. In Canada alone, 23,200 new cases of breast cancer in women are predicted to be diagnosed in 2010, with 5300 deaths1. Survivors of breast cancer constitute the largest population of cancer survivors in North America2, and with increasing improvements in screening, management, and cancer treatment, the number of breast cancer survivors is expected to expand further in coming years3. Not only are survivors increasing in number, but cancer therapies are also expanding in both number and sophistication4, adding complexity to the scope of follow-up practice and placing demands on care providers to remain current in their understanding of breast cancer.
“Survivorship” is defined by the National Coalition of Cancer Survivorship (http://www.canceradvocacy.org/) as the period from diagnosis through the remainder of life, and in the broadest definition, also includes the friends and family of the cancer patient. As more research is done on survivorship, a different definition has emerged to connote a distinct phase from the completion of primary and adjuvant cancer treatment until recurrence or death5. During this time of transition, the focus on issues related to diagnosis and treatment diminishes, shifting toward concerns related to surveillance, management of ongoing side effects, and health promotion. For purposes of the present work, “survivorship” refers to this latter definition.
The concept of survivorship care has received increased attention in the last several years. The report from the U.S. Institute of Medicine on cancer survivorship6 recommends that cancer patients completing treatment should be provided with a comprehensive care plan that is reviewed with the patient during a formal consultation. Nurses, oncology physicians, and primary care physicians recognize the value of such care7; however, there are several barriers to implementation, including lack of research on optimal methods to deliver survivorship care, heterogeneous patient populations and health-care settings, and complex care necessitating multiple providers. Continuity and coordination of care is difficult, with many patients unclear about who is responsible for their ongoing care during the survivorship phase5,8. Limitations in resources present a further challenge, with competing demands on care providers and health care systems.
Despite the barriers, multiple programs have been developed by the U.S. National Coalition of Cancer Survivorship (http://www.canceradvocacy.org/), the American Society of Clinical Oncology9, and The Lance Armstrong Foundation (http://www.livestrong.org), attempting to attend to survivorship care in a more comprehensive fashion by addressing concerns beyond the previous focus of “follow-up care,” which focused mainly on surveillance to detect recurrence and on the management of physical side effects (acute, chronic, and neoplastic). The expected scope of care in the years after completion of treatment has shifted6, placing different demands on care providers. In addition to surveillance to detect recurrence, health care providers manage the effects of cancer and its treatment (physical, psychosocial, and information needs) and ensure that the patient’s general medical and preventive health concerns are met.
Throughout North America, survivors of breast cancer receive care from both oncologists and primary care physicians in diverse practice settings10,11. Some studies involving survivors of breast cancer have shown that, compared with follow-up care from oncologists, follow-up care with a primary care physician results in similar rates of recurrence detection and of health-related quality of life12,13. Other results indicate that breast cancer survivors perceive a high quality of general care from their primary care physicians14 and have higher satisfaction with that care than with the care provided by specialists15. Furthermore, findings suggest that breast cancer survivors have lower confidence in the ability of primary care physicians to deliver cancer-specific care14, that primary care physicians may be inadequately informed about appropriate surveillance10,16 and that those physicians may tend to provide less cancer-specific surveillance than oncologists do17,18. Interestingly, patient preference is largely affected by the practice to which they are accustomed rather than by evidence about which practice is most effective19.
The optimal method of care is not known, but primary care physicians will likely continue to have an increasingly key role in survivorship care, given the increasing number of survivors and the resultant challenge for health resources5. It is thus essential that primary care physicians providing such care have knowledge of current oncology practices and of issues commonly experienced by survivors of breast cancer. Self-evaluation is a method used by physicians to identify potential gaps in their knowledge base or skill set. It is thought that perceived low self-confidence in a domain of their clinical practice would prompt a physician to seek further education and training on that topic, through dialogue with colleagues, literature search, or other means16.
