Abstract
Purpose
Despite initial sensitivity to chemotherapy, ovarian cancers (OVCA) often develop drug-resistance, which limits patient survival. Using specimens and/or genomic data from 289 patients and a panel of cancer cell lines, we explored genome-wide expression changes that underlie the evolution of OVCA chemo-resistance and characterized the BCL2 antagonist of cell death (BAD) apoptosis pathway as a determinant of chemo-sensitivity and patient survival.
Experimental Design
Serial OVCA cell cisplatin treatments were performed in parallel with measurements of genome-wide expression changes. Pathway analysis was performed on genes associated with increasing cisplatin-resistance (EC50). BAD-pathway expression and BAD-protein phosphorylation were evaluated in patient samples and cell lines as determinants of chemo-sensitivity and/or clinical outcome and as therapeutic targets.
Results
Induced in vitro OVCA cisplatin-resistance was associated with BAD-pathway expression (P < 0.001). In OVCA cell lines and primary specimens, BAD-protein phosphorylation was associated with platinum-resistance (n = 147, P < 0.0001) and also with overall patient survival (n = 134, P = 0.0007). Targeted modulation of BAD-phosphorylation levels influenced cisplatin sensitivity. A 47-gene BAD-pathway score was associated with in vitro phosphorylated-BAD levels and with survival in 142 patients with advanced-stage (III/IV) serous OVCA. Integration of BAD-phosphorylation or BAD-pathway score with OVCA surgical cytoreductive status was significantly associated with overall survival by log-rank test (P = 0.004 and <0.0001, respectively).
Conclusion
The BAD apoptosis pathway influences OVCA chemo-sensitivity and overall survival, likely via modulation of BAD-phosphorylation. The pathway has clinical relevance as a biomarker of therapeutic response, patient survival, and as a promising therapeutic target.
Keywords: BAD apoptosis pathway, survival, ovarian cancer, principal component analysis, cisplatin
INTRODUCTION
The development of chemoresistance dramatically affects survival for patients with ovarian cancer (OVCA); thus, targeted therapies that increase chemosensitivity offer the potential to significantly improve outcome. Although most patients with OVCA demonstrate remarkable sensitivity to platinum-based chemotherapy during primary therapy, these patients eventually develop platinum-resistant, recurrent disease (1, 2). Once platinum-resistance has developed, few active therapeutic options exist, and patient survival is generally short-lived (3). In this context, platinum-resistance is frequently viewed as a surrogate clinical marker for more generic chemoresistance, and defining the molecular changes that drive the evolution of the platinum-resistant phenotype could contribute to a broader understanding of human cancer chemoresistance. Changes in cellular drug efflux, increased cellular glutathione levels, increased DNA repair, and drug tolerance have all been shown to contribute to platinum resistance (4–6). More recently, genomic studies have defined gene expression signatures that may discriminate between cancers that are innately chemosensitive versus those that are chemoresistant (7–9). However, the genome-wide expression changes associated with the transition of an OVCA cell from chemosensitive to chemoresistant are less clear, and the discrete biologic pathways that drive the process are unknown. Moreover, how these pathways influence clinical outcomes and their potential as therapeutic targets remain to be defined.
In this study, we tracked the genome-wide expression changes associated with the evolution of in vitro cisplatin-resistance. In doing so, we identified a pathway that appears to have a pivotal and wide-ranging influence on human cancer chemosensitivity, likely via phosphorylation of a key apoptotic protein. We evaluated the BCL2 antagonist of cell death (BAD) apoptosis pathway and phospho-protein in OVCA cell lines and patient samples/datasets 1) as a potential biomarker of chemotherapy response and overall survival and 2) as a therapeutic target to reverse OVCA chemoresistance.
METHODS
Overview
A panel of OVCA cell lines was subjected to serial cisplatin-treatment, and induced cisplatin-resistance was quantified. In parallel, genome-wide expression changes were measured, and genes with expression correlating with increasing cisplatin-resistance were analyzed for representation of biologic pathways. In light of the association between cisplatin-resistance and expression of BAD-pathway kinases and phosphatases, we measured levels of phosphorylated BAD (pBAD) protein in both treated cell lines and chemosensitive and chemoresistant OVCA patient samples. BAD phosphorylation status was modified in vitro using targeted siRNA and phosphorylation-site mutagenesis strategies, and the impact on cisplatin sensitivity was measured. Expression of the BAD pathway was studied in a range of cancer cell types, and the influence on sensitivity to a variety of chemotherapeutics was measured. Finally, a BAD-pathway expression signature was developed and evaluated in treated cell lines and in patient datasets. To execute these analyses, 3 sample/datasets were used: 1) a panel of 8 cell lines, which were subjected to serial cisplatin treatments, 2) genome-wide expression data from 142 patients treated at Duke University Medical Center and Moffitt Cancer Center (MCC) (including 114, previously reported (8) and 28 new samples), and 3) 147 OVCA samples obtained from the University of Minnesota (UMN, n = 49) and MCC (n = 98) and analyzed by immunoflourescence for phospho-BAD protein levels. As such, this study included analysis of data/specimens from 289 (142 + 147) OVCA patients treated at MCC, Duke, and UMN.
Induction of In Vitro Platinum Resistance
The OVCA cell lines, A2008, A2780CP, A2780S, C13, IGROV1, OV2008, OVCAR5, and T8 were provided by Dr. Patricia Kruk (Department of Pathology, College of Medicine, University of South Florida, Tampa, FL) and maintained as previously described (10) (see Supplementary Data). Of note, C13 is a cisplatin derivative of OV2008, and T8 is a topotecan-resistant sub-clone of IGROV1. Such paired sensitive/resistant cell lines were included in the analysis to ensure that we were able to identify genomic changes associated with increased cisplatin-resistance from a variety of baseline sensitivity/resistance states. Cells were subjected to sequential treatment with increasing doses of cis-diammine-dichloroplatinum (cisplatin), using three dosing schedules resulting in 144 treatment/expansion cycles (Supplementary Figure S1). Treatment schedules A, B, and C included three treatments with 1, 2, and 3 µg/mL cisplatin, respectively, followed by three treatments with 3, 4, and 5 µg/mL, respectively. Each cisplatin treatment was followed by a cell recovery/expansion phase. Both cisplatin-resistance and genome-wide expression changes were measured serially in each cell line at baseline and after 3 and 6 cisplatin-treatment/expansion cycles. We quantified cisplatin-resistance using CellTiter-96 MTS proliferation assays (Fisher Scientific) and analyzed genome-wide expression using Affymetrix Human U133 Plus 2.0 GeneChips as previously described (10, 11) (Gene Expression Omnibus (GEO) accession number GSE23553). Mycoplasma testing was performed on the cell lines every 6 months following manufacturer’s protocol (Stratagene).
Statistical Analysis of Cell Line Array Data
Pearson correlation was used to identify genes associated with OVCA development of cisplatin resistance (EC50). Expression was calculated using the robust multi-array average algorithm (12) implemented in Bioconductor (http://www.bioconductor.org) extensions to the R-statistical programming environment as described previously (13). Probe sets with expression ranges <2-fold (maximum/minimum) and control probes (i.e., AFFX_* probe sets) were excluded from the analysis. For each cell line, Pearson correlation coefficients were calculated for expression data and cisplatin EC50 (Supplementary Table S1). Genes/probe sets demonstrating expression/EC50 correlations (|R| > 0.85) were subjected to biological pathway analysis using GeneGo/MetaCore™ software (Supplementary Table S2). Maps/pathways were identified using the GeneGo/MetaCore™ statistical test for significance (P < 0.001).
Primary OVCA Patient Samples
OVCA samples/datasets from 289 patients treated at MCC, Duke, and UMN were analyzed in this study, including: 1) genome-wide expression data from 142 patients treated at Duke and MCC (including 114, previously reported, (8), and 28 new samples) and 2) 147 OVCA samples obtained from UMN (n = 49) and MCC (n = 98) and analyzed by immunoflourescence (IF) for pBAD protein levels. In brief, all 289 patients were known to have advanced-stage (III/IV), serous epithelial OVCA and underwent primary cytoreductive surgery followed by primary therapy with a platinum-based regimen (+/− taxane or cyclophosphamide). Additional details are provided in the Supplementary Data.
