Abstract
MPT83 (Rv2873), a surface lipoprotein excreted in the culture of Mycobacterium tuberculosis, is immunoreactive in antibody assays in humans and animals and provides protection as a combined DNA vaccine in mice and cattle. This study was undertaken to determine the reactivity of MPT83 in T helper 1 (Th1)-cell assays, i.e., antigen-induced proliferation and gamma interferon (IFN-γ) secretion, using peripheral blood mononuclear cells (PBMCs) obtained from Mycobacterium bovis bacillus Calmette-Guérin (BCG)-vaccinated and/or M. tuberculosis-infected healthy subjects. PBMCs were tested with complex mycobacterial antigens and pools of synthetic peptides corresponding to MPT63, MPT83, MPB70, LppX, PPE68, CFP10, and ESAT-6. The results showed that MPT83 is among the strongest Th1 cell antigens of M. tuberculosis, and it was recognized equally strongly by BCG-vaccinated and by BCG-vaccinated and M. tuberculosis-infected healthy subjects. Furthermore, HLA heterogeneity of the responding donors suggested that MPT83 was presented to Th1 cells by several HLA-DR molecules. The analysis of the mature MPT83 sequence (amino acids [aa] 1 to 220) and its 14 overlapping synthetic peptides for binding prediction to HLA class II molecules and actual recognition of the peptides by PBMCs from HLA-DR-typed subjects in antigen-induced proliferation and IFN-γ assays suggested that Th1 cell epitopes were scattered throughout the sequence of MPT83. In addition, the HLA-promiscuous nature of at least three peptides, i.e., P11 (aa 151 to 175), P12 (aa 166 to 190), and P14 (aa 196 to 220), was suggested by HLA-DR binding predictions and recognition by HLA-DR heterogeneous donors in Th1 cell assays. These results support the inclusion of MPT83 in an antigen cocktail to develop a new antituberculosis vaccine.
INTRODUCTION
Tuberculosis (TB) is a major global health problem, and in spite of international efforts to control the disease, TB remains a major challenge to global public health in the 21st century (69). The most recent estimates by the World Health Organization suggest that the worldwide incidence of TB is increasing, with 9.4 million new cases of TB and 1.7 million deaths in 2009 (69). A combination of better diagnostics, drugs, and vaccines is expected to dramatically alter the TB epidemic (28, 35), but it is suggested that vaccines will have the greatest impact in reducing the incidence of disease (35). Mycobacterium bovis bacillus Calmette-Guérin (BCG), the currently used vaccine in humans to protect against TB, has been in use since 1921. However, it has several disadvantages, including the lack of consistent protection in different parts of the world (31), and may cause TB in immunocompromised subjects, including AIDS patients, who are usually at a very high risk of developing TB (15). Thus, there is an urgent need to identify new and safe vaccine candidates to achieve the global control of TB.
The culture filtrate of Mycobacterium tuberculosis (MT-CF) contains secreted and excreted proteins of M. tuberculosis (37), and immunization with MT-CF protects mice and guinea pigs against challenge with virulent M. tuberculosis (14, 17). Furthermore, the protective potentials of several MT-CF proteins, e.g., Ag85 complex, ESAT-6, CFP10, MPT-63, MPT-64, MPT-83, and MPB70, etc., have been demonstrated in animal models of TB (20, 33, 39, 58, 64, 70, 71). All of these antigens, except MPT83, have also been shown to be immunodominant in humans for recognition by T helper 1 (Th1) cells in an HLA-promiscuous manner and induce the release of Th1 cytokines that correlate with protective immunity (40, 41, 42, 59, 65).
Although MPT83 has been studied previously for antibody responses in animals and humans (16, 30, 32) and found to be protective as a combined DNA vaccine in mice and cattle (20, 64), the information on Th1 cell reactivity of this protein in humans, which is considered the hallmark of protective immunity in TB (3, 7, 8, 18, 19, 61), is nonexistent, particularly in M. bovis BCG-vaccinated and M. tuberculosis-infected and noninfected healthy humans. In this study, the Th1 cell reactivity of MPT83 was studied in such a group of subjects living in Kuwait by using peripheral blood mononuclear cells (PBMCs) and a pool of overlapping synthetic peptides covering the sequence of the full-length MPT83 protein. In addition, for comparative evaluation, PBMCs were also tested with complex mycobacterial antigens and several major antigens of M. tuberculosis, i.e., ESAT-6 (Rv3875, ESXA), CFP10 (Rv3874, ESXB), PPE68 (Rv3873), MPB70 (Rv2875), LppX (Rv2945c), and MPT63 (Rv1926c). Furthermore, the permissive and promiscuous nature of MPT83 and its peptides was determined by predicting their binding to several alleles of frequently expressed HLA-DR molecules using computational programs (24, 56, 62, 67). In addition, the non-HLA-restricted presentation of MPT83 to T cells was determined by studying the actual recognition of the peptides by PBMCs obtained from HLA-DR heterogeneous subjects in Th1 cell assays.
MATERIALS AND METHODS
Complex mycobacterial antigens and synthetic peptides.
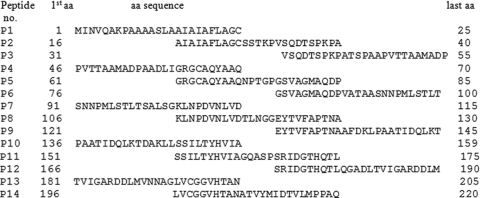
The complex mycobacterial antigens used in this study were irradiated whole-cell M. tuberculosis H37Ra and M. bovis BCG (29, 50), M. tuberculosis culture filtrate (MT-CF) enriched for secreted antigens, and purified M. tuberculosis cell walls (MT-CW) (48). MT-CF and MT-CW were kindly provided by J. T. Belisle (Colorado State University, Fort Collins, CO). Fourteen synthetic peptides (25-mers overlapping neighboring peptides by 10 residues) spanning the sequence of full-length MPT83 (Fig. 1) were purchased from Thermo Hybaid GmbH, Ulm, Germany. These peptides, as well as the synthetic peptides covering the sequences of MPT63 (43), MPB70 (10), LppX (5), PPE68 (48), ESAT-6 (48), and CFP10 (53), were synthesized using fluorenylmethoxycarbonyl (Fmoc) chemistry, as described previously (11, 49). The stock concentrations (5 mg/ml) of the peptides were prepared in normal saline (0.9%) by vigorous pipetting, and the working concentrations were prepared by further dilution in tissue culture medium RPMI-1640, as previously described (54).
Fig. 1.
Fourteen (P1 to P14) 25-mer synthetic peptides covering the entire sequence of MPT83. The peptides overlap each other by 10 aa. The single-letter designations for amino acids are used.
Study subjects and isolation of PBMCs.
The study subjects were M. bovis BCG-vaccinated healthy adults randomly selected from the group of blood donors at the Central Blood Bank, Kuwait. The primary immunization with BCG was performed at 4 1/2 years of age, followed by M. tuberculosis purified protein derivative (PPD) skin test at 13 years of age and a booster immunization with BCG in PPD skin test-negative subjects. At the time of blood collection, all the donors were PPD skin test positive (>10 mm, as determined with tuberculin PPD RT 23 from the Statens Serum Institute, Copenhagen, Denmark). PBMCs were isolated from the buffy coats of healthy donors by using standard procedures (9, 44). In brief, each buffy coat was diluted with warm tissue culture medium (RPMI 1640) at a ratio of 1:2 and gently mixed. Two volumes of the diluted buffy coat was loaded on top of 1 volume of a Lymphoprep gradient (Pharmacia Biotech, Uppsala, Sweden). After centrifugation, the white ring of PBMCs between the plasma and the Lymphoprep was removed and washed three times with RPMI 1640. The cells were finally suspended in complete tissue culture medium (RPMI 1640, 10% human AB serum, penicillin [100 U/ml], streptomycin [100 μg/ml], gentamicin [40 μg/ml]) and counted with a Coulter counter (Coulter Electronics Ltd., Luton, Beds, England).