In addition to self-assessment and continued learning, a smooth handover at the time of transition from active cancer treatment to cancer survivorship, with effective communication between oncologists and primary care physicians, is an important measure of effective survivorship care5,20–22. Although communication between oncologists and primary care physicians has been identified as an area requiring improvement10,14, little is known about the preferred content and format of communication. Guidelines on the appropriate follow-up care of breast cancer survivors are available20,23, but whether physicians actually use them is difficult to know.
Breast cancer treatments and concepts about survivorship have evolved considerably in the past few years. For specialists and primary care physicians, the challenges of providing survivorship care are greater than ever. Given the increasing complexities of survivorship care, we conducted the present study to assess the confidence of primary care physicians in their ability to care for survivors of breast cancer, and to explore potential ways to improve their success in providing such care. Secondary objectives were to determine if confidence varied according to the volume of breast cancer survivors in their practice and to ascertain adherence to recommended follow-up guidelines.
2. METHODS
2.1. Study Setting and Population
The BC Cancer Agency (bcca) provides all radiotherapy services and manages the budget for all antineoplastic drugs in the Canadian province of British Columbia. The agency consists of 5 regional cancer centres with a single electronic and paper charting system and a centralized transcription and letter dissemination process. Throughout the course of cancer treatment, patients are seen regularly by their oncologists, and the primary care physician receives correspondence from the oncologist after each clinical encounter. Patients are encouraged to see their primary care physician while on active treatment, but routine visits are not scheduled by the bcca on their behalf.
According to the bcca patient population database, approximately two thirds of breast cancer patients are discharged from the agency within 1 year of completion of chemotherapy or radiation therapy. At the time of discharge from the cancer centre, oncologists typically dictate a letter that sets out the diagnosis, treatment or treatments received, surveillance recommendations, and the recommended type and duration of adjuvant endocrine therapy. Dictations by medical students or residents working with an oncologist are reviewed and edited by the attending oncologist before being signed and distributed.
The population surveyed was primary care physicians who provide follow-up care for patients with nonmetastatic breast cancer. For the period between June 2007 and August 2008 (3–18 months before the first survey mailing), we identified 1023 primary care physicians to whose care at least 1 woman with nonmetastatic breast cancer was discharged from the bcca.
2.2. Questionnaire
An English-language self-administered survey was mailed to a physician sample. The questionnaire was developed by 2 oncologists (SLS, ESW) and was designed to obtain the perspectives of the primary care physicians on their ability to manage various aspects of survivorship care for breast cancer patients, and to identify potential ways to assist them in enhancing this aspect of their practice. Before distribution, the survey was tested with 4 primary care physicians for face validity, content, relevance, and time required for completion; it was then revised accordingly.
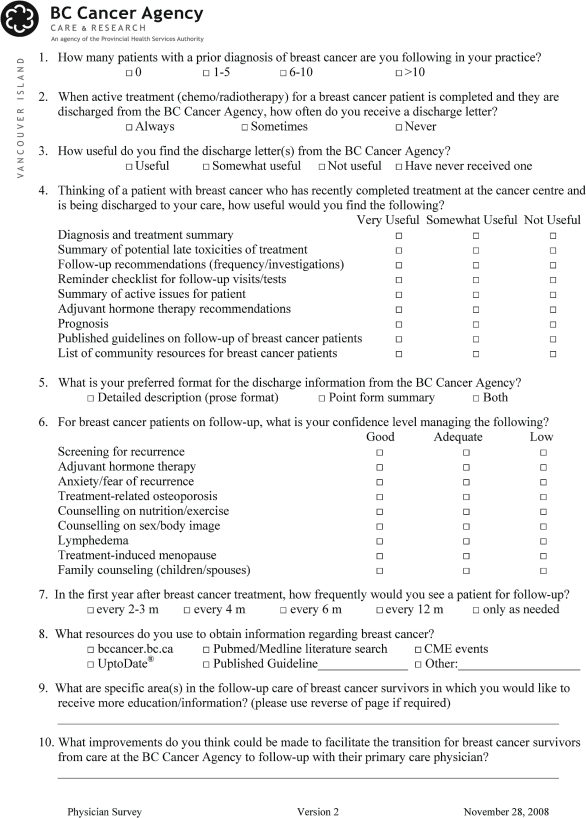
To facilitate a high response rate, the final version of the questionnaire (Figure 1) was intentionally condensed to 1 page and was designed for completion within 2–3 minutes. Respondents were encouraged to use the reverse side of the page if further space was required for additional comments.
