Abstract
Background:
Contemporary screening for prostate cancer frequently identifies small volume, low-grade lesions. Some clinicians have advocated focal prostatic ablation as an alternative to more aggressive interventions to manage these lesions. To identify which patients might benefit from focal ablative techniques, we analysed the surgical specimens of a large sample of population-detected men undergoing radical prostatectomy as part of a randomised clinical trial.
Methods:
Surgical specimens from 525 men who underwent prostatectomy within the ProtecT study were analysed to determine tumour volume, location and grade. These findings were compared with information available in the biopsy specimen to examine whether focal therapy could be provided appropriately.
Results:
Solitary cancers were found in prostatectomy specimens from 19% (100 out of 525) of men. In addition, 73 out of 425 (17%) men had multiple cancers with a solitary significant tumour focus. Thus, 173 out of 525 (33%) men had tumours potentially suitable for focal therapy. The majority of these were small, well-differentiated lesions that appeared to be pathologically insignificant (38–66%). Criteria used to select patients for focal prostatic ablation underestimated the cancer's significance in 26% (34 out of 130) of men and resulted in overtreatment in more than half. Only 18% (24 out of 130) of men presumed eligible for focal therapy, actually had significant solitary lesions.
Conclusion:
Focal therapy appears inappropriate for the majority of men presenting with prostate-specific antigen-detected localised prostate cancer. Unifocal prostate cancers suitable for focal ablation are difficult to identify pre-operatively using biopsy alone. Most lesions meeting criteria for focal ablation were either more aggressive than expected or posed little threat of progression.
Keywords: prostate cancer, unifocal, regional ablation, prostatectomy
As a consequence of repeated testing for prostate-specific antigen (PSA), prostate cancer is now the most common male malignancy in North America and Europe (Jemal et al, 2010). Of the 217 730 men diagnosed with this disease in the United States, approximately half were classified as low-risk disease (Stamey et al, 2004; Cooperberg et al, 2007). Recent data from the European Randomized Screening for Prostate Cancer Trial suggest that many of these cases pose little threat of disease progression and that only 1 of every 37–48 men diagnosed by PSA testing may benefit from aggressive treatment (Roobol et al, 2009). Although this number-needed-to-treat may reduce as the length of follow-up increases within this trial, it is likely that overtreatment will still be prevalent for screen-detected cancers.
The concern surrounding the potential for overtreatment of localised prostate cancer has led many clinicians to propose alternative treatment strategies. Some clinicians have advocated active surveillance, but many patients are hesitant to accept this approach because of the fear of disease progression (Denberg et al, 2006). Focal prostate ablation has recently emerged as a less invasive alternative to radical prostatectomy and a more acceptable approach than active surveillance (Sartor et al, 2008).
The objective of focal ablative intervention is to destroy cancerous prostate tissue without targeting the entire gland. High-intensity frequency ultrasound (HIFU), photothermal and cryotherapy are promising techniques that offer the potential of lower morbidity when compared with radical surgery, external beam radiation or brachytherapy. Unfortunately few centres have reported long-term outcomes to validate this approach and there are no reported controlled trials that confirm the efficacy of these treatments (Onik et al, 2008; Challacombe et al, 2009; Lindner et al, 2009; Warmuth et al, 2010).
One major concern surrounding the efficacy of focal therapy stems from the observation that many prostate cancers are not solitary. Depending upon the patient population selected, how the tissue was processed and which definitions are used, as many as 50–87% of prostate cancers have multiple sites within the gland (Meiers et al, 2007). Many of these lesions cannot be detected pre-operatively by biopsy or imaging.
The present study is based on a cohort of men with screen-detected prostate cancer, who then underwent radical prostatectomy as part of a randomised controlled trial (Donovan et al, 2003). Our aims were, first, to estimate the proportion of men with screen-detected prostate cancer for whom focal therapy would be appropriate. Second, to establish whether measures taken during the diagnostic process could be used to identify those men for whom focal therapy would be a suitable treatment of their prostate cancer. Third, to detail the pathological characteristics of tumours suitable for focal ablation.
Patients and methods
Patient population
Data used in this analysis were prospectively collected from 525 men who underwent radical prostatectomy within the ProtecT trial (NCT00632983; HTA 96/20/06; HTA 96/20/99) (inclusion criteria described in: Donovan et al, 2003; Lane et al, 2010), a large randomised trial testing the efficacy of prostate cancer treatment in men detected through population-based PSA testing. Men recruited into ProtecT study were identified from community medical practices and aged 50–69 years at initial invitation with no prostatic symptoms. Men included in this study were those randomised to or choosing surgery after having been diagnosed with prostate cancer following a 10 core trans-rectal biopsy performed because of a single-serum PSA value between 3 and 19.9 ng ml−1, in whom complete pathological records were available at the time of this analysis. Men included in the ProtecT trial were used, as opposed to those from a tertiary center case series, to avoid biasing the sample towards high-risk tumours. The study population is described in Table 1.