Statistical Analysis of Primary OVCA Genomic Data
Probe sets differentially expressed between primary platinum therapy complete responder (CR; n = 101) and incomplete-responder (IR; n = 41) OVCA samples were identified using Student’s t-test (P < 0.01) and subjected to GeneGo/MetaCore™ pathway analysis.
Characterization of the BAD-Apoptosis Pathway Proteins in Primary OVCAs and Cell Lines
Total BAD, pBAD (serine-112, -136, -155), non-phosphorylated BAD (Genscript), and BAD phosphatase PP2C/PPM1A (Santa Cruz Biotechnology) protein levels were evaluated in a subset of the cell line panel (8 cisplatin-treated OVCA cell lines) and in primary OVCA samples by Western blot or by immunofluorescence as previously described (14, 15).
Western Blot Analysis
Cells were harvested in media using a Cell Lifter, washed with cold PBS, and solubilized using SDS lysis buffer (2% SDS, 10% glycerol, 0.06 M Tris, pH 6.8). The resultant lysate (50 µg) was immediately separated on SDS-PAGE gels and transferred to nitrocellulose membranes. Membranes were blocked in Tris-buffered saline containing 0.05% Tween 20 (TBST)-5% nonfat milk and incubated with primary antibody in TBST-5% nonfat milk overnight at 4°C. Membranes were washed three times for 5 minutes with TBST and incubated with the appropriate secondary antibody in TBST-5% non-fat milk for 90 minutes at room temperature. Membranes were again washed three times for 5 minutes with TBST, and antibody binding was visualized by chemiluminescence on autoradiography film.
Immunofluorescence Microscopy
Slides were deparaffinized and rehydrated using xylene followed by serial dilutions of ethanol and subjected to heat-induced epitope retrieval by incubation in Tris-EDTA buffer (10 mM Tris base, 1 nM EDTA, 0.05% Tween 20, pH 9.0) for 20 minutes at 100°C. Slides were washed in PBS, incubated in blocking serum (0.3% Triton X-100, 0.1% normal goat serum in PBS) for 1 hour at room temperature, and exposed to primary antibody in blocking serum for 48 hours at 4°C. Slides were washed 3× in PBS, incubated with fluorescent-labeled secondary antibody in blocking serum for 2 hours at room temperature, and counterstained and mounted with Prolong Gold containing DAPI (Invitrogen). Images were acquired as TIFF files using the Zeiss Axio Imager Z1 automated fluorescent scope and analyzed for percent expressing cells using Image Pro Plus software.
siRNA Transfection
RNA duplexes for PP2C/PPM1A (s10909 and s10919, ABI), cAMP-dependent protein kinase (PKA; 6406 and 6574, Cell Signaling), and pFlag-600 vectors containing full-length BAD harboring serine (S) to alanine (A) mutations of the individual phosphorylation sites (S112A, S136A, S155A) (kind gifts from Dr. Hong Gang Wang, MCC) were transfected using the Nucleofector transfection kit, according to manufacturer’s protocols (Amaxa). Briefly, cells (4×106) were suspended in 0.1 mL electroporation buffer V containing 1 µM siRNA and pulsed once using program X-001. Pulsed cells were resuspended in 0.5 mL of complete media without antibiotics and incubated at 37°C for 15 minutes before experimentation. The Silencer negative control no. 2 siRNA (4390846, ABI), a non-targeting siRNA duplex, was used as a control. MTS cell viability analyses (CellTiter96, Promega) was used to evaluate cellular proliferation rate at 72 hours for cells expressing wild-type, S112A, S136A, and S155A mutations.
Analysis of Apoptotic Nuclei
Morphologic assessment of condensed chromatin and fragmented DNA was used to quantify percent apoptotic nuclei. Cells were fixed in 4% paraformaldehyde, and nuclei were stained with bis-benzimide trihydrochloride (0.5 µg/ml; Molecular Probes) and quantified using fluorescence microscopy (15).
Evaluation of BAD-Pathway Genes
The BAD-pathway score was computed in the panel of OVCA cells previously subjected to serial cisplatin treatment. It was also independently computed for the clinical-genomic OVCA dataset (n = 142 OVCA samples from MCC and Duke). For the cell line data, Pearson correlation was used to test any linear relationship between the BAD-pathway score derived from the cell line data and levels of pBAD proteins. For the clinical-genomic OVCA dataset, log-rank test with Kaplan-Meier survival curves was used to test if the median-split BAD-pathway score derived from the OVCA patient data was associated with overall survival.
Specifically, using genomic data from the panel of OVCA cells previously subjected to serial cisplatin treatment, principal component analysis was used to derive a BAD-pathway gene expression signature with a corresponding “pathway score” that represents overall gene expression levels for BAD-pathway genes. The generation of the signature used data from cell lines only; no patient data were used. Details of the statistical methodology used to generate the BAD-pathway gene expression signature are provided in the Supplementary Data. Briefly, as outlined above, using the GeneGo/MetaCore™ statistical test for significance, analysis of gene expression/EC50 data from for the panel of OVCA CIS-treated cell lines, identified the BAD apoptosis pathway (P < 0.001) to be associated with cell line CIS resistance. GeneGo/MetaCore™-defined objects (genes) within the BAD pathway, associated with OVCA cell line CIS EC50, were thus identified. All probesets, for each BAD pathway object identified in this way, were selected for inclusion in generation of the principal component analysis score. These 98 probesets represented 47 genes. For this cell line data, Pearson correlation was used to test any linear relationship between the BAD-pathway score derived from the cell lines and levels of pBAD proteins. The BAD-pathway gene expression signature score developed in OVCA cell lines was evaluated in an independent set of 142 MCC/Duke OVCA samples. For this clinical-genomic OVCA dataset, log-rank test with Kaplan-Meier survival curves were used to test any association between the BAD-pathway score (“high” versus “low” based upon a median value cut-off) and overall survival for patients with OVCA. No data from the 142 MCC/Duke OVCA samples were used to identify the 47-gene signature; the MCC/Duke ovarian data was a completely independent evaluation set.
