Abstract
Background
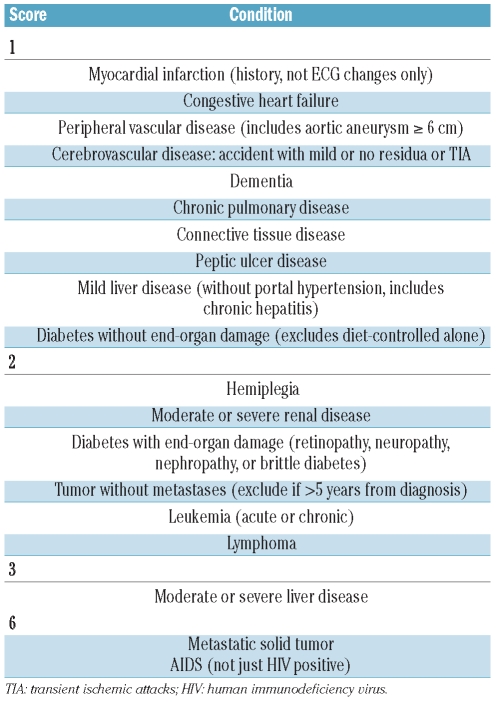
Comorbidities may affect survival and choice of treatment among cancer patients. In fact, comorbidities have been identified as significant determinants of response to therapy in older patients with acute myeloid leukemia, breast cancer, head and neck cancer, and lung cancer. The Charlson comorbidity index and adult comorbidity evaluation-27 are lists of comorbidities with a weight assigned from 1 to 6 for the former and from 0 to 3 for the latter score, derived from relative risk estimates of a proportional hazard regression model using clinical data.
Design and Methods
We retrospectively evaluated the Charlson index and adult comorbidity evaluation-27 score in a cohort of 125 elderly (> 60 years) patients with chronic phase chronic myeloid leukemia who received dasatinib after showing resistance or intolerance to imatinib with the aim of establishing associations between comorbidities and the development of pleural effusions or compliance with the drug treatment.
Results
We found a significant association between the Charlson index as well as the adult comorbidity evaluation-27 score and the rate of drug reduction or suspension: with regards to the Charlson index, 49% of score 0 patients had a dose reduction compared to 63% of patients with score 1, 74% of those with score 2 and 100% of patients with score 3–5 (P=0.03); with regards to the adult comorbidity evaluation-27 score, 45% of patients had score 0–1 and 69% of patients with score 2–3 had a dose reduction. Of the 65 patients with Charlson score 0, 29% had at least one suspension of treatment (79% for hematologic and 21% for non-hematologic toxicity), compared to 46% of patients with score 1 (37% for hematologic and 69% for non-hematologic toxicity), 58% of patients with score 2 (36% for hematologic and 64% for non-hematologic toxicity) and 100% of patients with score 3 or 4 (all patients for both types of toxicity). High adult comorbidity index-27 scores identified patients at high risk of grade 3/4 hematologic toxicity. Forty-one patients (32.8%) experienced pleural effusion during treatment: the highest scores for both indices were associated with an increased risk of pleural effusions.
Conclusions
In elderly patients with chronic myeloid leukemia treated with dasatinib, the rate of drug reduction or suspension and the incidence of pleural effusions seem to be associated with the presence of comorbidities: stratification according to the Charlson index and adult comorbidity evaluation-27 score before dasatinib therapy may enable the identification of patients at risk of major toxicities.
