Abstract
Candida albicans and mutans streptococci are frequently detected in dental plaque biofilms from toddlers afflicted with early childhood caries. Glucosyltransferases (Gtfs) secreted by Streptococcus mutans bind to saliva-coated apatite (sHA) and to bacterial surfaces, synthesizing exopolymers in situ, which promote cell clustering and adherence to tooth enamel. We investigated the potential role Gtfs may play in mediating the interactions between C. albicans SC5314 and S. mutans UA159, both with each other and with the sHA surface. GtfB adhered effectively to the C. albicans yeast cell surface in an enzymatically active form, as determined by scintillation spectroscopy and fluorescence imaging. The glucans formed on the yeast cell surface were more susceptible to dextranase than those synthesized in solution or on sHA and bacterial cell surfaces (P < 0.05), indicating an elevated α-1,6-linked glucose content. Fluorescence imaging revealed that larger numbers of S. mutans cells bound to C. albicans cells with glucans present on their surface than to yeast cells without surface glucans (uncoated). The glucans formed in situ also enhanced C. albicans interactions with sHA, as determined by a novel single-cell micromechanical method. Furthermore, the presence of glucan-coated yeast cells significantly increased the accumulation of S. mutans on the sHA surface (versus S. mutans incubated alone or mixed with uncoated C. albicans; P < 0.05). These data reveal a novel cross-kingdom interaction that is mediated by bacterial GtfB, which readily attaches to the yeast cell surface. Surface-bound GtfB promotes the formation of a glucan-rich matrix in situ and may enhance the accumulation of S. mutans on the tooth enamel surface, thereby modulating the development of virulent biofilms.
INTRODUCTION
Bacterial and fungal interactions commonly occur within the human body that often influence the transition of the host from a healthy to a diseased state (46). Candida albicans is the most commonly detected fungal organism found on human mucosal surfaces, and it often associates with a variety of pathogenic bacterial species, including Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus (41, 46). In the human mouth, C. albicans colonizes mucosal and prosthetic surfaces while interacting with a wide range of oral Streptococcus species, which can lead to the formation of complex microbial communities (17, 18). Pathological changes in the oral mucosa under prostheses, known as denture stomatitis, are primarily caused by trauma, a lack of access of saliva, and C. albicans colonization of both soft-tissue and acrylic surfaces (9). However, oral streptococci, particularly Streptococcus gordonii and Streptococcus sanguinis, are also frequently detected in addition to C. albicans (9, 17, 57). Although much of the prior research has focused on the role of the fungus in soft-tissue complications and its interactions with S. gordonii, C. albicans may also influence the pathogenesis of dental caries disease (24), particularly in early childhood caries (ECC) (12, 37, 39, 50).
ECC, a highly virulent variant of the ubiquitous disease dental caries, is painful, difficult, and expensive to treat (5). ECC is a public health problem affecting mostly socially deprived toddlers and preschool children (5, 13). The disease is characterized by an overwhelming infectious challenge and caries-promoting feeding behaviors (5, 60). Infection by mutans streptococci (particularly Streptococcus mutans) and the subsequent establishment of virulent biofilms on the tooth surface, along with the frequent consumption of dietary sugar (e.g., sucrose), are associated with an increased prevalence of ECC (45, 60). However, other additional acidogenic and aciduric organisms may also be associated with the progression of the disease (20).
S. mutans thrives in the complex oral microbiome because it (i) effectively utilizes dietary sucrose (and possibly starch) to rapidly synthesize exopolysaccharides (EPS) through glucosyltransferases (Gtfs) and a fructosyltransferase that are adsorbed to surfaces, (ii) adheres tenaciously to glucan-coated surfaces, and (iii) is highly acidogenic and acid tolerant (33, 48, 51). This unique combination of virulence attributes allows S. mutans to effectively colonize the tooth enamel surface, form a polymeric matrix, and create an acidic milieu, enhancing the development of pathogenic biofilms. The Gtfs secreted by S. mutans are incorporated into the salivary pellicle that is formed on a saliva-coated hydroxyapatite (sHA) surface, and they can synthesize large amounts of EPS in situ (6, 59, 62). Furthermore, Gtfs, particularly GtfB, bind to the cell surfaces of other oral microorganisms that do not produce glucans (e.g., Actinomyces and Veillonella spp.), which makes them de facto glucan producers (40, 59). Surface-associated glucans provide sites for avid binding by S. mutans (and possibly other oral microorganisms) that enhance cohesion between cells and adherence to the sHA surface. These glucan-mediated processes promote the accumulation and establishment of cariogenic organisms within an EPS-rich matrix that is tightly adherent to the tooth surface (44). The presence of S. mutans on oral surfaces and constant exposure to dietary sucrose favor the production of EPS (such as glucans) and acids, which creates a highly cohesive and aciduric environment (27, 38, 44). The low pH in the matrix and at the biofilm-tooth surface interface results in the dissolution of enamel.
C. albicans also adheres to dental surfaces, produces EPS, forms biofilms, and is highly acidogenic and acid tolerant (19, 25). Furthermore, C. albicans appears to enhance S. mutans biofilm formation in vitro (47, 57). Microbiological studies of saliva and plaque-biofilm samples from children with ECC reveal a direct association between the presence of C. albicans (along with S. mutans) and the development of the disease (12, 37, 39). Recently, we detected both C. albicans and S. mutans in plaque-biofilm samples collected from children affected by severe ECC using species-specific probes designed for real-time quantitative PCR (P. S. Agidi, M. I. Klein, and H. Koo, unpublished data). Furthermore, the ECC plaque samples contained elevated amounts of water-insoluble EPS compared to those of samples from healthy individuals. However, the underlying mechanisms that modulate this potential fungal-bacterial interaction have not been explored. It has been shown that C. albicans and S. mutans enhance binding to each other and to acrylic surfaces in the presence of sucrose (8, 18). Scanning electron microscopy images also reveal glucan-like structures that form between cocci and yeasts, suggesting that glucans may play a role in mediating their interactions (8).
Therefore, we hypothesized that S. mutans-derived Gtfs would bind to the C. albicans cell surface to produce EPS in situ. The presence of surface-formed glucans would increase S. mutans binding to the yeast cell and concomitantly enhance the ability of C. albicans to adhere to the sHA surface. If these hypotheses are supportable, C. albicans may help to promote the formation of a glucan-rich matrix and may also enhance the accumulation of S. mutans on the tooth enamel surface. This relationship, in addition to enhanced acidity (25), may explain the detection of elevated amounts of S. mutans (along with C. albicans) and EPS in the plaque from toddlers with ECC, thereby modulating the development of virulent biofilms.
MATERIALS AND METHODS
Microbial strains and culture conditions.
The bacterial strains used for the production of Gtfs were Streptococcus anginosus KSB8, which harbors the gtfB gene (for GtfB production); S. mutans WHB 410, from which the gtfB, gtfD, and ftf genes were deleted (for GtfC production); and S. anginosus NH5, which contains the gtfD gene (for GtfD production). S. mutans UA159 (ATCC 700610; serotype c), a proven virulent cariogenic dental pathogen selected for genomic sequencing (1), and C. albicans SC5314, a well-characterized strain whose genome has been sequenced, were used for binding experiments; the C. albicans strain used was kindly provided by Constantine Haidaris (Department of Microbiology and Immunology, University of Rochester Medical Center). The cultures were stored at −80°C in tryptic soy broth (S. mutans) or Sabouraud dextrose broth (C. albicans) containing 20% glycerol.
