Abstract
Objective
Despite the negative effects of depression in Parkinson’s disease, there is currently no evidence-based standard of care. The purpose of this study was to examine the efficacy of individually-administered Cognitive Behavior Therapy (CBT) versus clinical monitoring (with no new treatment) for depression in this medical population.
Methods
Eighty depressed (DSM-IV criteria) patients with Parkinson’s disease participated in an NIH-sponsored randomized-controlled trial of CBT vs. clinical monitoring (1:1 ratio) in an academic medical center from April 2007 to July 2010. All patients concurrently continued under the care of their personal physicians on stable medication regimens. The Hamilton Depression Rating Scale (HAM-D 17) was the primary outcome. CBT was modified to meet the unique needs of the Parkinson’s population and provided for 10 weeks. Assessments were completed at baseline and 5 (midpoint), 10 (end of treatment), and 14 weeks (follow-up) post-randomization by blind raters.
Results
The CBT group reported greater reductions in depression (HAM-D 17) vs. clinical monitoring (P<.0001). At week 10, mean HAM-D change was 7.35 for CBT vs. 0.05 for clinical monitoring (P<.0001). CBT was also superior to clinical monitoring on several secondary outcomes (i.e., Beck Depression Inventory, anxiety, quality of life, coping, Parkinson’s disease symptom ratings). There were more treatment responders in the CBT group (56% vs. 8%, P<.0001).
Conclusions
CBT may be a viable approach for the treatment of depression in Parkinson’s disease. Further research is needed to replicate and extend these findings.
Introduction
Parkinson’s disease, the second most common neurodegenerative disorder in the US, is defined by the motor triad of tremor, rigidity, and bradykinesia. The majority of patients also experience non-motor complications (1), which are more closely associated with rates of disability and distress than are the motor symptoms of Parkinson’s disease (2). Depression, the most prevalent non-motor concern (3), affects approximately 50% of patients (4). Depression in Parkinson’s disease is characterized by high rates of psychiatric comorbidity (5) and executive dysfunction (6), and is linked with faster physical and cognitive decline (7), poorer quality of life (8), and increased caregiver burden (9). Despite these negative effects, there is currently no evidence-based standard of care.
Pharmacological interventions have received the most empirical attention to date. Antidepressants (10,11), dopamine agonists (12), and alternative treatments, such as omega-3 fatty acids (13), have demonstrated beneficial effects in preliminary controlled studies. Psychotherapeutic approaches, such as cognitive behavior therapy (CBT) have been the focus of fewer scientific investigations, despite demonstrated efficacy in the aged (14) and other debilitating medical conditions (15). Only small pilot studies have examined the utility of CBT for depression in Parkinson’s disease with promising results (16, 17, 18, 19, 20, 21). In other patient groups, CBT has shown comparable effects to antidepressants for mild depression, with combination treatment appearing most effective for moderate-to-severe forms of depression (22). Additional research is needed to inform the development of specific treatment recommendations for this medical population.
The purpose of this study was to conduct the first randomized-controlled trial of CBT for depression in Parkinson’s disease. We hypothesized that CBT would result in greater decreases in depressive symptoms, anxiety, negative thoughts, sleep disturbance, and caregiver burden, and greater improvements in quality of life, coping, and social support than clinical monitoring (with no new treatment). Furthermore, we hypothesized that there would be more “treatment responders” in the CBT group. The impact of CBT on Parkinson’s disease symptom ratings was also explored.
Methods
The study had the full approval of the Robert Wood Johnson Medical School IRB. After a complete description of the study to participants, written informed consent was obtained (prior to the initiation of any study procedures). Participants received the study treatment at no cost and were compensated $20 for each in-person and $10 for each telephone assessment. Treatment and evaluation occurred at Robert Wood Johnson Medical School. Patients enrolled in the study with a caregiver.
Half of the participants received CBT, plus clinical monitoring. The other half only received clinical monitoring. This “additive” design has been recommended for use when exploring the relative efficacy of a new psychotherapy intervention (23).
All patients concurrently continued under the care of their personal physicians on stable medical regimens. Depression was addressed in the same manner that it was handled (e.g., antidepressant medication at a stable dose) prior to the study. No new depression treatment (other than CBT in the experimental condition) was provided to study participants. Patients assigned to the control group (clinical monitoring only) had the option to receive the CBT package after week 14.
Patients
Participants were recruited from the Richard E. Heikkila Movement Disorders Clinic, local newspapers, and the New Jersey Chapter of the American Parkinson’s Disease Association between April 2007 and March 2010. The final follow-up occurred July 2010. Patient inclusion criteria were: 1) Parkinson’s disease by research criteria (24); 2) Primary Major Depression, Dysthymia, or Depression Not Otherwise Specified per the Structured Clinical Interview (SCID) for the Diagnostic and Statistical Manual of Mental Disorders 4th Edition (DSM-IV); 3) Clinical Global Impression Severity Scale ≥ 4 [at least moderately ill (25)]; 4) ages 35–85; 5) Stable medication regimen ≥ 6 weeks; 6) Family member or friend willing to participate. Expert panel guidelines were followed regarding the diagnosis of depression in Parkinson’s disease (26). Patients with comorbid anxiety disorders were eligible to enroll as long as the depressive disorder was primary.
Patients in both study groups continued with mental health care (other than CBT) that was stabilized (≥ 6 weeks) prior to baseline. Medication use and mental health care utilization was tracked throughout the study. New depression treatment was a criterion for early termination.
Patient exclusion criteria included: 1) Dementia [score below 5th percentile for age on memory and at least one other subscale on the Mattis Dementia Rating Scale (27) ]; 2) Off-time ≥50% of the day; 3) Suicidal Ideation; 4) Unstable medical conditions; 5) Bipolar, Psychotic Spectrum, or Substance Abuse Disorders (DSM-IV); 6)Receiving CBT elsewhere.
Caregiver inclusion/exclusion criteria encompassed: 1) ages 25–85; 2) daily contact with the study patient; 3) no unstable medical or psychiatric conditions (clinical interview).
Randomization and Masking
Appropriate candidates were allocated to receive CBT plus clinical monitoring or clinical monitoring only (1:1 ratio), by computer generated random assignment (run by the statistical consultant MAG). Randomization was stratified by antidepressant use at screening (yes/no) and done in blocks of 6 consecutive patients within each stratum.
All follow-up (i.e., post-baseline) assessments were conducted by independent evaluators without knowledge of treatment condition. Patients were instructed not to reveal group assignment to raters. Patients and therapists were not blind given the nature of the treatment.
