Abstract
Context
Little is known about rural clinicians’ perspectives regarding early childhood immunization delivery, their adherence to recommended best immunization practices, or the specific barriers they confront.
Purpose
To examine immunization practices, beliefs, and barriers among rural primary care clinicians for children in Oregon and compare those who deliver all recommended immunizations in their practices with those who do not.
Methods
A mailed questionnaire sent to all physicians, nurse practitioners, and physician assistants practicing primary care in rural communities throughout Oregon.
Findings
While 39% of rural clinicians reported delivering all childhood immunizations in their clinic, 43% of clinicians reported that they refer patients elsewhere for some vaccinations and 18% provided no immunizations in the clinic whatsoever. Leading reasons for referral include inadequate reimbursement, parental request, and storage and stocking difficulties. Nearly a third of respondents reported that they had some level of concern about the safety of immunizations, and 14% reported that concerns about safety were a specific reason for referring. Clinicians who delivered only some of the recommended immunizations were less likely than non-referring clinicians to have adopted evidence-based best immunization practices.
Conclusions
This study of rural clinicians in Oregon demonstrates the prevalence of barriers to primary-care-based immunization delivery in rural regions. While some barriers may be difficult to overcome, others may be amenable to educational outreach and support. Thus, efforts to improve population immunization rates should focus on promoting immunization “best practices” and enhancing the capacity of practices to provide immunizations and assuring that any alternative means of delivering immunizations are effective.
Keywords: child health, health services, immunizations, primary care, rural
Childhood immunizations are estimated to prevent 33,101 premature deaths and 13.6 million cases of vaccine preventable illnesses per birth cohort of approximately 4 million children born annually.1 Despite evidence of efficacy, challenges persist for comprehensive timely vaccination of children. The 2003 National Immunization Survey data found that children were undervaccinated a mean of 172 days for all vaccines combined during the first 2 years of life.2
Strong evidence identifies several barriers to immunization delivery. Barriers include patients’ socioeconomic status, underutilization of health care services, lack of parental knowledge about their children’s immunization status, underutilization of tracking systems by providers, immunization records scattered across multiple providers, and missed opportunities to immunize at non-preventive care visits.3
Other factors affecting the success of immunization delivery include the setting in which children receive their immunizations and geographic location. Research has shown that children immunized at public clinics are more likely to experience delays in immunizations than those immunized in their primary care provider’s office.4,5 Today, the majority of childhood vaccinations are delivered in primary care practice settings rather than in public health clinics, a trend encouraged by the Vaccines for Children (VFC) program, which provides no-cost vaccines to private clinicians for Medicaid-eligible and other children in need.6
Living in a rural community has a significant impact on immunization delivery in clinicians’ offices.7–9 Oregon consistently ranked in the bottom third of states for childhood immunization rates throughout the 2000s, with a nadir in 2005 when it ranked 47th out of 50.10 Internal reviews conducted by the Oregon Immunization Program, which provides publicly funded vaccines for approximately 60% of Oregon’s children through VFC and Federal Section 317 funds, indicate that rural children are less likely than those in urban and suburban regions to be adequately immunized. Reviews further demonstrate that rural clinicians are less likely to be active participants in the state’s immunization registry, Oregon Immunization ALERT. To date, information regarding potentially modifiable barriers to maximizing immunization rates for rural children is lacking. The purposes of this study were to 1) describe the diversity of providers serving children in rural Oregon; 2) describe rural Oregon clinicians’ approaches taken to delivery and tracking of early (0 to 36 months) childhood immunizations, including referrals; and 3) identify differences in immunization practices and perceptions about immunizations among referring and non-referring clinicians, including differences in their use of evidence-based immunization practices.
Methods
Study Setting and Target Population
We targeted clinicians practicing in rural communities throughout Oregon who provided primary care services to infants and children from birth through 3 years of age. Using membership databases from the Oregon Board of Medical Examiners and the Oregon Board of Nursing, we identified 1,158 physicians, nurse practitioners, and physician assistants who met eligibility criteria based upon their specialty (pediatrics, family medicine, general practice) and rural practice location. We used the 2004 Oregon Office of Rural Health definition of rural—“all geographic areas 10 or more miles from a population centroid of a population of 30,000 or more”11—to identify rural clinicians and also applied Rural Urban Commuting Area (RUCA) codes to further differentiate rural communities.11,12
Questionnaire Design
We developed a questionnaire using items from pre-existing clinician surveys, including the American Academy of Family Physicians (AAFP) 2004 and 2005 immunization survey13 and a statewide immunization practice survey conducted by the Washington Department of Health in 1998.14 Items queried clinicians’ approaches to ensuring that children in their practice are appropriately immunized, perceived barriers to delivering immunizations in the office setting, and use of evidence-based practices based on CDC-recommended guidelines published by the CDC Community Task Force on Community Preventive Services.15 Data were collected regarding clinician, practice, and community characteristics; personal perceptions of clinicians regarding childhood immunizations; and responses to clinical vignettes to identify immunization delivery practices in the face of minor illnesses when vaccinations are recommended. Immunization practices were assessed only among immunizing clinicians.