Table 1. Radical prostatectomy features of unifocal and multifocal tumours.
|
Unifocal significant tumours
|
Multifocal tumours
|
|||||
|---|---|---|---|---|---|---|
| n | % | n | % | P-valuea | Multivariable P-valueb | |
| Total | 173 | 352 | ||||
| Age (years, mean (s.d.)) | 61.4 (5.0) | 60.7 (4.9) | 0.9 | |||
| Differentiation | ||||||
| Gleason 5 or 6 | 132 | 78.6 | 121 | 35.2 | ||
| Gleason 3+4=7 | 28 | 16.7 | 174 | 50.6 | ||
| Gleason 4+3=7 | 4 | 2.4 | 38 | 11.0 | ||
| Gleason 8–10 | 4 | 2.4 | 11 | 3.2 | ||
| Missing | 5 | 2.8 | 8 | 2.3 | <0.001 | 0.3 |
| Stage | ||||||
| pT2 | 149 | 86.4 | 212 | 60.3 | ||
| pT3 | 24 | 13.6 | 140 | 39.7 | <0.001 | 0.2 |
| Insignificant cancer c | ||||||
| Insignificant (Epstein) | 69 | 39.9 | 2 | 0.6 | <0.001 | <0.001 |
| Insignificant (Liberal) | 118 | 68.2 | 39 | 11.1 | <0.001 | <0.001 |
| Other pathological features | ||||||
| Vascular invasion | 0 | 0.0 | 15 | 4.3 | 0.001 | 0.1 |
| HGPIN | 150 | 87.7 | 331 | 94.3 | 0.09 | 0.3 |
| Seminal Vesicle invasion | 1 | 0.6 | 29 | 8.3 | <0.001 | 0.3 |
| Tumour volume (ml, mean (s.d.)) | ||||||
| Total | 1.18 (1.7) | 4.33 (9.7) | <0.001 | <0.001 | ||
| Dominant | 1.05 (1.7) | 3.64 (7.8) | <0.001 | 0.001 | ||
| Secondary | 0.16 (0.4) | 0.77 (3.7) | 0.08 | 0.4 | ||
| Tertiary | 0.05 (0.1) | 0.15 (0.3) | 0.02 | 0.8 | ||
| Nomogram score (mean (s.d.)) d | ||||||
| Risk of indolent cancer | 0.75 (0.2) | 0.58 (0.3) | <0.001 | 0.9 | ||
Abbreviations: HGPIN=high-grade prostatic intraepithelial neoplasia; s.d.=standard deviation.
χ2-test for all variables except tumour volume, and age (t-test).
Backward elimination logistic regression using parameters with univariable significance.
Histological definition from the prostatectomy specimen: Epstein's: < 0.5 ml tumour volume, Gleason score < 6, organ confined; liberal: pT2, Gleason score <6, organ confined, no adverse features.
Score calculated using Kattan–Steyerberg nomogram (Steyerberg et al, 2007).
Pathological analysis
Pathologic assessment of needle biopsy prostate cores and radical prostatectomy specimens was made by specialist urological pathologists using standardized protocols and agreed reporting pro-formas. Prostate biopsy specimens were classified as predicting insignificant disease if they met Epstein's criteria (PSA density <0.15 ng ml−1, Gleason score ⩽6, two cores or less with cancer and no core containing more than 50% cancer) (Epstein et al, 1994) and predicting low risk if they met the following criteria; PSA ⩽20 ng ml−1, Gleason score ⩽6, ⩽50% positive cores, ⩽20 mm cancer and at least 40 mm benign tissue (Kattan et al, 2003; Steyerberg et al, 2007). For each tumour, we calculated the pre-operative risk of indolent disease using the Kattan–Steyerberg Nomogram (Steyerberg et al, 2007) and identified tumours that satisfied the proposed consensus criteria predicting tumour unifocality (i.e., PSA ⩽10 ng ml−1 or PSAD⩽0.15 ng ml−1 g−1, Gleason sum score ⩽6, cumulative cancer volume ⩽10 mm, ⩽7 mm of cancer within one core and ⩽33% of needle cores with cancer) (Sartor et al, 2008).
Radical prostatectomy specimens were completely embedded, mapped and the tumour apportioned between five regions: anterior to the urethra, posterior left, posterior right, posterior apical and posterior base. Tumours located entirely or mostly (no more than 20% of volume in an adjacent region) within one prostate region were defined as solitary tumours. Tumour volume was calculated using a three-dimensional method (Chen et al, 2003). Multiple tumours were identified as those with discrete malignancies separated by one low-power field diameter. The tumour with the most advanced stage, highest grade or highest volume was defined as the dominant tumour. Insignificant tumours in the prostatectomy specimens were classified according to the Epstein's criteria (⩽0.5 ml tumour volume, Gleason score ⩽6, organ confined) (Epstein et al, 2005) and more liberal criteria (any volume, pT2, Gleason score ⩽6, organ confined, no adverse features (e.g., vascular invasion)) (Sengupta et al, 2008; Lee et al, 2009). Solitary single cancers and multifocal tumours with a dominant solitary focus and insignificant secondary foci were defined as those suitable for focal therapy.
