Abstract
The search for a safe and efficacious vaccine for Ebola virus continues, as no current vaccine candidate is nearing licensure. We have developed (i) replication-competent, (ii) replication-deficient, and (iii) chemically inactivated rabies virus (RABV) vaccines expressing Zaire Ebola virus (ZEBOV) glycoprotein (GP) by a reverse genetics system based on the SAD B19 RABV wildlife vaccine. ZEBOV GP is efficiently expressed by these vaccine candidates and is incorporated into virions. The vaccine candidates were avirulent after inoculation of adult mice, and viruses with a deletion in the RABV glycoprotein had greatly reduced neurovirulence after intracerebral inoculation in suckling mice. Immunization with live or inactivated RABV vaccines expressing ZEBOV GP induced humoral immunity against each virus and conferred protection from both lethal RABV and EBOV challenge in mice. The bivalent RABV/ZEBOV vaccines described here have several distinct advantages that may speed the development of inactivated vaccines for use in humans and potentially live or inactivated vaccines for use in nonhuman primates at risk of EBOV infection in endemic areas.
INTRODUCTION
The Ebolavirus genus of the family Filoviridae comprises four viral species; Zaire, Sudan, Cote d'Ivoire, and Reston Ebola virus (EBOV) (36). A potential fifth species, Bundibugyo, was recently associated with an outbreak of hemorrhagic fever in Uganda in 2007. Since the identification of Zaire EBOV (ZEBOV) in the 1970s, at least 20 human outbreaks have been reported in Central Africa (36). Fatal EBOV infection is characterized by flu-like symptoms and high fever followed by coagulopathy, hemorrhagic manifestations, shock, and multiorgan failure. While case fatality rates vary between outbreaks and among the EBOV species, ZEBOV has been associated with up to 90% lethality (25). In addition, outbreaks of lethal EBOV infection have been reported in nonhuman primates (NHPs), including gorillas and chimpanzees, in endemic areas (1, 24, 25, 47, 48). EBOV has also emerged as a significant biodefense concern because of its extreme virulence and capability to induce disease via aerosolization (15, 19).
Several strategies have been employed to identify vaccine candidates that confer protection from EBOV. Immunization with the EBOV glycoprotein (GP), which mediates viral attachment and entry, has been shown to confer protection from homologous EBOV species in NHPs. Specifically, delivery of GP by DNA vaccination, virus-like particles, or by expression from recombinant viruses, including adenovirus, vesicular stomatitis virus (VSV), or paramyxoviruses, has been shown to induce humoral and cellular immunity to EBOV, although the exact correlate(s) of protective immunity remains incompletely defined (3, 4, 8, 14, 18, 42–45, 51, 52). Because of unsuccessful cross-protection studies and the known high amino acid sequence divergence of GP across the EBOV species, it is believed that a multivalent vaccine will be required to provide protection from all EBOV species (14). Recently, cross-protection against Bundibugyo EBOV was demonstrated by DNA/adenovirus prime-boost vaccination with Sudan EBOV and ZEBOV, indicating the potential for heterologous protection (16, 18). Taken together, these prior vaccination strategies have firmly established that efficient immunization with EBOV GP confers protection from lethal EBOV challenge in rodents and NHPs. As the disease course of EBOV in humans resembles that observed in NHPs, it is anticipated that human vaccination will be an effective means of disease prevention. Despite the successful preclinical studies of the above vaccine candidates, obstacles remain which may hinder their licensure and utilization, including safety concerns, preexisting vector immunity, and manufacturing, dosage, or schedule issues. As such, the identification of additional vaccine candidates continues with a focus on killed vaccines that might have optimal safety profiles.
The objective of the present study was to identify novel vaccine candidates for EBOV with a maximum potential of licensure and utilization. To this end, we chose the rabies virus (RABV) vaccine platform, which would allow rapid development of replication-competent, replication-deficient, and chemically inactivated vaccine candidates, increasing the likelihood that an appropriate balance between vaccine immunogenicity and reactogenicity would be achieved. In addition, RABV causes an estimated 24,000 deaths per year in Africa, and this is believed to be an underestimate (6, 20, 37), so a bivalent RABV/EBOV vaccine would be an effective public health tool in Central Africa. RABV is a nonsegmented, negative-strand RNA virus of the Rhabdoviridae family. Although wild-type RABV almost always causes a fatal central nervous system (CNS) disease in mammalian species (37), in its attenuated form, the RABV vaccine has proven to be an excellent vaccine vector (5, 10–12, 27–29, 39, 41, 46). Highly attenuated, recombinant RABV vaccine vectors expressing HIV-1 and other viral antigens, such as severe acute respiratory syndrome coronavirus S and hepatitis C virus E1 and E2, have been shown to be safe and to induce both humoral and cellular immune response in small-animal models (26, 28–30, 39). In the case of HIV-1, these RABV vaccine candidates have been characterized by potent induction of humoral and cellular immunity in mice and NHPs and are avirulent after peripheral administration. The RABV vaccine vectors are generated from a reverse genetics system derived from the live-attenuated SAD B19 RABV vaccine, which is used for wildlife vaccination in Europe (49, 50). Further attenuated RABV vectored vaccines have been generated by the introduction of mutations in the RABV glycoprotein (G) as well as the deletion of the RABV G; these viruses are propagated on trans-complementing cell lines that express RABV G (17, 29, 31). These recombinant viruses have been demonstrated to be growth deficient or restricted in vitro and in vivo and are strongly immunogenic (17, 29, 31). Furthermore, beta-propiolactone-mediated inactivation of RABV vectored vaccines has been used to generate killed vaccine candidates that should have optimal safety profiles (39, 40).