Procedure
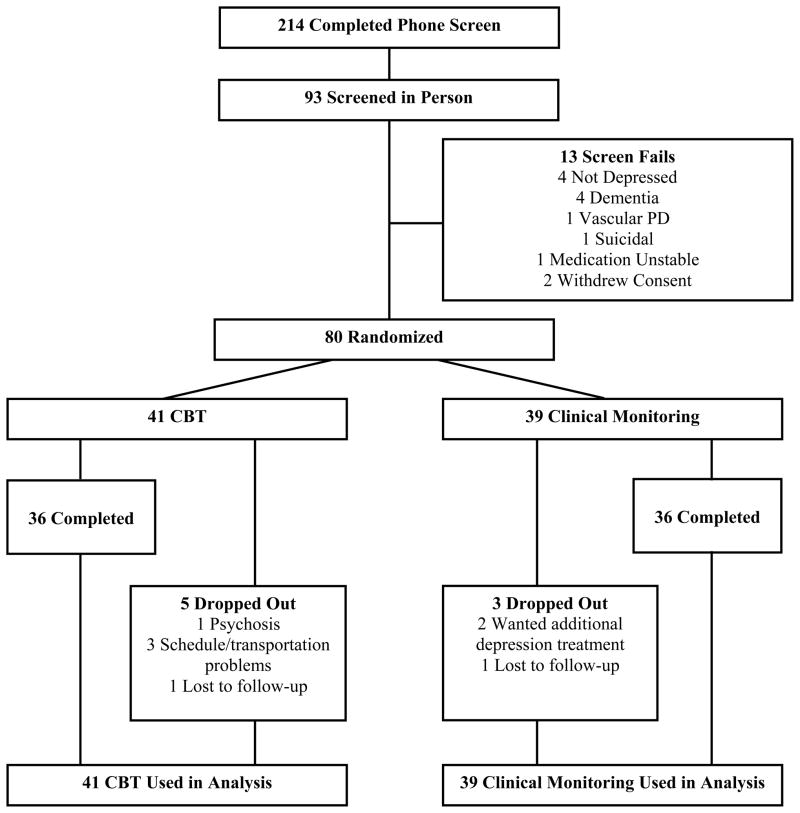
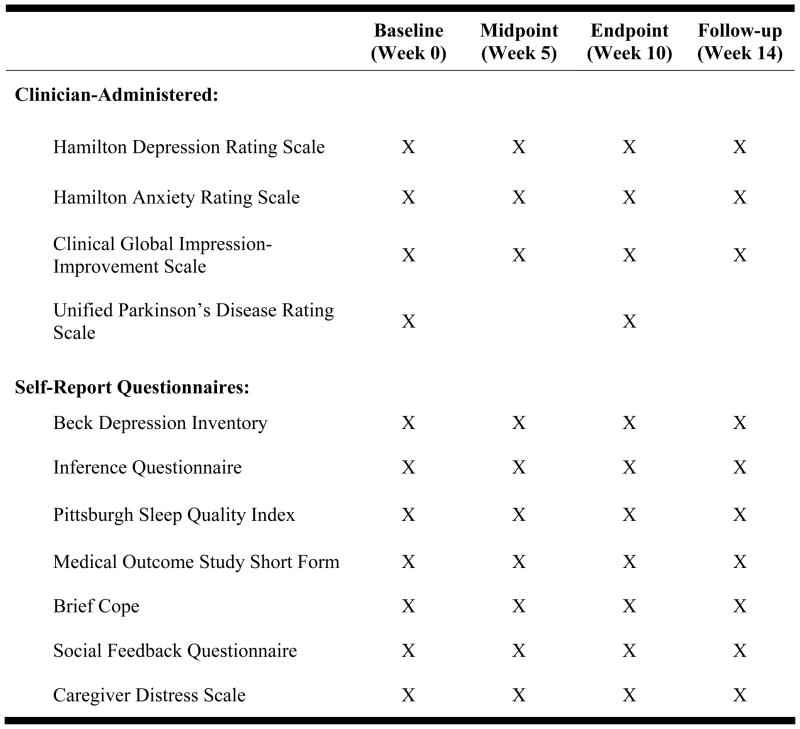
Potential participants called our office to receive information about the study and to complete a preliminary screening (Figure 1). Appropriate individuals were scheduled for a face-to-face appointment, where a statement of informed consent (patient and caregiver) was reviewed and signed, demographic information was obtained, inclusion/exclusion criteria were assessed (RDD, MHM, MM) and baseline evaluations were completed (Figure 2). Those who met eligibility criteria were enrolled and randomized to treatment arm as described above. Participants were re-assessed 5 (midpoint), 10 (end of treatment), and 14 weeks post-randomization (one month follow-up). Phone calls were made at weeks 2 and 7 to assess patient safety.
Figure 1.
Flow of Participants through the Study
Figure 2.
Schedule of Events
Raters received extensive training from the first author (RDD) in SCID, Hamilton Depression Rating Scale [HAM-D-17(28)], and Hamilton Anxiety Rating Scale [HAM-A(29)] administration. Both Hamilton interviews were standardized (by RDD) at the outset of the trial and a coding dictionary was developed to facilitate accurate scoring of patient responses.
Change in the HAM-D-17 total score was the primary outcome. HAM-D inter-rater reliability was >.95 [(intra-class correlation), based on 234 interviews (50 patients), selected by computer generated random numbers]. Secondary outcomes included responder status [defined a priori as depression much improved or very much improved on the Clinical Global Impression-Improvement Scale; CGI-I or ≥ 50% reduction in the baseline HAM-D 17 score (30)], depression [Beck Depression Inventory; BDI (31)], anxiety (HAM-A), negative thoughts [Inference Questionnaire (32)], sleep [Pittsburgh Sleep Quality Index (33)], quality of life [social functioning, physical role limitations, and physical disability subscales of the Medical Outcome Study Short Form (34)], coping [positive reframing and problem-focused subscales of the Brief Cope (35)], social support [Social Feedback Questionnaire (36)], caregiver burden [Caregiver Distress Scale (37)], and Parkinson’s symptom ratings [Unified Parkinson’s Disease Rating Scale total score (38)].
Interventions
CBT
The CBT package employed in this trial was tailored to the unique needs of the Parkinson’s population and is described in detail elsewhere (19,39). In brief, specific modifications included a stronger emphasis on behavioral and anxiety management techniques than traditionally integrated into CBT protocols for depression, and the inclusion of a supplemental caregiver educational program. These changes were intended to address the psychiatric complexity and executive dysfunction that characterize the population.