RESULTS
Expression of BAD-Pathway Genes Correlates with the Evolution of Platinum Resistance
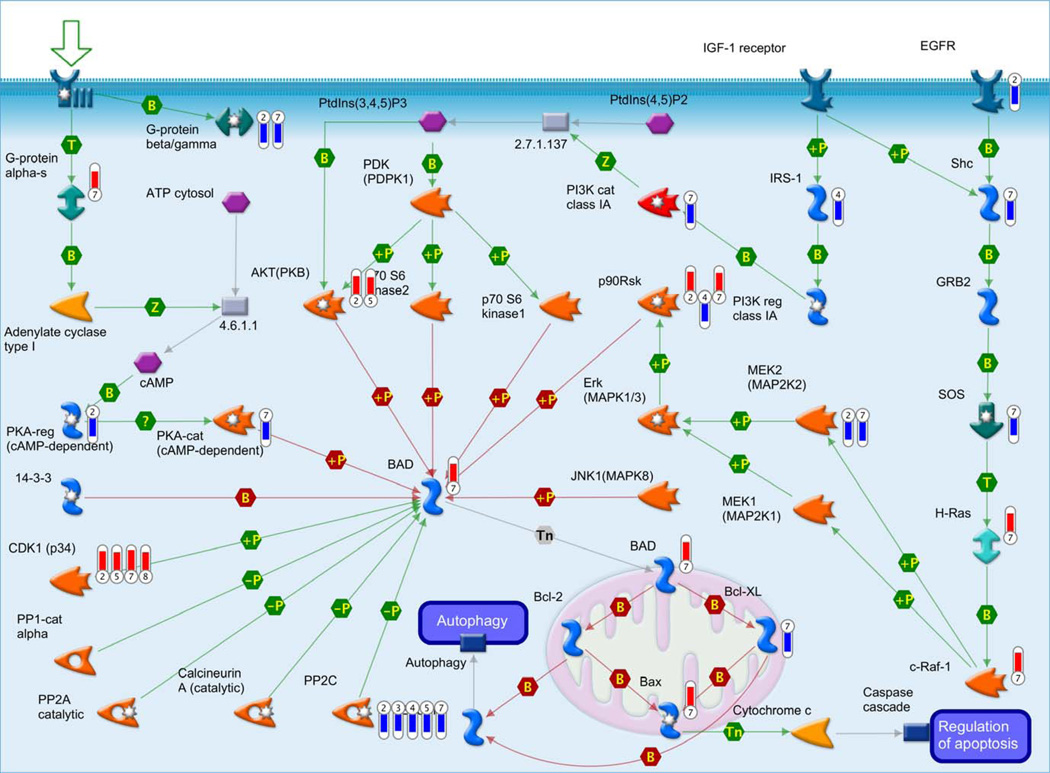
In the OVCA cell lines that we subjected to serial cisplatin treatment, expression of 3,111 unique probe sets, representing 2,434 unique genes, correlated across dose levels with cisplatin-resistance, as measured by EC50 (Pearson correlation coefficient >0.85, absolute value). GeneGO MetaCore™ analysis identified the “BAD phosphorylation, apoptosis and survival” pathway to be associated with development of in vitro cisplatin-resistance (P < 0.001) (Fig. 1). This BAD-pathway includes 47 genes (98 probe sets in Affymetrix 133A chip; Supplementary Table S3), which were used to derive a BAD-pathway score in the cell line data and the OVCA patient samples. Statistical significance was derived from the number of genes that were input into the analysis software, the number of input genes present in a specific pathway, and the actual number of genes in that pathway. Thus, the P value represents the probability that mapping a set of genes to a particular pathway occurs by chance. BAD-pathway genes found to be associated with the evolution of in vitro cisplatin-resistance included BAD, Bax, BcL-XL, PP2C/PPM1A, AKT, EGFR, IRS-1, Shc, H-Ras, CDK1, G-protein alpha-s, G-protein beta/gamma, PI3K cat class 1A, c-Raf-1, p90Rsk, MEK2 (MAP2K2), PKA-cat, and PKA-reg (Fig. 1).
Figure 1.
BAD pathway in genes associated with induced cisplatin-resistance. Thermometers indicate those genes with positive (upward pointing) and negative (downward pointing) correlations between expression and increased cisplatin-resistance (EC50) (P < 0.001 for pathway enrichment): upward pointing thermometers identify genes with increasing expression associated with increasing OVCA cisplatin-resistance, and downward pointing thermometers identify genes with decreasing expression associated with increasing OVCA cisplatin-resistance. Numbers 1–8 at base identify the cell line (1 = T8, 2 = OVCAR5, 3 = OV2008, 4 = IGROV1, 5 = C13, 6 = A2780S, 7 = A2780CP, 8 = A2008) demonstrating changes in expression of that gene with increasing cisplatin-resistance.
Genes Associated with Patient OVCA Platinum Response
In 142 OVCA patient samples, 397 probe sets, representing 347 unique genes, were identified as differentially expressed (P < 0.01) between CR versus IR primary OVCAs (Supplementary Table S2). Pathway analysis of these 347 unique genes demonstrated representation of the “BAD-phosphorylation, apoptosis and survival” pathway to be approaching statistical significance (P < 0.08). Analysis of IR versus CR (P < 0.05 threshold) for patients subjected to optimal versus suboptimal surgical cytoreduction demonstrated representation of the BAD-pathway at a statistically significant level (P = 0.004 and <0.001, respectively).
BAD-Protein Phosphorylation Status Is Associated with In Vitro and In Vivo Chemo-Resistance and Overall Survival
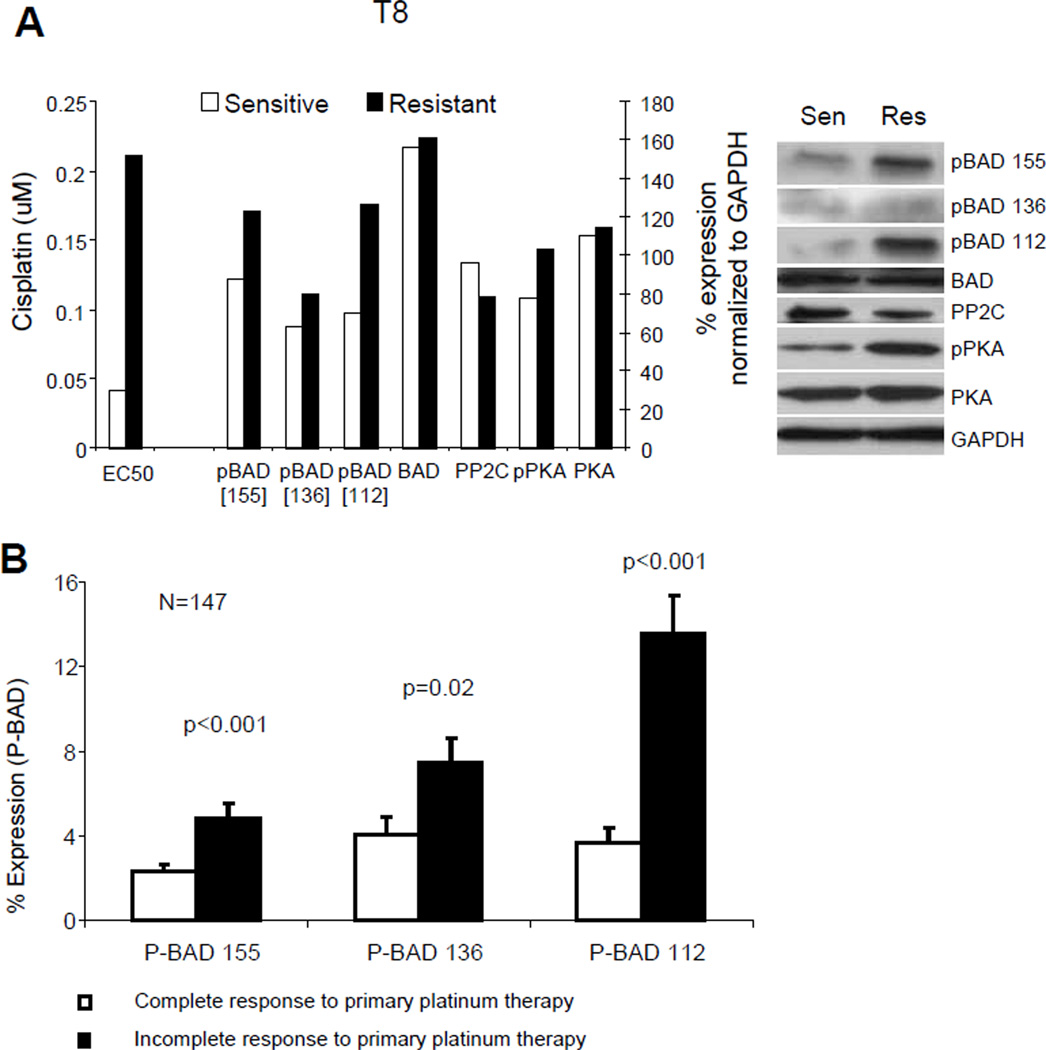
Many of the BAD-pathway genes found to be associated with evolution of in vitro cisplatin resistance are known to influence BAD phosphorylation (Fig. 1). We therefore tested the hypothesis that BAD protein-phosphorylation status is associated with OVCA cisplatin resistance. Protein levels of total BAD, pBAD (serine-112, -136, and -155), total BAD protein, the BAD phosphatase PP2C/PPM1A, the phosphorylated form of the BAD kinase PKA, and total PKA protein were evaluated by Western blot analysis or immunofluorescence in 1) OVCA cell lines subjected to serial cisplatin treatment (T8) and/or 2) 147 primary OVCA samples (MCC/UMN) (Fig. 2).