Statistical analysis
Measures made before surgery were evaluated for their ability to identify those suitable for focal therapy using univariable logistic regression, a multivariable model determined by backward selection and Harrell's concordance index (Harrell et al, 1982; Catto et al, 2009). For regression, we analysed age of the patient, serum PSA, prostate volume, PSA density, Gleason grade, digital rectal examination findings and measures of tumour extent in the biopsy core. Independence between variables was determined before inclusion (r<0.5) and separate models used for collinear variables. The predictive power of the final multivariable models was evaluated using sensitivity, specificity, positive predictive value, and the area under the receiver operating characteristic curve. All tests were two-tailed, performed within SPSS statistical software (Version 18.0, 2010, SPSS Inc., Chicago, IL, USA) and significance was defined as a P-value <0.05.
Results
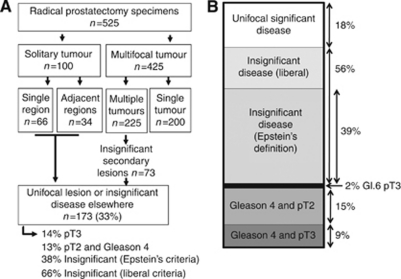
We report data from 525 men within the ProtecT trial who underwent radical prostatectomy with curative intent. At diagnosis, the average patient age was 61 years (s.d. 5), the average serum PSA was 6.1 ng ml−1 (s.d. 3.6) and the average prostate size was 34.4 ml (TRUS volume, s.d. 15.2). Of the 525 men, 512 (97.5%) harboured Gleason score 6 or 7 disease, 496 (94.5%) had 10 or more biopsy cores assessed and 423 (80.6%) were diagnosed following the first biopsy. Solitary prostate cancers were identified in the prostatectomy specimens of 100 (19%) men (Table 1, Figure 1A). Of these, tumour was located in a single region in 66 and in two adjacent regions in 34 men. The remaining 425 men had multifocal lesions consisting of either a diffuse dominant tumour (200 men, 47%) or multiple cancers (225 men, 53%). In these men, the secondary lesions were insignificant in 33% (73 out of 225) and hence may be suitable for focal treatment (Eggener et al, 2007). Thus, 33% of men (173 out of 525) had tumours suitable for focal ablation (i.e., unifocal significant tumours).
Figure 1.
Tumour focality in prostate cancer. (A) Flowchart of tumour focality within the samples described within this report. (B) The pathological details of tumours fulfilling the criteria for focal therapy. The thick black line represents the 2% of tumours that are pT3 and Gleason 3+3=6.
Men with unifocal significant tumours had a lower Gleason score (χ2-test, P<0.001), lower stage (P<0.001), fewer cores positive at biopsy (mean=11% of cores had cancer (95% CI: 6–16%)) vs 33% for multifocal tumours (28–38%), ANOVA P<0.001), less disease within these cores (mean cumulative length of unifocal cancer=6 mm (95% CI: 3–10 mm) vs 20 mm for multifocal disease (16–25 mm, ANOVA P<0.001)) and less vascular invasion in the prostatectomy specimen than those with multifocal disease (χ2-test, P=0.06) (Table 1). Of note, multifocal tumours were found more easily than unifocal ones (84% detected at first biopsy vs 73% for unifocal cancers, χ2-test, P=0.007). Multivariable analysis revealed that tumour unifocality was most associated with pathologically defined insignificant disease and tumour volume (P<0.0001). Focal ablation is not recommended for tumours with poorly differentiated components or with capsular invasion (Sartor et al, 2008). In total, 118 out of 173 (68%) of unifocal cancers were Gleason score ⩽6 and pT2. Of these, 69 out of 118 (58%) and 118 out of 118 (100%) were pathologically insignificant according to Epstein's and the liberal definitions, respectively. Therefore, between 56 out of 123 (47%) and 9 out of 123 (7%) of unifocal tumours were Gleason 6, pT2 and pathologically significant, depending upon the definition of pathological insignificance.