Survey Methods
The survey was distributed to 1,158 identified rural Oregon clinicians in December 2004 through February 2005. A subset of 328 clinicians for whom email addresses could be obtained received an electronic survey, in part to ascertain the effectiveness of this mode of distribution. The remainder received a survey via standard mail. Two weeks later, a follow-up reminder postcard was sent via US Mail to all clinicians except those with Return To Sender addresses (N=23). A reminder email was also sent to the email subset at the same time. Three weeks after the initial mailing the survey was re-sent via US Priority Mail to all practitioners who had not yet responded. Finally, the clinics of all non-respondents whose office phone numbers could be identified received a phone call from trained study personnel to ascertain eligibility status, and to invite eligible clinicians to respond. The Oregon Health & Science University (OHSU) Institutional Review Board approved this study.
Exclusions From Analysis
Respondents were deemed ineligible if they did not see children 0–36 months; if their stated primary specialty was anything other than family medicine, general medicine, or pediatrics; or if they had moved out of the state or away from a rural community as previously defined. Returned surveys were also excluded if there was a preponderance of missing information precluding meaningful analysis. For example, 6 subjects were excluded from analyses based upon the provider’s immunization referral status, because they did not indicate whether they provided all, some or no immunizations to the target population.
Statistical Analysis
Descriptive statistics were computed to describe the composition of the sample and response frequencies. Chi-square, Fisher’s exact and t tests were conducted to determine statistical associations between key variables of interest.
Results
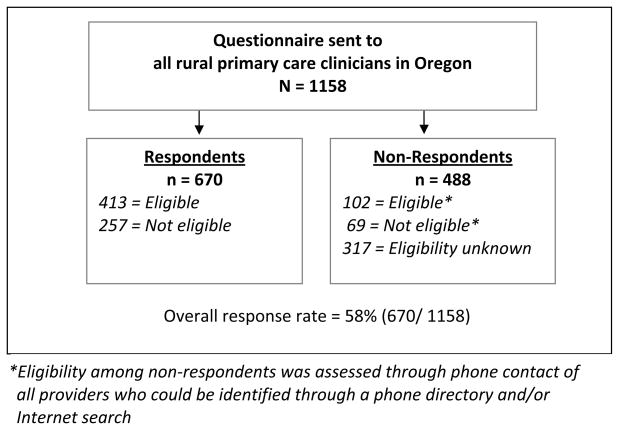
The overall response rate was 58% (Figure 1). Among 670 returned surveys, 413 were eligible for analysis—providing primary care services for children ages 0 to 36 months. The eligibility of the non-respondents (42%) is described in Figure 1. The number of responses to individual survey items varied slightly due to skipped items by some respondents. Two-thirds of the respondents were physicians and one-third were non-physician clinicians (Table 1). Consistent with medical practice in rural communities, the majority were in family medicine (82%) or general practice (3%), with pediatricians and other pediatric clinicians comprising the remaining 15% of respondents. The majority of clinicians had been in practice in their current community 10 or fewer years (range 0.5 to 50 years), and they were in physician-owned private practices (56%). Thirteen percent of respondents were in hospital-owned practices and 4% were employees of university-affiliated practices. Additionally, 18% practiced in federally designated Rural Health Clinics, 11% in Federally Qualified Health Centers, and 1% of respondents reported practicing in Indian Health Service and tribal practices. While all eligible respondents were in rural practices based upon the Oregon Office of Rural Health definition, further categorization using RUCA codes demonstrated that 18% practiced in metropolitan areas, 56% in large rural towns, 15% in small rural towns, and 11% in isolated rural locations.
Figure 1.
Survey response details
Table 1.