HLA typing of PBMCs.
PBMCs were HLA typed genomically by using sequence-specific primers in PCR, as described previously (47). In brief, an HLA-DR “low resolution” kit containing the primers to type for DRB1, DRB3, DRB4, and DRB5 alleles was purchased from Dynal AS (Oslo, Norway) and used in a PCR as specified by the manufacturer. DNA amplifications were carried out in a Gene Amp PCR system 2400 (Perkin-Elmer, Cetus), and the amplified products were analyzed by agarose gel electrophoresis, using standard procedures. Serologically defined HLA-DR specificities were determined from the genotypes by following the guidelines provided by Dynal AS.
Antigen- and peptide-induced proliferation of PBMCs.
Antigen- and peptide-induced proliferation of PBMCs was performed by using standard procedures (4). In brief, PBMCs (2 × 105 cells/well) suspended in 50 μl of complete tissue culture medium were seeded into the wells of 96-well tissue culture plates (Nunc, Roskilde, Denmark). Antigen or peptide in 50 μl of complete medium was added to the wells in triplicate at an optimal concentration of 5 μg/ml. Whole bacilli were used at a concentration of 10 μg (wet weight) per ml. The final volume of the culture in each well was adjusted to 200 μl. The plates were incubated at 37°C in a humidified atmosphere of 5% CO2 and 95% air. The cultures were pulsed for 4 h on day 6 with 1 μCi of [3H]thymidine (Amersham Life Sciences, Little Chalfont, United Kingdom) and harvested on filter mats with a Skatron harvester (Skatron Instruments AS, Oslo, Norway), and the amount of radioactivity incorporated was measured by liquid scintillation counting (5). The radioactivity incorporated was obtained as counts per minute (cpm). The average cpm was calculated from triplicate cultures stimulated with each antigen or peptide as well as from triplicate wells of negative-control cultures lacking antigen. Cellular proliferation results are presented below by using the stimulation index (SI), which is defined as follows: SI = cpm in antigen-stimulated cultures/cpm in cultures without antigen. An SI of ≥2 was considered a positive proliferative response in response to a given antigen (6, 44).
IFN-γ assay.
Supernatants (100 μl) were collected from antigen-stimulated cultures of PBMCs (96-well plates) before being pulsed with [3H]thymidine. The supernatants were kept frozen at −70°C until assayed for gamma interferon (IFN-γ) activity, as described previously (6). In brief, the amounts of IFN-γ in the supernatants were quantified by using immunoassay kits (Beckman Coulter/Immunotech, S.A., Marseille, France) as specified by the manufacturer. The detection limit of the IFN-γ assay kit was 0.08 international units (IU)/ml. Secretion of IFN-γ in response to a given antigen was considered positive when ΔIFN-γ (the IFN-γ concentration in cultures stimulated with antigen minus the IFN-γ concentration cultures without antigen) was ≥1.5 IU/ml (45, 60).
Interpretation of antigen-induced proliferation and IFN-γ secretion results and statistical analysis.
An antigen/peptide was considered a strong, moderate, or weak stimulator of PBMC in proliferation and IFN-γ responses based on the percentage of positive responses. The responses were considered strong with a percentage of positive responses of >60%, moderate with a percentage of positive responses from 40 to 60% and weak with a percentage of positive responses of <40% (43, 48). The statistical analysis was performed using a Z test to identify significant differences (P < 0.05) with respect to the percentage of positive results in response to various antigens in antigen-induced proliferation and IFN-γ assays.
HLA-DR binding prediction analysis of MPT83 and its peptides.
HLA-DR binding propensity along the primary structure of MPT83 and the sequence of its peptides was first analyzed using ProPred at the default setting (threshold value of 3.0), which is a graphical web tool for the prediction of major histocompatibility complex (MHC) class II binding regions in antigenic protein sequences using the server (http://www.imtech.res.in/raghava/propred/) (62). This server has been suggested as a useful tool in locating the promiscuous binding regions that can bind to a total of 51 alleles belonging to nine serologically defined HLA-DR molecules encoded by the DRB1 and DRB5 genes (62). In addition, three other prediction methods, i.e., NetMHCII 2.2 (56), Petrochemitric (24), and IEDB Consensus (67), were also used to predict binding of MPT83 peptides to 12 to 14 HLA-DR alleles, including HLA DRB1*0101, DRB1*0301, DRB1*0401, DRB1*0701, DRB1*1101, and DRB1*1501 supertype alleles, which are expected to cover approximately >95% of any given human population (27). The sequences/peptides predicted to bind ≥50% alleles of HLA-DR molecules analyzed were considered promiscuous for binding (45, 53).
RESULTS
Th1 cell responses of PBMCs to complex and single mycobacterial antigens.
PBMCs from M. bovis BCG-vaccinated healthy subjects were divided into two groups, i.e., ESAT-6/CFP10 responders and nonresponders, and tested for antigen-induced proliferation and IFN-γ secretion, in response to complex mycobacterial antigens, including the whole cells of M. tuberculosis H37Rv and M. bovis BCG, MT-CF, and MT-CW and the cocktails of synthetic peptides of MPT83, MPB70, LppX, PPE68, ESAT-6, and CFP10, to represent single antigens.
The results showed that all of the complex mycobacterial antigens were strong stimulators of PBMCs from both groups in antigen-induced proliferation and IFN-γ secretion assays with no statistical difference in positive responses between the two groups and the various complex mycobacterial antigens (P > 0.05) (Table 1). In addition, in CFP10/ESAT6 responders, MPT83, MPB70, LppX, PPE68, CFP10, and ESAT6 showed strong responses in both assays, whereas MPT63 induced a moderate response in proliferation and a weak response in the IFN-γ assay, which were significantly lower than those of other single antigens (P < 0.05) (Table 1). Furthermore, in this group of subjects, only MPT63 showed significantly lower positive results than the complex mycobacterial antigens in both assays (P < 0.05), whereas the responses to PPE68, CFP10, and ESAT-6 were statistically similar to those of the complex mycobacterial antigens in both assays and to those of MPT83, MPB70, and LppX in IFN-γ assays (P > 0.05).
Table 1.
Antigen-induced proliferation and IFN-γ results with PBMCs from CFP10/ESAT6 responder and nonresponder healthy subjects in response to complex and single mycobacterial antigens
| Antigen | No. positive/no. tested (% positive) |
|||
|---|---|---|---|---|
| CFP10/ESAT6 responders |
CFP10/ESAT6 non-responders |
|||
| Proliferationa | IFN-γb | Proliferation | IFN-γ | |
| M. tuberculosis | 36/38 (95) | 21/23 (91) | 46/49 (94) | 30/31 (97) |
| MT-CF | 36/39 (92) | 23/23 (100) | 49/49 (100) | 30/31 (97) |
| MT-CW | 21/21 (100) | 16/16 (100) | 47/49 (96) | 27/29 (93) |
| BCG | 8/8 (100) | 10/11 (91) | 35/40 (88) | 21/25 (84) |
| MPT63 | 16/39 (41) | 8/23 (35) | 17/49 (35) | 10/31 (32) |
| MPT83 | 27/39 (69) | 17/23 (74) | 33/49 (67) | 16/31 (52) |
| MPB70 | 25/39 (64) | 16/23 (70) | 28/49 (57) | 12/28 (43) |
| LppX | 23/36 (64) | 16/23 (70) | 11/45 (24) | 9/28 (32) |
| PPE68 | 33/39 (85) | 18/23 (78) | 29/48 (60) | 15/28 (54) |
| CFP10 | 35/39 (90) | 20/23 (87) | 0/48 (0.0) | 0/28 (0.0) |
| ESAT-6 | 31/39 (80) | 20/23 (87) | 0/49 (0.0) | 0/28 (0.0) |
A positive response was defined as antigen-induced proliferation with an SI (defined in Materials and Methods) of ≥2.