C. albicans SC5314 and S. mutans UA159 cells were grown to mid-exponential phase (optical densities at 600 nm [OD600], 0.65 and 0.5, respectively) in ultrafiltered (membrane with a 10-kDa molecular mass cutoff) tryptone-yeast extract broth (UFTYE; pH 7.0 and 5.5 for S. mutans and C. albicans, respectively) containing 1% (wt/vol) glucose and harvested by centrifugation (6,000 × g, 10 min, 4°C). The cells were then washed three times in ice-cold adsorption buffer (50 mM KCl, 1.0 mM KPO4, 1.0 mM CaCl2, 0.1 mM MgCl2, pH 6.5). C. albicans cells were in yeast form, as observed microscopically. An S. mutans cell suspension was sonicated using a Branson Sonifier 450 (five 15-s pulses with 5-s intervals at 20 W; Branson Ultrasonics Corp., Danbury, CT) to obtain a single-cell suspension (verified by light microscopy). The OD600 of both cell preparations was adjusted to 1.0 ± 0.05, and the cells were counted in a Petroff-Hausser cell-counting chamber (1 × 109 yeast cells/ml and 9 × 109 S. mutans cells/ml; Hausser Scientific Partnership, Horsham, PA).
Gtf enzymes.
The GtfB, GtfC, and GtfD enzymes (EC 2.4.1.5) were prepared from culture supernatants of S. anginosus and S. mutans WHB410 constructs and purified to near homogeneity by hydroxylapatite (HA) column chromatography as described by Wunder and Bowen (63) and Koo et al. (29). Gtf activity was measured by the incorporation of [14C]glucose from labeled sucrose (NEN Research Products, Boston, MA) into glucans (29, 51). One unit of enzyme activity was defined as the amount of Gtf enzyme that incorporates 1 μmol of glucose into glucans over the 2-h reaction.
Gtfs binding to the C. albicans cell surface.
The Gtfs were adsorbed to the microbial cells as detailed elsewhere (51, 59). C. albicans yeast cells (ranging from 0.25 × 109 to 1 × 109/ml) were mixed with saturating amounts of each of the Gtfs (25 μg/ml, 3 U) in adsorption buffer and incubated for 60 min at 37°C; yeast cells were also incubated in buffer alone (without Gtf) as controls. Following adsorption of the enzyme, the cells were pelleted by centrifugation (6,000 × g, 10 min. 4°C) and the supernatant (containing unbound Gtf) was saved. The pellet was resuspended (washed) with adsorption buffer to remove the loosely bound Gtf and centrifuged, and the supernatant was saved; the washing procedure was repeated twice. The washed, Gtf-coated yeast cells (or cells without adsorbed Gtf) were resuspended in 250 μl of adsorption buffer and mixed with 250 μl of [14C]glucose-sucrose substrate (0.2 μCi/ml; 100.0 mmol of sucrose/liter, 20 μmol of dextran 9000/liter, and 0.02% sodium azide in adsorption buffer, pH 6.5) for 2 h at 37°C. In addition, each of the supernatants (250 μl) was also incubated with the sucrose substrate. The amount of enzymatic activity of surface-bound and unbound Gtfs was measured by the incorporation of [14C]glucose from labeled sucrose into glucans using scintillation counting (51). All assays were done in quadruplicate in at least three different experiments. Results from our preliminary experiments show that GtfB binds the most effectively to C. albicans surfaces, followed by GtfC. In contrast, GtfD bound poorly to the yeast cell surface (see Fig. S1 in the supplemental material). GtfB was therefore selected for further investigation.
Fluorescence imaging of surface-adsorbed glucans.
Glucan formation by GtfB adsorbed to the yeast cell surface was visualized by a novel fluorescence imaging technique using labeled soluble dextran as described by Klein et al. (23). Soluble dextrans serve as primers for GtfB and are incorporated into newly formed glucans by the enzyme during extracellular polysaccharide synthesis (14, 23). Briefly, 1 μM Alexa Fluor 647-labeled dextran conjugate (10,000 molecular weight; absorbance/fluorescence emission maxima, 647/668 nm; Molecular Probes Inc., Eugene, OR) was added to a reaction mixture containing C. albicans yeast cells (1 × 109/ml) with or without surface-adsorbed GtfB and sucrose substrate (final concentration of 100 mmol sucrose/liter in adsorption buffer, pH 6.5) for 1 h of incubation at 37°C; the fluorescence-labeled dextran does not stain the microbial cells at the concentrations used in this study (23). Following incubation, 20 μl of the mixture was placed on a glass slide and imaging was performed using a 40× water immersion objective lens (0.8 numerical aperture) in a Leica TCS SP1 microscope (Leica Lasertechnik GmbH, Heidelberg, Germany) equipped with argon ion and helium neon lasers fixed at 488 and 633 nm. Triple dichroic (488/543/633) and emission filters (Chroma Technology Corp., Rockingham, VT) were selected for detection of Alexa Fluor 647. Differential interference contrast (DIC) was also used in combination with fluorescence imaging to visualize C. albicans yeast cells (23).
Mutanase and dextranase susceptibility.
The glucans formed on yeast cells by surface-adsorbed GtfB were examined for susceptibility to glucanohydrolases as described by Kopec et al. (30). Mutanase [α(1,3)-glucanase; EC 3.2.1.59] produced by Trichoderma harzianum and dextranase [α(1,6)-glucanase; EC 3.2.1.11] produced by Penicillium aculeatum were used in this experiment. The enzymes (Novo Nordisk, Denmark) were kindly provided by William H. Bowen (Center for Oral Biology, University of Rochester Medical Center). Briefly, glucans were formed on the yeast cell surface using the methods described for the GtfB binding assay. The surface glucans were precipitated, collected by centrifugation, and washed four times with ice-cold 75% (vol/vol) ethanol, and the amounts were determined by scintillation counting (51). One hundred micrograms of glucans was then resuspended in 0.1 M sodium acetate buffer (pH 5.5) and sonicated (three 10-s pulses at an output of 7 W) to create a homogeneous suspension. The suspension was mixed with saturating amounts of mutanase or dextranase (10 U of enzyme) in 0.1 M sodium acetate buffer (pH 5.5; optimum pH for enzymatic activity) in a total reaction volume of 300 μl and incubated for 4 h at 30°C as detailed elsewhere (15, 30). In addition, the enzyme susceptibility of glucans formed by GtfB adsorbed to sHA, S. mutans cell surfaces, and in solution phase was determined. One unit of activity of the mutanase or dextranase was defined as the amount of enzyme that releases 1 μmol of reducing sugar from preformed mutan or dextran over a 4-h reaction as determined colorimetrically (15, 30, 55).
Fluorescence imaging of S. mutans bound to C. albicans.
S. mutans cells (grown to mid-log phase) were washed three times with adsorption buffer, resuspended, and sonicated to obtain single cells (28). The bacterial cells were labeled with 2.5 μM SYTO 9 green fluorescent nucleic acid stain (480/500 nm; Molecular Probes Inc., Eugene, OR) as described by Klein et al. (23). Fluorescently labeled S. mutans (1 × 109 cells/ml) was mixed with (i) unlabeled C. albicans (1 × 109 cells/ml) with surface-bound GtfB glucans (labeled with Alexa Fluor 647) or (ii) unlabeled C. albicans without surface glucans and incubated at 37°C for 2 h. After incubation, the suspensions were immediately visualized using a confocal microscope (Leica TCS SP1). Triple dichroic (488/543/633) and emission filters (Chroma Technology Corp., Rockingham, VT) were selected for detection of SYTO 9 and Alexa Fluor 647, and DIC was also used to visualize the microbial cells (23).
C. albicans adherence to experimental salivary pellicle (sHA) and to glucans in the pellicle (gsHA) formed on a hydroxyapatite surface.
Adherence assays were conducted with radiolabeled C. albicans yeast cells as described by Schilling and Bowen (51) and Branting et al. (8). To study the adherence of yeast cells to sHA, HA beads were incubated with clarified whole saliva (free of Gtf activity) to form an experimental salivary pellicle on the apatite surface (28, 29). To study microbial adherence to gsHA, sHA beads were exposed to saturating amounts of GtfB and incubated with sucrose (100 mmol/liter, final concentration) at 37°C for 4 h to allow glucan formation on the surface (28, 51). The radiolabeled yeast cells were obtained from UFTYE (pH 5.5) containing 3 μCi/ml l-[4,5-3H]leucine (Perkin-Elmer Life and Analytical Sciences, Boston, MA) (8). Uncoated or glucan-coated C. albicans cells (1 ×109/ml) were incubated with sHA or gsHA. After 60 min, the beads were washed using adsorption buffer to remove unbound cells, and the number of adherent yeast cells was determined by liquid scintillation counting (28, 51).