Demographic Characteristics and Immunization Referral and Delivery Practices
| Characteristic | Respondent Totals N (% by column, N=413) | Deliver all immunizations N (% by row characteristic) | Delivers some/refers some immunizations N (% by row characteristic) | Delivers no immunizations N (% by row characteristic) | P value |
|---|---|---|---|---|---|
| Total N1 | 413 | 158 (39) | 177 (43) | 72 (18) | |
| Discipline (N=406) | .45 | ||||
| MD/DO | 278 (68) | 108 (39) | 121 (44) | 46 (17) | |
| NP | 91 (22) | 34 (39) | 40 (45) | 14 (16) | |
| PA | 43 (10) | 16 (37) | 15 (35) | 12 (28) | |
| Specialty (N=407) | <.0001 | ||||
| Family Medicine | 340 (82) | 121 (36) | 150 (45) | 63 (19) | |
| Pediatrics | 61 (15) | 37 (61) | 22 (36) | 2 (3) | |
| General Practice | 12 (3) | 0 (0) | 5 (42) | 7 (58) | |
| Years practicing in Community (N=406) | .49 | ||||
| ≤ 5 | 150 (37) | 65 (44) | 62 (42) | 21 (14) | |
| 6 – 10 | 94 (23) | 35 (38) | 43 (47) | 14 (15) | |
| 11 – 20 | 96 (23) | 32 (34) | 41 (44) | 21 (22) | |
| > 20 | 71 (17) | 26 (37) | 29 (41) | 16 (23) | |
| Practice Ownership/Practice Designation (>1 may be selected) (N=385) | |||||
| Private (Physician or physican group) | 220 (56) | 75 (34) | 100 (46) | 43 (20) | .03 |
| Hospital | 50 (13) | 18 (37) | 27 (55) | 4 (8) | .14 |
| University-affililated | 17 (4) | 9 (60) | 6 (40) | 0 (0) | .12 |
| Rural Health Clinic | 72 (18) | 25 (35) | 37 (52) | 9 (13) | .31 |
| FQHC | 44 (11) | 28 (64) | 14 (32) | 2 (5) | .00 |
| Indian Health Service | 5 (1) | 4 (80) | 1 (20) | 0 (0) | .20 (F)3 |
| Tribal | 5 (1) | 2 (40) | 3 (60) | 0 (0) | .85 (F)3 |
| Other entity | 42 (11) | 18 (44) | 15 (37) | 8 (20) | .58 |
| Community Rurality (RUCA2-based) (N=409) | .00 | ||||
| Metro | 76 (18%) | 43 (58) | 28 (38) | 3 (4) | |
| Large rural town | 230 (56%) | 83 (37) | 102 (45) | 42 (19) | |
| Small rural town | 60 (15%) | 18 (31) | 27 (46) | 14 (24) | |
| Isolated rural town | 47 (11%) | 14 (30) | 20 (43) | 13 (28) |
Six of the 413 subjects eligible for analysis were missing data about referring vs not referring patients for immunizations, so the overall N for the related columns is 407. Number of valid responses may vary slightly by item.
Rural-Urban Commuting Area codes. http://www.ers.usda.gov/Data/RuralUrbanCommutingAreaCodes/
Fisher’s exact test used to calculate the P value due to small cell size
Referrals for immunizations
Of the 413 eligible respondents, 407 (98.5%) provided information about their immunization referral practices and form the group we focused on with the remainder of our analyses. As shown in Table 1, 39% of rural clinicians reported delivering all immunizations and referred no patients to outside sources for receipt of immunizations. Over two-fifths (43%) of clinicians report delivering some, but not all, immunizations in their clinic, and referring children for the remainder; and nearly 1 in 5 clinicians referred all children to outside sources for immunizations. Two characteristics were particularly associated with the likelihood of providing all early childhood immunizations: provider specialty and rurality. Nearly two-thirds of pediatricians provided all immunizations and did not refer out, compared with approximately one-third of family practitioners (P < .0001). Rurality was also strongly associated with the provision of immunizations, with a decline in immunization delivery as the local area becomes more rural (P < .01). Medical discipline (MD/DO, NP, or PA) and years practicing in the community were not related to providers’ delivery of all, some, or no immunizations in their practices.
Although over 80% of respondents reported that children received some or all immunizations in their clinic, 90% noted that children received immunizations at the County Health Department and 30% reported children receiving immunizations at a Community Health Center. We sought to examine differences in immunization practices and beliefs among those providers who give some but not all immunizations in their clinics (referred to hereafter as “referring” clinicians), compared to those who deliver all immunizations (“non-referring” clinicians). Thus, results presented below reflect the responses of clinicians who provide all or some immunizations in their practices (n = 335).