A response was considered positive if the IFN-γ concentration in a culture stimulated with antigen minus the IFN-γ concentration in a culture without antigen was ≥1.5 IU/ml.
In CFP10/ESAT6 nonresponders, MPT83, MPB70, and PPE68 showed moderate to strong Th1 responses, whereas MPT63 and LppX induced weak Th1 responses (Table 1). However, positive responses to all single antigens were statistically lower than those of the complex mycobacterial antigens (P < 0.05) in both assays. Furthermore, the responses to MPT83, MPB70, and PPE68 were statistically similar to each other (P > 0.05) but significantly higher than the responses induced by MPT63 and LppX (P < 0.05) in antigen-induced proliferation assays, whereas the differences in positive responses to all single antigens in IFN-γ assays were nonsignificant (P > 0.05) (Table 1).
Compared for significant differences in Th1 cell responses to single antigens, i.e., MPT63, MPT70, MPT83, LppX, and PPE68, in the ESAT-6/CFP10 responders versus ESAT-6/CFP10 nonresponders, only LppX showed significantly higher responses in ESAT-6/CFP10 responders than nonresponders in both assays and PPE68 in proliferation assays (P < 0.05) (Table 1).
HLA-DR binding prediction analysis of MPT83 and its peptides.
The analysis of the MPT83 sequence for binding prediction to HLA-DR molecules showed that this protein was predicted to bind all of the 51 HLA-DR alleles included in the ProPred graphical web tool (Table 2; see Fig. S1 in the supplemental material). In addition, ProPred identified 11 T-cell epitope regions of 9 to 24 residues in length, which were scattered throughout the MPT83 sequence, i.e., amino acids (aa) 1 to 12, aa 19 to 27, aa 59 to 68, aa 81 to 89, aa 95 to 104, aa 107 to 119, aa 122 to 130, aa 132 to 140, aa 143 to 166, aa 189 to 204, and aa 208 to 217 (Table 2). Of these, four regions, i.e., aa 107 to 119, 143 to 166, 189 to 204, and 208 to 217, were predicted to be HLA promiscuous (Table 2) Furthermore, the analysis of individual MPT83 peptide sequences (P1 to P14; Fig. 1) by ProPred suggested that 11 of the peptides were HLA-DR binders and five of them, i.e., P1 (aa 1 to 25), P8 (106 to 130), P11 (151 to 175), P13 (181 to 205), and P14 (196 to 220), qualified to be promiscuous binders, as they were predicted to bind >50% alleles of HLA-DR molecules included in ProPred (Table 3).
Table 2.
ProPred analysis for prediction of HLA-DR binding regions in MPT83 sequence
| HLA-DR allele | Allele bindingb in predicted regions (aa range) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–220 | 1–12 | 19–27 | 59–68 | 81–89 | 95–104 | 107–119 | 122–130 | 132–140 | 143–166 | 189–204 | 208–217 | |
| DRB1.1 | 2/2 | 2/2 | 1/2 | 1/2 | 0/2 | 0/2 | 0/2 | 1/2 | 1/2 | 1/2 | 2/2 | 2/2 |
| DRB1.3 | 7/7 | 2/7 | 0/7 | 0/7 | 7/7 | 0/7 | 5/7 | 0/7 | 0/7 | 7/7 | 6/7 | 7/7 |
| DRB1.4 | 2/9 | 0/9 | 0/9 | 0/9 | 0/9 | 7/9 | 9/9 | 1/9 | 0/9 | 4/9 | 3/9 | 9/9 |
| DRB1.7 | 2/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 |
| DRB1.8 | 6/6 | 5/6 | 1/6 | 4/6 | 0/6 | 0/6 | 4/6 | 1/6 | 0/6 | 6/6 | 1/6 | 6/6 |
| DRB | 9/9 | 7/9 | 0/9 | 0/9 | 1/9 | 0/9 | 4/9 | 0/9 | 0/9 | 8/9 | 8/9 | 9/9 |
| DRB1.13 | 11/11 | 7/11 | 1/11 | 0/11 | 0/11 | 0/11 | 4/11 | 0/11 | 0/11 | 9/11 | 6/11 | 11/11 |
| DRB1.15 | 3/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 2/3 | 3/3 | 1/3 |
| DRB5.1 | 2/2 | 2/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 | 0/2 | 0/2 |
| P/Ta | 51/51 | 25/51 | 3/51 | 5/51 | 8/51 | 9/51 | 26/51 | 3/51 | 1/51 | 39/51 | 29/51 | 47/51 |
P/T, no. of HLA-DR alleles predicted to bind/no. of alleles tested.
No. of alleles predicted to bind/no. of alleles included in ProPred, in predicted HLA-DR binding regions (aa range) in the sequence of MPT83.
Table 3.
ProPred analysis for HLA-DR binding prediction of synthetic peptides of MPT83
| HLA-DR allele | Binding of MPT83 peptideb |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 | |
| DRB1.1 | 2/2 | 1/2 | 0/2 | 1/2 | 0/2 | 0/2 | 0/2 | 1/2 | 1/2 | 0/2 | 1/2 | 0/2 | 2/2 | 2/2 |
| DRB1.3 | 2/7 | 0/7 | 0/7 | 0/7 | 0/7 | 7/7 | 0/7 | 5/7 | 0/7 | 7/7 | 5/7 | 0/7 | 6/7 | 7/7 |
| DRB1.4 | 0/9 | 0/9 | 0/9 | 0/9 | 0/9 | 0/9 | 7/9 | 9/9 | 1/9 | 3/9 | 2/9 | 0/9 | 3/9 | 9/9 |
| DRB1.7 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 |
| DRB1.8 | 5/6 | 1/6 | 0/6 | 4/6 | 0/6 | 0/6 | 0/6 | 5/6 | 1/6 | 1/6 | 6/6 | 0/6 | 1/6 | 6/6 |
| DRB1.11 | 7/9 | 0/9 | 0/9 | 0/9 | 0/9 | 1/9 | 0/9 | 4/9 | 0/9 | 7/9 | 5/9 | 0/9 | 8/9 | 9/9 |
| DRB1.13 | 8/11 | 1/11 | 0/11 | 0/11 | 0/11 | 0/11 | 0/11 | 4/11 | 0/11 | 3/11 | 7/11 | 0/11 | 6/11 | 11/11 |
| DRB1.15 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 0/3 | 2/3 | 0/3 | 3/3 | 1/3 |
| DRB5.1 | 2/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 0/2 | 2/2 | 0/2 | 0/2 | 0/2 |
| P/Ta | 26/51 | 3/51 | 0/51 | 5/51 | 0/51 | 8/51 | 9/51 | 28/51 | 3/51 | 21/51 | 30/51 | 0/51 | 29/51 | 47/51 |
P/T, no. of HLA-DR alleles predicted to bind/no. of alleles tested.
No. of alleles predicted to bind/no. of alleles included in ProPred, in synthetic MPT83 peptides.
Experimental evaluation of MPT83 and its peptides for promiscuous presentation to Th1 cells and comparisons with computational prediction methods.