Micropipette technique.
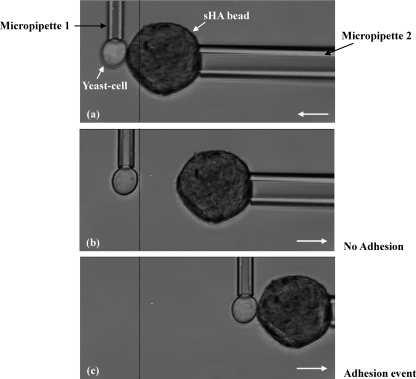
Micropipette experiments were performed on the stage of an Olympus IX70 inverted microscope (Spectra Services Inc., Rochester, NY) using a Hamamatsu RS-70 charge-coupled device (Microvideo Instruments, Avon, MA) at room temperature (22°C) as described previously (34, 35). Two micropipettes were positioned perpendicular to each other in a dual-entry chamber mounted on the microscope stage, one to hold the bead (sHA or gsHA) and another to manipulate the single cell (a yeast cell with or without surface-formed glucans) (see Results and Fig. 5). A C. albicans cell with surface-formed glucans was carefully held by aspirating a yeast cell in a region of the surface where large aggregates of glucan were not evident. C. albicans displaying large masses of glucan with extensive dispersion of the polysaccharides away from the yeast cell surface were avoided to keep from fouling the pipette tip. Nevertheless, the analysis reflects the true binding interaction, as the chemistry of adhesion would be the same whether a large mass of glucan or a thin coating were present on the cell surface. The bead and the yeast cell were held in contact for 5 s and then separated. The pipette holding the cell was made to be flexible so that a measurable deflection could be observed as the cell and bead were separated when there was adhesion between the two surfaces. The experiments were recorded on a DVD and subsequently analyzed using Scion Image software to determine the fraction of contacts resulting in adhesion. An adhesion event was scored when there was detectable deflection of the pipette holding the cell when the bead was withdrawn (see Results and Fig. 5). Adhesion probability was calculated as the total number of adhesive events divided by the total number of touches, which indicates the avidity of binding between the two surfaces (35).
Fig. 5.
Interaction between a sHA bead and a single yeast cell during a micropipette experiment. (a) Initial contact (when micropipette 2 moves toward micropipette 1 until the sHA bead touches the yeast cell). (b) No adhesion (after the bead is pulled back beyond the initial contact point). (c) Adhesive event (after the bead is pulled back with the attached cell beyond the initial contact point). An adhesive event is recorded when micropipette 1 (holding a C. albicans yeast cell) moves beyond the initial contact point due to binding of the cell to the sHA bead (immobilized by micropipette 2).
S. mutans accumulation on sHA in the presence of glucan-coated C. albicans.
Adhesion assays were conducted according to Branting et al. (8) and Schilling and Bowen (51), with the following modifications. Radiolabeled S. mutans cells were obtained from UFTYE (pH 7.0) containing 5 μCi/ml [3H]thymidine (Perkin-Elmer Life and Analytical Sciences, Boston, MA) (51). Radiolabeled S. mutans, unlabeled C. albicans, and sHA beads were mixed together under 3 distinct experimental conditions, (i) S. mutans plus C. albicans plus sHA, (ii) S. mutans plus C. albicans GtfB (but no glucans) plus sHA, and (iii) S. mutans plus C. albicans GtfB glucans plus sHA. In addition, S. mutans alone was incubated with sHA (S. mutans plus sHA). The final concentrations of bacterial and yeast cells were 9 × 109 S. mutans cells/ml and 1 × 109 C. albicans cells/ml, for a proportion similar to that described by Branting et al. (8). The mixed cells were incubated with sHA in adsorption buffer at 37°C for 2 h. Following incubation, the beads were washed with adsorption buffer to remove unbound cells and the number of S. mutans cells adherent to sHA was determined by liquid scintillation counting (8, 51). Fluorescence and DIC imaging of each of the conditions were also performed using SYTO 9, Alexa Fluor 647, and DIC as described in the previous sections.
Statistical analyses.
An exploratory analysis of the binding, micropipette, and glucan susceptibility assay data was performed to select the statistical test. The assumptions of equality of variances and normal distribution of errors were also checked. The data were then analyzed using analysis of variance (ANOVA), and the F test was used to test for differences among the groups. When significant differences were detected, pairwise comparisons were made between all of the groups using Tukey's method to adjust for multiple comparisons. JMP version 8.02 statistical software was used to perform the analyses. The level of significance was set at 5%.
RESULTS
S. mutans GtfB binds to C. albicans yeast cells in an enzymatically active form.
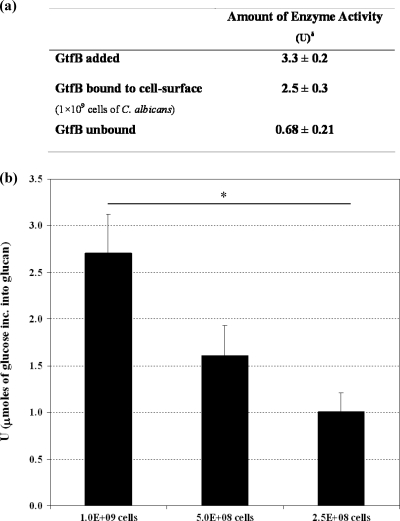
C. albicans SC5314 cells (1 × 109/ml) were incubated with GtfB (25 μg/ml, 3 U) and then washed to remove unbound GtfB. The amount of GtfB activity contributed by the Gtf adsorbed to the yeast cell surface, as well as that from any unbound GtfB, is shown in Fig. 1a. After the initial removal of unbound or loosely attached GtfB, further washes failed to desorb detectable amounts of GtfB (data not shown). These data indicate that GtfB was adsorbed to the yeast cell surface and was enzymatically active. In addition, the amount of glucan produced by surface-adsorbed GtfB was proportional to the number of yeast cells available for GtfB binding (Fig. 1b), suggesting that the binding of GtfB to the yeast cell surface was saturable.
Fig. 1.
Amount of enzyme activity of GtfB adsorbed to C. albicans SC5314 cells. δ, 1 U of Gtf activity was defined as the amount of enzyme that incorporates 1 μmol of glucose into glucan over 2 h. C. albicans cells were incubated with GtfB and washed to remove unbound enzyme. Cells with adsorbed GtfB (or without GtfB bound, as a control) were then exposed to sucrose, and glucan formation was assayed after 2 h of incubation. (a) Amounts of enzyme activity of GtfB adsorbed on the yeast cell surface and unbound GtfB (data shown are means ± standard deviations; n=12). (b) Amounts of glucans formed according to the number of yeast cells available for GtfB binding. The asterisk indicates that the values (error bars shown standard deviations; n=12) are statistically significantly different from each other (P < 0.05, ANOVA, comparison for all pairs using Tukey's test).
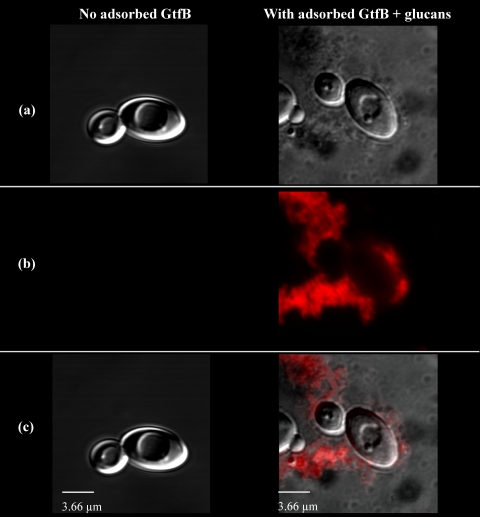
To further confirm that glucans form on the cell surface, we used fluorescence and DIC imaging to directly observe the polymers formed in situ. C. albicans cells, with or without adsorbed GtfB, were incubated in sucrose substrate (or buffer alone) and then visualized using confocal microscopy. As shown in Fig. 2, adherent glucans of various sizes and structures can be clearly visualized on the C. albicans cell surface, which form a glucan-yeast complex (Fig. 2c). The yeast cell surface was covered by glucans not homogeneously but rather in an uneven manner, with some areas and some cells displaying more glucans than others. Considering that GtfB bound to the C. albicans surface, GtfB-adsorbed yeast cells were subjected to protein desorption under three conditions (2), isotonic (weakly bound), high-salt (moderately bound), and urea (strongly bound) elutions. No GtfB was observed in the isotonic elution. In contrast, GtfB was detected in the high-salt (mostly) and urea elutions, indicating that GtfB was at least moderately bound to the C. albicans yeast cell surface (see Fig. S2 in the supplemental material).