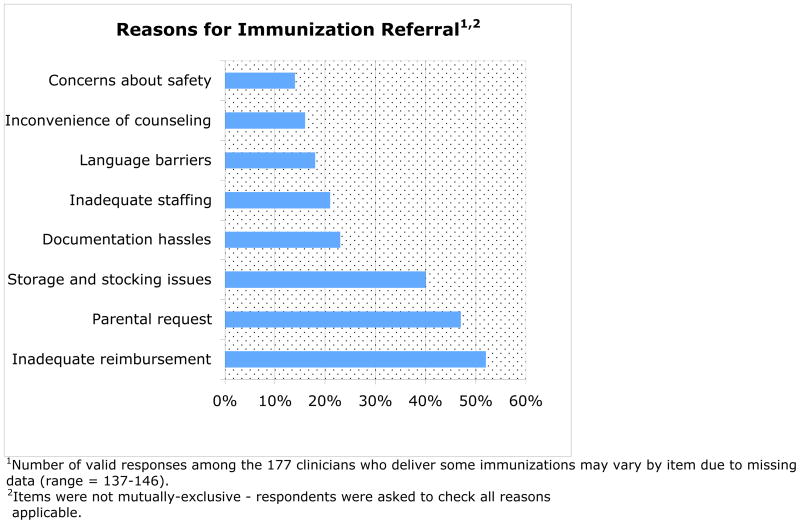
Reasons for immunization referrals
Figure 2 lists the leading reasons clinicians refer immunizations, ranked by percentages. Inadequate reimbursement (52%), parental request (47%) and storage and stocking issues (40%) were the most often cited reasons. Other notable reasons included documentation hassles, inadequate staffing, language barriers, the inconvenience of counseling about vaccines, and concerns about vaccine safety.
Figure 2.
Reasons for immunization referral (“Referring” Clinicians, total N=177)
Vaccines delivered and reasons for not delivering some vaccinations
Among clinicians who routinely provided at least some immunizations to children within their practices (n=335), nearly all (98%) provided DTaP, IPV, MMR, Hib, and Hepatitis B to their patients. In contrast, referral was significantly more common for varicella (82%), pneumococcus (86%) and influenza (6%). Hepatitis A vaccine, recommended for all children over age 2 in Oregon since1999,16 was routinely delivered by only 64% of these clinicians.
Reasons for not delivering vaccines varied across the commonly referred vaccines (Table 2). For instance, among those not providing varicella immunizations, 73% listed the difficulty of properly storing the vaccine. An absence of school requirements was a reason given among 46% and 56% of clinicians who did not routinely deliver pneumococcus and hepatitis A, respectively. Nearly one-fifth stated they considered recommendations for hepatitis A and pneumococcus vaccines to be too new. Less than 3% cited the inconvenience of administering vaccines or vaccine-related liability concerns as reasons why they elected to forgo administering certain individual vaccines.
Table 2.
Antigen-Specific Reasons for Not Delivering Vaccines1
| Varicella | Pneumococcus | Influenza | Hep A | |
|---|---|---|---|---|
| Total not given | 37 | 37 | 65 | 117 |
| Reason why vaccine not given* | N (%) | N (%) | N (%) | N (%) |
| Cost of vaccine to family | 3 (8) | 8 (22) | 6 (9) | 22 (19) |
| Reimbursement for vaccine | 3 (8) | 6 (16) | 4 (6) | 15 (13) |
| Problems with vaccine storage administration | 27 (73) | 1 (3) | 1 (2) | 9 (8) |
| Schools do not require vaccine | 1 (3) | 17 (46) | 13 (20) | 66 (56) |
| Vaccine-related liability concerns | 1 (3) | 1 (3) | 2 (3) | 2 (2) |
| Inconvenience of administering | 0 (0) | 1 (3) | 4 (6) | 2 (2) |
| Marginal value | 1 (3) | 5 (14) | 9 (14) | 26 (22) |
| Parental opposition | 1 (3) | 3 (8) | 11 (17) | 21 (18) |
| Recommendations still too new | 1 (3) | 7 (19) | 4 (6) | 17 (15) |
| Lack of availability | 0 (0) | 7 (19) | 39 (60) | 3 (3) |
| Other | 6 (16) | 8 (22) | 7 (11) | 11 (9) |
| No reason given | 2 (5) | 2 (5) | 3 (5) | 8 (7) |
Note: Respondents were asked to check all reasons applicable, which accounts for item totals exceeding 100%.