Patients received 10 weekly individual sessions (60–75 minutes) of manualized CBT. Treatment incorporated exercise, behavioral activation, thought monitoring and restructuring, relaxation training, worry control, and sleep hygiene, and was augmented with 4 separate individual caregiver educational sessions (30–45 minutes), intended to provide caregivers with the skills needed to facilitate patients’ practice of CBT techniques learned in session. For example, caregivers were taught to help patients identify negative thoughts and replace them with more balanced alternatives and were given tools to assist patients complete therapy goals (i.e., exercise, socializing). The primary focus was not to address the caregivers’ own personal concerns. The treatment manual is available by request from RDD.
Therapist training and treatment fidelity
RDD and two doctoral level psychologists (KLB and JF) conducted CBT. Prior to treating study patients, KLB and JF received extensive training in CBT for depression in Parkinson’s disease, which included treating two non-study patients each, with audiotape review of all sessions by RDD (N=40). Throughout the trial, RDD and LAA (an independent expert in CBT in medical populations) reviewed audiotapes from therapy sessions (based on training and supervision needs) and assessed therapist skill and treatment fidelity on the Cognitive Therapy Scale (40), a widely used and validated CBT competence measure [with a score ≥ 40 reflecting proficiency (N= 150; mean = 55.74, SD= 6.52)].
Clinical Monitoring
All patients received close clinical monitoring of their depressive symptoms by study personnel during follow-up phone calls (weeks 2 and 7; 30 minutes each) and evaluations (weeks 5, 10, and 14; 60–90 minutes each). All patients continued on stable treatment regimens under the care of their personal physicians who also monitored their medical and psychiatric status. No new depression treatment (other than CBT in the experimental condition) was provided to study participants.
Statistical Analyses
Data was analyzed using SAS Version 9.1. An intent-to-treat approach was employed in all analyses, which included all 80 randomized patients. The primary outcome (HAM-D change) was evaluated at baseline and weeks 5, 10, and 14 using mixed-models repeated measures analysis of variance (SAS PROC MIXED) with restricted maximum likelihood estimation. Treatment group (CBT, clinical monitoring), assessment point (baseline, weeks 5, 10, and 14), and their interaction were fixed effects. The patient was treated as a random effect. The group-by- time interaction was the fixed effect of interest. Spatial power (a function of the square root of days that a given assessment occurred for a given patient) was used to model the covariance structure for all analyses, as this model yielded the best fit for the data among all covariate structures examined. Gender, block, strata (antidepressant use), and baseline cognition (Dementia Rating Scale total) were examined as covariates. Because there was no significant effect for any of these variables (p>.25), they were removed from the final model.
Responder status was examined separately at weeks 10 and 14 and cross-tabulated with treatment group. The Fisher exact test was used to compare the rate of response between CBT and clinical monitoring. Mixed models analyses (as described above) were used to explore all other secondary outcomes. Because multiple tests capitalize on chance, all p-values for these secondary outcomes were adjusted for multiple tests by the Holm method using permutation-type re-samplings (100,000 re-samples; two-tailed) in SAS PROC MULTTEST (raw p values are not reported). Effect sizes were calculated for all primary and secondary outcomes (Table 2). Planned contrasts to examine changes specific to a particular time point (i.e., week 10) were only conducted if the overall omnibus F test (Table 2) remained significant after adjustment for multiple comparisons. Least squared means are presented in the text and tables.
Table 2.
Outcome Variables
| CBT (n=41) | Clinical Monitoring (n=39) | |||||
|---|---|---|---|---|---|---|
| PRIMARY OUTCOMES | Mean1 (SD) | Mean (SD) | F | p- valuea | Cohen’s d2 | |
| Hamilton Depression Rating Scale b | Baseline | 20.93 (4.56) | 19.38 (4.56) | 30.74 | <.0001 | 1.59 |
| Midpoint | 14.92 (4.73)* | 19.71 (4.56) | ||||
| Endpoint | 13.58 (4.72)* | 19.33 (4.55) | ||||
| Follow-up | 14.52 (4.75)* | 19.31 (4.63) | ||||
|
| ||||||
|
SECONDARY OUTCOMES
| ||||||
| Beck Depression Inventory b | Baseline | 19.18 (7.47) | 19.05 (7.37) | 9.77 | .001 | 1.1 |
| Midpoint | 13.29 (7.59) | 16.33 (7.31) | ||||
| Endpoint | 9.74 (7.40)* | 17.45 (7.17) | ||||
| Follow-up | 11.18 (7.58)* | 16.20 (7.39) | ||||
|
| ||||||
| Hamilton Anxiety Rating Scale b | Baseline | 19.32 (4.41) | 18.49 (4.35) | 11.65 | .001 | .98 |
| Midpoint | 15.41 (4.55)* | 18.88 (4.35) | ||||
| Endpoint | 14.73 (4.54)* | 18.21 (4.35) | ||||
| Follow-up | 15.36 (4.60)* | 18.30 (4.43) | ||||
|
| ||||||
| Unified Parkinson’s Disease Rating Scaleb | Baseline | 45.69 (17.42) | 48.03 (17.21) | 17.51 | .001 | .41 |
| Endpoint | 40.11 (17.73)* | 49.59 (17.28) | ||||
|
| ||||||
| Brief Cope – Positive Reframing c | Baseline | 4.59 (1.63) | 4.23 (1.61) | 4.25 | .05 | .80 |
| Midpoint | 4.82 (1.72) | 4.30 (1.64) | ||||