Fig. 2.
Visualization of glucans synthesized in situ by GtfB adsorbed to C. albicans SC5314 yeast cells. C. albicans cells were incubated with GtfB (or buffer) and washed to remove unbound GtfB. Cells with adsorbed GtfB (or without GtfB bound, as a control) were then exposed to sucrose, and glucan formation was assayed after 2 h of incubation. (a) DIC image of C. albicans cells after incubation with sucrose (100× oil objective, numerical aperture 1.4). (b) Image obtained with laser excitation at 633 nm for detection of glucans (Alexa Fluor 647). (c) Overlaid DIC and fluorescence images.
Hydrolysis of surface-bound glucans by mutanase and dextranase.
The glucans synthesized by GtfB adsorbed to sHA surfaces show a profile of α-1,3- and α-1,6-linked glucose distinct from that of the polymer molecule formed by the same enzyme in solution (30, 59). Thus, we also investigated whether the GtfB adsorbed to the yeast cell surface could synthesize distinctive glucans. We determined the susceptibility of glucans (100 μg) synthesized on the C. albicans cell surface to the action of the glucanohydrolases (mutanase and dextranase) by measuring the reducing sugars released during digestion (Table 1). We also examined the digestion profile of glucans (100 μg) formed by GtfB present on sHA and on S. mutans cell surfaces. In general, all of the surface-adsorbed glucans were resistant to complete breakdown by either mutanase or dextranase, which agrees with previous observations (30). However, the extent of glucan digestion by dextranase was significantly different among the experimental conditions.
Table 1.
Susceptibility of glucans to digestion by mutanase and dextranasea
| Enzyme and site of GtfB glucan formation | Mean amt of total reducing sugars released (μg) ± SD |
|---|---|
| Mutanase | |
| Solution | 65.3 ± 6.8 |
| sHA surface | 49.1 ± 10.1 |
| S. mutans surface | 60.1 ± 11.8 |
| C. albicans surface | 58.0 ± 8.3 |
| Dextranase | |
| Solution | 11.9 ± 0.3 |
| sHA surface | 18.0 ± 4.9 |
| S. mutans surface | 19.7 ± 4.8 |
| C. albicans surface | 41.3 ± 6.7b |
The data shown are means of three separate experiments. For each experiment, 100 μg of glucan and 10 U of mutanase or 10 U of dextranase were used (15).
Statistically significantly different (P < 0.05, ANOVA, comparison for all pairs using Tukey's test).
Based on the total amount of reducing sugar released, glucans synthesized on the yeast cell surface were more susceptible to dextranase than those formed on either sHA or the S. mutans cell surface (P < 0.05). The data suggest that the polymer has an elevated amount and proportion of 1,6-linked glucose. The ratio of dextranase- to mutanase-susceptible glucans was higher in the polymer formed on the C. albicans yeast cell surface than in that on other surfaces (P < 0.05). The formation of distinctive surface-adsorbed glucans may provide unique binding sites for S. mutans to the yeast cell surface while simultaneously influencing the ability of C. albicans to adhere to the pellicle formed on the hydroxyapatite surface.
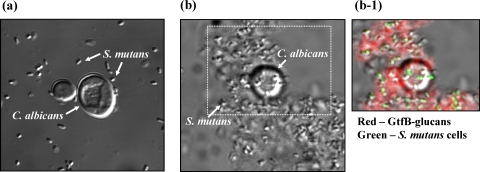
Glucans synthesized in situ promote S. mutans binding to C. albicans yeast cells.
S. mutans binds poorly to C. albicans yeast cells (8, 18). We sought to determine whether glucans formed by GtfB on the yeast cell surface could enhance S. mutans binding to yeast cells. Uncoated C. albicans or yeast cells with surface-formed glucans were incubated with S. mutans UA159 cells and then examined using fluorescence imaging and DIC microscopy. The photomicrograph in Fig. 3a shows few S. mutans cells bound to uncoated C. albicans cells. In contrast, large numbers of S. mutans cells can be observed bound to the glucans formed on the yeast cell surface (Fig. 3b). The selected field of view (Fig. 3b–1) shows individual fluorescently labeled bacterial cells (in green) that are mostly adherent to the glucan matrix (in red) formed on the C. albicans surface.
Fig. 3.
S. mutans UA159 cells binding to C. albicans SC5314 cells with and without surface-formed GtfB glucans. Cells of C. albicans (with or without surface-formed GtfB glucans) and S. mutans were incubated together (1 h) and then analyzed using DIC and fluorescence imaging. (a) DIC image of C. albicans and S. mutans cells after incubation (100× oil objective, numerical aperture 1.4). (b) DIC image of GtfB glucan on C. albicans and S. mutans cells after incubation. (b-1) Overlaid DIC and fluorescence images of the field of view selected in panel b. Laser excitation at 488 nm was used for detection of SYTO 9-labeled S. mutans cells (green), and laser excitation at 633 nm was used for detection of Alexa Fluor 647-labeled GtfB glucans (red).
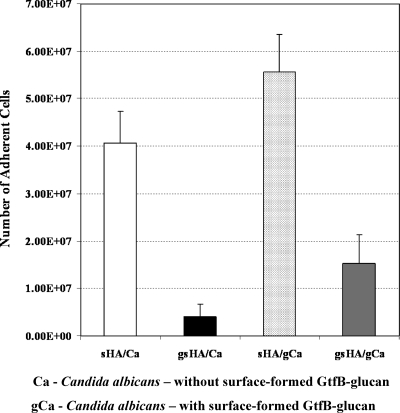
Glucans synthesized in situ affect C. albicans adherence to sHA and gsHA surfaces.
C. albicans can bind to acrylic and apatite surfaces (8, 47). Here we investigated whether glucans formed in situ influence the adherence of C. albicans yeast cells to sHA or gsHA. Radiolabeled C. albicans cells were incubated with either sHA or gsHA. In gsHA, the glucans form an amorphous polymeric layer which covers most of the sHA surface such that microbial binding to the apatite surface is mediated mostly by glucans formed in the pellicle (51). The results presented in Fig. 4 show that yeast cells bound in much higher numbers to the experimental salivary pellicle (sHA) than to glucans formed in the pellicle (gsHA) (P < 0.05). The presence of glucans on the yeast cell surface (gCa) also increased the adherence of C. albicans to gsHA compared to that of yeast cells without in situ glucans (P < 0.05; Fig. 4).
Fig. 4.
Adherence of C. albicans (with or without in situ GtfB glucan) to experimental salivary pellicle (sHA) and to glucans synthesized in the pellicle (gsHA) formed on a hydroxyapatite surface. The data shown are mean values ± standard deviations (n=12). All of the values are statistically significantly different from each other (P < 0.05, ANOVA, comparison for all pairs using Tukey's test), but the difference between the sHA/Ca and sHA/gCa values is not statistically significant (P > 0.05).