Several pre-operative measures were associated with the presence of a unifocal cancer (Table 2). Owing to covariate correlation (r>0.5), biopsy features describing tumour extent (bilateral disease, total and maximal tumour length and percentage of cores with cancer) and insignificant cancer definitions were incorporated separately into models. The likelihood of unifocal disease increased with a high nomogram score (HR 4.3 (95% CI: 1.8–10.5)), in tumours fulfilling the focal treatment criteria (HR 2.4 (1.5–3.8)) and those appearing as low risk on biopsy (HR 2.9 (1.8–4.4)). In contrast, tumour bilaterality on biopsy (HR 0.27 (0.17–0.42)), increasing numbers of involved cores (HR 0.49 (0.04–0.9)) and high Gleason grade (HR 0.6 (0.4–0.9)) reduced the risk of unifocal disease. When compared with other parameters, bilateral disease on biopsy was the feature most strongly associated with multifocal disease.
Table 2. Pre-operative features of unifocal and multifocal prostate cancers.
|
Unifocal
|
Multifocal
|
HR 95% CI
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | P-value Univariable analysisa | P-value Multivariable analysisb | HR | Low | High | |
| Interval data | |||||||||
| Serum PSA at diagnosis (ng ml−1) | 5.5 | 3.1 | 6.4 | 3.8 | 0.005 | 0.07 | |||
| TRUS prostate volume (ml) | 36.8 | 16.2 | 33.2 | 14.5 | 0.014 | 0.3 | |||
| PSA density | 0.17 | 0.14 | 0.22 | 0.16 | 0.001 | 0.08 | |||
| Total length of tissue (mm) | 131.3 | 35.7 | 130.7 | 33.9 | 0.9 | ||||
| Positive cores (% of total) | 11 | 31.4 | 33 | 47.2 | <0.001 | 0.001 | 0.49 | 0.04 | 0.9 |
| Cumulative cancer length (mm) | 6 | 24.5 | 20 | 40.4 | <0.001 | 0.09 | |||
| Maximal tumour length (mm) | 3.1 | 2.7 | 5.1 | 5.7 | <0.001 | 0.08 | |||
| Nomogram prediction | 0.75 | 0.24 | 0.58 | 0.29 | <0.001 | <0.001 | 4.3 | 1.8 | 10.5 |
| Categorical data | n | % | n | % | |||||
| Gleason score | |||||||||
| Gleason 5–6 | 151 | 87.3 | 239 | 67.9 | |||||
| Gleason 7 | 20 | 11.5 | 102 | 29.2 | |||||
| Gleason 8–10 | 2 | 1.2 | 10 | 2.9 | <0.001 | 0.009 | 0.6 | 0.4 | 0.9 |
| Number of biopsy sessions | |||||||||
| One | 126 | 72.8 | 297 | 84.4 | |||||
| Two or more | 47 | 27.2 | 55 | 15.6 | 0.007 | 0.1 | |||
| Number of biopsy cores | |||||||||
| 10 or fewer | 131 | 75.7 | 297 | 84.4 | |||||
| More than 10 | 42 | 24.3 | 55 | 15.6 | 0.3 | ||||
| Lobes involved 2008 Focal therapy criteria, insignificant cancer | |||||||||
| Bilateral | 36 | 20.8 | 164 | 46.6 | <0.001 | <0.001 | 0.27 | 0.17 | 0.42 |
| Yes | 68 | 42.8 | 62 | 18.2 | <0.001 | 0.002 | 2.4 | 1.5 | 3.8 |
| Epstein's criteria | 59 | 37.1 | 51 | 15.0 | <0.001 | 0.9 | 0.9 | 0.83 | 0.97 |
| Low risk | 134 | 77.5 | 171 | 48.6 | <0.001 | 0.001 | 2.9 | 1.8 | 4.4 |
Abbreviations: CI=confidence interval; HR=Hazards ratio; PSA=prostate-specific antigen; TRUS=transrectal ultrasound.
ANOVA for continuous and χ2-test for categorical data.
Backward elimination logistic regression.
On the basis of this information available following prostate biopsy, 130 (25%) of the 525 men were predicted as being suitable for focal ablation (Table 3, Figure 1B). A review of their surgical specimens showed that 92 (71%) of these men harboured well-differentiated tumours. In total, 39% met Epstein's criteria and 56% met the more liberal criteria for insignificant disease. Overall, 31 (24%) had Gleason grade 4 elements and 14 (11%) had extracapsular extension. Multifocal disease was present in 106 out of 130 (82%) of these men. Of these, the second focus was pathologically insignificant in 61 out of 106 (57%). If these criteria were used to direct focal ablation within our patients, they would have correctly identified 18% of men with clinically significant solitary tumours; but would have also included 56% of men with pathologically insignificant tumours and 26% of men with poorly differentiated or locally advanced cancers (Figure 1A).