Here, we describe the generation of live-attenuated and inactivated RABV vaccines expressing ZEBOV GP and demonstrate their molecular properties, virulence, immunogenicity, and protective efficacies against RABV and EBOV in mice. In addition to the advantages of the RABV vaccine platform described above, it is anticipated that the current advanced state of RABV vaccine safety, production, and distribution may accelerate the clinical development of the inactivated ZEBOV GP vaccines.
MATERIALS AND METHODS
Plasmid construction.
The full-length coding region of the ZEBOV GP was amplified with primers RP777 (GTGTGAATTCCGGAACGTACGCCGCCACCATGGGTGTTACAGGAATATTGCAGTTACCTCGT) and RP778 (GGAAGCTAGCTCACTAAAAGACAAATTTGCATATACAGAATAAAGC) and cloned into the BsiWI and NheI sites of a modified BNSP RABV vector that encodes glutamic acid at position 333 of the RABV glycoprotein (29). The resulting plasmid was designated cBNSP333-GP. A truncated version of GP that contains the ecto- and transmembrane domains but lacks the cytoplasmic tail was amplified with primers RP777 and RP781 (GGAAGCTAGCCTAGTTAACGCATATACAGAATAAAGCGATAACTGCAA), digested with BsiWI and HpaI, and ligated to the HpaI-NheI fragment of pSN-VSV-G (13), which contains the cytoplasmic tail of the RABV G. The fusion gene was then digested with BsiWI and NheI and cloned into cBNSP333 to generate cBNSP-GPGCD. The G-deleted constructs BNSPΔG-GP and BNSPΔG-GPGCD were generated by digestion of the G-containing parent plasmids BNSP-GP and BNSP-GPGCD with PacI and SmaI and religation of the blunted fragments.
Virus recovery from cDNA and propagation.
G-containing and G-deficient recombinant RABV were recovered and grown as described previously (17, 53).
Western blot assays.
BSR cells were infected at a multiplicity of infection (MOI) of 2 to 5 at 34°C. At 24, 48, and 72 h postinfection, the cells were washed once in phosphate-buffered saline (PBS) and resuspended in lysis buffer (50 mM Tris-HCl [pH 7.4], 150 mM NaCl, 1% NP-40, 0.1% sodium dodecyl sulfate [SDS], 1× protease inhibitor cocktail [Sigma]) on ice for 30 min. The suspension was transferred to a microcentrifuge tube and spun for 10 min at 16,000 × g to remove cell debris. Proteins were separated by SDS-9% polyacrylamide gel electrophoresis (PAGE) and transferred to a nitrocellulose membrane (Whatman, Minnetonka, MN). Blots were blocked for 1 h in 5% dry milk powder in Tris-buffered saline (TBS; pH 7.4). After being blocked, blots were washed twice using a 0.05% TBS-Tween 20 solution and incubated overnight at 4°C with polyclonal monkey anti-EBOV antibody or monoclonal antibody against RABV phosphoprotein. Blots were then washed four times with 0.1% TBS-Tween. Secondary goat anti-human or goat anti-mouse horseradish peroxidase (HRP)-conjugated antibodies (diluted 1:50,000; Jackson ImmunoResearch) were added, and blots were incubated for 1 h at room temperature (RT). Blots were washed four times with 0.1% TBS-Tween and once with PBS (pH 7.4). Chemiluminescence analysis using WestPico substrate (Pierce) was performed as instructed by the vendor.
Electron microscopy.
BSR cells were grown in Dulbecco's modified Eagle's medium (Gibco) supplemented with 5% fetal bovine serum (FBS; HyClone) and 1% penicillin-streptomycin for 24 h. Monolayers were washed one time with 1× PBS and then infected with virus at an MOI of 0.1 in Cellgro Complete serum-free medium (Mediatech). Flasks were incubated at 37°C-5% CO2 for 72 to 96 h. For double-immunogold labeling, infected cells were fixed in their respective flasks for 10 min in 0.1% paraformaldehyde (PFA) in Millonig's buffer. The cells were incubated with KZ52 human anti-Ebola GP antibody for 3 h at room temperature. After wash steps with Cellgro Complete medium (Mediatech Inc., Manassas, VA), the cells were incubated with goat anti-human-5-nm colloidal gold (Ted Pella, Redding, CA) conjugate for 2 h at room temperature. After wash steps, the cells were incubated with rabbit anti-rabies virus G antibody (Jackson ImmunoResearch, West Grove, PA) for 3 h at room temperature. After wash steps, the cells were incubated with goat anti-rabbit-15-nm colloidal gold conjugates for 2 h at room temperature. After wash steps, the cells were fixed using 2.5% glutaraldehyde, 2.0% paraformaldehyde in Millonig's sodium phosphate buffer (Tousimis Research, Rockville, MD). After scraping and pelleting, the samples were washed repeatedly in Millonig's buffer and incubated for 2 h in 1.0% osmium tetroxide in the same buffer. Following rinsing steps in ultrapure water and en bloc staining with 2.0% uranyl acetate, the samples were dehydrated in a series of graded ethanols and infiltrated and embedded in DER-736 plastic resin. Embedded blocks were sectioned using a Reichert-Jung Ultracut E ultramicrotome. Fifty- to 70-nm sections were collected on 200-mesh copper grids and poststained with Reynold's lead citrate. Electron microscopy specimens were examined in a FEI Tecnai Spirit Twin transmission electron microscope operating at 80 kV.