To further assess the ability of C. albicans cells to bind to sHA or gsHA, we measured the number of adherence events between individual C. albicans cells and single sHA or gsHA beads using a novel single-cell micromechanical approach. The micropipette technique (35) allows precise measurement of adhesion events between different bead-cell pairs, which would complement the binding assays using scintillation spectroscopy. An adhesive event is scored when there is detectable binding between the two interacting surfaces (as detailed in Fig. 5), which is used to calculate the adhesion probability. The adhesion probability of yeast cell-sHA bead binding was more than 80%, indicating a high avidity of binding between these two surfaces (Table 2). In contrast, the adhesive events of C. albicans were greatly reduced when it was interacting with gsHA, which is consistent with the yeast cells binding poorly to glucans formed in the pellicle (Fig. 4). The presence of glucans on the C. albicans yeast cell surface (gCa) enhanced adhesion to gsHA. The interactions between gCa and sHA showed a very high avidity of binding, such that the binding force between the surfaces exceeded the upper limit of the separation force that can be applied using the micropipette technique. Nevertheless, the micromechanical data further confirm the results obtained from scintillation spectroscopy analyses, showing that C. albicans (with or without surface glucans) binds effectively to sHA but much less effectively to gsHA.
Table 2.
Probability of adhesion between C. albicans (with or without in situ-formed glucan) and sHA (or gsHA) surfaces
| Conditiona | Mean adhesion probability (%) ± SDb |
|---|---|
| Ca-sHA | 80.5 ± 15.5 |
| Ca-gsHA | 1.8 ± 5.1 |
| gCa-sHA | —c |
| gCa-gsHA | 63.2 ± 19.1 |
Ca, C. albicans without surface-formed GtfB glucan; gCa, C. albicans with surface-formed GtfB glucan.
Adhesion probability was calculated as the total number of adhesive events divided by the total number of touches (contacts) (n=16). The values for Ca-sHA, Ca-gsHA, and gCa-gsHA are significantly different from each other (P < 0.05, ANOVA, comparison for all pairs using Tukey's test).
—, interaction between gCa and sHA not measurable by the micropipette technique because the force of binding between the surfaces exceeded the upper limit of the separation force that can be applied by the technique.
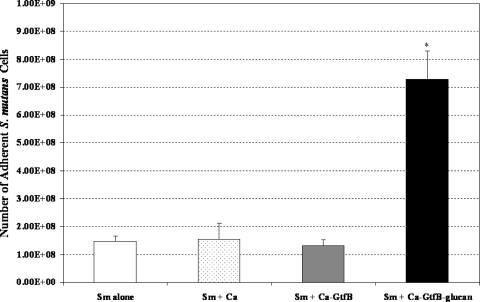
Interactions of S. mutans with in situ glucans formed on the C. albicans cell surface enhance bacterial accumulation on sHA.
The presence of glucans formed on the C. albicans cell surface enhanced the binding of S. mutans to the yeast cells. C. albicans adheres effectively to the experimental salivary pellicle (sHA). Thus, we investigated whether the presence of C. albicans (with or without surface-formed glucans) could enhance S. mutans accumulation on sHA surfaces when these strains were mixed together. In our adhesion experiments, the assays were conducted without sucrose to avoid de novo synthesis of glucans (see Materials and Methods). Figure 6 shows that the presence of glucan-coated yeast cells significantly enhances (5- to 6-fold increase) the accumulation of S. mutans on the sHA surface compared to that of S. mutans cells incubated alone or mixed with C. albicans without surface-formed glucans (P < 0.05). In addition, the same experimental conditions were analyzed using fluorescence imaging to visualize C. albicans-S. mutans-sHA interactions (see Fig. S3 in the supplemental material). The images show large numbers of S. mutans cells bound to glucan-coated C. albicans cells, which in turn were adherent to the sHA surface. We also found that the number of glucan-coated S. mutans cells alone bound to sHA was significantly lower than the number of bacterial cells bound when combined with glucan-coated C. albicans (see Fig. S4 in the supplemental material). The data indicate that C. albicans cells may facilitate S. mutans colonization of and accumulation on the sHA surface by acting as “bacterial carriers” when glucans are formed on the yeast cell surface.
Fig. 6.
Influence of C. albicans (with or without surface-formed glucan) on S. mutans accumulation on experimental salivary pellicle (sHA) formed on a hydroxyapatite surface. The data shown are mean values ± standard deviations (n=12). The value marked with an asterisk is significantly different from the others (P < 0.05, ANOVA, comparison for all pairs using Tukey's test). Sm, S. mutans; Ca, C. albicans; Ca-GtfB, C. albicans with surface-adsorbed GtfB (no glucan); Ca-GtfB-glucan, C. albicans with surface GtfB glucan.
DISCUSSION
The bacterial-fungal interactions in the presence of localized (e.g., physical trauma, poor dental hygiene, lack of saliva) and/or systemic insults (e.g., host immune system deficiencies) can lead to diseases at various sites in the human body, including the oral cavity (41, 46). Physical interactions (e.g., cell-to-cell adhesions), chemical exchanges (extracellular signaling molecules), and changes in the environment (e.g., pH) are common ways that bacteria and fungi impact each other's survival or virulence (46). The majority of studies have focused on the role of bacteria in enhancing Candida sp. carriage and infection processes in the oral cavity. For example, the adhesive interactions between C. albicans and oral streptococci, particularly S. gordonii, have been implicated in enhanced host colonization, biofilm formation, and virulence by the opportunistic pathogen at mucosal and acrylic surfaces (3, 17, 41). Our investigations show that C. albicans cells may also play a significant role in modulating extracellular matrix formation in situ and at the same time enhance S. mutans carriage on the tooth surface, which are critical factors in the development of virulent (cariogenic) biofilms, such as those associated with ECC.
Results from the present study have demonstrated that a streptococcal exoenzyme (GtfB) binds tightly to the C. albicans yeast cell surface, converting the cells to de facto glucan producers. These observations extend previous reports showing that GtfB binds to other, nonstreptococcal, bacteria, including Actinomyces naeslundii, Lactobacillus casei, and Veillonella sp. (22, 40, 59), and demonstrate that this versatile streptococcal molecule can also mediate cross-kingdom interactions.
The exact identities of the GtfB binding sites on the yeast cell surface are unknown. Previous studies have shown that the presence of six 65-amino-acid carboxyl-terminal direct repeating units of GtfB has a major role in the binding of the enzyme to the cell surface of oral streptococci. The C terminus of GtfB differs from that of GtfC and GtfD, which may explain the selective adsorption of the GtfB enzyme to bacterial surfaces (22, 59). However, the composition and molecular architecture of the cell wall of C. albicans are quite distinctive. The cell wall is composed primarily of β-glucan, chitin, and mannan (11). β-Glucans (branched polymers containing β-1,3 and β-1,6 linkages) are the main cell wall constituents. They are found throughout the cell wall, but β-1,3-glucans are concentrated in the inner portion near the plasma membrane, forming a rigid skeletal layer in association with chitin. The inner skeletal layer acts as a scaffold for a dense outer layer of fibrillar glycoproteins extending outward, which are connected to the rigid β-1,3-glucan by a flexible β-1,6 soluble glucan moiety (21, 58). In addition, C. albicans encodes a class of adhesins termed glycosylphosphatidylinositol-dependent cell wall proteins (GPI-CWPs). Among them, Als (agglutinin-like sequence), an immunoglobulin-like adhesin, and Eap1 (enhanced adherence to polystyrene) mediate the adhesion of C. albicans cells to polystyrene and endothelial and epithelial human cells (26, 32).
The selective binding of GtfB and changes in the glucan products (elevated α-1,6-linked glucose) suggest highly specific and C terminus-mediated interactions with cell wall components of C. albicans. Although there is no direct evidence in the current literature, it is conceivable that the C terminus and the glucan-binding domain (GBD) of GtfB may recognize and bind the glycoproteins, the soluble glucans, and/or mannan within the yeast cell wall structure and/or interact with GPI-CWP adhesins, which could also change the conformation and function of the enzymes. Disruption of the tertiary structure of the GBD could affect the (β/α)8 barrel structure in the catalytic domain, subsequent glucan binding, and the branching process. These changes could influence the assembly of glucans by GtfB that is adsorbed to the C. albicans cell surface, resulting in a distinctive polymer, as observed in this study. Clearly, there is a direct interaction between streptococcal GtfB and the C. albicans yeast cell surface. It is noteworthy that the expression of cell wall proteins changes during the transition of different morphological states of C. albicans cells (56), which may affect GtfB binding to their surface. We are currently investigating the binding affinity of GtfB for each of the C. albicans cell morphologies (yeast, pseudohyphae, and hyphae); our preliminary studies thus far have shown that pseudohyphae can also bind GtfB in active form. Further studies using C. albicans mutant strains defective in the expression of cell wall constituents (and distinct cell cycles/morphologies) and single-molecule force atomic spectroscopy should elucidate the (i) molecular/structural nature of GtfB binding sites on the cell surface, (ii) conformational changes, (iii) effects on glucans structure, and (iv) bacterial binding properties.