Table 3. Pathological features of tumours fulfilling pre-operative criteria for focal ablation.
|
Suitable for focal ablation
|
Unsuitable for focal ablation
|
||||
|---|---|---|---|---|---|
| n | % | n | % | χ2-test, P-value | |
| Total | 130 | 370 | |||
| Age (mean (s.d.)) | 61.3 (5.1) | 60.6 (4.9) | |||
| Differentiation | |||||
| Gleason 5 or 6 | 92 | 70.8 | 143 | 38.6 | |
| Gleason 3+4=7 | 30 | 23.1 | 166 | 44.9 | |
| Gleason 4+3=7 | 1 | 0.8 | 41 | 11.1 | |
| Gleason 8–10 | 0 | 0.0 | 14 | 3.8 | |
| Missing | 7 | 5.4 | 6 | 1.6 | <0.001 |
| Stage | |||||
| pT2 | 114 | 87.7 | 216 | 58.4 | |
| pT3 | 14 | 10.8 | 145 | 39.2 | |
| Missing | 2 | 1.5 | 9 | 2.4 | <0.001 |
| Insignificant cancer a | |||||
| Insignificant (Epstein) | 47 | 39.2 | 28 | 8.2 | <0.001 |
| Insignificant (liberal) | 73 | 56.2 | 70 | 19.7 | <0.001 |
| Other pathological features | |||||
| Vascular invasion | 0 | 0.0 | 15 | 4.1 | 0.02 |
| HGPIN | 121 | 93.1 | 338 | 91.8 | 0.65 |
| Seminal Vesicle invasion | 1 | 0.8 | 29 | 7.9 | 0.003 |
| Perineural invasion | 11 | 8.5 | 109 | 29.8 | <0.001 |
| Prostatectomy findings | |||||
| Single tumour | 17 | 13.1 | 94 | 25.4 | |
| Multiple tumours | 113 | 86.9 | 276 | 74.6 | 0.004 |
| Unifocal disease | 24 | 18.5 | 67 | 18.1 | |
| Multifocal cancers | 106 | 81.5 | 303 | 81.9 | 0.93 |
| Tumour volume | |||||
| Mean (s.d.) | 1.51 (3.2) ml | 4.04 (9.3) ml | <0.001 | ||
| Prostate volume b | |||||
| Mean (s.d.) | 42.8 (17.5) ml | 31.4 (13.3) ml | <0.001 | ||
| Prostatectomy weight | |||||
| Mean (s.d.) | 56.5 (21.4) g | 46.2 (17.2) g | <0.001 | ||
Abbreviations: HGPIN=high-grade prostatic intraepithelial neoplasia; s.d.=standard deviation.
Histological definition from the prostatectomy specimen.
Determined by transrectal ultrasound (TRUS) measurement.
t-test, P-value.
The criteria used to select men for focal prostate ablation did not reliably identify solitary lesions (Concordance index (C-index)=0.50), pathologically significant disease (C-index=0.64–0.71), tumour stage (C-index=0.65), tumour grade (C-index=0.68) or tumour volume (C-index=0.75). Men meeting these criteria were likely to harbour smaller tumours in larger prostates when compared with the other men in the study cohort (Table 3). In fact, the criteria developed to identify men for focal treatment were more likely to select patients on the basis of prostate volume (C-index=0.76) rather than tumour parameters.
Discussion
Our study demonstrates that focal prostate ablation is an inappropriate therapy for the majority of men presenting with PSA-detected localised prostate cancer. We found that measures available following prostate biopsy could not reliably identify men with solitary tumours amenable for focal therapy. Among men who do harbour well-differentiated solitary lesions, the majority are small lesions that are probably best managed by active surveillance.
Consensus criteria developed by experts to identify men for focal prostate ablation mostly relied on prostate weight and tumour volume and thus did not reliably identify clinically significant solitary prostate lesions. Of greater concern, these criteria included as many as one quarter of the men harbouring Gleason grade 4 disease or with capsular invasion (Figure 1B).
When we evaluated all the measures available following prostate biopsy, we found that markers of tumour extent could accurately identify men who should not receive focal prostate ablation, but we were unable to identify reliably those men with solitary lesions who would benefit from focal therapy. For example, when more than 50% of biopsy cores were involved with tumour, we found that most of these tumours (>95%) were multifocal. In contrast, multifocal disease was present in 75% of men with only 1 mm of cancer in one biopsy core. Our data support the concept of template-mapping protocols before performing regional ablation, and suggest the need for formal prospective evaluation of this method.
Our study may be limited in that it underestimates the proportion of solitary or insignificant cancers present in contemporary European or North-American practices. Reports describing these populations, however, reveal a similar proportion of solitary, multifocal or bilateral lesions to that we observed in our data (Table 4). Frequent testing for PSA may find prostate cancers earlier in their natural history, but the anatomical distribution of these cancers appears to be comparable to those identified in the United Kingdom.