| Endpoint | 5.78 (1.70)* | 4.09 (1.67) | ||||
| Follow-up | 5.16 (1.75) | 4.33 (1.68) | ||||
|
| ||||||
| Brief Cope – Problem Focused c | Baseline | 15.87 (3.87) | 16.10 (3.84) | 3.32 | .12 | .61 |
| Midpoint | 16.55 (4.05) | 14.86 (3.90) | ||||
| Endpoint | 17.28 (4.01) | 15.14 (3.95) | ||||
| Follow-up | 16.69 (4.11) | 16.20(3.96) | ||||
|
| ||||||
| Medical Outcomes Short-Form Health Survey – Social Functioning c | Baseline | 58.44 (22.05) | 54.17 (21.78) | 5.07 | .02 | .81 |
| Midpoint | 72.30 (23.07)* | 54.13 (22.03) | ||||
| Endpoint | 73.51 (22.82)* | 51.32 (21.71) | ||||
| Follow-up | 70.92 (23.34)* | 53.64 (22.37) | ||||
|
| ||||||
| Medical Outcomes Short-Form Health Survey – Physical Disability c | Baseline | 54.00 (27.46) | 49.30 (27.12) | 2.60 | .27 | .31 |
| Midpoint | 55.13 (28.26) | 51.73 (27.28) | ||||
| Endpoint | 63.15 (27.99) | 49.89 (27.08) | ||||
| Follow-up | 54.84 (28.32) | 48.00 (27.49) | ||||
|
| ||||||
| Medical Outcomes Short-Form Health Survey – Physical Role Limitations c | Baseline | 23.75 (33.18) | 21.80 (32.77) | 3.43 | .12 | .58 |
| Midpoint | 40.99 (34.95) | 17.47 (33.35) | ||||
| Endpoint | 37.54 (34.50) | 16.42 (32.73) | ||||
| Follow-up | 32.45 (35.59) | 24.86 (33.96) | ||||
|
| ||||||
| Social Feedback Questionnaire b | Baseline | 4.68 (4.25) | 5.54 (4.20) | 1.33 | .60 | .01 |
| Midpoint | 3.77 (4.47) | 4.83 (4.25) | ||||
| Endpoint | 4.05 (4.40) | 4.62 (4.20) | ||||
| Follow-up | 4.18 (4.50) | 6.42 (4.32) | ||||
|
| ||||||
| Pittsburgh Sleep Quality Index b | Baseline | 10.93 (4.02) | 11.20 (4.02) | 1.06 | .60 | .24 |
| Midpoint | 9.92 (4.20) | 11.10 (4.06) | ||||
| Endpoint | 9.56 (4.14) | 10.82 (4.09) | ||||
| Follow-up | 10.16 (4.24) | 10.31 (4.11) | ||||
|
| ||||||
| Inference Questionnaire b | Baseline | 6.92 (3.41) | 6.92 (3.37) | .63 | .60 | .35 |
| Midpoint | 6.00 (3.70) | 6.65 (3.50) | ||||
| Endpoint | 4.97 (3.56) | 6.19 (3.38) | ||||
| Follow-up | 5.57 (3.64) | 6.37 (3.50) | ||||
|
| ||||||
| Caregiver Distress Scale b | Baseline | 24.26 (14.88) | 22.45 (14.88) | 1.31 | .60 | .21 |
| Midpoint | 23.24 (15.61) | 20.92 (15.43) | ||||
| Endpoint | 21.08 (15.34) | 22.41 (15.20) | ||||
| Follow-up | 20.92 (15.71) | 21.34 (15.41) | ||||
Least squares means are presented.
Cohen’s d is calculated for the acute treatment period of baseline to endpoint.
All p values for secondary outcomes have been adjusted by the HOLM Method.
Lower scores reflect improvement.
Higher scores reflect improvement.
Change significant from baseline at p ≤.001
Sample size was determined a priori based on power analyses. Power calculations were based on the HAM-D 17, setting alpha at 0.05, power at 0.80, a predicted effect size of d = 0.70 [based on past CBT pilot work in Parkinson’s disease conducted by RDD (19) and published literature regarding CBT for depression (41)], and the potential for 20% attrition. These parameters indicated that 40 patients per group were needed to obtain the desired effect.
Results
Eighty patients with Parkinson’s disease and their caregivers were enrolled. Forty-one patients (51%) were randomized to CBT and 39 (49%) to clinical monitoring. Ninety percent of patients (N=72) completed the study (Figure 1). The mean number of CBT sessions attended was 9.17 (median and mode of 10). The mean number of caregiver sessions completed was 2.90 (median and mode of 4). Forty- three patients (54%) were taking a stable dose of antidepressant medication at baseline and reported compliance with their prescribed regimen throughout the trial. See Table 1 for a breakdown of baseline clinical and demographic information.
Table 1.
Baseline Demographic and Clinical Information
| Total (N = 80) | CBT (n = 41) | Clinical Monitoring (n = 39) | pavalue | |
|---|---|---|---|---|
| Genderb | .86 | |||
| Male | 48 (60%) | 25 (61%) | 23 (59%) | |
| Female | 32 (40%) | 16 (39%) | 16 (41%) | |
|
| ||||
| Agec | 64.56 (10.53) | 63.73 (9.89) | 65.44 (11.23) | .47 |
|
| ||||
| Parkinson’s Disease Duration (years) | 6.34 (5.51) | 6.53 (5.53) | 6.13 (5.56) | .74 |
|
| ||||
| Age of Parkinson’s Disease Onset | 58.21 (11.78) | 57.12 (11.22) | 59.36 (12.39) | .40 |
|
| ||||
| Depression Duration (current episode; years) | 2.84 (3.06) | 3.13 (3.36) | 2.54 (2.72) | .39 |
|
| ||||
| Primary DSM-IV Diagnosis | ||||
| Major Depressive Disorder | 65 (81%) | 33 (81%) | 32 (82%) | .74 |
| Dysthymia | 8 (10%) | 5 (12%) | 3 (8%) | |
| Depression Not Otherwise Specified | 7 (9%) | 3 (7%) | 4 (10%) | |
|
| ||||
| Comorbid Anxiety Disorder | 45 (56.3%) | 26 (63%) | 19 (49%) | .19 |
|
| ||||
| Antidepressant Used | 43 (54%) | 22 (54%) | 21 (54%) | .99 |
|
| ||||
| Clinical Global Impression Scale – Severity | 4.41 (.57) | 4.44 (.63) | 4.38 (.49) | .67 |
|
| ||||
| Hamilton Depression Rating Scale Score | 20.18 (4.27) | 20.93 (4.56) | 19.38 (4.56) | .11 |
|
| ||||
| Beck Depression Inventory Score | 19.30 (7.97) | 19.18 (7.47) | 19.05 (7.37) | .90 |
|
| ||||
| Hamilton Anxiety Rating Scale Score | 18.95 (4.33) | 19.32 (4.41) | 18.49 (4.35) | .36 |
|
| ||||
| Dementia Rating Scale Score | 138.24 (4.9) | 139.44 (3.8) | 136.97 (5.5) | .02* |
|
| ||||
| Parkinson’s Disease Stage (Hoehn and Yahr) | 2.14 (0.77) | 2.12 (0.90) | 2.16 (0.83) | .81 |
|
| ||||
| Race | ||||
| White | 74 (93%) | 38 (93%) | 36 (91%) | .39 |