FIGURE 1.
Questionnaire exploring the perspectives of primary care physicians on their ability to manage various aspects of survivorship care for patients with nonmetastatic breast cancer.
2.3. Survey Methods
From the identified list of primary care physicians, 1000 were randomly selected using a modified Dillman methodology for survey administration24. Two mailings were done. The first mailing in December 2008 included a cover letter, the questionnaire, and a postage-paid return envelope. Physicians were asked to respond anonymously by fax or mail. A second mailing in January 2009, with a modified cover letter instructing participants not to complete the survey twice, again contained the questionnaire and a postage-paid return envelope.
All respondents were anonymous. The study, including the questionnaire and cover letters, was approved by the University of British Columbia Ethics Board.
2.4. Statistical Analysis
The analysis included descriptive statistics focusing on frequencies. Frequencies were calculated based on the total number of responses for each question, because not all respondents completed every question. The Pearson chi-square test was used to assess whether responses varied depending on the selfreported number of breast cancer survivors followed in the physician’s practice. The Fisher exact test was used when responses were unevenly distributed.
3. RESULTS
3.1. Respondent Characteristics
Of the 1000 surveys distributed, 590 were returned, 351 after the first mailing, and an additional 239 after the second mailing. Two surveys were deemed ineligible because the physician was no longer in practice, and one was returned as undeliverable. The survey completion rate was thus 59% (587/997).
All respondents indicated that their current practice included at least 1 breast cancer survivor, with 61% (353/581) indicating that they had more than 10 survivors in their practice; 28% (164/581), 6–10 survivors; and 11% (64/581), 1–5 survivors. Because responses were anonymous, additional demographic information on respondents was not available.
3.2. Confidence Managing Survivors of Breast Cancer
Table i summarizes the self-rated confidence of primary care physicians in managing survivors of breast cancer, reported as a frequency responding to good, adequate, and low. Respondents were most confident managing surveillance for recurrence. Confidence in this domain improved as the number of breast cancer survivors in the physician’s practice increased [χ2(2, N = 577) = 9.665, p = 0.008]. Areas with the highest frequency of responses indicating low confidence included providing family counselling (22.3%), managing lymphedema (23.6%), and counselling on sex and body image (24.2%). Responses were independent of the number of patients followed.
TABLE I.
Perceived confidence among primary care physicians about managing survivorship care for breast cancer patients
| Topic | Respondents (n) |
Frequency |
|||||
|---|---|---|---|---|---|---|---|
|
Good or adequate |
|||||||
| Good | Adequate | Low | Overall | Follow ≤10 survivors | Follow >10 survivors | ||
| Screening for recurrence | 577 | 0.77 | 0.22 | 0.01 | 0.99 | 0.96 | 1.00 |
| Anxiety or fear of recurrence | 574 | 0.54 | 0.43 | 0.03 | 0.97 | 0.97 | 0.97 |
| Treatment-related osteoporosis | 576 | 0.49 | 0.43 | 0.08 | 0.92 | 0.91 | 0.94 |
| Counselling on nutrition and exercise | 576 | 0.45 | 0.44 | 0.11 | 0.89 | 0.87 | 0.90 |
| Treatment-induced menopause | 577 | 0.37 | 0.51 | 0.12 | 0.88 | 0.81 | 0.92 |
| Adjuvant hormone therapy | 578 | 0.30 | 0.55 | 0.15 | 0.85 | 0.80 | 0.88 |
| Family counselling (children or spouse) | 575 | 0.25 | 0.51 | 0.24 | 0.76 | 0.74 | 0.78 |
| Lymphedema | 576 | 0.21 | 0.55 | 0.24 | 0.76 | 0.73 | 0.79 |
| Counselling on sex and body image | 577 | 0.30 | 0.44 | 0.26 | 0.74 | 0.70 | 0.76 |
Primary care physicians with more than 10 survivors of breast cancer in their practice were more confident that those with fewer than 10 survivors with regard to managing adjuvant hormone therapy [χ2(2, N = 578) = 11.321, p = 0.003], managing treatment-related osteoporosis [χ2(2, N = 576) = 13.673, p = 0.001], managing treatment-induced menopause [χ2(2, N = 577) = 20.685, p < 0.0005], and counselling on nutrition and exercise [χ2(2, N = 576) = 16.429, p < 0.0005, Table i].