Table 4. Previous reports of prostate cancer size and location.
| Reference | Center | Collection | Selection | N | Country | Solitary or unilateral (%) |
|---|---|---|---|---|---|---|
| Villers et al (1992) | Single | Retro | None | 234 | United States | 50 |
| Miller and Cygan (1994) | Single | Retro | None | 151 | United States | 44 |
| Djavan et al (1999) | Single | Retro | None | 308 | Austria | 33 |
| Wise et al (2002) | Single | Retro | None | 486 | United States | 17 |
| Noguchi et al (2003) | Single | Retro | T1c disease | 222 | United States | 24 |
| Ng et al (2004) | Single | Retro | None | 364 | United States | 15 |
| Eichelberger and Cheng (2004) | Single | Retro | None | 312 | United States | 15 |
| Horninger et al (2004) | Single | Retro | PSA <4.0 ng ml−1 | 80 | Austria | 35 |
| Cheng et al (2005) | Single | Retro | Small volume (<0.5 ml) | 62 | United States | 31 |
| Torlakovic et al (2005) | Single | Retro | None | 46 | Croatia | 35 |
| Muezzinoglu et al (2006) | Multi | Retro | None | 947 | United States, Turkey and Japan | 27 |
| Scales et al (2007) | Multi | Retro | Low riska | 261 | United States | 35 |
| Mouraviev et al (2007) | Single | Retro | None | 1184 | United States | 19 |
| Tareen et al (2009) | Single | Retro | None | 1467 | United States | 21 |
| Polascik et al (2009) | Single | Retro | Low/intermediate riskb | 538 | United States | 23 |
| Ward et al (2009) | Single | Retro | Unilateral disease on biopsy | 180 | United States | 17 |
| This series | Multi | Prospective | None | 525 | United Kingdom | 33 |
| Mean | 28 |
Abbreviation: PSA=prostate-specific antigen.
T1c or T2a, PSA⩽10 ng ml−1, Gleason ⩽6 and less than three positive cores.
⩽T2c, PSA⩽10 and Gleason ⩽7.
In summary, our analysis suggests that the majority of men presenting with prostate cancer following testing for PSA are inappropriate candidates for focal prostate ablation. Men who harbour solitary prostate cancers most often have insignificant disease that might be best managed by active surveillance (van den Bergh et al, 2009), whereas men harbouring multi-focal prostate cancers usually have clinically significant disease that requires more extensive treatment.
Acknowledgments
We thank Professor Lars Holmberg for his advice and critical appraisal of this work. The ProtecT study is funded by the Health Technology Assessment Programme of the National Institute for Health Research in the UK (projects 96/20/06 and 96/20/99). We thank other members of the ProtecT Study Group including John Anderson, Miranda Benney, Prasad Bollina, Sally Burton, Daniel Dedman, Alan Doherty, Garrett Durkan, Ingrid Emmerson, David Gillatt, Louise Goodwin, John Graham, David Gunnell, Helen Harris, Barbara Hattrick, Peter Holding, David Jewell, Clare Kennedy, Sue Kilner, Peter Kirkbride, Roger Kockelbergh, Howard Kynaston, Hing Leung, Malcolm Mason, Teresa Mewes, Steven Oliver, Alan Paul, Ian Pedley, Philip Powell, Liz Salter, Mark Sidaway, Carol Torrington, Lyn Wilkinson and Andrea Wilson.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
References
- Catto JW, Abbod MF, Linkens DA, Larre S, Rosario DJ, Hamdy FC (2009) Neurofuzzy modeling to determine recurrence risk following radical cystectomy for nonmetastatic urothelial carcinoma of the bladder. Clin Cancer Res 15: 3150–3155 [DOI] [PubMed] [Google Scholar]
- Challacombe BJ, Murphy DG, Zakri R, Cahill DJ (2009) High-intensity focused ultrasound for localized prostate cancer: initial experience with a 2-year follow-up. BJU Int 104: 200–204 [DOI] [PubMed] [Google Scholar]
- Chen ME, Johnston D, Reyes AO, Soto CP, Babaian RJ, Troncoso P (2003) A streamlined three-dimensional volume estimation method accurately classifies prostate tumors by volume. Am J Surg Pathol 27: 1291–1301 [DOI] [PubMed] [Google Scholar]
- Cheng L, Poulos CK, Pan CX, Jones TD, Daggy JK, Eble JN, Koch MO (2005) Preoperative prediction of small volume cancer (less than 0.5ml) in radical prostatectomy specimens. J Urol 174: 898–902 [DOI] [PubMed] [Google Scholar]