To further analyze the promiscuous presentation of MPT83 and its peptides to Th1 cells, PBMCs of 17 subjects responding to the peptide pool of MPT83 were tested for reactivity to individual peptides of MPT83 in antigen-induced proliferation (Table 4) and IFN-γ secretion assays (Table 5). HLA-DR typing of the subjects demonstrated that they represented a heterogeneous group of donors expressing DR1, DR2, DR3, DR4, DR6, DR7, DR10, DR51, DR52, and DR53 molecules (Table 4), thus indicating the permissive and promiscuous nature of MPT83 in presentation to Th1 cells. To identify the Th1 cell-reactive and promiscuous peptides of MPT83, PBMCs from all the 17 subjects were tested in both assays for reactivity to individual peptides of MPT83, i.e., P1 to P14. The results showed that positive responses were obtained with all the peptides in 2 to 10 donors in antigen-induced proliferation (Table 4) and 1 to 11 donors in IFN-γ secretion assays (Table 5). Furthermore, the heterogeneity of HLA-DR molecules expressed in the donors suggested that all peptides may have been presented to Th1 cells by more than one HLA-DR molecule (Table 4 and 5).
Table 4.
Antigen-induced proliferation of HLA-DR typed PBMCs to the peptide pool and individual synthetic peptides of MPT83
| PBMC donor |
Antigen-induced proliferation (SI) of PBMCs in response toc: |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | HLA-DR | MPT83pool | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 |
| 1 | 1, 3, 52 | 12 | 2.0 | 2.0 | 1.7 | 2.0 | 1.7 | 1.1 | 1.2 | 1.3 | 0.8 | 1.0 | 1.0 | 3.1 | 2.5 | 0.8 |
| 2 | 4, 53 | 5.8 | 0.9 | 1.0 | 0.8 | 1.0 | 0.8 | 0.6 | 0.6 | 0.8 | 0.6 | 1.0 | 1.5 | 2.5 | 0.9 | 1.9 |
| 3 | 6, 7, 52, 53 | 14 | 0.3 | 0.5 | 0.5 | 1.4 | 0.4 | 0.4 | 0.3 | 0.3 | 0.6 | 1.3 | 8.0 | 0.9 | 1.3 | 1.8 |
| 4 | 7, 53 | 3.1 | 0.5 | 1.0 | 0.7 | 0.7 | 0.5 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 2.6 | 0.8 | 0.7 | 4.0 |
| 5 | 3, 52 | 2.8 | 0.6 | 0.4 | 0.3 | 0.4 | 0.3 | 0.4 | 0.5 | 0.3 | 0.4 | 2.5 | 1.4 | 1.2 | 1.0 | 14 |
| 6 | 6, 7, 52, 53 | 6.1 | 0.2 | 0.3 | 0.4 | 0.5 | 0.2 | 0.3 | 0.3 | 0.9 | 0.2 | 0.4 | 9.7 | 2.3 | 2.1 | 4.6 |
| 7 | 2, 7, 51, 53 | 2.2 | 0.7 | 0.8 | 2.8 | 0.7 | 0.8 | 0.4 | 1.2 | 0.4 | 3.2 | 1.1 | 1.1 | 1.4 | 1.8 | 4.3 |
| 8 | 4, 10, 53 | 2.8 | 0.9 | 1.0 | 1.0 | 0.9 | 0.9 | 0.7 | 1.0 | 1.0 | 0.9 | 0.8 | 1.9 | 0.6 | 0.7 | 3.2 |
| 9 | 3, 6, 52 | 2.8 | 1.4 | 1.0 | 1.0 | 1.6 | 3.3 | 1.8 | 0.8 | 1.5 | 1.8 | 0.7 | 2.4 | 0.7 | 0.6 | 0.6 |
| 10 | 6, 10, 52 | 5.6 | 2.7 | 2.4 | 0.8 | 4.5 | 2.9 | 2.1 | 4.6 | 1.0 | 0.8 | 4.3 | 3.6 | 5.0 | 0.9 | 2.4 |
| 11 | 3, 6, 52 | 2.3 | 3.0 | 6.1 | 1.0 | 2.5 | 2.2 | 5.7 | 1.8 | 2.1 | 0.5 | 1.6 | 3.1 | 0.8 | 1.0 | 1.2 |
| 12 | 1, 3, 52 | 4.1 | 0.6 | 1.3 | 1.1 | 0.7 | 0.4 | 0.6 | 0.4 | 0.7 | 3.7 | 9.3 | 1.0 | 1.8 | 1.2 | 8.4 |
| 13 | 3, 4, 52, 53 | 5.6 | 1.6 | 1.3 | 1.7 | 1.7 | 1.3 | 1.1 | 2.1 | 1.6 | 1.2 | 0.7 | 2.3 | 1.8 | 1.8 | 4.5 |
| 14 | 5, 7, 51, 53 | 8.8 | 3.0 | 0.9 | 6.2 | 6.2 | 1.1 | 1.3 | 1.9 | 2.1 | 2.2 | 1.3 | 7.6 | 2.0 | 1.7 | 8.1 |
| 15 | 2, 4, 51, 53 | 2.8 | 2.1 | 1.6 | 1.2 | 1.4 | 0.7 | 1.5 | 0.7 | 0.8 | 0.7 | 0.8 | 1.1 | 1.4 | 1.9 | 1.9 |
| 16 | 2, 7, 51, 53 | 2.4 | 3.0 | 5.1 | 2.7 | 4.5 | 3.0 | 7.8 | 0.9 | 1.2 | 0.9 | 1.2 | 0.9 | 1.2 | 1.2 | 0.9 |
| 17 | NDb | 6.0 | 1.8 | 1.1 | 0.5 | 0.7 | 0.8 | 0.8 | 0.4 | 0.6 | 0.6 | 0.8 | 0.8 | 1.2 | 0.6 | 2.4 |
| P/Ta | 17/17 | 6/17 | 4/17 | 3/17 | 5/17 | 4/17 | 3/17 | 2/17 | 2/17 | 3/17 | 3/17 | 8/17 | 5/17 | 2/17 | 10/17 | |
P/T, no. of subjects showing positive responses/no. of subjects tested.
ND, not determined.
The positive antigen-induced proliferation responses (SI ≥ 2.0) are given in boldface.
Table 5.