Keywords: chronic myeloid leukemia, dasatinib, Charlson comorbidity index, adult comorbidity evaluation 27 (ACE-27)
Introduction
Despite the beneficial effect of imatinib treatment in chronic myeloid leukemia (CML), some patients develop resistance and/or intolerance to this drug and need to switch to second-generation tyrosine kinase inhibitors such as nilotinib or dasatinib.1,2 Dasatinib is an oral dual tyrosine kinase inhibitor active against abl and Src-family kinases; it inhibits BCR–ABL1 with a 50% inhibitory concentration (IC50) of less than 1 nmol/L and its structure is based on a different chemical scaffold to that of imatinib with a 325-fold greater potency.3
Pleural/pericardial effusions are possible complications during treatment with dasatinib and are usually managed by reducing the dose of the drug administered or discontinuing the drug completely.4 Changing the dasatinib regimen from 70 mg twice daily to 100 mg once daily reduces the risk of this complication.5 Several factors have been indicated to predispose to pleural effusions, such as a previous history of cardiac disease or auto-immune disorders, a previous skin rash as an adverse event occurring during imatinib treatment, hypertension, hypercholesterolemia, advanced disease phase, twice daily dosing regimen, and high dose of the drug.6,7
Comorbidity, as defined by Feinstein,8 is any distinct additional clinical entity that pre-exists or occurs during the clinical course of a patient with a primary disease. Comorbidities may affect survival and choice of treatment among cancer patients: in fact they have been identified as significant determinants of response to therapy in older patients with acute myeloid leukemia, female breast cancer, head and neck cancer or lung cancer.9,10 The Charlson comorbidity index (CCI) is a list of 19 comorbid conditions: each condition has a weight assigned from 1 to 6, which was derived from relative risk estimates of a proportional hazard regression model using clinical data. The adult comorbidity evaluation-27 (ACE27) is a new 27-item comorbidity index for patients with cancer.9 The ACE27 was developed through modification of the Kaplan-Feinstein Comorbidity Index. ACE27 includes comorbid conditions of various organ systems such as cardiovascular, respiratory, gastrointestinal, renal, endocrine, neurological, psychiatric, rheumatological, and immunological systems, as well as malignancy, substance abuse, and body weight. Each category has three grades (1, mild; 2, moderate; and 3, severe), with the overall comorbidity score defined according to the highest ranked single ailment. Two or more grade 2 ailments occurring in different organ systems result in a grade 3 assignment. ACE27 grades were listed as 0, 1, 2 or 3 in the hospital information system.
There are only limited data in the literature on the role of comorbidities in CML patients, and the data are essentially from patients who were candidates for allogeneic bone marrow transplantation.11 The aim of our study was to establish the impact of comorbidities in the setting of elderly CML patients switched to dasatinib following resistance to imatinib, and to assess their possible role in the development of toxicities.
Design and Methods
The present study included 125 patients aged over 60 years old with CML in chronic phase treated in 21 Italian Centers, who received dasatinib after being resistant or intolerant to imatinib. Participating centers were asked to send data on all consecutive chronic phase CML patients who fulfilled the following inclusion criteria, irrespective of response or median time on treatment: (i) age greater than 60 years; (ii) in chronic phase at the time of starting dasatinib. No exclusion criteria were considered. Patients were treated with dasatinib given for compassionate use or prescribed, from 2007, after imatinib resistance or intolerance. Baseline data (sex, age, Sokal risk, imatinib dose, reason for switching to dasatinib, other therapy, starting dose of dasatinib) were recorded at the time of both imatinib and dasatinib treatment: during this latter treatment we also recorded the dosage, any side effects and grades of toxicity, days of interruptions, and reasons for discontinuing the drug. Responses to standard-dose imatinib were defined according to European LeukemiaNet recommendations.12
Intolerance to imatinib was defined as the occurrence of severe or moderate but persistent or recurrent hematologic or extra-hematologic toxicity during imatinib treatment, requiring permanent drug discontinuation. Hematologic and extra-hematologic toxicities were graded according to the World Health Organization (WHO) scale, such that severe toxicity was considered grade 3–4 on the WHO scale and moderate toxicity as grade 2 on the WHO scale.
Comorbidities were registered in all patients at the time of diagnosis by medical staff, before any therapeutic intervention. On the basis of the information collected we retrospectively calculated the modified CCI and ACE27 (Table 1).9 Analyses were conducted of the impact of stratification according to the CCI and the hematologic and non-hematologic toxicities experienced during dasatinib treatment. A complete ACE27 data form is available on http://oto.wustl.edu/clinepi/calc.html (Clinical Outcomes Research Office’s Website). This study was approved by the Ethics Board and all patients provided informed consent according to institutional guidelines.
Table 1.
Charlson comorbidity index.
Statistical analyses were carried out using the SPSS software package. In particular, responses and frequency of toxicities were compared using a χ2 or Fisher’s exact test. With a Cochran-Armitage test of trend we assessed the presence of an association between variables with several categories. P values less than 0.05 were considered statistically significant.