- Cooperberg MR, Broering JM, Kantoff PW, Carroll PR (2007) Contemporary trends in low risk prostate cancer: risk assessment and treatment. J Urol 178: S14–S19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denberg TD, Melhado TV, Steiner JF (2006) Patient treatment preferences in localized prostate carcinoma: the influence of emotion, misconception, and anecdote. Cancer 107: 620–630 [DOI] [PubMed] [Google Scholar]
- Djavan B, Susani M, Bursa B, Basharkhah A, Simak R, Marberger M (1999) Predictability and significance of multifocal prostate cancer in radical prostatectomy specimen. Tech Urol 5: 139–142 [PubMed] [Google Scholar]
- Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, Jewell D, Powell P, Gillatt D, Dedman D, Mills N, Smith M, Noble S, Lane A (2003) Prostate testing for cancer and treatment (ProtecT) feasibility study. Health Technology Assessment (Winchester, England) 7: 1–88 [DOI] [PubMed] [Google Scholar]
- Eggener SE, Scardino PT, Carroll PR, Zelefsky MJ, Sartor O, Hricak H, Wheeler TM, Fine SW, Trachtenberg J, Rubin MA, Ohori M, Kuroiwa K, Rossignol M, Abenhaim L (2007) Focal therapy for localized prostate cancer: a critical appraisal of rationale and modalities. J Urol 178: 2260–2267 [DOI] [PubMed] [Google Scholar]
- Eichelberger LE, Cheng L (2004) Does T2b prostate cancrinoma exist? Critical appraisal of the 2002 TNM classification of prostate carcinoma. Cancer 100: 2573–2576 [DOI] [PubMed] [Google Scholar]
- Epstein JI, Sanderson H, Carter HB, Scharfstein DO (2005) Utility of saturation biopsy to predict insignificant cancer at radical prostatectomy. Urology 66: 356–360 [DOI] [PubMed] [Google Scholar]
- Epstein JI, Walsh PC, Carmichael M, Brendler CB (1994) Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA 271: 368–374 [PubMed] [Google Scholar]
- Harrell Jr FE, Califf RM, Pryor DB, Lee KL, Rosati RA (1982) Evaluating the yield of medical tests. JAMA 247: 2543–2546 [PubMed] [Google Scholar]
- Horninger W, Berger AP, Rogatsch H, Gschendtner A, Steiner H, Niescher M, Klocker H, Bartsch G (2004) Characteristics of prostate cancers detected at low PSA levels. Prostate 58: 232–237 [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60: 277–300 [DOI] [PubMed] [Google Scholar]
- Kattan MW, Eastham JA, Wheeler TM, Maru N, Scardino PT, Erbersdobler A, Graefen M, Huland H, Koh H, Shariat SF, Slawin KM, Ohori M (2003) Counseling men with prostate cancer: a nomogram for predicting the presence of small, moderately differentiated, confined tumors. J Urol 170: 1792–1797 [DOI] [PubMed] [Google Scholar]
- Lane JA, Hamdy FC, Martin RM, Turner EL, Neal DE, Donovan JL (2010) Latest results from the UK trials evaluating prostate cancer screening and treatment: the CAP and ProtecT studies. Eur J Cancer 46: 3095–3101 [DOI] [PubMed] [Google Scholar]
- Lee MC, Dong F, Stephenson AJ, Jones JS, Magi-Galluzzi C, Klein EA (2009) The epstein criteria predict for organ-confined but not insignificant disease and a high likelihood of cure at radical prostatectomy. Eur Urol 58(1): 90–95 [DOI] [PubMed] [Google Scholar]
- Lindner U, Weersink RA, Haider MA, Gertner MR, Davidson SR, Atri M, Wilson BC, Fenster A, Trachtenberg J (2009) Image guided photothermal focal therapy for localized prostate cancer: phase I trial. J Urol 182: 1371–1377 [DOI] [PubMed] [Google Scholar]
- Meiers I, Waters DJ, Bostwick DG (2007) Preoperative prediction of multifocal prostate cancer and application of focal therapy: review 2007. Urology 70: 3–8 [DOI] [PubMed] [Google Scholar]
- Miller GJ, Cygan JM (1994) Morphology of prostate cancer: the effects of multifocality on histological grade, tumor volume and capsule penetration. J Urol 152: 1709–1713 [DOI] [PubMed] [Google Scholar]
- Mouraviev V, Sun L, Madden JF, Mayes JM, Moul JW, Polascik TJ (2007) Prostate cancer laterality does not predict prostate-specific antigen recurrence after radical prostatectomy. Urology 70: 1141–1145 [DOI] [PubMed] [Google Scholar]
- Muezzinoglu B, Frolov A, Ohori M, Scardino PT, Ayala M, Wheeler TM (2006) Clinicopathological significance of multifocal prostate cancer (abstract). Lab Invest 86: 151A [Google Scholar]
- Ng JC, Koch MO, Daggy JK, Cheng L (2004) Perineural invasion in radical prostatectomy specimens: lack of prognostic significance. J Urol 172(6 Part 1): 2249–2251 [DOI] [PubMed] [Google Scholar]