Antigen-induced IFN-γ secretion by HLA-DR typed PBMCs to the peptide pool and individual synthetic peptides of MPT83
| PBMC donor |
IFN-γ secretion (IU/ml) by PBMCs in response toc: |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | HLA-DR | MPT83pool | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 |
| 1 | 1, 3, 52 | 16 | 2.2 | 1.2 | 1.8 | 1.0 | 1.9 | 1.8 | 1.4 | 2.4 | 2.6 | 2.6 | 0.7 | 5.6 | 1.0 | 1.3 |
| 2 | 4, 53 | 21 | 0.9 | 1.0 | 0.6 | 1.2 | 0.9 | 1.7 | 2.0 | 0.9 | 0.8 | 1.7 | 1.4 | 3.9 | 1.3 | 3.3 |
| 3 | 6, 7, 52, 53 | 53 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 42 | 3.5 | <0.4 | <0.4 |
| 4 | 7, 53 | 9.2 | 0.7 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 0.6 | 1.9 | 0.7 | 1.0 | <0.4 | <0.4 | 4.5 |
| 5 | 6, 52 | 6.6 | 0.8 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 3.2 | <0.4 |
| 6 | 3, 52 | 17 | 0.9 | 1.1 | <0.4 | <0.4 | <0.4 | <0.4 | 1.8 | 2.3 | 0.4 | 0.5 | 5.2 | <0.4 | <0.4 | 0.7 |
| 7 | 6, 7, 52, 53 | 38 | 2.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 33 | <0.4 | <0.4 | 30 |
| 8 | 4, 10, 53 | 21 | <0.4 | <0.4 | 8.0 | 2.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 7.3 |
| 9 | 1, 6, 52 | 7.0 | 2.9 | <0.4 | 11 | 3.5 | 0.9 | 3.2 | 7.5 | <0.4 | <0.4 | <0.4 | 1.4 | <0.4 | <0.4 | 4.4 |
| 10 | 3, 6, 52 | 4.0 | 6.0 | <0.4 | <0.4 | <0.4 | 4.0 | <0.4 | <0.4 | 10 | 1.1 | 5.7 | 0.7 | <0.4 | <0.4 | <0.4 |
| 11 | 6, 10, 52 | 19 | 1.7 | <0.4 | 1.1 | <0.4 | <0.4 | 4.4 | 25 | 2.0 | <0.4 | 1.5 | 10 | 5.3 | 2.0 | 1.5 |
| 12 | 3, 6, 52 | 6.7 | 2.3 | 17 | 0.9 | 2.4 | 4.6 | 11 | 5.8 | 4.7 | 1.5 | 15 | 11 | 1.5 | 1.8 | 4.6 |
| 13 | 1, 3, 52 | 21 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 6.9 | 13 | <0.4 | <0.4 | 3.4 | 0.5 | <0.4 |
| 14 | 2, 6, 51, 52 | 11 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | <0.4 | 16 | 4.3 | 5.9 | <0.4 | 5.1 | 19 |
| 15 | 3, 4, 52, 53 | 18 | <0.4 | 0.4 | 0.6 | 1.0 | 6.5 | <0.4 | 0.6 | 5.1 | 2.4 | 0.8 | 1.5 | 2.0 | 2.0 | 23 |
| 16 | 5, 7, 51, 53 | 7.4 | 0.8 | 0.7 | <0.4 | 11 | 1.7 | <0.4 | 1.5 | 21 | 5.4 | 11 | 18 | 1.6 | 1.0 | 16 |
| 17 | NDb | 4.6 | 1.1 | <0.4 | <0.4 | 0.5 | 1.0 | 0.9 | 1.5 | 1.0 | 1.5 | 1.0 | 0.5 | 2.2 | 1.0 | 5.0 |
| P/Ta | 17/17 | 6/17 | 1/17 | 3/17 | 4/17 | 5/17 | 5/17 | 7/17 | 8/17 | 8/17 | 7/17 | 8/17 | 9/17 | 5/17 | 11/17 | |
P/T, no. of subjects showing positive responses/no. of subjects tested.
ND, not determined.
The positive antigen-induced proliferation responses (SI ≥ 2.0) are given in boldface.
The results of HLA-DR binding prediction by ProPred, NetMHCII 2.2, Petrochemitric, and IEDB Consensus methods further showed that MPT83 protein was capable of binding to molecules expressed from all HLA-DR alleles included in the analysis (see Table S1 in the supplemental material). In addition, a direct comparison between HLA-DR binding prediction methods and Th1 cell responses of PBMCs to various peptides of MPT83 showed that three peptides were strong stimulators of Th1 cell reactivity, i.e., P11, P12, and P14, of which P11 and P14 were predicted to be HLA promiscuous by three of the four methods, whereas only the Petrochemitric method predicted the HLA-promiscuous nature of P12 (see Table S1 in the supplemental material).
DISCUSSION
In this study, MPT83 was evaluated, using overlapping synthetic peptides, for Th1 cell reactivity in M. bovis BCG-vaccinated and PPD-positive healthy subjects residing in Kuwait. Furthermore, HLA-DR binding prediction analysis of MPT83 and its peptides, as well as HLA-DR typing of MPT83 responders, was performed to determine the promiscuous nature of the full-length protein and its peptides. To my knowledge, this is the first study to determine Th1 cell reactivity of MPT83 and its peptides in HLA-DR-typed M. bovis BCG-vaccinated healthy humans and their binding prediction to HLA-DR alleles.
The test systems used to determine Th1 cell reactivity were antigen-induced proliferation and IFN-γ secretion assays. Both of these assays require culture of PBMCs separated from a venous blood sample by density gradient centrifugation (39). However, the measurement of IFN-γ concentration in culture supernatants is considered more sensitive and specific than proliferation assays (7). Since antigen-induced proliferation and IFN-γ secretion have been correlated with protective immunity in tuberculosis (22, 25, 26), in order to identify new candidates for safer subunit vaccines, it is important to identify major M. tuberculosis antigens and peptides recognized by human Th1 cells in these assays.
To determine the immunological reactivity of M. tuberculosis proteins, full-length proteins purified from cultures of M. tuberculosis or purified recombinant proteins, expressed in Escherichia coli, have been used (39, 40, 41). However, obtaining full-length proteins from cultures of pathogenic M. tuberculosis is extremely hazardous and technically demanding (39). On the other hand, the production of purified recombinant mycobacterial proteins has often been notoriously difficult in E. coli (1, 2, 12). To overcome the problems associated with the expression and purification of recombinant mycobacterial proteins, pools of overlapping synthetic peptides have been successfully used in the past to replace recombinant or natural M. tuberculosis proteins in Th1 cell assays (40, 41, 55). The inclusion of pools of peptides corresponding to other secreted protein antigens of M. tuberculosis, which have been previously characterized for Th1 cell reactivity in M. bovis BCG-vaccinated healthy subjects, i.e., MPT63 (43), MPB70 (10), and LppX (5), helped to compare the responses induced by MPT83.
Among the antigens tested in this study, Th1 cell responses to ESAT-6 and CFP10 have been correlated with M. tuberculosis infection/latent TB in healthy subjects (23, 46, 63, 66). Therefore, to determine if latent infection with M. tuberculosis could have an effect on the Th1 cell responses to various antigens used in this study, the donors were divided into ESAT-6/CFP10 responders and nonresponders to indicate M. tuberculosis infection and noninfection, respectively (10, 34). PBMCs from both donor groups had strong responses to all complex mycobacterial antigens without significant differences between the two donor groups (Table 1), which suggested the suitability of the donors to test for reactivity to single antigens. The responses to MPT83, MPB70, and PPE68 were strong in CFP10/ESAT-6 responders and moderate in nonresponders, without significant differences between the two groups (P > 0.05). The only antigen that showed significantly weaker positivity (P < 0.05) in ESAT-6/CFP10 nonresponders, compared to responders, was LppX. The overall results suggest that infection with M. tuberculosis did not affect the level of Th1 cell reactivity to BCG and most antigens of M. tuberculosis used in this study. Furthermore, the study confirms strong to moderate reactivity of MPB70 and PPE68 in M. tuberculosis-infected and noninfected BCG-vaccinated healthy subjects, as reported previously (5, 10, 45, 48), and identifies MPT83 as an immunodominant cross-reactive antigen in humans, like Ag85B and MPB70 (10, 50).
Although the gene for PPE68 is present in the M. tuberculosis-specific RD1 segment (13, 36), statistically similar responses in the ESAT-6/CFP10 responders and nonresponders could be due to the presence of an immunodominant epitope (aa 124 to 137), which is conserved in several PPE proteins of M. tuberculosis, BCG, and environmental mycobacteria (48, 57). Similarly, one of the immunodominant peptides of MPT83, i.e., P14 (aa 196 to 220), shares 84 to 100% sequence identity with BCG, several species of environmental mycobacteria, and the immunodominant epitope of MPT70 (see Table S2 in the supplemental material). Therefore, in addition to BCG vaccination and infection with M. tuberculosis, exposure to environmental mycobacteria may also have contributed to strong and moderate responses to MPT83, PPE68, and MPT70 in CFP10/ESAT-6 responders and nonresponders, respectively. In contrast to the present report, Whelan et al. from the United Kingdom have reported weak responses to MPT83 and MPB70 in M. bovis-infected cattle (68). This could be due to species differences and/or a low load of exposure to environmental mycobacteria, as demonstrated for nonrecognition of the cross-reactive epitope of PPE68 (aa 124 to 137) in mice (21) and weak recognition of PPE68 in BCG-vaccinated healthy subjects from Denmark (57).