Results
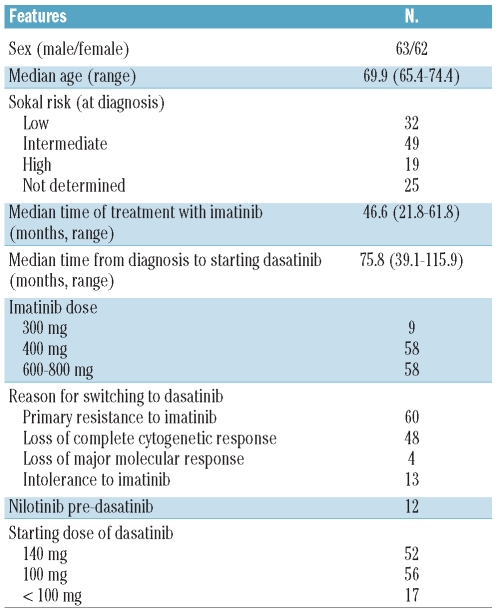
The patients’ clinical features are shown in Table 2. There were 63 males and 62 females; the Sokal risk score at diagnosis was low in 34 patients, intermediate in 49, high in 19 and not evaluable in 25. The median age at the time of starting dasatinib therapy was 69.9 years (interquartile range, 65.4–74.4), the median interval from diagnosis to dasatinib therapy was 75.8 months (interquartile range, 39.1–115.9); 57/125 patients (45.6%) had received interferon-based therapy before imatinib. As regards imatinib treatment, all but nine patients had initially received the 400 mg daily standard dosage and in 58/125 patients (46.4%) the dosage was increased to 600–800 mg/day; overall, the median period of imatinib treatment was 46.6 months (interquartile range, 21.8–61.8). Thirteen patients were considered as intolerant to imatinib treatment and 112 as resistant to this therapy. The starting dosage of dasatinib was 140 mg in 52 patients, 100 mg in 56 patients and less than 100 mg in the remaining 17 patients.
Table 2.
Clinical features of 125 elderly CML patients at the time of starting dasatinib therapy.
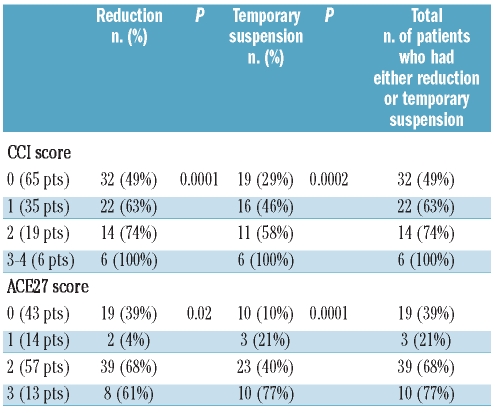
Table 3 shows the correlations between CCI stratification and toxicity and adjustment of dasatinib dose. With regards to the CCI stratification, a score of 0 was assigned to 65 patients, whereas a score of 1 or more was assigned to 60 patients (35 patients, score 1; 19 patients, score 2; 5 patients, score 3; 1 patient, score 4). We found a significant association between CCI score and the rate of drug dose reduction or suspension: during dasatinib treatment 49% of score 0 patients had a dose reduction compared to 63% of patients with score 1, 74% of patients with score 2 and 100% of patients with score 3 or 4 (P=0.0001, Table 3). Of the 65 patients with score 0, 29% had at least one suspension (79% for hematologic and 21% for non-hematologic toxicity), compared to 46% of patients with score 1 (37% for hematologic and 69% for non-hematologic toxicity), 58% of patients with score 2 (36% for hematologic and 64% for non-hematologic toxicity) and 100% of patients with score 3 or 4 (all patients for both types of toxicity) (P=0.0002). ACE27 stratification identified high frequencies of reductions and temporary suspensions in patients with score 2 or 3.
Table 3.
Correlations between CCI and ACE27 stratification and dasatinib dose adjustment
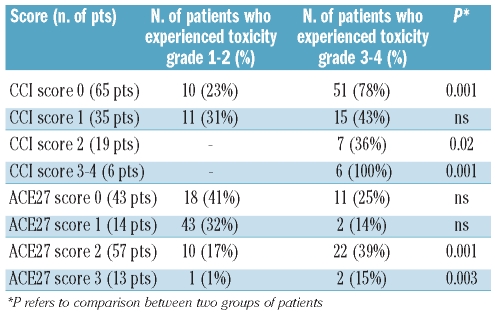
Both the CCI and ACE27 stratification were able to identify patients with a high risk of developing hematologic toxicity: grade 3/4 neutropenia and thrombocytopenia most frequently occurred in patients with an overall CCI score of 2–4 and a grade 2 or higher ACE27 score (Table 4).