| Black | 1 (1%) | 0 (0%) | 1 (3%) | |
| Asian | 4 (5%) | 3 (7%) | 1 (3%) | |
| Pacific Islander | 1 (1%) | 0 (0%) | 1 (3%) | |
|
| ||||
| Ethnicity | .57 | |||
| Hispanic | 3 (4%) | 2 (5%) | 1 (3%) | |
| Non-Hispanic | 77 (96%) | 39 (95%) | 38 (97%) | |
|
| ||||
| Marital Status | .28 | |||
| Married | 57 (71%) | 32 (78%) | 25 (64%) | |
| Divorced | 12 (12%) | 6 (15%) | 6 (15%) | |
| Widowed | 9 (11%) | 3 (7%) | 6 (16%) | |
| Never Married | 2 (3%) | 0 (0%) | 2 (5%) | |
|
| ||||
| Education | .60 | |||
| High School Diploma | 12 (15%) | 7 (17%) | 5 (13%) | |
| Some College | 14 (17%) | 7 (17%) | 7 (17%) | |
| College Degree | 19 (24%) | 7 (17%) | 12 (31%) | |
| Graduate Degree | 35 (44%) | 20 (49%) | 15 (39%) | |
|
| ||||
| Receiving Disability | 27 (34%) | 16 (39%) | 11 (28%) | .31 |
|
| ||||
| # Comorbid Medical Conditions | 2.50 (1.81) | 2.20 (1.55) | 2.82 (2.02) | .13 |
|
| ||||
| # Current Axis I Diagnoses | 1.80 (0.92) | 1.88 (0.81) | 1.72 (1.03) | .44 |
|
| ||||
| # Parkinson’s Disease Medications | 1.75 (1.04) | 1.80 (1.23) | 1.69 (0.80) | .63 |
|
| ||||
| # Psychotropic Medications | 1.25 (1.15) | 1.20 (1.15) | 1.31 (1.17) | .67 |
|
| ||||
| # Total Medications | 7.64 (3.99) | 7.17 (3.40) | 8.13 (4.53) | .29 |
|
| ||||
| # Past Depression Med Trials | 1.29 (1.67) | 1.17 (1.36) | 1.41 (1.96) | .53 |
|
| ||||
| Deep Brain Stimulation | 3 (4%) | 2 (5%) | 1 (3%) | .59 |
|
| ||||
| History of Psychotherapy | 50 (62%) | 27 (66%) | 23 (59%) | .53 |
|
| ||||
| Current Supportive Counseling | 7 (9%) | 3 (7%) | 4 (10%) | .64 |
|
| ||||
| Time (weeks) to Week 10 Evaluation | 11.79 (2.75) | 11.70 (3.40) | 11.90 (1.87) | .76 |
|
| ||||
| Time (weeks) to Week 14 Evaluation | 15.90 (4.03) | 15.74 (4.85) | 16.08 (3.00) | .71 |
CBT and Clinical Monitoring were compared at baseline on relevant demographic and clinical variables to check for group equivalence with t or χ2 tests as appropriate.
A nominal baseline difference was observed on the Dementia Rating Scale total score. No significant differences emerged on any other variable. Baseline Dementia Rating Scale score was added as a covariate in the analysis of primary outcome. The Dementia Rating Scale was not a significant covariate (p=.48) and thus removed from the final analysis.
N’s and % are presented for categorical variables.
Means and standard deviations are presented for continuous variables.
For those taking antidepressant medications, the average length of treatment on the stable regimen was 2 years and this did not differ between treatment groups (p=.60).
Overall Treatment-by-Time Effects
Primary Outcome
The CBT group reported significantly greater reductions in depression (HAM-D 17) vs. clinical monitoring F (3,215) = 30.74, P<.0001.
Secondary Outcomes
Notable effects were also observed on depression [BDI: F(3,210)=9.77, P=.001)], anxiety [F(3,214)=11.65, P=.001], social functioning [F (3,209)= 5.07, P=.02], positive reframing [F (3,204)=4.25, P=.05], and Parkinson’s symptom ratings [F(1,68)=17.51, P=.001] for those receiving CBT vs. clinical monitoring (Table 2). No significant group-by-time improvements were noted for sleep, inferences, problem-focused coping, physical disability, physical role limitations, social support, or caregiver burden.
End of Treatment (week 10)
Primary Outcome
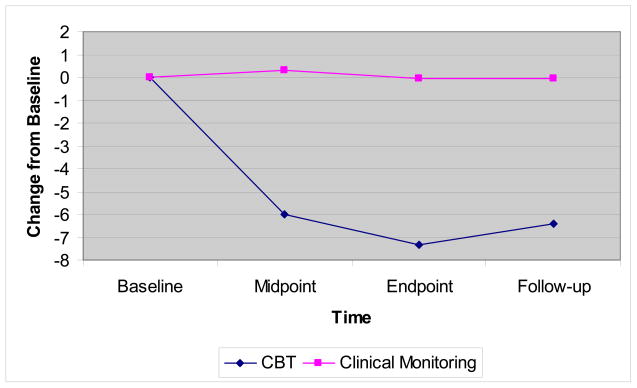
The mean HAM-D score was 13.58 [95% CI: 12.12 –15.03] for CBT and 19.33 [95% CI: 17.89–20.77] for clinical monitoring (Table 2). Mean change from baseline was 7.35 for CBT vs. 0.05 for clinical monitoring [F( 1,215)=76.34, P<.0001; Cohen’s d=1.59; Figure 3].
Figure 3.
Hamilton Depression Rating Scale
Secondary Outcomes
The mean BDI score was 9.74 [95% CI: 7.46–12.02] for CBT vs. 17.45 for clinical monitoring [95% CI: 15.19–19.72]. Mean change from baseline was 9.44 for CBT and 1.60 for clinical monitoring [F( 1,210)=27.25, P<.0001; Cohen’s d=1.1]. Significant improvements were also observed on anxiety [F (1,214)=25.83, P<.0001], social functioning [F (1,209)= 14.27, P<.001], and positive reframing [F(1,204)= 10.69, P=.001] for CBT vs. clinical monitoring (Table 2). While there was no significant group-by-time interaction on negative inferences, exploratory analyses suggested that treatment responders exhibited greater decreases in negative thoughts than non-responders F( 2,77)=4.70, P=.01.
Moreover, exploratory subscale analysis of the Unified Parkinson’s Disease Rating Scale (significant group-by-time effect noted above for the total score) indicated change for mood [F(1,68)= 39.75, P<.001] and motor functioning [F(1,68)=5.90, P=.02] favoring CBT. Specifically, the mean motor score was 21.10 for CBT [95% CI: 17.95–24.26] and 25.38 [95% CI: 22.26–28.49] for clinical monitoring. Mean motor change was 1.11 (improvement) for CBT vs. −2.16 (worsening) for clinical monitoring.
One-month follow-up (week 14)
Planned contrasts (baseline to week 14) demonstrated that improvements in depression [HAMD: F( 1,215)=55.62, P<.0001; BDI: F( 1,210)=11.14, P=.001], anxiety [F (1,214)=18.88, P<.0001], and social functioning [F (1,209)= 7.09, P=.008] were maintained at follow-up (Table 2). Treatment responders continued to exhibit larger decreases in negative thoughts than non-responders F(3,76)=3.04, P=.03. Parkinson’s symptom ratings were not conducted at week 14.