Figure 2.
BAD-protein phosphorylation is associated with platinum resistance. A, Comparison of cisplatin EC50 as determined by MTS cell viability assays and percent expression normalized to GAPDH of phosphorylated-BAD (pBAD) isoforms (pBAD-155, -136, -112), total BAD, PP2C (PPM1A), phosphorylated PKA (pPKA), and total PKA as measured by Western blot at baseline and after in vitro induction of platinum resistance in T8 OVCA cells. B, Percent expression of pBAD at serine-155, -136, and -112 by immunofluorescence in an independent set of 147 primary advanced-stage OVCA samples, including platinum-sensitive/complete responders (n = 86) and platinum-resistant/incomplete-responders (n = 61). Error bars indicate standard error of the mean.
OVCA cell lines subjected to in vitro cisplatin-treatment/expansion cycles
Serially treated OVCA cells demonstrated higher cisplatin EC50 values and corresponding overall higher levels of both pBAD (serine-112, -136, -155) and pPKA than before serial cisplatin treatment (Fig. 2A). In contrast, protein levels of the BAD phosphatase PP2C/PPM1A were expressed at lower levels in serially cisplatin-treated cells.
Primary OVCA samples
Consistently, analysis of 147 patient primary OVCAs revealed higher levels of pBAD (serine-112, -136, and -155) in platinum-resistant (IR) than in platinum-sensitive (CR) samples (P < 0.001, P = 0.02, and P < 0.001, respectively) (Fig. 2B). Immunofluorescence data were available for 134/147 samples for analysis of serine-112, 134/147 for serine-136, and 137/147 for serine-155. Median level of pBAD of each serine was used to as a cutoff to dichotomize patients into two groups, high versus low level of pBAD. Log-rank test with Kaplan-Meier survival curves revealed that patients with low levels of serine-112 had superior survival versus patients with high levels of pBAD (P = 0.001) (Fig. 3A).
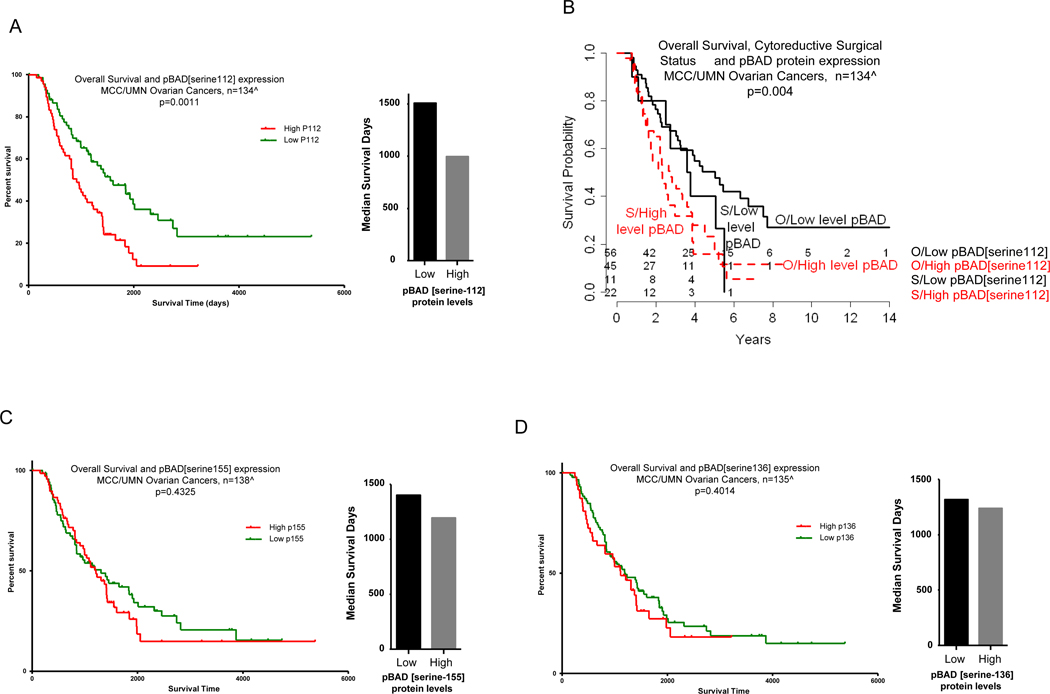
Figure 3.
Low expression levels of pBAD protein is associated with overall survival. A, pBAD (serine-112) levels and overall survival, represented by Kaplan-Meier curves (left) and bar graphs for median survival (right). B, Kaplan-Meier overall survival curves for pBAD (serine-112) levels with cytoreductive status. C, pBAD (serine-155) levels and overall survival, represented by Kaplan-Meier curves (left) and bar graphs for median survival (right). D, pBAD (serine-136) levels and overall survival, represented by Kaplan-Meier curves (left) and bar graphs for median survival (right). MCC/UMN, Moffitt Cancer Center and University of Minnesota datasets. ^Information available out of 147 samples. The numbers at risk are shown at bottom of graphs. Log-rank test P values indicate significance. O, optimal; S, suboptimal.
Integration of the median-cutoff pBAD (serine-112) with the cytoreductive surgery (optimal versus suboptimal) showed significant association with overall survival (P = 0.004 by log-rank test) (Fig. 3B). Specifically, patients who had optimal cytoreductive surgery with low levels of pBAD (serine-112) had superior survival versus patients who had optimal cytoreductive surgery with high levels of pBAD (adjusted P = 0.03 by Holm method (16) (Fig. 3B). While it was not statistically significant, the same trend was observed for patients who had suboptimal cytoreductive surgery with low pBAD (serine-112) levels versus patients who had suboptimal debulking with high pBAD (serine-112) levels (adjusted P = 1). Similarly, patients who had suboptimal cytoreductive surgery with low pBAD (serine-112) had survival that trended toward superiority, but was not statistically significant, compared with patients who had optimal cytoreductive surgery with high levels of pBAD (adjusted P = 1; Fig. 3B). Patients who had suboptimal cytoreductive surgery with high levels of pBAD (serine-112) had the poorest overall survival (Fig. 3B). Serine-136 and -155 levels were not associated with overall survival. Although log-rank test with Kaplan-Meier survival curves revealed no statistically significant differences in survival based upon levels of pBAD serine-136 (P = 0.40) or pBAD serine-155 (P = 0.43), patients with high- versus low-levels of pBAD at both of these phospho-sites were observed to have lower median survival, although differences did not reach statistical significance (P = 0.6 and 0.2, respectively; Fig. 3C and 3D).