- Noguchi M, Stamey TA, McNeal JE, Nolley R (2003) Prognostic factors for multifocal prostate cancer in radical prostatectomy specimens: lack of significance of secondary cancers. J Urol 170: 459–463 [DOI] [PubMed] [Google Scholar]
- Onik G, Vaughan D, Lotenfoe R, Dineen M, Brady J (2008) The ‘male lumpectomy’: focal therapy for prostate cancer using cryoablation results in 48 patients with at least 2-year follow-up. Urol Oncol 26: 500–505 [DOI] [PubMed] [Google Scholar]
- Polascik TJ, Mayes JM, Schroek FR, Sun L, Madden JF, Moul JW, Mouraviev V (2009) Patient selection for hemiablative focal therapy of prostate cancer: variables predictive of tumor unilaterality based upon radical prostatectomy. Cancer 115: 2104–2110 [DOI] [PubMed] [Google Scholar]
- Roobol MJ, Kerkhof M, Schroder FH, Cuzick J, Sasieni P, Hakama M, Stenman UH, Ciatto S, Nelen V, Kwiatkowski M, Lujan M, Lilja H, Zappa M, Denis L, Recker F, Berenguer A, Ruutu M, Kujala P, Bangma CH, Aus G, Tammela TL, Villers A, Rebillard X, Moss SM, de Koning HJ, Hugosson J, Auvinen A (2009) Prostate cancer mortality reduction by prostate-specific antigen-based screening adjusted for nonattendance and contamination in the European Randomised Study of Screening for Prostate Cancer (ERSPC). Eur Urol 56: 584–591 [DOI] [PubMed] [Google Scholar]
- Sartor AO, Hricak H, Wheeler TM, Coleman J, Penson DF, Carroll PR, Rubin MA, Scardino PT (2008) Evaluating localized prostate cancer and identifying candidates for focal therapy. Urology 72: S12–S24 [DOI] [PubMed] [Google Scholar]
- Scales Jr CD, Presti Jr JC, Kane CJ, Terris MK, Aronson WJ, Amling CL, Freedland SJ (2007) Predicting unilateral prostate cancer based on biopsy features: implications for focal ablative therapy-results from the SEARCH database. J Urol 178: 1249–1252 [DOI] [PubMed] [Google Scholar]
- Sengupta S, Blute ML, Bagniewski SM, Inman B, Leibovich BC, Slezak JM, Myers RP, Zincke H (2008) After radical retropubic prostatectomy ‘insignificant’ prostate cancer has a risk of progression similar to low-risk ‘significant’ cancer. BJU Int 101: 170–174 [DOI] [PubMed] [Google Scholar]
- Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J (2004) The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years? J Urol 172: 1297–1301 [DOI] [PubMed] [Google Scholar]
- Steyerberg EW, Roobol MJ, Kattan MW, van der Kwast TH, de Koning HJ, Schroder FH (2007) Prediction of indolent prostate cancer: validation and updating of a prognostic nomogram. J Urol 177: 107–112 [DOI] [PubMed] [Google Scholar]
- Tareen B, Sankin A, Godoy G, Temkin S, Lepor H, Taneja SS (2009) Appropriate candidates for hemiablative focal therapy are infrequently encountered among men selected for radical prostatectomy in contemporary cohort. Urology 73: 351–354 [DOI] [PubMed] [Google Scholar]
- Torlakovic G, Torlakovic E, Skovlund E, Neslan JM, Reith A, Danielsen HE (2005) Volume related sequence of tumor distribution pattern in prostate carcinoma: importance of posterior midline crossover in predicting tumor volume, extracapsular extension, and seminal vesicle invasion. Croat Med J 46: 429–435 [PubMed] [Google Scholar]
- van den Bergh RC, Roemeling S, Roobol MJ, Aus G, Hugosson J, Rannikko AS, Tammela TL, Bangma CH, Schroder FH (2009) Outcomes of men with screen-detected prostate cancer eligible for active surveillance who were managed expectantly. Eur Urol 55: 1–8 [DOI] [PubMed] [Google Scholar]
- Villers A, McNeal JE, Freiha FS, Stamey TA (1992) Multiple cancers in the prostate. Morphologic features of clinically recognized versus incidental tumors. Cancer 70(9): 2313–2318 [DOI] [PubMed] [Google Scholar]
- Ward JF, Nakanishi H, Pisters L, Babaian RJ, Troncoso P (2009) Cancer ablation with regional templates applied to prostatectomy specimens from men who were eligible for focal therapy. BJU Int 104: 490–497 [DOI] [PubMed] [Google Scholar]
- Warmuth M, Johansson T, Mad P (2010) Systematic review of the efficacy and safety of high-intensity focussed ultrasound for the primary and salvage treatment of prostate cancer. Eur Urol 58: 803–815 [DOI] [PubMed] [Google Scholar]
- Wise AM, Stamey TA, McNeal JE, Clayton JL (2002) Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 60: 164–169 [DOI] [PubMed] [Google Scholar]