Treatment Response
At week 10, 23/41 (56%) patients receiving CBT and 3/39 (8%) receiving clinical monitoring met criteria for treatment response (Fisher’s exact P <.0001). At week 14, 21 patients in the CBT group (51%) and 0 patients in the clinical monitoring group (0%) met criteria for response (Fisher’s exact P<.0001).
Number Needed to Treat
The number needed to treat based on responders for CBT vs. clinical monitoring was 2.1, with an absolute risk reduction of 48%.
Discussion
The results of this first randomized controlled trial suggest that CBT may be a feasible and possibly efficacious approach to treating depression in Parkinson’s disease. Ninety-percent of the sample completed the study and 88% of patients randomized to CBT attended all 10 treatment sessions. CBT was associated with significant improvements on all clinician-rated and self-report measures of depression. Gains were observed by the end of treatment (week 10) and maintained during follow-up (week 14). Effect sizes were large for both the HAM-D (1.59) and BDI (1.1). Response rates favored CBT at weeks 10 (56% vs. 8%) and 14 (51% vs. 0%).
The CBT group also reported greater improvements in quality of life, coping, and anxiety, as well as less motor decline. These results underscore several points. First, CBT patients reported less avoidance of and greater enjoyment from social activities, as well as the use of positive reframing as a coping strategy in response to daily stress. Second, treatment effects may generalize to the negative thoughts and avoidance behaviors that maintain anxiety. Third, the incorporation of anxiety management strategies, such as worry control and relaxation, into a CBT program for primary depression in Parkinson’s disease may be useful. Lastly, consistent with previous findings, sub-optimally treated depression may accelerate Parkinson’s-related physical disability (7,42).
While there was no significant group by time interaction on inferences, treatment responders exhibited larger decreases in negative thinking compared to nonresponders. Since negative thoughts are a primary target of CBT, it follows that people who did not “respond” to treatment would not exhibit changes in thinking patterns. Despite moderate effect sizes, the impact of CBT on problem-focused coping and perceptions of role-limitations and physical disability were no longer significant after controlling for multiple comparisons. CBT also had no substantial effects on sleep, social support, or caregiver burden.
There are no controlled trials of CBT for depression in Parkinson’s disease with which to compare these results. However, completion rates, response rates, and effect sizes are comparable to those observed in randomized trials of CBT in other populations (41). For example, the literature suggests that the average effect size of CBT for depression vs. a similar comparison condition to the one utilized in this study (i.e., no new treatment) is .67 (41). Thus, this initial randomized-controlled trial offers preliminary data to suggest that the beneficial effects of CBT observed in other patient groups might not be attenuated by the disease process (i.e., neurodegeneration, neurotransmitter changes, dysfunction in brain regions/pathways).
This study also has several limitations related to the interpretation of efficacy. First, the study design did not include an attention-matched control or alternative psychosocial intervention. Although the additive approach and comparison condition employed did control for threats to internal validity (i.e., time, spontaneous remission, regression to the mean, history, effects of repeated testing) and are appropriate for use in early phase psychotherapy trials (23, 43), the role of non-specific factors, such as the increased attention and social contact received by the CBT group, cannot be adequately explored. It is also not possible to isolate which aspects of the CBT package (e.g., caregiver sessions, exercise) were most helpful. Related to this, we cannot rule out the placebo effect as a partial explanation for differences between groups. However, several factors make this explanation less likely. Throughout the trial, it was emphasized that the impact of both study treatments (CBT and clinical monitoring) on depression in Parkinson’s disease was not yet known and that there may not be any personal benefit from participation. Additionally, the chronic nature of depression in the sample, progressive nature of Parkinson’s disease (i.e., not an acute stressor), durability of CBT gains exhibited over 14 weeks, changes in negative cognition that accompanied treatment response, minimal improvement observed in the clinical monitoring condition, and comparability of results to CBT trials in other populations suggests that the impact of CBT may be larger than that which can be explained by placebo response alone. Of note, a CBT effect size of .75 is obtained when comparing CBT data from this study to pill placebo data from our own recent double-blind placebo-controlled antidepressant trial for depression in Parkinson’s disease (10).
Second, despite an average reduction of 7.35 points, the mean HAM-D score of 13.58 for the CBT group at week 10 still reflects moderate depressive symptoms. This finding may in part be due to the high rate of somatic complaints experienced by Parkinson’s patients, independent of depression, as well as the inclusive scoring approach employed (44). For example, all reported symptoms were counted towards HAM-D ratings despite potential overlap with the physical symptoms of Parkinson’s disease (i.e., psychomotor slowing, fatigue). Importantly, the BDI emphasizes cognitive symptoms of depression (i.e., guilt, hopelessness) and the week 10 BDI score of 9.7 for the CBT group indicates minimal symptoms of depression. Third, given the psychiatric comorbidity in the sample and the inclusion of two anxiety management modules in the CBT package, it is possible that reduced anxiety could have influenced depression treatment response. Because the depression effect remained robust (P<.0001) when controlling for HAM-A change (exploratory analyses), it is unlikely that improved anxiety was a main mechanism of action. Fourth, motor functioning results warrant prudent interpretation. Although the group-by-time interaction on motor scores at week 10 was statistically significant, the effect size was small (.13) and may be an artifact of the sample.
It is also necessary to acknowledge that our results may not generalize to those with more advanced stage disease, severe depression, dementia, sub-optimal social supports, inability to travel to weekly therapy, and limited access to specialized mental health resources. In addition, we could not explore the longer-term durability of treatment gains because the follow-up period was limited to one-month for ethical reasons (protocol restrictions regarding changing depression treatment). Lastly, treatment side effects were not assessed prospectively. Collectively, these limitations suggest that the results should be viewed as a preliminary first step in the establishment of an evidence base for CBT in Parkinson’s disease.
The precise cause of depression in Parkinson’s disease is unclear, with both biological and psychosocial factors implicated in its onset and maintenance (45). As a whole, the results of this trial suggest that cognitive behavior therapy for depression in patients with Parkinson’s disease may be beneficial, independent of etiology. Further research is needed to replicate and extend these findings.
Acknowledgments
This study was funded by 1 K23 NS052155-01A2 awarded to Dr. Dobkin by the National Institute of Neurological Disorders and Stroke (NIH/NINDS). The full trial protocol can be assessed by contacting Dr. Dobkin at dobkinro@umdnj.edu. This trial is registered at clinicaltrials.gov: Identifier NCT00464464.