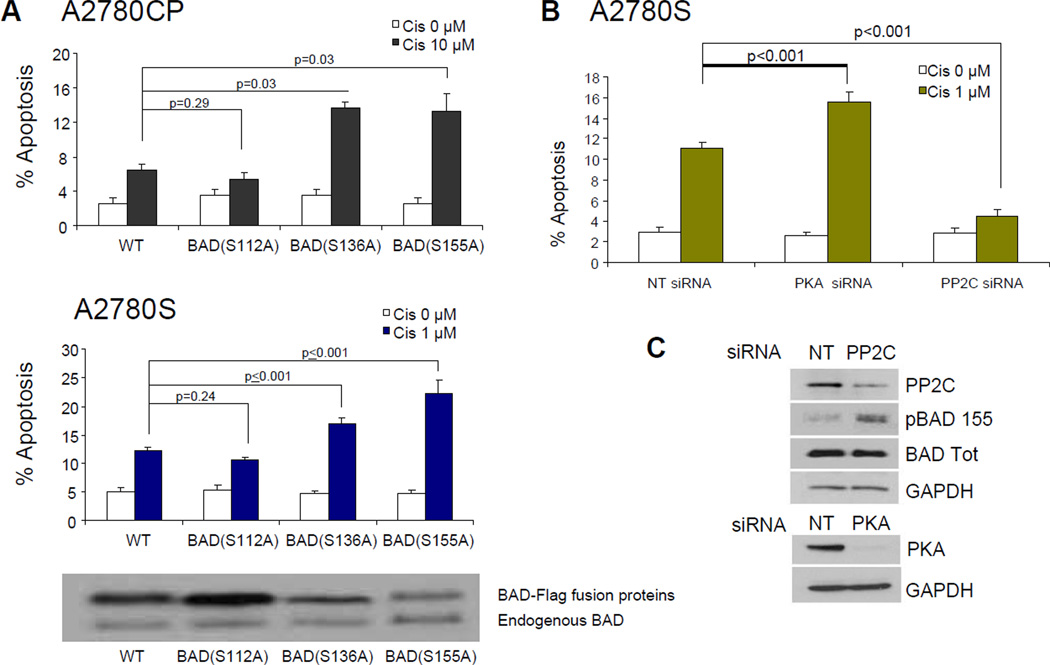
Direct and indirect modulation of BAD phosphorylation status
Modulation of BAD phosphorylation status influenced cisplatin sensitivity in OVCA cell lines. Over-representation of non-phosphorylated BAD by transfection of A2780S and A2780CP cells with vectors containing serine (S) to alanine (A) mutations (BAD[S136A], BAD[S155A]) in BAD (site mutations that prevent phosphorylation of the BAD protein) resulted in increased cisplatin-induced apoptosis compared to cells transfected with wild-type BAD (Fig. 4A). In contrast, cells transfected with BAD[S112A] had no effect on cisplatin sensitivity (Fig. 4A). MTS cell viability analysis (CellTiter96, Promega) demonstrated that cells expressing wild-type, S112A, S136A, and S155A mutations maintained similar proliferation rates after 72 hours of growth.
Figure 4.
Modulation of BAD-protein phosphorylation status influences cisplatin sensitivity. A, OVCA cell lines A2780S and A2780CP were transfected with pFlag-600 vectors expressing wild-type BAD (WT) or BAD harboring serine (S) to alanine (A) point mutations in serine-112, -136, or -155 (S112A, S136A, S155A). These S-to-A phosphorylation site mutations prevent phosphorylation of the BAD protein. Transfected cells were treated with vehicle or 1 µM (A2780S) or 10 µM (A2780CP) cisplatin for 48 hours and evaluated for the presence of apoptotic nuclei. B, Percent apoptotic nuclei in A2780S cells in the presence of 1 µM cisplatin after siRNA depletion of PKA and PP2C. Similar results were observed using two different siRNAs for each PP2C and PKA. Error bars indicate standard error of the mean. C, Western blot showing depletion of PP2C and PKA by siRNA. Controls included a non-targeting siRNA (NT). GAPDH was used as a loading control.
The role of pBAD (serine-155) in cisplatin sensitivity was further evaluated in A2780S cells by depletion of PKA and PP2C/PPM1A using siRNA. Depletion of PKA and PP2C/PPM1A resulted in reduced target protein expression (Fig. 4B). Depletion of PKA decreased pBAD levels and increased cisplatin-induced apoptosis compared to cells transfected with a non-targeting control siRNA. In contrast, cells depleted of PP2C/PPM1A demonstrated increased pBAD levels and decreased cisplatin-induced apoptosis (Fig. 4B and C).
A 47-gene BAD-pathway score is associated with in-vitro phospho-BAD levels and human cancer clinical outcome
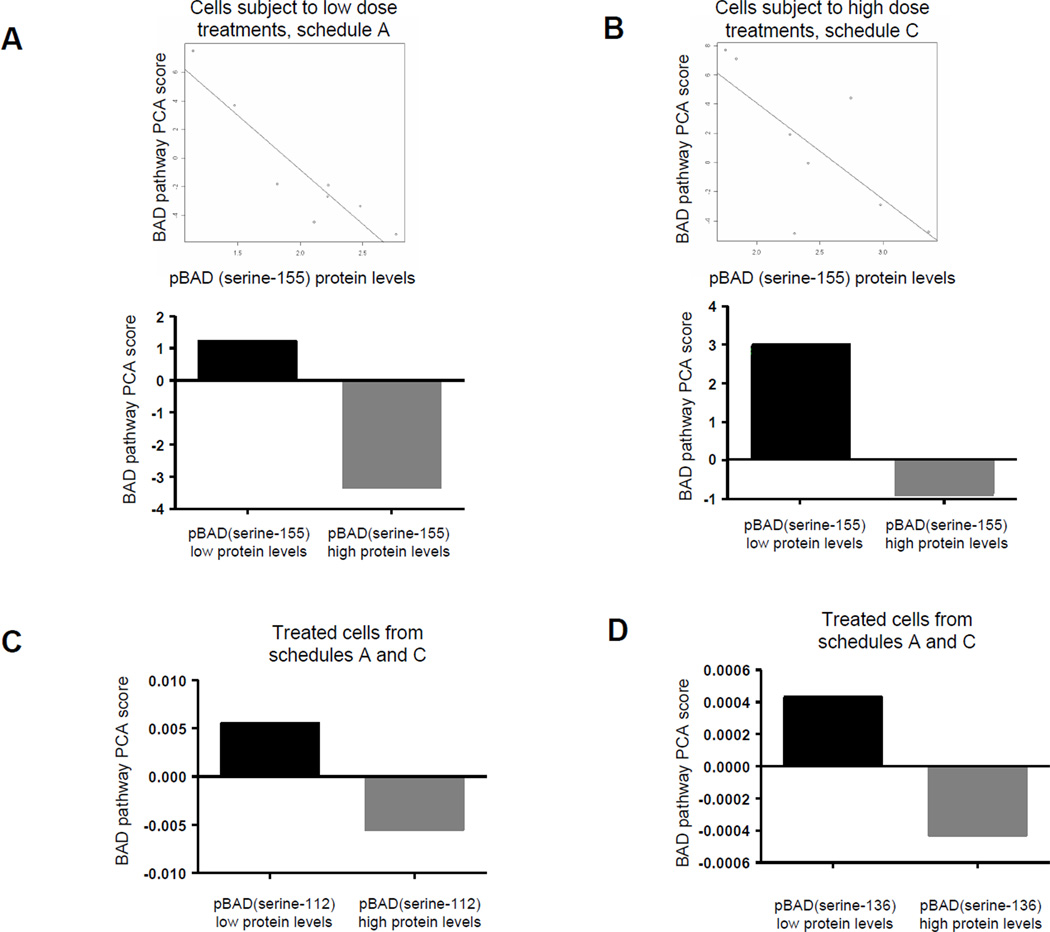
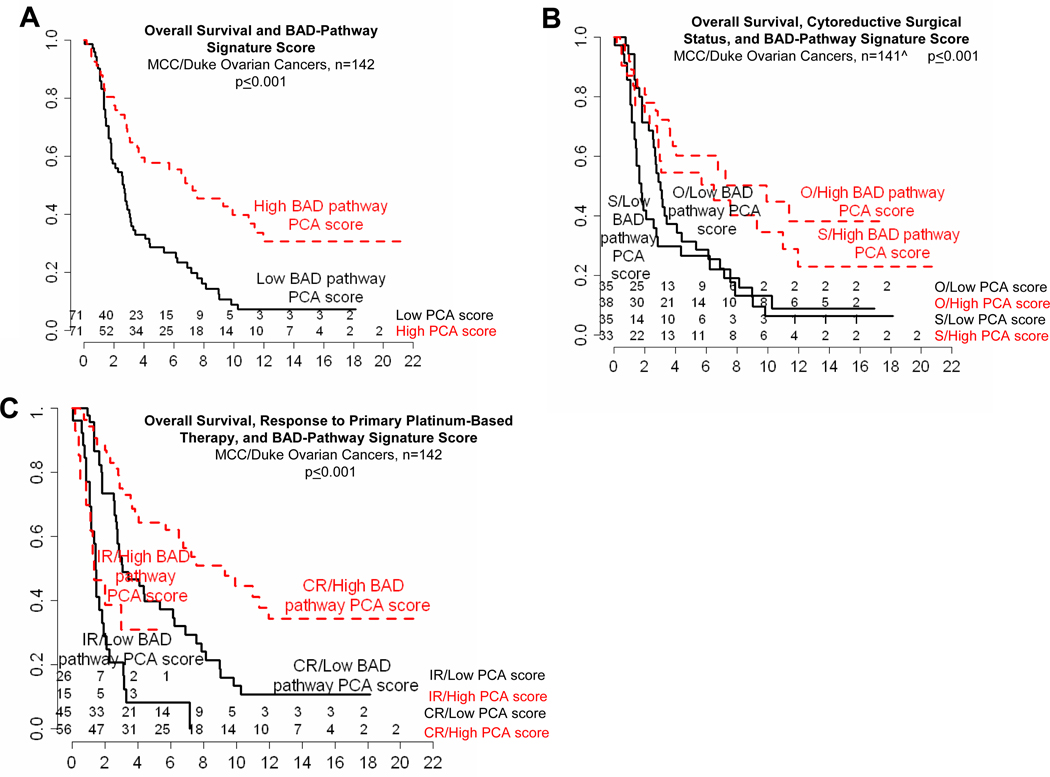
Based on the above data, we developed a 47-gene BAD-pathway score in the cell line data and evaluated it in an OVCA genomic dataset data (Supplementary Table S3). For cell lines, we identified a negative correlation between BAD-pathway signature score and levels of pBAD (serine-155) protein in cells treated with low-dose cisplatin (schedule A; Pearson score = −0.92, P = 0.001) and higher dose cisplatin (schedule C; Pearson score = −0.72, P = 0.045) (Fig. 5A and B). Although pBAD (serine-112 and 136) levels did not demonstrate statistically significant correlations with BAD-pathway score, when high and low dosing schedules are evaluated together (schedules A and C), mean BAD pathway score is higher in cells with low versus high levels of pBAD (serine-112) and pBAD (serine-136) using median pBAD as a cut-off (Fig. 5C and D). For the OVCA patient data, the BAD-pathway score was associated with overall survival from OVCA (n = 142, P ≤ 0.0001, Fig. 6A), Furthermore, the OVCA genomic dataset was evaluated with regard to BAD-pathway score and surgical cytoreductive (debulking, n = 141; debulking status unavailable for 1 of 142 patients) status (optimal: <1 cm; suboptimal: >1 cm residual tumor at conclusion of surgery, P < 0.0001, Fig. 6B) and also response to primary platinum-based therapy (CR or IR, P < 0.0001, Fig. 6C). The association of high BAD-pathway score and favorable outcome was observed in patients who underwent optimal and suboptimal debulking (optimal: adjusted P = 0.007, suboptimal: adjusted P = 0.06). Most importantly, OVCA patients with a high BAD-pathway score who underwent suboptimal debulking had a survival that trended toward superiority versus patients with a low BAD-pathway score who underwent optimal debulking (adjusted P = 0.19). Similarly, patients who demonstrated an IR to primary platinum-based therapy but had a high BAD-pathway score had no statistical difference in survival compared to those patients who demonstrated a CR but had a low BAD-pathway score (adjusted P = 0.22). When evaluated with debulking status and response to primary platinum-based therapy, grade, and age, the Cox proportional hazards model revealed that the BAD-pathway score was an independent variable associated with survival (P = 0.01).