3.3. Potential Means to Assist Primary Care Physicians in Providing Care for Breast Cancer Survivors
Among respondents, 80% (463/581) indicated that they “always” receive a discharge letter from the bcca; 19% (110/581), that they “sometimes” receive such a letter; and only 1% (8/581), that they “never” receive such a letter. Of those who answered the question pertaining to the utility of discharge letters, 92% (528/575) found them “useful” and 8% (47/575), “somewhat useful.” The preferred format for written discharge information was point form (43%) or a combination of point form and detailed description (38%). Detailed description alone was preferred by 19%. Compared with primary care physicians having fewer than 10 breast cancer survivors in their practice, those with more than 10 survivors were more likely to prefer point form alone (49% vs. 38%, p = 0.032).
3.4. Preferences of Primary Care Physicians for Communication from Oncologists
Table ii illustrates the content preferred by primary care physicians for communications at the time of discharge from the cancer centre. The most common “very useful” elements were a summary of diagnosis and treatment, the recommended follow-up protocol, and the recommended adjuvant hormonal therapy. Published guidelines on breast cancer follow-up and a list of community resources were the items with the least utility, although more than half the primary care physicians still indicated that those items would be “very useful.” The number of breast cancer survivors followed did not influence the preferences of primary care physicians for the type of information to be communicated at the time of discharge, except for the diagnosis, the treatment summary, and the adjuvant hormone information. The response rate by primary care physicians who followed more than 10 survivors was 91% compared with 95.1% for physicians who followed fewer than 10 survivors (Fisher exact test, p = 0.015). Similarly, 93.7% of physicians following more than 10 survivors described adjuvant hormone information as “very useful,” with 89.3% of those following fewer than 10 survivors answering the same way (Fisher exact test, p = 0.043).
TABLE II.
Perception among primary care physicians of the utility of discharge communication information
| Topic | Respondents (n) | Frequency (n responses) | ||
|---|---|---|---|---|
| Very useful | Somewhat useful | Not useful | ||
| Diagnosis and treatment summary | 582 | 0.97 (568) | 0.03 (16) | 0.00 (0) |
| Recommended follow-up | 582 | 0.96 (559) | 0.04 (24) | 0.00 (1) |
| Recommended adjuvant hormone therapy | 579 | 0.92 (534) | 0.08 (47) | 0.00 (0) |
| Summary of active issues | 581 | 0.85 (495) | 0.13 (76) | 0.02 (12) |
| Reminder checklist for follow-up | 576 | 0.85 (493) | 0.12 (71) | 0.02 (14) |
| Summary of potential late toxicities | 581 | 0.84 (489) | 0.14 (84) | 0.02 (10) |
| Prognosis | 581 | 0.84 (489) | 0.15 (85) | 0.02 (9) |
| Guidelines on breast cancer follow-up | 577 | 0.61 (355) | 0.34 (194) | 0.05 (30) |
| List of community breast cancer resources | 576 | 0.56 (322) | 0.38 (220) | 0.06 (36) |
3.5. Resources used by Primary Care Physicians to Obtain Knowledge About Breast Cancer
Table iii summarizes the resources most commonly used to obtain educational information on breast cancer, which include continuing medical education events, the bcca Web site (http://www.bccancer.bc.ca), and the UptoDate Web site (http://www.uptodate.com: UptoDate Inc., Waltham, MA, U.S.A.). UptoDate is an evidence-based, peer-reviewed medical information resource available electronically on the Web and mobile devices.