Use of evidence-based practices
Adherence to evidence-based best practices in immunization care differed by clinician referral status (Table 3). Providers who gave all recommended immunizations in their practice were more likely than those who delivered only some immunizations to adhere to each of the best practice measures, with significant differences for participation in VFC (P = .00); having a system for tracking patient immunization status (P = .01); and having conducted a review of the immunization status of the clinic’s patient population (P < .0001). Best practice measures not reaching significant differences included screening patients’ immunization status at all visits (P = .06) and sending out patient reminders (P = .08). In addition, non-referring clinicians tended to adopt a broad range of best practices more commonly than referring clinicians, demonstrated by their increased likelihood (77% vs 59%) of incorporating 5 or more of these evidence-based best practices.
Table 3.
Evidence-Based Best Practices Measures by Referral Status
| Best Practice | Deliver all immunizations % of N1 | Deliver some/refer some immunizations % of N2 | P value |
|---|---|---|---|
| Offer vaccine-only visits | 84 | 80 | .36 |
| Participate in VFC3 | 94 | 82 | .00 |
| Give as many shots as indicated | 72 | 67 | .39 |
| Screen immunization status at all visits | 62 | 51 | .06 |
| Have a system to identify children who are behind on immunizations | 69 | 54 | .01 |
| Send out patient reminders (phone or mail) | 53 | 43 | .08 |
| Have conducted a review of immunization status of child population | 47 | 23 | <.0001 |
| Incorporates 5 or more best practices | 77 | 59 | .00 |
N range = 143–158.
N range = 157–177.
Excludes 31 subjects who responded “don’t know.”
Among clinicians providing all or some vaccines (N =335), 71% submitted data to ALERT and 66% reported accessing ALERT to check immunizations. Participation in the Vaccines for Children (VFC) program was strongly associated with submitting data and accessing immunization records within the ALERT system.
Clinician perceptions and beliefs about immunizations
Participating clinicians did not believe that immunizations were any less important today than 10 years ago. Yet, a relatively high percentage of respondents were concerned about the safety of immunizations, a finding that did not differ by clinicians’ immunization referral status (Table 4). Approximately one-fifth of referring and non-referring clinicians reported reluctance to incorporate new vaccines into their practice. A high proportion of respondents reported a belief that immunizations are the main reason that parents come in for well child visits, and non-referring clinicians held this belief more frequently than referring clinicians. Finally, more than 80% of all respondents agreed that electronic record systems could streamline immunization delivery.
Table 4.
Perceptions About Immunizations by Referral Status
| Deliver all immunizations % of N1 | Deliver some/refer some immunizations % of N2 | P value | |
|---|---|---|---|
| Safety of immunizations concerns me | 30 | 27 | .54 |
| Usually need more info on vaccine safety | 16 | 12 | .34 |
| Reluctant to incorporate new vaccines | 16 | 22 | .14 |
| Receipt of immunizations is the main reason that parents come for well-child visits | 73 | 62 | .03 |
| A computer system can streamline immunization delivery | 85 | 80 | .21 |
N range =141–154.
N range = 162–174.
Clinician vaccination practices during minor illnesses
We asked about delivering DTaP vaccine to 4-month-old and 12-month-old children, and the 12-month MMR in the face of 5 individual clinical presentations: a fever to 102.5 F, URI (afebrile), gastroenteritis, persistent otitis media, and bronchiolitis. Neither the non-referring nor referring group of clinicians reported strict adherence to current recommendations about vaccine delivery in the face of acute minor illness.17,18 Only in the face of a URI do clinicians follow guidelines to proceed with immunization, avoiding a “missed opportunity.”
Discussion
The results of our survey help shed more light on the issues facing rural clinicians in Oregon, point to key areas for improvement of childhood immunization delivery, and have implications for other rural settings in the United States.
Referrals for immunizations
We found that nearly 20% of rural primary care clinicians in Oregon referred all children in their practice for immunizations, and an additional 43% referred children for some immunizations even though immunizations are among the most fundamental preventive health services offered to children. This degree of referral was occurring despite widespread recommendations targeted at ensuring that immunization delivery occurs within primary care practices and the “medical home.” The national Vaccines for Children program started in the 1990s has been generally shown to reduce referrals to public health clinics.18,19 There is evidence that these efforts have been effective toward improving immunization rates. Private practice clinicians vaccinate most US children (60.4%) as compared to public health departments (24.2%) and mixed public/private venues (14.29%).6
Barriers to immunizations
Despite efforts to align immunization delivery with primary care practice, in the face of growing recommendations to vaccinate children concerns about clinicians’ ability to sustain this role seems to be growing.20 Our study, conducted during the 10th anniversary of the VFC program, suggests that such concerns may persist, particularly among rural practitioners.