Figure 5.
High BAD-pathway signature principal component analysis (PCA) score is associated with low expression levels of pBAD protein. Scatter plots show negative correlation between PCA score and pBAD (serine-155) protein levels and bar graphs show inverse relationship between mean PCA score and pBAD (serine-155) protein levels in cell lines subjected to low-dose (A) treatment schedule A (p=0.001) and high-dose (B) treatment schedule C (P=0.045). Mean PCA sc ore was associated with low pBAD (serine-112) (C) and low pBAD (serine-136) (D) protein levels in treated cells from combined schedules A and C. For the bar graphs, the appropriate median pBAD (serine-155, -136, or -112) protein levels was used as the cut off.
Figure 6.
High BAD-pathway signature PCA score is associated with favorable clinical outcome. A–C, Kaplan-Meier curves depicting the association between BAD-pathway signature PCA score and overall survival from cancer for MCC and Duke datasets. ^Information available for 141 of 142 samples. The numbers at risk are shown at bottom of graphs. Log-rank test P values indicate significance. CR, complete response; IR, incomplete response; O, optimal; S, suboptimal.
DISCUSSION
Few clinical or biologic events affect the outcome for patients with OVCA more than response to chemotherapy. In this study, using a novel in vitro strategy, we identified and characterized the BAD-apoptosis pathway to be influential in the response of OVCA to chemotherapy, likely via modulation of BAD phosphorylation; we also identified expression of this pathway to be independently associated with clinical outcome for patients with OVCA. Furthermore, levels of the pBAD protein are not only associated with mRNA expression of the pathway (measured by a 47-gene pathway signature score) but are also independently associated with survival from OVCA. We provide extensive validation of our findings (and the importance of the BAD pathway) with in vitro functional studies and in vivo and in silico analyses of 289 patient specimens and/or datasets. Our findings are further validated by the fact that many of our BAD pathway signature genes, including RAF1, BAD, PPM1B, PPM1F, GNAS, PRKAR1A, BAX, PIK3CD, and PTPN11, have previously been reported to be associated with OVCA chemo-sensitivity (8, 10, 17–21). Our work builds upon previous reports that suggest that phosphorylation of the BAD protein may be associated with cisplatin-resistance in ovarian and head and neck cancer cell lines (22, 23). Interestingly however, Konstantinopoulos et al, recently analyzed four microarray datasets including 265 advanced-stage OVCAs and identified and validated a 19-gene prognostic model. Neither the 19-gene model nor the pathways associated with high- versus low-risk disease included representation of the BAD pathway (24).
BAD is a member of the BCL2 family of proteins, which are characterized by the presence of up to 4 BCL2-homology domains (25). This family includes inhibitors and promoters of apoptosis, such that cell survival versus death is determined by the relative ratio of pro-apoptotic (e.g., BCL-Xs, BAD, Bax, Bak) and anti-apoptotic (e.g., Bcl-2, Bcl-xL, MCL-1, A1, BAG-1) family members (25–28). BAD selectively hetero-dimerizes with Bcl-xL and Bcl-2 but not with Bax, Bcl-xs, Mcl-1, A1, or itself. When BAD dimerizes with Bcl-xL, Bax is displaced, mitochondrial membrane permeability increases, and apoptosis is induced (29). However, BAD function is regulated by phosphorylation (including serine-112, -136, and -155). When phosphorylated, BAD is unable to heterodimerize with Bcl-2 or Bcl-xL, freeing Bcl-xL to dimerize and functionally sequester Bax, such that it is no longer free to induce apoptosis (29). Thus, the phosphorylation status of BAD determines whether Bax is displaced from Bcl-xL to drive cell death. BAD is thought to be phosphorylated at serine-136 by protein kinase B (PKB/Akt) (30). In contrast, serine-112 is phosphorylated by mitogen-activated protein kinase-activated protein kinase-1 (MAPKAP-K1, also called RSK) and PKA. Serine-155, at the center of the BAD BH3 domain, is phosphorylated preferentially by PKA, which also inhibits Bcl-xL binding (31–33). Conversely, the activity of a series of phosphatases, including PP1, PP2A, and PPM1 (PP2C/PPM1A), as well as calcineurin, has been shown to have pro-apoptotic effects via de-phosphorylation of BAD (34, 35).