TABLE III.
Resources used by primary care physicians to obtain information about breast cancer
| Resource | Frequency (n responses) |
|---|---|
| Continuing medical education events | 0.607 (355) |
| Provincial cancer centre Web site | 0.446 (261) |
| UptoDate.coma | 0.318 (186) |
| Published guideline | 0.198 (116) |
| Literature search or academic journals | 0.132 (77) |
UptoDate Inc., Waltham, MA, U.S.A.
The most common responses to the open-ended question concerning areas in which primary care physicians would like more information were adjuvant endocrine treatment and a surveillance reminder checklist. Updates on new research findings and information on late effects were also mentioned. When asked for suggestions to improve the transition of care, the most common response was a request for “complete information.” Others requested the development of electronic follow-up templates that would integrate with electronic medical records to help guide follow-up practice.
3.6. Adherence to Practice Guidelines
About half the primary care physicians (51%) reported that they see patients every 2–3 months in the first year after breast cancer treatment. Most respondents (97%, 556/576) indicated that they saw patients at least every 6 months, as recommended by Canadian published guidelines20. Adherence to recommended follow-up frequency was not influenced by the number of patients followed.
4. DISCUSSION
Previous randomized trials have demonstrated that, compared with follow-up by oncologists, follow-up of breast cancer survivors by primary care physicians results in better patient satisfaction15, improved surveillance for non-cancer health issues18, and equivalent rates of detection of recurrence12,13. However, the training of specific primary care physicians in post-treatment care of cancer patients is limited25, and patients have lower confidence in the ability of their primary care physicians to care for them after a cancer diagnosis14,26. Centres across North America have varying follow-up practices (that is, oncologist only, combined oncologist and primary care physician, primary care physician only), but primary care physicians are recognized to play an integral role in patient care, whether for post-treatment care, psychosocial support, or management of other medical issues27. Since those earlier-mentioned follow-up studies were completed, the scope of care thought to be required for cancer survivors has changed5,6,9,12, from a focus primarily on surveillance for detecting recurrence to a more comprehensive approach that addresses medical, psychological, and social factors. The degree to which primary care physicians are equipped to manage various aspects of survivorship care for breast cancer patients is largely unknown.
We have shown that primary care physicians report confidence in their ability to provide care for survivors of breast cancer and that they appear to adhere to guideline-recommended20 follow-up frequency. The degree of a physician’s self-confidence in ability to manage biomedical aspects of care such as endocrine therapy, osteoporosis, menopause, and the provision of information on nutrition and exercise appears to improve as the number of breast cancer survivors followed increases. That finding suggests a learning curve in those domains. The learning curve may be a result of breast cancer survivors bringing those issues to the attention of their primary care physicians more frequently because primary care physicians perceive those issues as part of their scope of practice (and thus ensure that they obtain information about them) or because those topics are more commonly included in continuing medical education events. By contrast, aspects of care showing low confidence despite the number of breast cancer survivors followed (lymphedema, counselling about sex and body image, family counselling) may have a sufficiently low incidence that primary care physicians rarely encounter them, may be perceived as being outside of the physician’s scope of practice, or may be underrepresented in continuing medical education. For example, lymphedema is less common with increased use of sentinel lymph node dissection, and it is managed primarily with massage and physiotherapy. Most primary care physicians have insufficient resources (training, time, and reimbursement) to provide counselling. Our observations in this area reinforce the need for a multidisciplinary approach to survivorship care, which likely needs the coordinated efforts of primary care physicians, specialists, nutritionists, exercise physiologists, counselors, and so on.
Most respondents rated their confidence in managing adjuvant hormones as good or adequate, even though aromatase inhibitors were introduced into practice only 3 years before our survey, with several studies having been published in a short period28–33. Oncologists in British Columbia typically initiate adjuvant hormonal therapy and outline the potential toxicities in the discharge communication. That practice may have helped to facilitate uptake of relevant information. Our survey questionnaire did not explicitly inquire about self-confidence in managing patients on tamoxifen versus patients on aromatase inhibitors, and so the confidence of the primary care physicians may have been overestimated in that area.