Table 4.
ACE27 and CCI stratification and hematologic toxicity (neutropenia and/or thrombocytopenia).
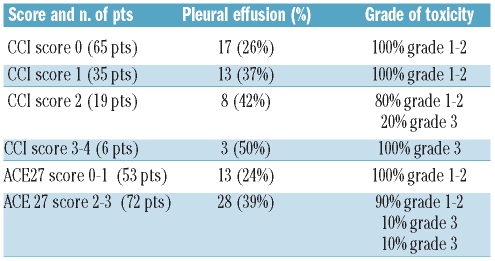
Table 5 shows the correlations between CCI and ACE27 stratification and the incidence and grade of pleural effusions. During dasatinib treatment, 41/125 patients (32.8%) presented with a pleural effusion, which was of grade 2 in 31 patients and of grade 3 or 4 in ten patients (24.4% of the 41 patients with pleural effusion and 8% of the entire cohort of patients), according to the WHO scale; in 11/41 patients (26.8%), there was a concomitant pericardial effusion. In addition, pleural effusion was recurrent in 19/41 patients (46.4%). The median time from starting dasatinib treatment to the occurrence of the first pleural effusion was 10.4 months (interquartile range, 2.2 – 18.1). Among the 41 patients with a pleural effusion, eight (19.5%) did not require interruption of dasatinib while 33 (80.5%) discontinued therapy; however, dasatinib was successfully restarted in 28/33 patients (84.8%) after a median period of 20 days (interquartile range, 15–38) and, overall, only five patients (12.1% of the 41 patients with a pleural effusion and 4% of the entire cohort of patients) required permanent discontinuation of dasatinib.
Table 5.
Correlations between CCI and ACE27 stratification and incidence and grade of pleural effusions.
CCI stratification applied to the 41 patients (32.8%) who experienced pleural effusion during treatment revealed that this complication occurred in 17 (26%) of the 65 patients with score 0, 13 (37%) of the 35 patients with score 1, in 8 (42%) of the 19 patients with score 2 and in 3 (50%) of the 6 patients with score 3 or 4. More pleural effusions occurred in patients who had a score of 1 or more but received a higher dose of dasatinib (140 mg). The severity of pleural effusions showed the same correlation: a grade 3 effusion was detected only in patients with a CCI score of greater than 2. Likewise, higher frequencies of pleural effusions were observed among patients with an ACE27 score of 2 or 3 and a similar correlation was seen regarding the intensity and severity of effusions. There were no differences among patients with or without pleural effusions as concerns response rate and overall survival (data not shown).
Discussion
The choice of second-line therapy of CML in the era of tyrosine kinase inhibitors is currently based on the type of mutation that developed during imatinib treatment and on comorbidities associated with the disease, because of the different side effects of the various drugs.14 Pleural effusion is a rather frequent complication of dasatinib therapy; it is usually mild to moderate and is associated with several risk factors, such as advanced disease phases, a twice-daily dosing schedule, a daily dose equal to or higher than 140 mg, and concomitant or previous cardiac disease.15 The pathogenesis is likely multi-factorial, and is possibly due to tyrosine-kinase inhibition or immune-mediated effects involving other tyrosine kinases (TEC or BTK of lymphocyte B and T signaling).7 The management of this side effect includes therapy interruption, drug dose reduction, steroids and diuretics and, only in a few severe instances, therapeutic thoracentesis.6,7,15 Data from a phase III trial showed a slight increase of the incidence of this side effect over time, but not of grade 4 cases, after a follow-up of 3 years.5 With adequate management and monitoring of patients with predisposing factors, the majority of individuals can continue therapy with the drug, even in the presence of this complication.