Using an in vitro model to induce OVCA cisplatin-resistance, we have identified expression of BAD-apoptosis pathway genes to be associated with the evolution of cisplatin-resistance and recognized that many of these genes are kinases or phosphatases that influence the phosphorylation status of the BAD protein. Consistently, we found that pBAD levels increased with OVCA cisplatin-resistance in both the cell lines and primary patient samples and that pBAD protein levels were associated with poor overall survival from OVCA. To validate our findings and the importance of the BAD pathway, we demonstrated that in vitro manipulation of pBAD levels (by siRNA depletion of a BAD kinase or BAD phosphatase or by targeted mutagenesis of some BAD-phosphorylation sites) resulted in a corresponding change in cisplatin-induced apoptosis, without changes to proliferation. To support and further explore the clinical relevance of these findings, we evaluated a 47-gene BAD-pathway score and phospho-BAD in a panel of OVCA cells in which we induced cisplatin resistance by serial treatments and an OVCA data/samples obtained from 289 patients. Our results show that a high BAD-pathway signature score is associated with low in vitro pBAD levels and favorable overall survival for patients with OVCA. Importantly, analyses of OVCA genomic data and pBAD protein levels from patients with advanced-stage disease have suggested that the influence of the BAD pathway on overall survival may be more important than the volume of residual disease at the completion of primary surgery, traditionally one of the most important clinical determinants of outcome for patients with OVCA. Such findings could have substantial implications for future clinical treatment of patients with this disease, although additional studies are required. Notably, survival for patients with low versus high levels of phospho-BAD was superior when considering each phosphorylation site (serine-112, -136, -155), however, only the serine-112 site reached statistical significance (Fig. 3). Clearly, additional functional analyses are warranted to better define the mechanistic basis to our observations; our analysis does not speak to the relative importance of each BAD phosphorylation sites, nor to any potential influence of sequence of BAD phosphorylation on cellular function and clinical outcome. Furthermore, it is worth noting that, while our data highlights the importance of this pathway, not all cell lines demonstrated associations between increasing CIS resistance and expression of BAD pathway genes, emphasizing that OVCA is a highly heterogeneous disease and it is likely that many other pathways and biologic processes contribute to the development of chemo-resistance and influence patient survival. In this regard, it is also noteworthy that use of the term “BAD pathway” may be somewhat arbitrary, given the interactions and crosstalk with other closely related proteins and pathways (e.g., RAS-RAF-MEK, PI-3k-AKT, BCL-XL/BAX) many of which have been associated with OVCA drug resistance (36–38).
In addition to characterizing a mechanism by which epithelial OVCAs develop resistance to chemotherapy, we have identified a pathway that has significant clinical relevance as a potential biomarker of therapeutic response and overall patient survival and as a promising therapeutic target. Use of such BAD pathway-based biomarkers could form the basis of an individualized therapeutic approach to women with OVCA, enabling patients to be stratified into high- and low-risk groups, the latter being offered more aggressive therapy, enrollment in clinical trials of novel agents, or the addition of pBAD inhibitors to standard of care drugs.
Statement of Translational Relevance.
Despite initial sensitivity to chemotherapy, patients with ovarian cancer (OVCA) often develop drug-resistance, which limits survival. In this study, we explored genome-wide expression changes that underlie the evolution of chemo-resistance and characterized the BCL2 antagonist of cell death (BAD) apoptosis pathway as a determinant of chemo-sensitivity and patient survival. Expression of the BAD pathway and also BAD-protein phosphorylation status was associated with in vitro and in vivo platinum resistance, as well as overall survival, in more than 140 patients with advanced-stage (III/IV) serous OVCA, independent of surgical cytoreductive status. The BAD apoptosis pathway influences OVCA chemo-sensitivity and overall survival, likely via modulation of BAD-phosphorylation. The pathway has clinical relevance as a biomarker of therapeutic response, patient survival, and as a promising therapeutic target.
Supplementary Material
ACKNOWLEDGMENTS
Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the funding agencies.
We thank Rasa Hamilton (Moffitt Cancer Center) for editorial assistance.
GRANT SUPPORT
This project was supported in part by National Cancer Institute Grant R21 CA-110499-01A2, the Ocala Royal Dames For Cancer Research Inc., the Phi Beta Psi Sorority, the Hearing the Ovarian Cancer Whisper, Jacquie Liggett Foundation, the Ovarian Cancer Research Fund, and the US Army Medical Research and Materiel Command under Award No. DAMD17-02-2-0051.
Footnotes
Conflicts of interest: None.
REFERENCES
- 1.Baker VV. Salvage therapy for recurrent epithelial ovarian cancer. Hematol Oncol Clin North Am. 2003;17:977–988. doi: 10.1016/s0889-8588(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 2.Hansen HH, Eisenhauer EA, Hansen M, Neijt JP, Piccart MJ, Sessa C, et al. New cytostatic drugs in ovarian cancer. Ann Oncol. 1993;4 Suppl 4:63–70. doi: 10.1093/annonc/4.suppl_4.s63. [DOI] [PubMed] [Google Scholar]
- 3.Herrin VE, Thigpen JT. Chemotherapy for ovarian cancer: current concepts. Semin Surg Oncol. 1999;17:181–188. doi: 10.1002/(sici)1098-2388(199910/11)17:3<181::aid-ssu7>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 4.Godwin AK, Meister A, O'Dwyer PJ, Huang CS, Hamilton TC, Anderson ME. High resistance to cisplatin in human ovarian cancer cell lines is associated with marked increase of glutathione synthesis. Proc Natl Acad Sci U S A. 1992;89:3070–3074. doi: 10.1073/pnas.89.7.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson SW, Laub PB, Beesley JS, Ozols RF, Hamilton TC. Increased platinum-DNA damage tolerance is associated with cisplatin resistance and cross-resistance to various chemotherapeutic agents in unrelated human ovarian cancer cell lines. Cancer Res. 1997;57:850–856. [PubMed] [Google Scholar]
- 6.Johnson SW, Swiggard PA, Handel LM, Brennan JM, Godwin AK, Ozols RF, et al. Relationship between platinum-DNA adduct formation and removal and cisplatin cytotoxicity in cisplatin-sensitive and -resistant human ovarian cancer cells. Cancer Res. 1994;54:5911–5916. [PubMed] [Google Scholar]
- 7.Benedetti V, Perego P, Luca Beretta G, Corna E, Tinelli S, Righetti SC, et al. Modulation of survival pathways in ovarian carcinoma cell lines resistant to platinum compounds. Mol Cancer Ther. 2008;7:679–687. doi: 10.1158/1535-7163.MCT-07-0450. [DOI] [PubMed] [Google Scholar]
- 8.Dressman HK, Berchuck A, Chan G, Zhai J, Bild A, Sayer R, et al. An integrated genomic-based approach to individualized treatment of patients with advanced-stage ovarian cancer. J Clin Oncol. 2007;25:517–525. doi: 10.1200/JCO.2006.06.3743. [DOI] [PubMed] [Google Scholar]