The strong reactivity of MPT83 in Th1 cell assays suggests that it could be useful in vaccine formulations against TB. However, Th1 cells recognize protein antigens in association with highly polymorphic HLA class II molecules and particularly HLA-DR molecules (38, 51, 52). Therefore, among the requirements for any antigen to qualify as a vaccine candidate is its recognition by an HLA-heterogeneous group of donors. To determine if MPT83 would qualify by this requirement, the PBMCs from MPT83-responding donors were typed for HLA-DR molecules. The results showed that the donors were quite heterogeneous and expressed various HLA-DR molecules that are frequently expressed in humans (Table 4). In addition, the promiscuous nature of MPT83 for binding to HLA-DR molecules was also identified by using computational methods. Although several computational methods are available for HLA-DR binding and the prediction of T cell epitopes, including ProPred, NetMHCII 2.2, Petrochemitric, and IEDB Consensus, etc. (24, 56, 62, 67), ProPred was evaluated first because comparative evaluations have previously been shown the usefulness of this method in predicting mycobacterial T-cell epitopes (5, 10, 44, 53). The overall results of computational analysis suggest that MPT83 was highly promiscuous for binding to HLA-DR molecules, as all of the HLA-DR specificities included in the computational methods were predicted to bind the MPT83 sequence (see Fig. S1 and Table S1 in the supplemental material). Among the three peptides showing strong Th1 cell responses, i.e., P11, P12, and P14, at least one of the methods predicted them to be HLA-promiscuous binders (see Table S1 in the supplemental material). However, none of the single peptides qualified to replace MPT83 as the best Th1 cell-stimulating peptide, i.e., P14 (aa 196 to 220), although a promiscuous HLA-DR binder with strong Th1 cell responses showed negative responses for 22% of MPT83-responding donors in Th1 cell assays. Thus, this protein behaves like other major antigenic proteins of M. tuberculosis, e.g., Ag85B, PPE68, MPT70, ESAT-6, and CFP10, etc., in which no single peptide could replace the complete protein sequences for Th1 cell reactivity (5, 10, 44, 47, 53). However, being a major Th1 cell antigen capable of stimulating Th1 cells from HLA-DR heterogeneous subjects, this protein may be considered in formulations to develop a new vaccine candidate against TB.
In addition to recognition by CD4+ Th1 cells by analyzing binding to MHC class II (HLA-DR) molecules, MPT83 was also analyzed for possible recognition by CD8+ Th1/cytotoxic cells by predicting to bind MHC class I (HLA A, B, and C) molecules using the server http://www.imtech.res.in/raghava/nhlapred/, which predicts binding to 67 MHC class I alleles. The analysis showed that the MPT83 sequence was predicted to bind 47/67 (70%) alleles, suggesting its HLA-promiscuous nature for recognition by CD8+ T cells as well (data not shown). This suggests that CD8+ T cells may also have contributed to the responses observed.
In conclusion, the results presented in this work demonstrate that MPT83 is a major Th1 cell-stimulating protein of M. tuberculosis, with the ability to induce positive responses in HLA-heterogeneous donors and ability to bind HLA molecules promiscuously. Furthermore, the Th1 cell epitopes are scattered throughout the protein sequence. These properties of MPT83 make it an interesting candidate, like Ag85B, HSP65, and MPT70 (39), for inclusion in a vaccine cocktail against TB.
Supplementary Material
ACKNOWLEDGMENTS
This study received financial support from Kuwait University Research Administration grant MI03/05. MT-CF and MT-CW were produced under NIH contract HHSN266200400091C/ADB contract NO-AI40092, “Tuberculosis Vaccine Testing and Research Materials Contract.”
The buffy coats from healthy donors were obtained from the Central Blood Bank, Kuwait, and Fatema Shaban provided technical help.
Footnotes
Supplemental material for this article may be found at http://cvi.asm.org/.
Published ahead of print on 18 August 2011.
REFERENCES
- 1. Ahmad S., Amoudy H. A., Thole J. E., Young D. B., Mustafa A. S. 1999. Identification of a novel protein antigen encoded by a Mycobacterium tuberculosis-specific RD1 region gene. Scand. J. Immunol. 49:515–522 [DOI] [PubMed] [Google Scholar]
- 2. Ahmad S., El-Shazly S., Mustafa A. S., Al-Attiyah R. 2004. Mammalian cell-entry proteins encoded by the mce3 operon of Mycobacterium tuberculosis are expressed during natural infection in humans. Scand. J. Immunol. 60:382–391 [DOI] [PubMed] [Google Scholar]
- 3. Al-Attiyah R., El-Shazly A., Mustafa A. S. 2006. Assessment of in vitro immunity to Mycobacterium tuberculosis in a human peripheral blood infection model using a luciferase reporter construct of M. tuberculosis H37Rv. Clin. Exp. Immunol. 145:520–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Al-Attiyah R., et al. 2006. Cytokine profiles in tuberculosis patients and healthy subjects in response to complex and single antigens of Mycobacterium tuberculosis. FEMS Immunol. Med. Microbiol. 47:254–261 [DOI] [PubMed] [Google Scholar]
- 5. Al-Attiyah R., Mustafa A. S. 2004. Computer-assisted prediction of HLA-DR binding and experimental analysis for human promiscuous Th1 cell peptides in a novel 24-kDa secreted lipoprotein (LppX) of Mycobacterium tuberculosis. Scand. J. Immunol. 59:16–24 [DOI] [PubMed] [Google Scholar]
- 6. Al-Attiyah R., Mustafa A. S. 2008. Characterization of human cellular immune responses to novel Mycobacterium tuberculosis antigens encoded by genomic regions absent in Mycobacterium bovis BCG. Infect. Immun. 76:4190–4198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Al-Attiyah R. J., Mustafa A. S. 2009. Mycobacterial antigen-induced T helper type 1 (Th1) and Th2 reactivity of peripheral blood mononuclear cells from diabetic and non-diabetic tuberculosis patients and Mycobacterium bovis bacilli Calmette-Guérin (BCG)-vaccinated healthy subjects. Clin. Exp. Immunol. 158:64–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Al-Attiyah R., Mustafa A. S., Abal A. T., Madi N. M., Andersen P. 2003. Restoration of mycobacterial antigen-induced proliferation and interferon-gamma responses in peripheral blood mononuclear cells of tuberculosis patients upon effective chemotherapy. FEMS Immunol. Med. Microbiol. 38:249–256 [DOI] [PubMed] [Google Scholar]
- 9. Al-Attiyah R., et al. 2004. In vitro cellular immune responses to complex and newly defined recombinant antigens of Mycobacterium tuberculosis. Clin. Exp. Immunol. 138:139–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Al-Attiyah R., Shaban F. A., Wiker H. G., Oftung F., Mustafa A. S. 2003. Synthetic peptides identify promiscuous human Th1 cell epitopes of the secreted mycobacterial antigen MPB70. Infect. Immun. 71:1953–1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Al-Khodari N. Y., Al-Attiyah R., Mustafa A. S. 2011. Identification, diagnostic potential, and natural expression of immunodominant seroreactive peptides encoded by five Mycobacterium tuberculosis-specific genomic regions. Clin. Vaccine Immunol. 18:477–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Amoudy H. A., Ahmad S., Thole J. E., Mustafa A. S. 2007. Demonstration of in vivo expression of a hypothetical open reading frame (ORF-14) encoded by the RD1 region of Mycobacterium tuberculosis. Scand. J. Immunol. 66:422–425 [DOI] [PubMed] [Google Scholar]