Although communication between oncologists and primary care physicians has been identified as a weakness10,14, primary care physicians in the current study appear to be satisfied with discharge communication from oncologists. This discrepancy might be attributable to differences in practice settings. The study by Nissen et al.10 was conducted in an integrated nonprofit urban health care system, in which primary care physicians had variable involvement in the care of survivors and did not provide exclusive follow-up in the first 2 years after treatment completion. By contrast, the present study was conducted in a centralized cancer care system that has for many years discharged patients to the community early after completion of active treatment, with semi-standardized discharge communication developed by oncologists who treat patients with breast cancer. This approach is recommended, given the high satisfaction rates in the present study.
The content of discharge information most consistently identified as “very useful” in our study included the summary of diagnosis and treatment, the recommended follow-up surveillance, and the recommended adjuvant hormone therapy. That finding is consistent with the literature11, and those information items are typically included in discharge communication. Although that result is encouraging, several other components thought to be useful to primary care physicians are currently not provided in the discharge communication from our centres, including a follow-up checklist, prognostic information, and information on late effects of treatment. That finding validates the Institute of Medicine consensus recommendations on a comprehensive discharge summary6. Providing those details may assist primary care physicians in providing more comprehensive care; however, the actual utility would need to be confirmed in subsequent studies.
The format of discharge communication requires further consideration. Letters from oncologists to primary care physicians often include lengthy descriptions that lack key information and contain unnecessary details21. Studies have shown that standardized discharge letters are preferred by primary care physicians as having more relevant, more accessible information21,34,35. Not surprisingly, most primary care physicians in our survey indicated a preference for point-form communication, either alone or in combination with detailed descriptions. We believe that this result speaks to the high clinical demands on primary care physicians, driving their need for concise, relevant information that can be quickly reviewed.
Knowing that continuing medical education workshops and online resources are the resources most frequently used by primary care physicians to obtain information on breast cancer can help to guide continuing education strategies. Many survey respondents indicated that electronic or written bulletins would be useful, which may again reflect a desire for quick, easily accessed information. Some requested electronic templates to assist them in the provision of follow-up care, similar to templates developed in the management of other chronic diseases such as hypertension and diabetes. The development of such clinical tools should be further explored.
Limitations of this study include a lack of information regarding respondent characteristics. The self-ratings of confidence in the ability to provide care may not in fact represent actual ability to provide such care. We acknowledge that care of cancer survivors is provided in diverse clinical settings, and that the findings from the present study may not be applicable to other settings. That said, for centres considering a shift from follow-up by oncologists to follow-up by primary care physicians, the results are encouraging. It is also acknowledged that the assessment of adherence to guidelines in our survey was simplified to one question and the responses may therefore not accurately reflect adherence to guidelines overall.
5. CONCLUSIONS
Increasing numbers of breast cancer survivors and the increasing complexity of care needed by this population place large demands on health care providers. Primary care physicians accustomed to providing care for survivors of breast cancer self-report confidence in managing most aspects of care. Lower confidence in some domains suggests that a multidisciplinary approach to survivorship care is needed. We recommend that primary care physicians be provided with discharge communication from oncologists that at minimum contains a summary of diagnosis and treatment, recommended surveillance, and recommended endocrine therapy. The provision of additional information on active patient issues and late effects of treatment, with a follow-up reminder checklist including follow-up guidelines and a point-form template for communication are considerations for further improvements in communication from oncologists to primary care physicians.
6. ACKNOWLEDGMENTS
The authors thank the contributing primary care physicians for their time and comments.
Footnotes
7. CONFLICT OF INTEREST DISCLOSURES
This work was supported by the Canadian Breast Cancer Foundation and by the BC Cancer Foundation. The authors have no conflicts of interest to declare.