- 9.Jazaeri AA, Awtrey CS, Chandramouli GV, Chuang YE, Khan J, Sotiriou C, et al. Gene expression profiles associated with response to chemotherapy in epithelial ovarian cancers. Clin Cancer Res. 2005;11:6300–6310. doi: 10.1158/1078-0432.CCR-04-2682. [DOI] [PubMed] [Google Scholar]
- 10.Boren T, Xiong Y, Hakam A, Wenham R, Apte S, Chan G, et al. MicroRNAs and their target messenger RNAs associated with ovarian cancer response to chemotherapy. Gynecol Oncol. 2009;113:249–255. doi: 10.1016/j.ygyno.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Bild AH, Yao G, Chang JT, Wang Q, Potti A, Chasse D, et al. Oncogenic pathway signatures in human cancers as a guide to targeted therapies. Nature. 2006;439:353–357. doi: 10.1038/nature04296. [DOI] [PubMed] [Google Scholar]
- 12.Irizarry RA, Hobbs B, Collin F, Beazer-Barclay YD, Antonellis KJ, Scherf U, et al. Exploration, normalization, and summaries of high density oligonucleotide array probe level data. Biostatistics. 2003;4:249–264. doi: 10.1093/biostatistics/4.2.249. [DOI] [PubMed] [Google Scholar]
- 13.Bolstad BM, Irizarry RA, Astrand M, Speed TP. A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. Bioinformatics. 2003;19:185–193. doi: 10.1093/bioinformatics/19.2.185. [DOI] [PubMed] [Google Scholar]
- 14.Chen N, Kamath S, Newcomb J, Hudson J, Garbuzova-Davis S, Bickford P, et al. Trophic factor induction of human umbilical cord blood cells in vitro and in vivo. J Neural Eng. 2007;4:130–145. doi: 10.1088/1741-2560/4/2/013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marchion DC, Bicaku E, Turner JG, Daud AI, Sullivan DM, Munster PN. Synergistic interaction between histone deacetylase and topoisomerase II inhibitors is mediated through topoisomerase IIbeta. Clin Cancer Res. 2005;11:8467–8475. doi: 10.1158/1078-0432.CCR-05-1073. [DOI] [PubMed] [Google Scholar]
- 16.Holm S. A simple sequentially rejective multiple test procedure. Scand J Statist. 1979;6:65–70. [Google Scholar]
- 17.Britten RA, Perdue S, Eshpeter A, Merriam D. Raf-1 kinase activity predicts for paclitaxel resistance in TP53mut, but not TP53wt human ovarian cancer cells. Oncol Rep. 2000;7:821–825. doi: 10.3892/or.7.4.821. [DOI] [PubMed] [Google Scholar]
- 18.Cvijic ME, Chin KV. Effects of RIalpha overexpression on cisplatin sensitivity in human ovarian carcinoma cells. Biochem Biophys Res Commun. 1998;249:723–727. doi: 10.1006/bbrc.1998.9223. [DOI] [PubMed] [Google Scholar]
- 19.Helleman J, Jansen MP, Span PN, van Staveren IL, Massuger LF, Meijer-van Gelder ME, et al. Molecular profiling of platinum resistant ovarian cancer. Int J Cancer. 2006;118:1963–1971. doi: 10.1002/ijc.21599. [DOI] [PubMed] [Google Scholar]
- 20.Perego P, Giarola M, Righetti SC, Supino R, Caserini C, Delia D, et al. Association between cisplatin resistance and mutation of p53 gene and reduced bax expression in ovarian carcinoma cell systems. Cancer Res. 1996;56:556–562. [PubMed] [Google Scholar]
- 21.Zhu QY, Wang Z, Ji C, Cheng L, Yang YL, Ren J, et al. C6-ceramide synergistically potentiates the anti-tumor effects of histone deacetylase inhibitors via AKT dephosphorylation and alpha-tubulin hyperacetylation both in vitro and in vivo. Cell Death Dis. 2:e117. doi: 10.1038/cddis.2010.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Do NY, Lim SC. A low level of nicotine-induced chemoresistance in a KB cell line. Mol Med Report. 2008;1:55–60. [PubMed] [Google Scholar]
- 23.Hayakawa J, Ohmichi M, Kurachi H, Kanda Y, Hisamoto K, Nishio Y, et al. Inhibition of BAD phosphorylation either at serine 112 via extracellular signal-regulated protein kinase cascade or at serine 136 via Akt cascade sensitizes human ovarian cancer cells to cisplatin. Cancer Res. 2000;60:5988–5994. [PubMed] [Google Scholar]
- 24.Konstantinopoulos PA, Cannistra SA, Fountzilas H, Culhane A, Pillay K, Rueda B, et al. Integrated analysis of multiple microarray datasets identifies a reproducible survival predictor in ovarian cancer. PLoS One. 6:e18202. doi: 10.1371/journal.pone.0018202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Danial NN, Korsmeyer SJ. Cell death: critical control points. Cell. 2004;116:205–219. doi: 10.1016/s0092-8674(04)00046-7. [DOI] [PubMed] [Google Scholar]
- 26.Dejean LM, Martinez-Caballero S, Guo L, Hughes C, Teijido O, Ducret T, et al. Oligomeric Bax is a component of the putative cytochrome c release channel MAC, mitochondrial apoptosis-induced channel. Mol Biol Cell. 2005;16:2424–2432. doi: 10.1091/mbc.E04-12-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desagher S, Osen-Sand A, Nichols A, Eskes R, Montessuit S, Lauper S, et al. Bid-induced conformational change of Bax is responsible for mitochondrial cytochrome c release during apoptosis. J Cell Biol. 1999;144:891–901. doi: 10.1083/jcb.144.5.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuwana T, Mackey MR, Perkins G, Ellisman MH, Latterich M, Schneiter R, et al. Bid, Bax, and lipids cooperate to form supramolecular openings in the outer mitochondrial membrane. Cell. 2002;111:331–342. doi: 10.1016/s0092-8674(02)01036-x. [DOI] [PubMed] [Google Scholar]
- 29.Yang E, Zha J, Jockel J, Boise LH, Thompson CB, Korsmeyer SJ. Bad, a heterodimeric partner for Bcl-XL and Bcl-2, displaces Bax and promotes cell death. Cell. 1995;80:285–291. doi: 10.1016/0092-8674(95)90411-5. [DOI] [PubMed] [Google Scholar]
- 30.del Peso L, Gonzalez-Garcia M, Page C, Herrera R, Nunez G. Interleukin-3-induced phosphorylation of BAD through the protein kinase Akt. Science. 1997;278:687–689. doi: 10.1126/science.278.5338.687. [DOI] [PubMed] [Google Scholar]
- 31.Lizcano JM, Morrice N, Cohen P. Regulation of BAD by cAMP-dependent protein kinase is mediated via phosphorylation of a novel site, Ser155. Biochem J. 2000;349:547–557. doi: 10.1042/0264-6021:3490547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan Y, Demeter MR, Ruan H, Comb MJ. BAD Ser-155 phosphorylation regulates BAD/Bcl-XL interaction and cell survival. J Biol Chem. 2000;275:25865–25869. doi: 10.1074/jbc.M004199200. [DOI] [PubMed] [Google Scholar]
- 33.Zhou XM, Liu Y, Payne G, Lutz RJ, Chittenden T. Growth factors inactivate the cell death promoter BAD by phosphorylation of its BH3 domain on Ser155. J Biol Chem. 2000;275:25046–25051. doi: 10.1074/jbc.M002526200. [DOI] [PubMed] [Google Scholar]
- 34.Klumpp S, Selke D, Krieglstein J. Protein phosphatase type 2C dephosphorylates BAD. Neurochem Int. 2003;42:555–560. doi: 10.1016/s0197-0186(02)00174-2. [DOI] [PubMed] [Google Scholar]
- 35.Yang L, Omori K, Suzukawa J, Inagaki C. Calcineurin-mediated BAD Ser155 dephosphorylation in ammonia-induced apoptosis of cultured rat hippocampal neurons. Neurosci Lett. 2004;357:73–75. doi: 10.1016/j.neulet.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 36.Castino R, Peracchio C, Salini A, Nicotra G, Trincheri NF, Demoz M, et al. Chemotherapy drug response in ovarian cancer cells strictly depends on a cathepsin D-Bax activation loop. J Cell Mol Med. 2009;13:1096–1109. doi: 10.1111/j.1582-4934.2008.00435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsu CY, Bristow R, Cha MS, Wang BG, Ho CL, Kurman RJ, et al. Characterization of active mitogen-activated protein kinase in ovarian serous carcinomas. Clin Cancer Res. 2004;10:6432–6436. doi: 10.1158/1078-0432.CCR-04-0893. [DOI] [PubMed] [Google Scholar]
- 38.Peng DJ, Wang J, Zhou JY, Wu GS. Role of the Akt/mTOR survival pathway in cisplatin resistance in ovarian cancer cells. Biochem Biophys Res Commun. 2010;394:600–605. doi: 10.1016/j.bbrc.2010.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.