We also observed that glucans synthesized in situ may enhance the adhesive interactions between S. mutans and C. albicans yeast cells. It is well established that the binding interactions of C. albicans with S. gordonii are mediated by streptococcal Ag I/II polypeptides (SspB) and cell wall polysaccharides with C. albicans adhesins, such as Als3 (6, 42, 53, 57). In contrast, S. mutans (despite expressing Ag I/II) appears to bind poorly to C. albicans cells (18). In our experiments, only a few S. mutans cells bound directly to the yeast cell surface, confirming previous studies. However, bacterial adherence was greatly enhanced in the presence of glucans on the C. albicans cell surface. S. mutans expresses multiple non-Gtf glucan-binding proteins (Gbps), which provide, in addition to cell-bound Gtfs, an enhanced ability to adhere to the polymer formed on surfaces (4, 51).
Earlier studies have shown that α-1,6-linked glucosyl residues in the glucan molecule confer a specific structure or conformation which S. mutans Gbps recognize as a binding site (31, 51, 52, 62). Among the Gbps, GbpC (and possibly GbpB) is cell wall bound and could function as a cell surface glucan receptor in S. mutans (4). Each of the Gbps appears to have a critical role in sucrose-dependent adhesion and biofilm formation by S. mutans, although loss of GbpC was the most disruptive (4, 36). GbpC may also be associated with S. mutans cell aggregation induced by dextrans (rich in α-1,6 linkages). In addition, cell-bound Gtfs have a strong affinity for α-1,6-linked glucan, which is dictated by the presence of a GBD (4, 61). The presence of an elevated proportion of α-1,6-linked glucose in the glucans produced by GtfB on the C. albicans cell surface could explain, in part, the large number of S. mutans cells bound to the polymer; treatment of surface-formed glucans with dextranase prior to incubation with S. mutans dramatically reduced bacterial binding to the treated yeast cell surface (M. Falsetta et al., unpublished data). The results presented here demonstrate that in situ-formed glucans can convert a less receptive cell surface into a highly adhesive site for S. mutans binding, making C. albicans an effective S. mutans carrier. Whether a similar biological phenomenon would occur with other morphological forms of C. albicans awaits further elucidation, as hyphae have been shown to support the direct attachment of oral streptococci, e.g., S. gordonii (3). Clearly, the presence of surface glucans dramatically influences the physical interactions between streptococci and yeast cells and may also affect interactions with sHA.
We have shown that C. albicans binds effectively to sHA but poorly to a glucan-coated sHA surface, as determined by standard adhesion assays using radiolabeled cells. Furthermore, the use of a novel micromechanical technique to measure the frequency of adhesion between C. albicans cells and a sHA (or gsHA) bead surface further enhanced our interpretation of the data obtained from the adhesion assays. The probability that a cell will adhere to a surface depends on the rate at which bonds between the molecules on the opposing surfaces can form, and the formation of adhesive bonds reflects contributions from multiple mechanisms operating on molecular and microscopic scales (35). The data indicate a high affinity of the yeast cell for saliva-coated surfaces. Considering that glucans mask host-derived bacterial binding sites in the pellicle (51), it appears that pellicle-binding sites are critical for the adhesion of yeast cells to sHA. These observations agree with previous studies which show that C. albicans adherence to hydroxyapatite is greatly stimulated when it is coated with either whole or parotid saliva compared to its adherence to hydrated uncoated HA beads (10, 11). There are indications that C. albicans adhesins may recognize basic proline-rich proteins in the pellicle (43). However, the identity of the cell wall protein and the type of adhesion receptor interactions remain to be elucidated. The GPI-CWP adhesins, such as Als and Eap1, found on the C. albicans cell surface have been shown to mediate adhesion to mucosal epithelial cells and to uncoated polystyrene (or acrylic) directly (11, 49, 57). However, little is known about their reactivity with saliva-coated surfaces (57). The N-terminal globular domains of these adhesins bind peptide or sugar ligands with high avidity and may recognize the various glycoproteins found in the human acquired pellicle (54).
The results of our experiments also demonstrated that the presence of glucans on the yeast cell surface enhanced the interaction of C. albicans cells to sHA. When in situ-formed glucans present on a single cell of C. albicans were placed in contact with the sHA surface (using a micropipette), the adhesive forces far exceeded the ability of the instrument to separate them, indicating strong binding between the surfaces. Interestingly, glucans formed by GtfB adsorbed to sHA did not promote the attachment of C. albicans. One possible explanation for this may be related to structural differences of the exopolymers assembled by GtfB bound to a solid/abiotic versus a cell wall surface (Table 1). As it binds to these two distinct surfaces, GtfB may undergo different conformational changes that can directly affect the process of glucan synthesis by the enzyme (and the glucosyl linkage pattern) (30, 59). The nature of the biophysical properties involved in the glucan-pellicle adhesive interactions is unknown and needs further investigation.
Furthermore, the adhesive interactions mediated by in situ glucans enhanced S. mutans carriage on the sHA surface. The data also show that the presence of C. albicans itself does not promote S. mutans accumulation on the sHA surface, likely due to limited binding between the bacterial and yeast cells, as observed here and by others (8, 18). Thus, the finding that glucan on the C. albicans surface could mediate the firm attachment of elevated numbers of S. mutans cells to sHA is novel. A similar intergeneric cooperative, glucan-dependent adhesion mechanism for S. mutans to bind to sHA has not, to our knowledge, been previously reported, in spite of numerous studies of influences of oral streptococci on adhesion and biofilm formation by C. albicans.
Previous studies reported coaggregation between C. albicans and S. mutans upon growth in sucrose medium, suggesting that glucan synthesis by the bacterium was essential for the cohesive interactions between cocci and yeast, resulting in the enhanced attachment and biofilm formation of C. albicans cells when adhering to acrylic and sHA surfaces (8, 47). However, it was unclear whether the bacterial-fungal coaggregation and further accumulation on surfaces were mediated by glucan molecules or simply by their being enmeshed with each other as a result of continuous EPS production over time. Our results show that the adhesive bacterium-yeast interaction may be more specific than just physical entrapment associated with de novo glucan synthesis. We propose that the glucans formed on the yeast cell surface by GtfB act as binding sites for S. mutans, forming a bacterial-fungal-EPS complex attached to the sHA surface. These results indicate physical interactions which are fundamentally different from those observed between C. albicans adhesins and streptococcal surface proteins and salivary protein in the pellicle. GtfB may represent an additional class of bacterium-derived products other than quorum-sensing molecules (3, 46) that could directly influence biofilm formation by both of these species (from two distinct kingdoms) by modulating: (i) the initial interaction between S. mutans and C. albicans, as well as between the yeast cell and sHA surface, and (ii) the establishment of the extracellular matrix (possibly in conjunction with an EPS, such as β-1,3-glucan, produced by C. albicans). In addition, it is equally possible that C. albicans could also adsorb GtfB from saliva, produce glucans, and then bind to S. mutans attached to sHA.