8. REFERENCES
- 1.Canadian Cancer Society . Toronto, ON: Canadian Cancer Society; 2010. Home > Canada Wide > About Cancer > Cancer Statistics > Statistics at a Glance > Breast Cancer Statistics [Web resource] [Available online at: http://www.cancer.ca/Canada-wide/About%20cancer/Cancer%20statistics/Stats%20at%20a%20glance/Breast%20cancer.aspx?sc_lang=en; cited August 19, 2010] [Google Scholar]
- 2.Burstein HJ, Winer EP. Primary care for survivors of breast cancer. N Engl J Med. 2000;343:1086–94. doi: 10.1056/NEJM200010123431506. [DOI] [PubMed] [Google Scholar]
- 3.Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–30. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 4.The Systemic Therapy Task Force . Systemic Therapy Task Force Report. Toronto, ON: Cancer Care Ontario; 2000. [Google Scholar]
- 5.Grunfeld E, Earle CC. The interface between primary and oncology specialty care: treatment through survivorship. J Natl Cancer Inst Monogr. 2010;2010:25–30. doi: 10.1093/jncimonographs/lgq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 7.Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–3. doi: 10.1200/JCO.2006.10.0826. [DOI] [PubMed] [Google Scholar]
- 8.Cheung WY, Neville BA, Cameron DB, Cook EF, Earle CC. Comparisons of patient and physician expectations for cancer survivorship care. J Clin Oncol. 2009;27:2489–95. doi: 10.1200/JCO.2008.20.3232. [DOI] [PubMed] [Google Scholar]
- 9.American Society of Clinical Oncology (asco) Alexandria, VA: ASCO; ASCO Cancer Treatment Summaries [Web page] n.d. [Available online at: http://www.cancer.net/patient/Survivorship/ASCO+Cancer+Treatment+Summaries; cited January 2011] [Google Scholar]
- 10.Nissen MJ, Beran MS, Lee MW, Mehta SR, Pine DA, Swenson KK. Views of primary care providers on follow-up care of cancer patients. Fam Med. 2007;39:477–82. [PubMed] [Google Scholar]
- 11.Del Giudice ME, Grunfeld E, Harvey BJ, Piliotis E, Verma S. Primary care physicians’ views of routine follow-up care of cancer survivors. J Clin Oncol. 2009;27:3338–45. doi: 10.1200/JCO.2008.20.4883. [DOI] [PubMed] [Google Scholar]
- 12.Grunfeld E, Mant D, Yudkin P, et al. Routine follow-up of breast cancer in primary care: a randomized trial. BMJ. 1996;313:665–9. doi: 10.1136/bmj.313.7058.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grunfeld E, Levine MN, Julian JA, et al. A randomized trial of long term follow-up for early stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol. 2006;24:848–55. doi: 10.1200/JCO.2005.03.2235. [DOI] [PubMed] [Google Scholar]
- 14.Mao JJ, Bowman MA, Stricker CT, et al. Delivery of survivorship care by primary care physicians: the perspective of breast cancer patients. J Clin Oncol. 2009;27:933–8. doi: 10.1200/JCO.2008.18.0679. [DOI] [PubMed] [Google Scholar]
- 15.Grunfeld E, Fitzpatrick R, Mant D, et al. Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: results from a randomized controlled trial. Br J Gen Pract. 1999;49:705–10. [PMC free article] [PubMed] [Google Scholar]
- 16.Wood ML. Communication between cancer specialists and family doctors. Can Fam Physician. 1993;39:49–57. [PMC free article] [PubMed] [Google Scholar]
- 17.Earle CC, Neville BA. Under use of necessary care among cancer survivors. Cancer. 2004;101:1712–19. doi: 10.1002/cncr.20560. [DOI] [PubMed] [Google Scholar]
- 18.Earle CC, Burstein HJ, Winer EP, Weeks JC. Quality of nonbreast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21:1447–51. doi: 10.1200/JCO.2003.03.060. [DOI] [PubMed] [Google Scholar]