Until now, no published studies performed a complete analysis of concomitant diseases or medications associated with dasatinib-induced pleural effusion, although Porkka et al. reported that older age (>66 years) is the most important negative prognostic factor, based on the results of an optimization phase III trial of dasatinib in patients resistant/intolerant to imatinib.4 The median age of patients enrolled in the 100 mg once daily arm of this trial was 56 years. The incidence of pleural effusions of all grades was 14% compared to 25% in the 70 mg twice daily arm and the last follow-up confirmed a slight increase of all grades and the absence of grade 4. In our series of elderly patients, the overall rate of pleural effusions was higher than that in other published studies, probably because we did not use exclusion criteria for observation of this group of patients. Recently, Khoury et al. reported the role of age in patients treated with front-line dasatinib 100 mg once daily: no age-related differences were found in efficacy, whereas the safety profile of the drug differed according to the age of the patients, with the fluid retention rate being 35% in patients aged over 65 years compared to 13% in patients aged under 46 years old.16 The effect of dasatinib combined with concomitant medications was recently examined in a sub-analysis of patients who received front-line dasatinib: the rate of fluid retention in patients who received dasatinib alone or associated with one to three of four or more concomitant medications was 9%, 23% and 24%, respectively. The pleural effusion rate was 1% in patients who took dasatinib alone and 13% in patients who took dasatinib in association with concomitant drugs.17
Comorbidities and poor performance status influence the prognosis of patients affected by cancers.9,10 Comorbidities may influence clinical decision-making concerning treatment; in studies on various types of cancer, comorbidities have been shown not only to affect cancer risk, but also to affect cancer survival by limiting treatment choices, especially in the subset of elderly patients.9 An accurate evaluation of extra-hematologic comorbidities must be part of the prognostic assessment of patients with CML, especially those who need treatment with a second-generation tyrosine kinase inhibitor. At present the choice of a second-line tyrosine kinase inhibitor can be based on an individual’s mutational profile and comorbidities.
In our experience, the application of two different comorbidity scores, i.e. the CCI and ACE27, might be of help in identifying patients at higher risk of the development of pleural effusions; such patients need close monitoring of adverse events during dasatinib treatment. In fact, we found a correlation between the CCI and ACE27 stratifications and the incidence of pleural effusion, with effusions being more frequent among patients with a score of 2 or more.
Both the CCI and ACE27 stratifications were able to identify patients at high risk of hematologic toxicity and decreased compliance: the higher the comorbidity score, the higher the risk of developing toxicity and consequent requirement for temporary drug suspension. The results of our study showed that the evaluation of comorbidities may help to identify patients at higher risk of scarce compliance due to toxicity: these findings do not imply that the drug cannot be used in this setting of patients nor that the patients cannot be protected from developing pleural effusions, based on the evaluation of comorbidities. Comorbidities deserve more attention during treatment in order to adjust the dose appropriately, periodically monitor cardiac safety, optimize blood pressure and serum cholesterol levels and promptly evaluate chest X-rays at the first appearance of symptoms of effusions, such as a dry cough or dyspnea.
In conclusion, evaluation of comorbidities in elderly CML patients before treatment with dasatinib could be useful to identify subjects at higher risk of developing complications and to tailor treatment.
Appendix
All these authors also contributed to this study. Federica Sorà (Ematologia, Università del Sacro Cuore, Roma), Enrico Montefusco (Ematologia, Ospedale Sant’Andrea, Roma), Dario Ferrero (Ematologia, Università di Torino), Pellegrino Musto (Ematologia, Rionero in Vulture), Mario Tiribelli (Ematologia, Università di Udine), Gianni Binotto (Ematologia, Università di Padova), Ubaldo Occhini (Ematologia, Ospedale San Donato, Arezzo), Raffaele Vallone (Ematologia, Benevento), Bruno Martino (Ematologia, Ospedale Bianchi-Melacrino-Morelli, Reggio Calabria).