This study affirmed several known disincentives to immunization delivery by clinicians and uncovered several additional factors influencing vaccination referral. Inadequate reimbursement for vaccine delivery should not be ignored. Studies report that reimbursement is often inadequate even to cover the fixed costs of immunizing children.20,21 Stocking and storing of vaccines can be burdensome and cost-ineffective to the practice, particularly in low-volume settings.22 The clinicians in our study reported lack of availability of pneumococcal and influenza vaccines as a barrier to adhering to immunization schedules. During the last decade there have been multiple disruptive shortages of vaccines, resulting in parental concern and stress on primary care practices.23 Difficulty in maintaining an inventory of childhood vaccines has been exacerbated by the dramatic increase in the number of recommended immunizations for children and adolescents. Since 1995 the number of recommended immunizations for children and adolescents increased from 9 vaccines to 18 vaccines in 2008.24 Reimbursement for delivery of immunizations has not kept pace with costs, resulting in a decline in the ratio of reimbursement to cost for private physicians.20,25
The majority of children are eligible for publicly subsidized vaccines with approximately 52% of Oregon’s children eligible for VFC and an additional 6% qualified for Section 317 vaccines.26 While children can now be protected from an increasingly long list of diseases, states and the federal government are increasingly challenged by the additional number and cost of recommended pediatric vaccines while trying to maintain adequate funding for publicly supplied vaccines. The private sector costs to purchase the recommended vaccines for children from birth to age 18 years have increased from $600 in 2000 to over $1500 per child in 2008.20 Even with government-supplied and subsidized vaccines, practices must still cover administration and vaccine handling costs, which may be particularly challenging for rural practices.
Best Practices and opportunities for improvement
Our study reports a strong association among clinicians delivering all immunizations and their compliance with best immunization practices. This finding is consistent with the general tenet of clinical quality improvement that adopting the entire package of quality measures for a given initiative or condition results in higher levels of performance.27 Nonetheless, there is room for improvement among all immunizing clinicians in using immunization registries, screening the immunization status of children at all visits, sending out patient reminders, reviewing the up-to-date status of children in the practice, giving as many shots as indicated, and encouraging the delivery of vaccinations during acute illness.
Suggestions for future study
This study also revealed several other important challenges that could be addressed within rural practice settings beyond cost and payment issues. The frequency with which providers listed language barriers, documentation hassles, and the inconvenience of counseling about vaccines (Figure 2) was noteworthy. Clinicians’ perceptions of inefficiencies in communication as barriers to immunization delivery merit further exploration in future intervention studies, particularly in rural clinical settings.
In our study nearly a third of providers reported concern about the safety of childhood immunizations and about one-sixth of clinicians reported they needed more information about vaccine safety. Clinicians in busy practices who for whatever reason have concerns about vaccine safety may be more apprehensive about providing immunizations they lack knowledge of or trust in. It is likely that for at least some clinicians, these concerns may lead to patient under-immunization. More recently, a 2007 national survey of primary care physicians (family medicine and pediatrics) regarding adoption of rotavirus vaccination found that 25% of family medicine physicians and 9% of pediatricians had safety concerns about the vaccine.8 A better understanding of the impact of provider vaccine concerns on immunization delivery may shed light on specific provider interventions.
We found that there is a reluctance to deliver immunizations to children experiencing an acute illness. This represents a missed opportunity to immunize. Interventions to increase the comfort level and acceptance of immunizations by clinicians and parents at times of an acute illness are needed.
Our study and others have documented that it takes the entire community and health care system to keep children up to date with immunizations. This requires coordination and collaboration between primary health care clinicians and their county health departments. For example, during this cooperative study involving a practice-based research network and the statewide immunization program, we learned of instances when vaccines were shared between the public and private vaccine providers at times of shortages. Identifying and disseminating exemplar models of cooperation and coordination between the private and public health sector could lead to further improvements.
Strengths and Limitations
A strength of our study is that we surveyed all rural primary care clinicians caring for children—crossing disciplines and primary care specialties. Several limitations should be noted. First, we do not know what the eligible non-respondents would have reported. This group of 102 individuals represents 8.8% of the surveyed population. We were unable to determine the eligibility of 27% (N=317) of the surveyed clinicians. The fact that we were unable to locate these individuals in the phone directory or through an Internet search makes it unlikely that they are actively practicing medicine in Oregon. Our response rate of 58% is typical for mailed physician surveys, which average a response rate of 54% to 61%.28,29 A second limitation is that as with most surveys, the data were self-reported by clinicians. A second phase in our rural Oregon Immunization Initiative consisted of a mixed-methods detailed evaluation of a subset of 11 primary care clinics regarding childhood immunization practices and barriers. Preliminary analysis indicates that the statewide survey data are consistent with our in-depth study. It was beyond the scope of this study to determine if the increased barriers and decreased adoption of best practices result in reduced immunization rates in these practices. A third limitation is that immunization recommendations have included rotavirus vaccine since 2006. We confined our study to early childhood immunization and did not study the clinician practices regarding adolescent immunization recommendations, which have changed significantly over the last 5 years.