We would like to thank Dr. Laura Marsh for her feedback on the revised version of this manuscript.
Role of the Sponsor: The NINDS had no role in design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. The content is solely the responsibility of the authors and does not represent the views of the NINDS, NIH, or Robert Wood Johnson Medical School.
Footnotes
Trial Registration: clinicaltrials.gov Identifier: NCT004644
Financial Disclosure: Dr. Dobkin has research support from the NIH/NINDS. Dr. Menza has had research support from NIH/NINDS, Astra-Zeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Forest Laboratories, GlaxoSmithKline, Lilly, Pfizer, Sanofi-Aventis, Sepracor, Takeda, and Wyeth, has been a consultant to the National Institutes of Health (NIMH/NINDS), GlaxoSmithKline, Kyowa, Lilly Research Laboratories, Pfizer, Sepracor, and Takeda, and has been a speaker for Sanofi-Aventis. Dr. Allen has had research support from NIMH and Sepracor. Dr. Gara has research support from NIMH. Dr. Mark has had research support from NIH/NINDS, Kyowa, Cephalon, and has been a speaker for Allergan, Boehringer Ingelheim, GlaxoSmithKline and Valeant. Dr. Bienfait was a postdoctoral fellow at RWJMS (2007–2009) when she worked on this project. Upon the completion of her fellowship, she accepted a position with Merck, where she is currently employed. Ms. Tiu and Dr. Friedman have no financial interests to disclose.
Author Contributions: Dr. Dobkin had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
Study Concept and Design: Dobkin, Menza, Allen, Gara, Mark
Acquisition of Data: Dobkin, Tiu, Bienfait, Friedman, Mark
Analysis and Interpretation of Data: Dobkin, Gara, Menza, Allen
Drafting of the Manuscript: Dobkin, Tiu
Critical Revision of the Manuscript for important intellectual content: Dobkin, Menza, Allen, Gara, Mark, Friedman, Bienfait
Statistical Analysis: Dobkin, Gara
Obtaining Funding: Dobkin, Menza
Administration, technical, or material support: Menza, Tiu, Bienfait, Friedman
Study Supervision: Dobkin, Allen, Mark, Menza
References
- 1.Kulisevsky J, Pagonabarraga J, Pascual-Sedano B, Garcia-Sanchez C, Gironell A. Prevalence and correlates of neuropsychiatric symptoms in Parkinson’s disease without dementia. Mov Disord. 2008;23:1889–1896. doi: 10.1002/mds.22246. [DOI] [PubMed] [Google Scholar]
- 2.Forsaa EB, Larsen JP, Wentzel-Larsen T, Herlofson K, Alves G. Predictors and course of health-related quality of life in Parkinson’s disease. Mov Disord. 2008;23:1420–1427. doi: 10.1002/mds.22121. [DOI] [PubMed] [Google Scholar]
- 3.Cummings JL. Depression and Parkinson’s disease. Am J Psychiatry. 1992;149:443–454. doi: 10.1176/ajp.149.4.443. [DOI] [PubMed] [Google Scholar]
- 4.Reijnders MA, Ehrt U, Weber WEJ, Aarsland D, Leentjens AF. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov Disord. 2008;23(2):183–189. doi: 10.1002/mds.21803. [DOI] [PubMed] [Google Scholar]
- 5.Menza MA, Robertson-Hoffmann DE, Bonapace AS. Parkinson’s disease and anxiety: comorbidity with depression. Biol Psychiatry. 1993;34:465–470. doi: 10.1016/0006-3223(93)90237-8. [DOI] [PubMed] [Google Scholar]
- 6.Santangelo G, Vitale C, Trojano L, Longo K, Cozzolino A, Grossi D, Barone P. Relationship between depression and cognitive dysfunctions in Parkinson’s disease without dementia. J Neurol. 2009;256(4):632–8. doi: 10.1007/s00415-009-0146-5. [DOI] [PubMed] [Google Scholar]
- 7.Starkstein SE, Mayberg HS, Leiguarda R, Preziosi TJ, Robinson RG. A prospective longitudinal study of depression, cognitive decline, and physical impairments in patients with Parkinson’s disease. J Neural Neurosurg Psychiatry. 1992;55:377–382. doi: 10.1136/jnnp.55.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Global Parkinson’s Disease Survey (GPDS) Steering Committee. Factors impacting on quality of life in Parkinson’s disease: results from an international survey. Mov Disord. 2002;17:60–67. doi: 10.1002/mds.10010. [DOI] [PubMed] [Google Scholar]
- 9.Martinez-Martin P, Forjaz MJ, Frades-Payo B, Rusiñol AB, Fernández-García JM, Benito-León J, Arillo VC, Barberá MA, Sordo MP, Catalán MJ. Caregiver burden in Parkinson’s disease. Mov Disord. 2007;22(7):924–931. doi: 10.1002/mds.21355. [DOI] [PubMed] [Google Scholar]
- 10.Menza M, Dobkin RD, Marin H, Mark MH, Gara M, Buyske S, Bienfait K, Dicke A. A controlled trial of antidepressants in patients with Parkinson’s disease and depression. Neurology. 2009;72:886–892. doi: 10.1212/01.wnl.0000336340.89821.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devos D, Dujardin K, Poirot I, Moreau C, Cottencin O, Thomas P, Destee A, Bordet R, Defebvre L. Comparison of Desipramine and Citalopram Treatments for Depression in Parkinson’s disease: A Double-Blind, Randomized Placebo Controlled Study. Mov Disord. 2008;23(6):850–857. doi: 10.1002/mds.21966. [DOI] [PubMed] [Google Scholar]
- 12.Barone P, Poewe W, Albrecht S, Debieuvre C, Massey D, Rascol O, Tolosa E, Weintraub D. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(6):573–580. doi: 10.1016/S1474-4422(10)70106-X. [DOI] [PubMed] [Google Scholar]
- 13.da Silva TM, Munhoz RP, Alvarez C, Naliwaiko K, Kiss A, Andreatini R, Ferraz AC. Depression in Parkinson’s disease: A double-blind, randomized, placebo-controlled study of omega 3 fatty acid supplementation. J Affect Disord. 2008;111(2-3):351–9. doi: 10.1016/j.jad.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Serfaty MA, Haworth D, Blanchard M, Buszewicz M, Murad S, King M. Clinical Effectiveness of Individual Cognitive Behavioral Therapy for Depressed Older People in Primary Care. Arch Gen Psychiatry. 2009;66 (12):1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 15.Mohr DC, Likosky W, Bertagnolli A, Goodkin DE, Van Der Wende J, Dwyer P, Dick LP. Telephone-administered cognitive-behavioral therapy for the treatment of depressive symptoms in multiple sclerosis. J Consult Clin Psychol. 2000;68(2):356–361. doi: 10.1037//0022-006x.68.2.356. [DOI] [PubMed] [Google Scholar]
