We read with interest the article by Della Porta and colleagues1 and the editorial of Prof. Cazzola2 relating to the role of comorbidities in myelodysplastic syndromes (MDS). We have previously published a paper on the role of comorbidities in MDS patients3 and we found it intriguing that a better definition can be made according to the match between the WPSS prognostic index and evaluation of comorbidities according to the MDS-specific comorbidity index (MDS-CI). A total of 418 MDS patients with comorbidities recorded at the time of diagnosis entered the analysis: data concerning comorbidities for another 32 patients were retrieved from our previous report. In the final cohort of 450 patients with comorbidity data available and conservatively treated, we tried to provide a better definition of outcome, as suggested in the Della Porta publication.1 Comorbidities were recorded at the time of diagnosis and provided by medical staff for the analysis. All patients were consecutively diagnosed and followed at our institute in a period between January 1992 and December 2006. The MDS-CI was applied as reported by Della Porta et al.1 Statistical analysis was carried out using SPSS software; survival was defined as survival from the time of diagnosis to last contact or death for any cause.
Application of the WPSS prognostic index4 was possible in 330 of 450 patients who entered this analysis (73%) according to cytogenetic availability of data: we identified 112 patients with very low/low risk (34%), 137 patients with intermediate risk (41.5%) and 81 patients with high/very high risk (24.5%). The median age of the whole population was 69 years (range 21–88 years) with a prevalence of males (male to female ratio 1.6). Overall, we found the presence of one or more comorbidities in 94% of the examined patients. Cardiac disorders were the most common comorbidities observed (40% of patients); the second most common was diabetes with organ damage in 22 cases. Application of the MDS-CI score identified 300 patients with score 0, 55 patients with score 1, 80 patients with score 2, and 15 patients with a score over 2. We found significant differences in overall survival according to MDS-CI stratification: from 38 months for low risk patients (score 0) to 22 months for high-risk patients (score >2, P=0.02).
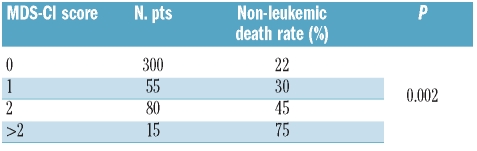
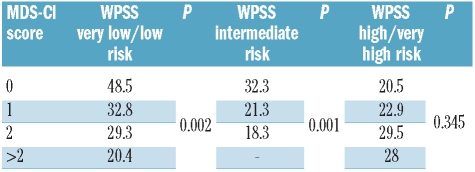
We then evaluated the prognostic effect of the MDS-CI on patients stratified according to the WPSS prognostic index. As suggested also in the article by Della Porta and colleagues,1 we assessed prognostic relevance of comorbidity in very low/low risk WPSS patients, intermediate and high/very high-risk patients. We found that in the first category, a significant difference in overall survival stratification was observed: from 48.5 months for patients with score 0 according to the MDS-CI to 20.4 months for patients with a score over 2 (P=0.002). In WPSS intermediate risk, we found similar significant differences in overall survival: from 32.3 months for patients with score 0 according to the MDS-CI to 18.3 months for patients with score 2 according to the MDS-CI (P=0.001). Conversely, we did not find any significant differences in WPSS high/very high-risk patients (Table 2). We also found significant the correlation between presence of comorbidities at baseline as stratified with MDS-CI and risk of non-leukemic death: from 22% in patients without comorbidities to 75% in patients with a score over 2 according to MDS-CI (P=0.002). Our analysis showed the feasibility of using the MDS-CI in a large series of consecutive MDS patients, diagnosed and followed in a single center. Our analysis also strengthens the results reported by Della Porta and colleagues1 because the value of comorbidity was confirmed in a cohort of patients similar to that observed in their original paper;1 in terms of median age (69 years in our series vs. 66 years in the Pavia experience), but with a higher percentage of patients with intermediate WPSS risk (41.5% in our series vs. 18% in the Pavia experience).
Table 2.
Non-leukemic death risk according to MDS-CI.
Table 1.
Overall survival (expressed in months) according to matched analysis between MDS-CI and WPSS.
MDS-CI is a very valid tool capable of differentiating MDS patients with very low/low and intermediate WPSS risk in terms of overall survival and non-leukemic death risk (Table 2). Thus, the prognostic relevance of comorbidities in MDS will help us to improve management of this disease and to better define clinical-decision making in the low risk category of these patients.
Footnotes
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Della Porta MG, Malcovati L, Strupp C, Ambaglio I, Kuendgen A, Zipperer E, et al. Risk stratification based on both disease status and extra-hematologic comorbidities in patients with myelodys-plastic syndrome. Haematologica. 2011;96(3):441–9. doi: 10.3324/haematol.2010.033506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cazzola M. Risk assessment in myelodysplastic syndromes and myelodysplastic/myeloproliferative neoplasms. Haematologica. 2011;96(3):349–52. doi: 10.3324/haematol.2010.030023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breccia M, Federico V, Latagliata R, Mercanti C, D’Elia GM, Cannella L, et al. Evaluation of comorbidities at diagnosis predicts outcome in myelodysplastic syndrome patients. Leuk Res. 2011;35(2):159–62. doi: 10.1016/j.leukres.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R, et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol. 2007;25(33):3503–10. doi: 10.1200/JCO.2006.08.5696. [DOI] [PubMed] [Google Scholar]