Conclusion
Rural clinicians face a number of challenges in providing immunizations to children, and our findings suggest that some are responding to these challenges by relinquishing responsibility for immunizing the children in their practices. This possibility would seem to be in potential conflict with the basic tenets of the highly touted medical home model for primary care.30 One study has already demonstrated that some providers, particularly family physicians, have considered ceasing all children’s immunization delivery.20
Vaccination delivery barriers, including financial pressures, increasingly complicated immunization schedules, vaccine storage challenges, vaccine shortages, concerns about immunization safety, and other related factors highlighted in this study may ultimately force a new model of immunization delivery within rural communities. Recent challenges regarding the delivery of adolescent immunizations have pointed to a need for a community-wide approach to immunization delivery.31 Whatever the model of tomorrow, our findings suggest that efforts to address immunization practice barriers should include more fully engaging, educating about, and responding to the needs of rural primary care clinicians, promoting links between providers and their local public health departments or other clinics to promote care coordination around immunization delivery. At risk may be the children who live in these rural communities and who may have few alternatives for vaccination.
References
- 1.Zhou F, Santoli J, Messonnier ML, et al. Economic evaluation of the 7-vaccine routine childhood immunization schedule in the United States, 2001. Arch Pediatr Adolesc Med. 2005 Dec;159(12):1136–1144. doi: 10.1001/archpedi.159.12.1136. [DOI] [PubMed] [Google Scholar]
- 2.Luman ET, Barker LE, Shaw KM, McCauley MM, Buehler JW, Pickering LK. Timeliness of childhood vaccinations in the United States: days undervaccinated and number of vaccines delayed. Jama. 2005 Mar 9;293(10):1204–1211. doi: 10.1001/jama.293.10.1204. [DOI] [PubMed] [Google Scholar]
- 3.Santoli JM, Setia S, Rodewald LE, O'Mara D, Gallo B, Brink E. Immunization pockets of need: science and practice. Am J Prev Med. 2000 Oct;19(3 Suppl):89–98. doi: 10.1016/s0749-3797(00)00209-9. [DOI] [PubMed] [Google Scholar]
- 4.Hueston WJ, Mainous AG, 3rd, Palmer C. Delays in childhood immunizations in public and private settings. Arch Pediatr Adolesc Med. 1994 May;148(5):470–473. doi: 10.1001/archpedi.1994.02170050028005. [DOI] [PubMed] [Google Scholar]
- 5.Groom H, Kolasa M, Wooten K, Ching P, Shefer A. Childhood immunization coverage by provider type. J Public Health Manag Pract. 2007 Nov–Dec;13(6):584–589. doi: 10.1097/01.PHH.0000296134.70014.b0. [DOI] [PubMed] [Google Scholar]
- 6.Orenstein WA, Douglas RG, Rodewald LE, Hinman AR. Immunizations in the United States: success, structure, and stress. Health Aff (Millwood) 2005 May–Jun;24(3):599–610. doi: 10.1377/hlthaff.24.3.599. [DOI] [PubMed] [Google Scholar]
- 7.Bergus GR, Ernst ME, Sorofman BA. Physician perceptions about administration of immunizations outside of physician offices. Prev Med. 2001 Mar;32(3):255–261. doi: 10.1006/pmed.2000.0801. [DOI] [PubMed] [Google Scholar]
- 8.Kempe A, Patel MM, Daley MF, et al. Adoption of rotavirus vaccination by pediatricians and family medicine physicians in the United States. Pediatrics. 2009 Nov;124(5):e809–816. doi: 10.1542/peds.2008-3832. [DOI] [PubMed] [Google Scholar]
- 9.Mainous AG, 3rd, Hueston WJ. Factors influencing the use of primary care physicians and public health departments for childhood immunization. J Ky Med Assoc. 1993 Sep;91(9):394–398. [PubMed] [Google Scholar]
- 10.National state, and urban area vaccination coverage among children aged 19–35 months--United States, 2005. MMWR Morb Mortal Wkly Rep. 2006 Sep 15;55(36):988–993. [PubMed] [Google Scholar]