ECC, also known as baby bottle tooth decay, is a unique form of the disease dental caries characterized by excessive ingestion of sucrose, usually from a bottle or a similar container (during nighttime) and high levels of S. mutans infection (5, 60). The mechanical use of the bottle nipple restricts the access of saliva to many sites in the mouth (7) while continuously providing sucrose. Sucrose is the most cariogenic dietary constituent because this sugar serves as a substrate for both glucan synthesis and acid production. Therefore, there is an unusually high level of sugar and infectious challenges which initiate a cycle of glucan matrix and acid production and plaque accumulation. This process selects most aciduric and acidogenic flora in the absence of adequate salivary flow; C. albicans flourishes in such an environment. Furthermore, many ECC patients are malnourished and some are immunocompromised (60); these factors make them particularly prone to infection by Candida ssp. Several clinical studies have shown evidence of a direct association between the presence of C. albicans along with S. mutans and the development of ECC (12, 37, 39, 50). The exact reasons are unclear.
Our study shows that the cooperative and sucrose-dependent interactions mediated by a bacterial product attaching to the fungal surface may enhance S. mutans carriage on the tooth enamel surface and concomitantly promote glucan-rich matrix development in situ. Glucan-mediated fungal-bacterial interactions may help to explain why S. mutans cells are found in elevated numbers (while increasing the amount of EPS) in plaque from toddlers with ECC. This may represent a potentially novel cross-kingdom interaction that is involved in the development of virulent biofilms associated with ECC. Further investigations using mutant strains defective in yeast cell wall components and GtfB expression (in S. mutans) should elucidate the role of glucan-mediated adhesive interactions in virulent biofilm development using a rat model of dental caries.
Supplementary Material
ACKNOWLEDGMENTS
We are thankful to Linda Callahan (Confocal and Conventional Microscopy Core) for technical assistance during fluorescence and DIC imaging of the surface-adsorbed glucans and microbial cells. We also thank Constantine Haidaris (Department of Microbiology and Immunology, University of Rochester) for kindly providing C. albicans SC5314 and William H. Bowen and Megan Falsetta (Center for Oral Biology) for critical reading of the manuscript.
This work was supported in part by NIH grant T32 DE07202-20.
Footnotes
Supplemental material for this article may be found at http://aem.asm.org/.
Published ahead of print on 29 July 2011.
REFERENCES
- 1. Ajdić D., et al. 2002. Genome sequence of Streptococcus mutans UA159, a cariogenic dental pathogen. Proc. Natl. Acad. Sci. U. S. A. 99: 14434–14439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ambatipudi K. S., et al. 2010. Human common salivary protein 1 (CSP-1) promotes binding of Streptococcus mutans to experimental salivary pellicle and glucans formed on hydroxyapatite surface. J. Proteome Res. 9: 6605–6614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bamford C. V., et al. 2009. Streptococcus gordonii modulates Candida albicans biofilm formation through intergeneric communication. Infect. Immun. 77: 3696–3704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Banas J. A., Vickerman M. M. 2003. Glucan-binding proteins of the oral streptococci. Crit. Rev. Oral Biol. Med. 14: 89–99 [DOI] [PubMed] [Google Scholar]
- 5. Berkowitz R. J., et al. 2009. Adjunctive chemotherapeutic suppression of mutans streptococci in the setting of severe early childhood caries. J. Public Health Dent. 69: 163–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bowen W. H., Koo H. 2011. Biology of Streptococcus mutans-derived glucosyltransferases: role in extracellular matrix formation of cariogenic biofilms. Caries Res. 45: 69–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bowen W. H., Lawrence R. A. 2005. Comparison of the cariogenicity of cola, honey, cow milk, human milk, and sucrose. Pediatrics 116: 921–926 [DOI] [PubMed] [Google Scholar]
- 8. Branting C., Sund M. L., Linder L. E. 1989. The influence of Streptococcus mutans on adhesion of Candida albicans to acrylic surfaces in vitro. Arch. Oral Biol. 34: 347–353 [DOI] [PubMed] [Google Scholar]
- 9. Budtz-Jörgensen E., Theilade E., Theilade J. 1983. Quantitative relationship between yeast and bacteria in denture-induced stomatitis. Scand. J. Dent. Res. 91: 134–142 [DOI] [PubMed] [Google Scholar]
- 10. Cannon R. D., Nand A. K., Jenkinson H. F. 1995. Adherence of Candida albicans to human salivary components adsorbed to hydroxylapatite. Microbiology 141: 213–219 [DOI] [PubMed] [Google Scholar]
- 11. Cannon R. D., Chaffin W. L. 1999. Oral colonization by Candida albicans. Crit. Rev. Oral Biol. Med. 10: 359–383 [DOI] [PubMed] [Google Scholar]
- 12. de Carvalho F. G., Silva D. S., Hebling J., Spolidorio L. C., Spolidorio D. M. 2006. Presence of mutans streptococci and Candida spp. in dental plaque/dentine of carious teeth and early childhood caries. Arch. Oral Biol. 51: 1024–1028 [DOI] [PubMed] [Google Scholar]
- 13. Dye B. A., et al. 2007. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 11 248: 1–92 [PubMed] [Google Scholar]
- 14. Hamada S., Torii M. 1978. Effect of sucrose in culture media on the location of glucosyltransferase of Streptococcus mutans and cell adherence to glass surfaces. Infect. Immun. 20: 592–599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hayacibara M. F., et al. 2004. The influence of mutanase and dextranase on the production and structure of glucans synthesized by streptococcal glucosyltransferases. Carbohydr. Res. 339: 2127–2137 [DOI] [PubMed] [Google Scholar]
- 16. Reference deleted.
- 17. Jenkinson H. F., Douglas L. J. 2002. Interactions between Candida species and bacteria in mixed infections, p. 357–373 In Brogden K. A., Guthmiller J. M. (ed.), Polymicrobial diseases. ASM Press, Washington, DC: [PubMed] [Google Scholar]
- 18. Jenkinson H. F., Lala H. C., Shepherd M. G. 1990. Coaggregation of Streptococcus sanguis and other streptococci with Candida albicans. Infect. Immun. 58: 1429–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jin Y., Samaranayake L. P., Samaranayake Y., Yip H. K. 2004. Biofilm formation of Candida albicans is variably affected by saliva and dietary sugars. Arch. Oral Biol. 49: 789–798 [DOI] [PubMed] [Google Scholar]
- 20. Kanasi E., et al. 2010. Clonal analysis of the microbiota of severe early childhood caries. Caries Res. 44: 485–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kapteyn J. C., et al. 2000. The cell wall architecture of Candida albicans wild-type cells and cell wall-defective mutants. Mol. Microbiol. 35: 601–611 [DOI] [PubMed] [Google Scholar]
- 22. Kato C., Kuramitsu H. K. 1991. Molecular basis for the association of glucosyltransferases with the cell surface of oral streptococci. FEMS Microbiol. Lett. 63: 153–157 [DOI] [PubMed] [Google Scholar]
- 23. Klein M. I., et al. 2009. Structural and molecular basis of the role of starch and sucrose in Streptococcus mutans biofilms development. Appl. Environ. Microbiol. 75: 837–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Klinke T., Guggenheim B., Klimm W., Thurnheer T. 2011. Dental caries in rats associated with Candida albicans. Caries Res. 45: 100–106 [DOI] [PubMed] [Google Scholar]
- 25. Klinke T., et al. 2009. Acid production by oral strains of Candida albicans and lactobacilli. Caries Res. 43: 83–91 [DOI] [PubMed] [Google Scholar]
- 26. Klotz S. A., et al. 2007. Candida albicans Als proteins mediate aggregation with bacteria and yeasts. Med. Mycol. 45: 363–370 [DOI] [PubMed] [Google Scholar]