- 16.Veazey C, Cook KF, Stanley M, Lai EC, Kunik ME. Telephone-administered cognitive behavioral therapy: a case study of anxiety and depression in Parkinson’s disease. J Clin Psychol in Med Settings. 2009;16(3):243–253. doi: 10.1007/s10880-009-9167-6. [DOI] [PubMed] [Google Scholar]
- 17.Feeney F, Egan S, Gasson N. Treatment of depression and anxiety in Parkinson’s disease: a pilot study using group cognitive behavioural therapy. Clin Psychol. 2005;9:31–38. [Google Scholar]
- 18.Cole K, Vaughan FL. Brief cognitive-behavioral therapy for depression associated with Parkinson’s disease: a single case series. Behav Cogn Psychother. 2005;33:89–102. [Google Scholar]
- 19.Dobkin RD, Allen LA, Menza M. Cognitive behavior therapy for depression in Parkinson’s disease: A pilot study. Mov Disord. 2007;22(7):946–952. doi: 10.1002/mds.21455. [DOI] [PubMed] [Google Scholar]
- 20.Dreising H, Beckmann J, Wermuth L, Skovlund S, Bech P. Psychologic effects of structured cognitive psychotherapy in young patients with Parkinson’s disease: a pilot study. Nordic J Psychiatry. 1999;53:217–221. [Google Scholar]
- 21.Farabaugh A, Locascio JJ, Yap L, Growdon J, Fava M, Crawford C, Matthews J, McCutchen J, Bunchin J, Pava J, Alpert JE. Cognitive-behavioral therapy for patients with Parkinson’s disease and comorbid major depressive disorder. Psychosomatics. 2010;51(2):124–129. doi: 10.1176/appi.psy.51.2.124. [DOI] [PubMed] [Google Scholar]
- 22.Hollon SD, Jarrett RB, Nierenberg AA, Thase ME, Trivedi M, Rush AH. Psychotherapy and medication in the treatment of adult and geriatric depression: which monotherapy or combined treatment? J Clin Psychiatry. 2005;66:455–468. doi: 10.4088/jcp.v66n0408. [DOI] [PubMed] [Google Scholar]
- 23.Borkovec T, Sibrava NJ. Psychotherapy research, suggested alternatives, and some strategies for the pursuit of the placebo phenomenon. J Clin Psychol. 2005;61:805–818. doi: 10.1002/jclp.20127. [DOI] [PubMed] [Google Scholar]
- 24.Gelb DG, Oliver E, Gilman S. Diagnostic criteria for Parkinson’s disease. Arch Neurol. 1999;56:33–39. doi: 10.1001/archneur.56.1.33. [DOI] [PubMed] [Google Scholar]
- 25.Guy W. ECDEU assessment manual for psychopharmacology. Washington, DC: U.S. Department of Health, Education, and Welfare; 1976. [Google Scholar]
- 26.Marsh L, McDonald WM, Cummings J, Ravina B NINDS/NIMH Work Group on Depression and Parkinson’s Disease. Provisional Diagnostic Criteria for Depression in Parkinson’s Disease: Report of an NINDS/NIMH Work Group. Mov Disor. 2006;21(2):148–58. doi: 10.1002/mds.20723. [DOI] [PubMed] [Google Scholar]
- 27.Mattis S. Dementia Rating Scale. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- 28.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamilton M. The assessment of anxiety status by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 30.Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer, Lavori PW, Rush AJ, Weisman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Arch Gen Psych. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford; 1979. [Google Scholar]
- 32.Alloy LB, Abramson LY. The Temple-Wisconsin Cognitive Vulnerability to Depression (CVD) Project: Conceptual background, design, and methods. J Cogn Psychother. 1999;13:227–262. [Google Scholar]
- 33.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Research and Practice. J Psychiatr Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36) Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 35.Carver CS. You want to measure coping but your protocol is too long: Consider the brief cope. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 36.Dobkin RD, Panzarella C, Alloy LB, Cascardi M, Truesdell K, Gara M. Assessing an interpersonal- cognitive risk factor for depression: Preliminary validation of the social feedback questionnaire. J Soc Pers Relat. 2007;24(5):765–780. [Google Scholar]
- 37.Cousins R, Davies ADM, Turnball CJ, Playfer JR. Assessing caregiver distress: A conceptual analysis and brief scale. Br J Clin Psychol. 2002;41(4):387–403. doi: 10.1348/014466502760387506. [DOI] [PubMed] [Google Scholar]
- 38.Fahn S, Elton RL. Members of the UPDRS development committee. Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, editors. Recent developments in Parkinson’s disease. Vol. 2. Florham Park (NJ): Macmillan Health Care Information; 1987. pp. 53–64. [Google Scholar]
- 39.Dobkin RD, Menza M, Bienfait KL. CBT for the treatment of depression in Parkinson’s disease: A promising non-pharmacological approach. Expert Rev Neurother. 2008;8(1):27–35. doi: 10.1586/14737175.8.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Young J, Beck AT. Cognitive Therapy Rating Scale Manual. 1980. [Google Scholar]
- 41.Driessen E, Hollon SD. Cognitive Behavioral Therapy for Mood Disorders: Efficacy, Moderators, and Mediators. Psychiatr Clin N Am. 2010;33:537–555. doi: 10.1016/j.psc.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marsh L, Williams JR. Effect of depression remission status on physical disability in Parkinson’s disease: longitudinal cohort study. Mov Disord. 2007;22(12):XIV–XV. (Abstract) [Google Scholar]
- 43.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, Ockene J, Kaplan R. The Selection and Design of Control Conditions for Randomized Controlled Trials of Psychological Interventions. Psychother Psychosom. 2009;78:275–284. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- 44.Schrag A, Barone P, Brown RG, Leentjens AFG, McDonald WM, Starkstein S, Weintraub D, Poewe W, Rascol O, Sampaio C, Stebbins GT, Goetz CG. Depression Rating Scales in Parkinson’s disease: Critique and Recommendations. Mov Disord. 2007;22(8):1077–1092. doi: 10.1002/mds.21333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weintraub D, Stern MB. Psychiatric Complications in Parkinson’s disease. Am J Geriatr Psychiatry. 2005;13(10):844–51. doi: 10.1176/appi.ajgp.13.10.844. [DOI] [PubMed] [Google Scholar]