- 11.Office of Rural Health O. [Accessed January 19, 2009.];What is "Rural" in Oregon. Available at: http://www.ohsu.edu/oregonruralhealth/
- 12.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005 Jul;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Temte JLYH, Schoof BK. Immunization Practices of Family Physicians--2004 and 2005. 40th National Immunization Conference; Atlanta, GA. 2006. [Google Scholar]
- 14.Gaudino JA, deHart MP, Cheadle A, et al. Childhood immunization registries: gaps between knowledge and action among family practice physicians and pediatricians in Washington state, 1998. Arch Pediatr Adolesc Med. 2002 Oct;156(10):978–985. doi: 10.1001/archpedi.156.10.978. [DOI] [PubMed] [Google Scholar]
- 15.Briss PA, Rodewald LE, Hinman AR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med. 2000 Jan;18(1 Suppl):97–140. doi: 10.1016/s0749-3797(99)00118-x. [DOI] [PubMed] [Google Scholar]
- 16.Prevention of hepatitis A through active or passive immunization: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1999 Oct 1;48(RR–12):1–37. [PubMed] [Google Scholar]
- 17.Kroger AT, Atkinson WL, Marcuse EK, Pickering LK. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006 Dec 1;55(RR–15):1–48. [PubMed] [Google Scholar]
- 18.Szilagyi PG. Measuring the success of the U.S. childhood immunization system. Am J Prev Med. 2001 May;20(4 Suppl):3–5. doi: 10.1016/s0749-3797(01)00288-4. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerman RK, Mieczkowski TA, Mainzer HM, et al. Effect of the Vaccines for Children program on physician referral of children to public vaccine clinics: a pre-post comparison. Pediatrics. 2001 Aug;108(2):297–304. doi: 10.1542/peds.108.2.297. [DOI] [PubMed] [Google Scholar]
- 20.Freed GL, Cowan AE, Clark SJ. Primary care physician perspectives on reimbursement for childhood immunizations. Pediatrics. 2008 Dec;122(6):1319–1324. doi: 10.1542/peds.2008-2033. [DOI] [PubMed] [Google Scholar]
- 21.Berman S. Is our vaccine system at risk for a future financial "meltdown?". Pediatrics. 2008 Dec;122(6):1372–1373. doi: 10.1542/peds.2008-2881. [DOI] [PubMed] [Google Scholar]
- 22.Guttmann A, Manuel D, Dick PT, To T, Lam K, Stukel TA. Volume matters: physician practice characteristics and immunization coverage among young children insured through a universal health plan. Pediatrics. 2006 Mar;117(3):595–602. doi: 10.1542/peds.2004-2784. [DOI] [PubMed] [Google Scholar]
- 23.Hinman AR, Orenstein WA, Santoli JM, Rodewald LE, Cochi SL. Vaccine shortages: history, impact, and prospects for the future. Annu Rev Public Health. 2006;27:235–259. doi: 10.1146/annurev.publhealth.27.021405.102248. [DOI] [PubMed] [Google Scholar]
- 24.CDC. Recommended immunization schedules for persons aged 0-18 years: United States, 2008. MMWR Morb Mortal Wkly Rep. 2008;57(1):Q-1–Q-4. [Google Scholar]
- 25.Glazner JE, Beaty BL, Pearson KA, Berman S. The cost of giving childhood vaccinations: differences among provider types. Pediatrics. 2004 Jun;113(6):1582–1587. doi: 10.1542/peds.113.6.1582. [DOI] [PubMed] [Google Scholar]
- 26.CDC. [Accessed July 12, 2009.];VFC: Populations Estimates Survey (PES) Available at: http://www.cdc.gov/vaccines/programs/vfc/projects/surveys/pop-estimates.htm.
- 27.Nolan T, Berwick DM. All-or-none measurement raises the bar on performance. Jama. 2006 Mar 8;295(10):1168–1170. doi: 10.1001/jama.295.10.1168. [DOI] [PubMed] [Google Scholar]
- 28.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997 Oct;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 29.Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res. 2001 Feb;35(6):1347–1355. [PMC free article] [PubMed] [Google Scholar]
- 30.The medical home. Pediatrics. 2002 Jul;110(1 Pt 1):184–186. [PubMed] [Google Scholar]
- 31.Szilagyi PG, Rand CM, McLaurin J, et al. Delivering adolescent vaccinations in the medical home: a new era? Pediatrics. 2008 Jan;121( Suppl 1):S15–S24. doi: 10.1542/peds.2007-1115C. [DOI] [PubMed] [Google Scholar]