- 19.de Bock GH, Bonnema J, Zwaan RE, van de Velde CJ, Kievit J, Stiggelbout AM. Patient’s needs and preferences in routine follow-up after treatment for breast cancer. Br J Cancer. 2004;90:1144–50. doi: 10.1038/sj.bjc.6601655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grunfeld E, Dhesy–Thind S, Levine M, on behalf of the Steering Committee on Clinical Practice Guidelines for the Care and Treatment of Breast Cancer Clinical practice guidelines for the care and treatment of breast cancer: follow-up after treatment for breast cancer (summary of the 2005 update) CMAJ. 2005;172:1319–20. doi: 10.1503/cmaj.045062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnes EA, Hanson J, Neumann CM, Nekolaichuk CL, Bruera E. Communication between primary care physicians and radiation oncologists regarding patients with cancer treated with palliative radiotherapy. J Clin Oncol. 2000;18:2902–7. doi: 10.1200/JCO.2000.18.15.2902. [DOI] [PubMed] [Google Scholar]
- 22.Dworkind M, Towers A, Murnaghan D, Guibert R, Iverson D. Communication between family physicians and oncologists: qualitative results of an exploratory study. Cancer Prev Control. 1999;3:137–44. [PubMed] [Google Scholar]
- 23.Khatcheressian JL, Wolff AC, Smith TJ, et al. on behalf of American Society of Clinical Oncology American Society of Clinical Oncology 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting. J Clin Oncol. 2006;24:5091–7. doi: 10.1200/JCO.2006.08.8575. [DOI] [PubMed] [Google Scholar]
- 24.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. New York, NY: Wiley; 2000. [Google Scholar]
- 25.Ferrell BR, Winn R. Medical and nursing education and training opportunities to improve survivorship care. J Clin Oncol. 2006;24:5142–8. doi: 10.1200/JCO.2006.06.0970. [DOI] [PubMed] [Google Scholar]
- 26.Sussman J, Baldwin LM. The interface of primary and oncology specialty care: from diagnosis through primary treatment. J Natl Cancer Inst Monogr. 2010;2010:18–24. doi: 10.1093/jncimonographs/lgq007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr. 2010;2010:72–80. doi: 10.1093/jncimonographs/lgq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med. 2003;349:1793–802. doi: 10.1056/NEJMoa032312. [DOI] [PubMed] [Google Scholar]
- 29.Howell A, Cuzick J, Baum M, et al. Results of the atac (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–2. doi: 10.1016/S0140-6736(05)74803-0. [DOI] [PubMed] [Google Scholar]
- 30.Thürlimann B, Keshaviah A, Coates AS, et al. on behalf of the Breast International Group (big) 1–98 Collaborative Group A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353:2747–57. doi: 10.1056/NEJMoa052258. [DOI] [PubMed] [Google Scholar]
- 31.Coates AS, Keshaviah A, Thürlimann B, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study big 1–98. J Clin Oncol. 2007;25:486–92. doi: 10.1200/JCO.2006.08.8617. [DOI] [PubMed] [Google Scholar]
- 32.Coombes RC, Kilburn LS, Snowdon CF, et al. Survival and safety of exemestane versus tamoxifen after 2–3 years’ tamoxifen treatment (Intergroup Exemestane Study): a randomized controlled trial. Lancet. 2007;369:559–70. doi: 10.1016/S0140-6736(07)60200-1. [DOI] [PubMed] [Google Scholar]
- 33.Forbes JF, Cuzick J, Buzdar A, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the atac trial. Lancet Oncol. 2008;9:45–53. doi: 10.1016/S1470-2045(07)70385-6. [DOI] [PubMed] [Google Scholar]
- 34.van Walraven C, Duke SM, Weinberg AL, Wells PS. Standardized or narrative discharge summaries. Which do family physicians prefer? Can Fam Physician. 1998;44:62–9. [PMC free article] [PubMed] [Google Scholar]
- 35.Braun TC, Hagen NA, Smith C, Summers N. Oncologists and family physicians. Using a standardized letter to improve communication. Can Fam Physician. 2003;49:882–6. [PMC free article] [PubMed] [Google Scholar]