Footnotes
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Deininger MW, O’Brien SG, Guilhot F, Goldman JM, Hochhaus A, Hughes TP, et al. International randomized study of inter-feron vs STI571 (IRIS) 8-year follow-up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP) treated with imatinib. Blood. 2009;114:1126. [Google Scholar]
- 2.Jabbour E, Cortes J, Kantarjian H. Dasatinib for the treatment of Philadelphia chromosome-positive leukemias. Expert Opin Investig Drugs. 2007;16(5):679–87. doi: 10.1517/13543784.16.5.679. [DOI] [PubMed] [Google Scholar]
- 3.Steinberg M. Dasatinib: a tyrosine kinase inhibitor for the treatment of chronic myelogenous leukemia and Philadelphia chromosome postive acute lymphoblastic leukemia. Clin Ther. 2007;29(11):2289–308. doi: 10.1016/j.clinthera.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Porkka K, Khoury HJ, Paquette RL, Matloub Y, Sinha R, Cortes JE. Dasatinib 100 mg once daily minimizes the occurrence of pleural effusion in patients with chronic myeloid leukemia in chronic phase and efficacy is unaffected in patients who develop pleural effusion. Cancer. 2010;116(2):377–86. doi: 10.1002/cncr.24734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah NP, Kantarjian H, Kim DW, Rea D, Dorlhiac-Llacer PE, Milone JH, et al. Intermittent target inhibition with dasatinib 100 mg once daily preserves efficacy and improves tolerability in imatinib-resistant and –intolerant chronic phase chronic myeloid leukemia. J Clin Oncol. 2008;26(19):3204–12. doi: 10.1200/JCO.2007.14.9260. [DOI] [PubMed] [Google Scholar]
- 6.Quintas-Cardama A, Kantarjian H, O’Brien S, Borthakur G, Bruzzi J, Munden R, Cortes J. Pleural effusion in patients with chronic myelogenous leukemia treated with dasatinib after imatinib failure. J Clin Oncol. 2007;25(25):3908–14. doi: 10.1200/JCO.2007.12.0329. [DOI] [PubMed] [Google Scholar]
- 7.de Lavallade H, Punnialingam S, Milojkovic D, Bua M, Korashad JS, Gabriel IH, et al. Pleural effusions in patients with chronic myeloid leukemia treated with dasatinib may have an immune-mediated pathogenesis. Br J Haematol. 2008;141(5):745–7. doi: 10.1111/j.1365-2141.2008.07108.x. [DOI] [PubMed] [Google Scholar]
- 8.Feinstein AR. The pre-therapeutic classification of comorbidity in chronic disease. J Cron Dis. 1970;23:455–68. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- 9.Breccia M, Frustaci AM, Cannella L, Stefanizzi C, Latagliata R, Cartoni C, et al. Comorbidities and FLT3-ITD abnormalities as independent prognostic indicators of survival in elderly acute myeloid leukemia patients. Hematol Oncol. 2009;27(3):148–53. doi: 10.1002/hon.889. [DOI] [PubMed] [Google Scholar]
- 10.Birim O, Kappetein AP, Bogers AJJC. Charlson comorbidity index as a predictor of long-term outcome after surgery for non-small cell lung cancer. Eur J Cardiothorac Surg. 2005;28(5):759–62. doi: 10.1016/j.ejcts.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 11.Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–19. doi: 10.1182/blood-2005-05-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baccarani M, Saglio G, Goldman JM, Hochhaus A, Simonsson B, Appelbaum F, et al. European LeukemiaNet. Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2006;108(6):1809–20. doi: 10.1182/blood-2006-02-005686. [DOI] [PubMed] [Google Scholar]
- 13.Gabert J, Beillard E, van der Velden VH, Bi W, Grimwade D, Pallisgaard N, et al. Standardization and quality control studies of real-time quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia- a Europe Against Cancer program. Leukemia. 2003;17(12):2318–57. doi: 10.1038/sj.leu.2403135. [DOI] [PubMed] [Google Scholar]
- 14.Mauro MJ. Appropriate sequencing of tyro-sine kinase inhibitors in chronic myelogenous leukemia: when to change? A perspective in 2009. Curr Opin Hematol. 2009;16(2):135–39. doi: 10.1097/MOH.0b013e3283257b2b. [DOI] [PubMed] [Google Scholar]
- 15.Breccia M, Alimena G. Pleural/pericardic effusions during dasatinib treatment: incidence, management and risk factors associated to their development. Expert Opin Drug Safety. 2010;9(5):713–21. doi: 10.1517/14740331003742935. [DOI] [PubMed] [Google Scholar]
- 16.Khoury HJ, Cortes JE, Kantarjian H, Baccarani M, Shah NP, Bradley-Garelik MB, et al. Safety and efficacy of dasatinib vs imatinib by baseline comorbidity in patients with chronic myeloid leukemia in chronic phase (CML-CP): analysis of the DASISION trial. Blood. 2010;116:3421. [Google Scholar]
- 17.Guilhot F, Kantarjian H, Shah NP, Hochhaus A, Bradley-Garelik MB, Dejardin D, Cortes JE. Dasatinib (versus imatinib) in patients with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP): analysis of safety and efficacy by use of baseline medications in the DASISION trial. Blood. 2010;116:2295. [Google Scholar]