- 13. Amoudy H. A., Al-Turab M. B., Mustafa A. S. 2006. Identification of transcriptionally active open reading frames within the RD1 genomic segment of Mycobacterium tuberculosis. Med. Princ. Pract. 15:137–144 [DOI] [PubMed] [Google Scholar]
- 14. Andersen P. 1994. Effective vaccination of mice against Mycobacterium tuberculosis infection with a soluble mixture of secreted mycobacterial proteins. Infect. Immun. 62:2536–2544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Azzopardi P., Bennett C. M., Graham S. M., Duke T. 2009. Bacille Calmette-Guérin vaccine-related disease in HIV-infected children: a systematic review. Int. J. Tuberc. Lung Dis. 13:1331–1344 [PubMed] [Google Scholar]
- 16. Azzurri A., et al. 2006. Serological markers of pulmonary tuberculosis and of response to anti-tuberculosis treatment in a patient population in Guinea. Int. J. Immunopathol. Pharmacol. 19:199–208 [PubMed] [Google Scholar]
- 17. Baldwin S. L., et al. 1998. Evaluation of new vaccines in the mouse and guinea pig model of tuberculosis. Infect. Immun. 66:2951–2959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bertholet S., et al. 2008. Identification of human T cell antigens for the development of vaccines against Mycobacterium tuberculosis. J. Immunol. 181:7948–7957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bourgarit A., et al. 2006. Explosion of tuberculin-specific Th1-responses induces immune restoration syndrome in tuberculosis and HIV co-infected patients. AIDS 20:F1–F7 [DOI] [PubMed] [Google Scholar]
- 20. Cai H., et al. 2005. Combined DNA vaccines formulated either in DDA or in saline protect cattle from Mycobacterium bovis infection. Vaccine 23:3887–3895 [DOI] [PubMed] [Google Scholar]
- 21. Demangel C., et al. 2004. Cell envelope protein PPE68 contributes to Mycobacterium tuberculosis RD1 immunogenicity independently of a 10-kilodalton culture filtrate protein and ESAT-6. Infect. Immun. 72:2170–2176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Demissie A., et al. 2004. Healthy individuals that control a latent infection with Mycobacterium tuberculosis express high levels of Th1 cytokines and the IL-4 antagonist IL-4δ2. J. Immunol. 172:6938–6943 [DOI] [PubMed] [Google Scholar]
- 23. Dheda K., van Zyl Smit R., Badri M., Pai M. 2009. T-cell interferon-gamma release assays for the rapid immunodiagnosis of tuberculosis: clinical utility in high-burden vs. low-burden settings. Curr. Opin. Pulm. Med. 15:188–200 [DOI] [PubMed] [Google Scholar]
- 24. Dimitrov I., Garnev P., Flower D. R., Doytchinova I. 2010. EpiTOP—a proteochemometric tool for MHC class II binding prediction. Bioinformatics 26:2066–2068 [DOI] [PubMed] [Google Scholar]
- 25. Fan X., Gao Q., Fu R. 2009. Differential immunogenicity and protective efficacy of DNA vaccines expressing proteins of Mycobacterium tuberculosis in a mouse model. Microbiol. Res. 164:374–382 [DOI] [PubMed] [Google Scholar]
- 26. Flynn J. L. 2004. Immunology of tuberculosis and implications in vaccine development. Tuberculosis (Edinb.) 84:93–101 [DOI] [PubMed] [Google Scholar]
- 27. Gupta S. K., et al. 2011. Identification of immunogenic consensus T-cell epitopes in globally distributed influenza-A H1N1 neuraminidase. Infect. Genet. Evol. 11:308–319 [DOI] [PubMed] [Google Scholar]
- 28. Hanekom W. A., Lawn S. D., Dheda K., Whitelaw A. 2010. Tuberculosis research update. Trop. Med. Int. Health 15:981–989 [DOI] [PubMed] [Google Scholar]
- 29. Hanif S. N. M., El-Shamy A. M., Al-Attiyah R., Mustafa A. S. 2008. Whole blood assays to identify Th1 cell antigens and peptides encoded by Mycobacterium tuberculosis-specific RD1 genes. Med. Princ. Pract. 17:244–249 [DOI] [PubMed] [Google Scholar]
- 30. Harboe M., et al. 2002. Generation of antibodies to the signal peptide of the MPT83 lipoprotein of Mycobacterium tuberculosis. Scand. J. Immunol. 55:82–87 [DOI] [PubMed] [Google Scholar]
- 31. Hawkridge A. 2009. Clinical studies of TB vaccines. Hum. Vaccin. 5:773–776 [DOI] [PubMed] [Google Scholar]
- 32. Hewinson R. G., Michell S. L., Russell W. P., McAdam R. A., Jacobs W. R., Jr 1996. Molecular characterization of MPT83: a seroreactive antigen of Mycobacterium tuberculosis with homology to MPT70. Scand. J. Immunol. 43:490–499 [DOI] [PubMed] [Google Scholar]
- 33. Kamath A. T., Feng C. G., Macdonald M., Briscoe H., Britton W. J. 1999. Differential protective efficacy of DNA vaccines expressing secreted proteins of Mycobacterium tuberculosis. Infect. Immun. 67:1702–1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lalvani A., et al. 2001. Enumeration of T cells specific for RD1-encoded antigens suggests a high prevalence of latent Mycobacterium tuberculosis infection in healthy urban Indians. J. Infect. Dis. 183:469–477 [DOI] [PubMed] [Google Scholar]
- 35. Lönnroth K., Raviglione M. M. 2008. Global epidemiology of tuberculosis: prospects for control. Semin. Respir. Crit. Care Med. 29:481–491 [DOI] [PubMed] [Google Scholar]
- 36. Mahairas G. G., Sabo P. J., Hickey M. J., Singh D. C., Stover C. K. 1996. Molecular analysis of genetic differences between Mycobacterium bovis BCG and virulent M. bovis. J. Bacteriol. 178:1274–1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Malen H., Berven F. S., Fladmark K. E., Wiker H. G. 2007. Comprehensive analysis of exported proteins from Mycobacterium tuberculosis H37Rv. Proteomics 7:1702–1718 [DOI] [PubMed] [Google Scholar]
- 38. Mustafa A. S. 2000. HLA-restricted immune response to mycobacterial antigens: relevance to vaccine design. Hum. Immunol. 61:166–171 [DOI] [PubMed] [Google Scholar]
- 39. Mustafa A. S. 2001. Biotechnology in the development of new vaccines and diagnostic reagents against tuberculosis. Curr. Pharm. Biotechnol. 2:157–173 [DOI] [PubMed] [Google Scholar]
- 40. Mustafa A. S. 2005. Recombinant and synthetic peptides to identify Mycobacterium tuberculosis antigens and epitopes of diagnostic and vaccine relevance. Tuberculosis (Edinb.) 85:367–376 [DOI] [PubMed] [Google Scholar]
- 41. Mustafa A. S. 2005. Mycobacterial gene cloning and expression, comparative genomics, bioinformatics and proteomics in relation to the development of new vaccines and diagnostic reagents. Med. Princ. Pract. 14(Suppl. 1):27–34 [DOI] [PubMed] [Google Scholar]
- 42. Mustafa A. S. 2009. Vaccine potential of Mycobacterium tuberculosis-specific genomic regions: in vitro studies in humans. Expert Rev. Vaccines 8:1309–1312 [DOI] [PubMed] [Google Scholar]
- 43. Mustafa A. S. 2009. Th1-cell reactivity and HLA-DR binding prediction for promiscuous recognition of MPT63 (Rv1926c), a major secreted protein of Mycobacterium tuberculosis. Scand. J. Immunol. 69:213–222 [DOI] [PubMed] [Google Scholar]