- 27. Koo H., Xiao J., Klein M. I., Jeon J. G. 2010. Exopolysaccharides produced by Streptococcus mutans glucosyltransferases modulate the establishment of microcolonies within multispecies biofilms. J. Bacteriol. 192: 3024–3032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Koo H., Nino de Guzman P., Schobel B. D., Vacca-Smith A. M., Bowen W. H. 2006. Influence of cranberry juice on glucan-mediated processes involved in Streptococcus mutans biofilm development. Caries Res. 40: 20–27 [DOI] [PubMed] [Google Scholar]
- 29. Koo H., et al. 2002. Effects of apigenin and tt-farnesol on glucosyltransferase activity, biofilm viability and caries development in rats. Oral Microbiol. Immunol. 17: 337–343 [DOI] [PubMed] [Google Scholar]
- 30. Kopec L. K., Vacca-Smith A. M., Bowen W. H. 1997. Structural aspects of glucans formed in solution and on the surface of hydroxyapatite. Glycobiology 7: 929–934 [DOI] [PubMed] [Google Scholar]
- 31. Landale E. C., McCabe M. M. 1987. Characterization by affinity electrophoresis of an alpha-1,6-glucan-binding protein from Streptococcus sobrinus. Infect. Immun. 55: 3011–3016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li F., Palecek S. P. 2008. Distinct domains of the Candida albicans adhesin Eap1p mediate cell-cell and cell-substrate interactions. Microbiology 154: 1193–1203 [DOI] [PubMed] [Google Scholar]
- 33. Loesche W. J. 1986. Role of Streptococcus mutans in human dental decay. Microbiol. Rev. 50: 353–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lomakina E. B., Waugh R. E. 2004. Micromechanical tests of adhesion dynamics between neutrophils and immobilized ICAM-1. Biophys. J. 86: 1223–1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lomakina E. B., Waugh R. E. 2009. Adhesion between human neutrophils and immobilized endothelial ligand vascular cell adhesion molecule 1: divalent ion effects. Biophys. J. 96: 276–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lynch D. J., Fountain T. L., Mazurkiewicz J. E., Banas J. A. 2007. Glucan-binding proteins are essential for shaping Streptococcus mutans biofilm architecture. FEMS Microbiol. Lett. 268: 158–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marchant S., Brailsford S. R., Twomey A. C., Roberts G. J., Beighton D. 2001. The predominant microflora of nursing caries lesions. Caries Res. 35: 397–406 [DOI] [PubMed] [Google Scholar]
- 38. Marsh P. D. 2003. Are dental diseases examples of ecological catastrophes? Microbiology 149: 279–294 [DOI] [PubMed] [Google Scholar]
- 39. Matee M. I., Mikx F. H., Maselle S. Y., Van Palenstein Helderman W. H. 1992. Mutans streptococci and lactobacilli in breast-fed children with rampant caries. Caries Res. 26: 183–187 [DOI] [PubMed] [Google Scholar]
- 40. McCabe R. M., Donkersloot J. A. 1977. Adherence of Veillonella species mediated by extracellular glucosyltransferase from Streptococcus salivarius. Infect. Immun. 18: 726–734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Morales D. K., Hogan D. A. 2010. Candida albicans interactions with bacteria in the context of human health and disease. PLoS Pathog. 6: e1000886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O'Sullivan J. M., Jenkinson H. F., Cannon R. D. 2000. Adhesion of Candida albicans to oral streptococci is promoted by selective adsorption of salivary proteins to the streptococcal cell surface. Microbiology 146: 41–48 [DOI] [PubMed] [Google Scholar]
- 43. O'Sullivan J. M., Cannon R. D., Sullivan P. A., Jenkinson H. F. 1997. Identification of salivary basic proline-rich proteins as receptors for Candida albicans adhesion. Microbiology 143: 341–348 [DOI] [PubMed] [Google Scholar]
- 44. Paes Leme A. F., Koo H., Bellato C. M., Bedi G., Cury J. A. 2006. The role of sucrose in cariogenic dental biofilm formation—new insight. J. Dent. Res. 85: 878–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Parisotto T. M., Steiner-Oliveira C., Silva C. M., Rodrigues L. K., Nobre-dos-Santos M. 2010. Early childhood caries and mutans streptococci: a systematic review. Oral Health Prev. Dent. 8: 59–70 [PubMed] [Google Scholar]
- 46. Peleg A. Y., Hogan D. A., Mylonakis E. 2010. Medically important bacterial-fungal interactions. Nat. Rev. Microbiol. 8: 340–349 [DOI] [PubMed] [Google Scholar]
- 47. Pereira-Cenci T., et al. 2008. The effect of Streptococcus mutans and Candida glabrata on Candida albicans biofilms formed on different surfaces. Arch. Oral Biol. 53: 755–764 [DOI] [PubMed] [Google Scholar]
- 48. Quivey R. G., Jr., Kuhnert W. L., Hahn K. 2000. Adaptation of oral streptococci to low pH. Adv. Microb. Physiol. 42: 239–274 [DOI] [PubMed] [Google Scholar]
- 49. Radford D. R., Challacombe S. J., Walter J. D. 1999. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit. Rev. Oral Biol. Med. 10: 99–116 [DOI] [PubMed] [Google Scholar]
- 50. Raja M., Hannan A., Ali K. 2010. Association of oral candidal carriage with dental caries in children. Caries Res. 44: 272–276 [DOI] [PubMed] [Google Scholar]
- 51. Schilling K. M., Bowen W. H. 1992. Glucans synthesized in situ in experimental salivary pellicle function as specific binding sites for Streptococcus mutans. Infect. Immun. 60: 284–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schilling K. M., Blitzer M. H., Bowen W. H. 1989. Adherence of Streptococcus mutans to glucans formed in situ in salivary pellicle. J. Dent. Res. 68 (Sp. Iss.): 1678–1680 [Google Scholar]
- 53. Silverman R. J., Nobbs A. H., Vickerman M. M., Barbour M. E., Jenkinson H. F. 2010. Interaction of Candida albicans cell wall Als3 protein with Streptococcus gordonii SspB adhesin promotes development of mixed-species communities. Infect. Immun. 78: 4644–4652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Siqueira W. L., Zhang W., Helmerhorst E. J., Gygi S. P., Oppenheim F. G. 2007. Identification of protein components in in vivo human acquired enamel pellicle using LC-ESI-MS/MS. J. Proteome Res. 6: 2152–2160 [DOI] [PubMed] [Google Scholar]
- 55. Somogy M. 1945. A new reagent for the determination of sugars. J. Biol. Chem. 160: 61–73 [Google Scholar]
- 56. Sudbery P., Gow N., Berman J. 2004. The distinct morphogenic states of Candida albicans. Trends Microbiol. 12: 317–324 [DOI] [PubMed] [Google Scholar]
- 57. ten Cate J. M., Klis F. M., Pereira-Cenci T., Crielaard W., de Groot P. W. 2009. Molecular and cellular mechanisms that lead to Candida biofilm formation. J. Dent. Res. 88: 105–115 [DOI] [PubMed] [Google Scholar]
- 58. Tokunaga M., Kusamichi M., Koike H. 1986. Ultrastructure of outermost layer of cell wall in Candida albicans observed by rapid-freezing technique. J. Electron Microsc. 35: 237–246 [PubMed] [Google Scholar]
- 59. Vacca-Smith A. M., Bowen W. H. 1998. Binding properties of streptococcal glucosyltransferases for hydroxyapatite, saliva-coated hydroxyapatite, and bacterial surfaces. Arch. Oral Biol. 43: 103–110 [DOI] [PubMed] [Google Scholar]
- 60. Vadiakas G. 2008. Case definition, aetiology and risk assessment of early childhood caries (ECC): a revisited review. Eur. Arch. Paediatr. Dent. 9: 114–125 [DOI] [PubMed] [Google Scholar]
- 61. van Hijum S. A., Kralj S., Ozimek L. K., Dijkhuizen L., van Geel-Schutten I. G. 2006. Structure-function relationships of glucansucrase and fructansucrase enzymes from lactic acid bacteria. Microbiol. Mol. Biol. Rev. 70: 157–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Venkitaraman A. R., Vacca-Smith A. M., Kopec L. K., Bowen W. H. 1995. Characterization of glucosyltransferaseB, GtfC, and GtfD in solution and on the surface of hydroxyapatite. J. Dent. Res. 74: 1695–1701 [DOI] [PubMed] [Google Scholar]
- 63. Wunder D., Bowen W. H. 1999. Action of agents on glucosyltransferases from Streptococcus mutans in solution and adsorbed to experimental pellicle. Arch. Oral Biol. 44: 203–214 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.