- 44. Mustafa A. S. 2009. HLA-promiscuous Th1-cell reactivity of MPT64 (Rv1980c), a major secreted antigen of Mycobacterium tuberculosis, in healthy subjects. Med. Princ. Pract. 18:385–392 [DOI] [PubMed] [Google Scholar]
- 45. Mustafa A. S. 2010. In silico binding predictions for identification of HLA-DR-promiscuous regions and epitopes of Mycobacterium tuberculosis protein MPT64 (Rv1980c), and their recognition by human Th1 cells. Med. Princ. Pract. 19:367–372 [DOI] [PubMed] [Google Scholar]
- 46. Mustafa A. S. 2010. Cell mediated immunity assays identify proteins of diagnostic and vaccine potential from genomic regions of difference of Mycobacterium tuberculosis. Kuwait Med. J. 42:98–105 [Google Scholar]
- 47. Mustafa A. S., Abal A. T., Shaban F., El-Shamy A. M., Amoudy H. A. 2005. HLA-DR binding prediction and experimental evaluation of mycolyltransferase (Ag85B), a major secreted antigen of Mycobacterium tuberculosis. Med. Princ. Pract. 14:140–146 [DOI] [PubMed] [Google Scholar]
- 48. Mustafa A. S., Al-Attiyah R., Hanif S. N. M., Shaban F. A. 2008. Efficient testing of large pools of Mycobacterium tuberculosis RD1 peptides and identification of major antigens and immunodominant peptides recognized by human Th1 cells. Clin. Vaccine Immunol. 15:916–924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mustafa A. S., Al-Saidi F., El-Shamy A. S., Al-Attiyah R. 2011. Cytokines in response to proteins predicted in genomic regions of difference of Mycobacterium tuberculosis. Microbiol. Immunol. 55:267–278 [DOI] [PubMed] [Google Scholar]
- 50. Mustafa A. S., El-Shamy A. M., Madi N. M., Amoudy H. A., Al-Attiyah R. 2008. Cell-mediated immune responses to complex and single mycobacterial antigens in tuberculosis patients with diabetes. Med. Princ. Pract. 17:325–330 [DOI] [PubMed] [Google Scholar]
- 51. Mustafa A. S., Lundin K. E. A., Meloen R. H., Shinnick T. M., Oftung F. 1999. Identification of promiscuous epitopes from the mycobacterial 65-kilodalton heat shock protein (HSP65) recognized by human CD4+ T cells of the Mycobacterium leprae memory repertoire. Infect. Immun. 67:5683–5689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mustafa A. S., Lundin K. E. A., Meloen R. H., Oftung F. 2000. Cross-reactive epitopes and HLA-restriction elements in human T cell recognition of the Mycobacterium leprae 18-kD heat shock protein. Clin. Exp. Immunol. 120:85–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mustafa A. S., Shaban F. A. 2006. Propred analysis and experimental evaluation of promiscuous Th1 cell epitopes of three major secreted antigens of Mycobacterium tuberculosis. Tuberculosis (Edinb.) 86:115–124 [DOI] [PubMed] [Google Scholar]
- 54. Mustafa A. S., Shaban F. 2010. Mapping of Th1-cell epitope regions of Mycobacterium tuberculosis protein MPT64 (Rv1980c) using synthetic peptides and T-cell lines from M. tuberculosis-infected healthy humans. Med. Princ. Pract. 19:122–128 [DOI] [PubMed] [Google Scholar]
- 55. Mustafa A., et al. 2006. Immunogenicity of Mycobacterium tuberculosis antigens in Mycobacterium bovis BCG-vaccinated and M. bovis-infected cattle. Infect. Immun. 74:4566–4572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nielsen M., Lund O. 2009. NN-align. An artificial neural network-based alignment algorithm for MHC class II peptide binding prediction. BMC Bioinformatics 10:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Okkels L. M., et al. 2003. PPE protein (Rv3873) from DNA segment RD1 of Mycobacterium tuberculosis: strong recognition of both specific T-cell epitopes and epitopes conserved within the PPE family. Infect. Immun. 71:6116–6612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pan Y., et al. 2003. Combined recombinant DNA vaccine results in significant protection against Mycobacterium tuberculosis. Sheng Wu Hua Xue Yu Sheng Wu Wu Li Xue Bao (Shanghai) 35:71–76(In Chinese.) [PubMed] [Google Scholar]
- 59. Pathan A. A., et al. 2001. Direct ex vivo analysis of antigen-specific IFN-gamma-secreting CD4 T cells in Mycobacterium tuberculosis-infected individuals: associations with clinical disease state and effect of treatment. J. Immunol. 167:5217–5225 [DOI] [PubMed] [Google Scholar]
- 60. Ravn P., et al. 2005. Prospective evaluation of a whole-blood test using Mycobacterium tuberculosis-specific antigens ESAT-6 and CFP-10 for diagnosis of active tuberculosis. Clin. Diagn. Lab. Immunol. 12:491–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sai Priya V. H., Latha G. S., Hasnain S. E., Murthy K. J., Valluri V. L. 2010. Enhanced T cell responsiveness to Mycobacterium bovis BCG r32-kDa Ag correlates with successful anti-tuberculosis treatment in humans. Cytokine 52:190–193 [DOI] [PubMed] [Google Scholar]
- 62. Singh H., Raghava G. P. S. 2001. ProPred: prediction of HLA-DR binding sites. Bioinformatics 17:1236–1237 [DOI] [PubMed] [Google Scholar]
- 63. Storla D. G., et al. 2009. Use of interferon gamma-based assay to diagnose tuberculosis infection in health care workers after short term exposure. BMC Infect. Dis. 9:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tian X., Cai H., Zhu Y. X. 2005. Immunogenicity and protection of divalent DNA vaccine encoding antigens MPT83 and MPT64 of Mycobacterium tuberculosis. Zhonghua Yi Xue Za Zhi. 85:1410–1413 (In Chinese.) [PubMed] [Google Scholar]
- 65. Valle M. T., et al. 2001. Epitope focus, clonal composition and Th1 phenotype of the human CD4 response to the secretory mycobacterial antigen Ag85. Clin. Exp. Immunol. 123:226–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Vassilopoulos D., Stamoulis N., Hadziyannis E., Archimandritis A. J. 2008. Usefulness of enzyme-linked immunospot assay (Elispot) compared to tuberculin skin testing for latent tuberculosis screening in rheumatic patients scheduled for anti-tumor necrosis factor treatment. J. Rheumatol. 35:1271–1276 [PubMed] [Google Scholar]
- 67. Wang P., et al. 2008. A systematic assessment of MHC class II peptide binding predictions and evaluation of a consensus approach. PLoS Comput. Biol. 4:e1000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Whelan A. O., et al. 2010. Development of a skin test for bovine tuberculosis for differentiating infected from vaccinated animals. J. Clin. Microbiol. 48:3176–3181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. World Health Organization 2010. Global tuberculosis control. WHO/HTM/TB/2010.7. World Health Organization, Geneva, Switzerland [Google Scholar]
- 70. Xue T., et al. 2004. RNA encoding the MPT83 antigen induces protective immune responses against Mycobacterium tuberculosis infection. Infect. Immun. 72:6324–6329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Zhang H., et al. 2010. Recombinant Mycobacterium smegmatis expressing an ESAT6-CFP10 fusion protein induces anti-mycobacterial immune responses and protects against Mycobacterium tuberculosis challenge in mice. Scand. J. Immunol. 72:349–357 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.