Virus spread assay.
Spread assays were conducted to analyze the capacity of the G-deleted RABV expressing GP to multiply on trans-complementing BSR-RVG, as well as on wild-type BSR cells. The complementing cell lines were induced by removal of doxycycline, followed by infection with the respective RABV at an MOI of 0.01. After 2 h, the virus was removed, cells were washed one time in PBS, and either doxycycline-containing or doxycycline-free medium was replenished. After incubation for 72 h at 34°C, cells were fixed with 80% acetone and viral antigen was detected with fluorescein isothiocyanate (FITC)-conjugated anti-RABV nucleoprotein (RABV-N) monoclonal antibody (Centocor) by using a fluorescence microscope.
Animal studies.
All animals were handled in strict accordance with good animal practices as defined by the relevant international guidelines (Association for Assessment and Accreditation of Laboratory Animal Care [AAALAC]; accreditation status Thomas Jefferson University [TJU; full], NIAID [full]) and national guidelines (TJU Animal Welfare Assurance number A3085-01; NIHAID A4149-01), and all animal work was approved by the Institutional Animal Care and Use Committee (IACUC) at TJU and the National Institute of Allergy and Infectious Diseases (NIAID). Animal use protocols were written and approved in accordance with Public Health Service Policy on Humane Care and Use of Laboratory Animals and the Guide for the Care and Use of Laboratory Animals (34). TJU IACUC protocol numbers 414I and 414J were utilized in this study. NIAID IACUC protocol number OSD-21E was utilized in this study.
Mouse pathogenicity experiments.
For peripheral inoculation, 6- to 8-week-old inbred BALB/c or outbred Swiss Webster mice were administered intraperitoneal (i.p.), intranasal (i.n.), or intramuscular (i.m.) injections of live virus or beta-propriolactone-inactivated virus at the concentrations indicated below in the figure legends. The i.m. injections were performed by administration of 50 μl into the hind leg muscle (gastrocnemius). Mice were monitored daily for clinical signs and signs of morbidity during the time periods indicated in the figure legends. Mice were individually or group weighed periodically as a measure of health status.
For analysis of viral neurovirulence, litters of 10 5-day-old Swiss Webster mouse pups were administered by the intracerebral (i.c.) route 10-μl injections containing serial dilutions of parental and RABV vaccines expressing GP. Mouse pups were monitored daily for clinical signs of encephalitis, and moribund mice were humanely euthanized. The number of surviving mice was recorded daily.
Mouse immunization and challenge.
For RABV challenge experiments, groups of 10 BALB/c mice were immunized i.m. with vehicle, 5 × 105 focus-forming units (FFU) of the indicated virus, or 10 μg of inactivated virus, on day 0 (1-dose group) or on days 0 and 14 (2-dose group). On day 30 postimmunization, all mice were bled and serum was isolated for analysis by enzyme-linked immunosorbent assay (ELISA) as described below. On day 50 postimmunization, 10 mice were challenged i.m. with the highly virulent RABV strain CVS-N2c and monitored for signs of encephalitis and morbidity for 21 days. Moribund mice were humanely euthanized. Mouse survival was recorded daily, and weights were measured periodically. Virulent RABV challenge was performed in a biosafety level 3 vivarium.
For challenge with mouse-adapted EBOV (MA-EBOV) (2), groups of 10 BALB/c mice were immunized i.m. with vehicle, 5 × 105 FFU of the indicated virus, or 10 μg of inactivated virus on day 0 (1 dose) or on days 0 and 14 (2 dose). On day 30 postimmunization, all mice were bled and serum was isolated for analysis by ELISA as described below. On day 77 postimmunization, mice were challenged i.p. with 1,000 PFU of MA-EBOV and monitored for signs of morbidity for 21 days. Moribund mice were humanely euthanized. Mouse survival was recorded daily, and weights were measured periodically. The MA-EBOV challenge experiment was approved by the University of Texas Medical Branch IACUC and performed in the Galveston National Laboratory biosafety level 4 laboratory at the University of Texas Medical Branch in Galveston, TX.
Antibody assays.
Mouse sera were tested in an indirect ELISA to evaluate humoral responses against EBOV-GP and RABV-G. GP antigen for coating ELISA plates was obtained by harvesting cell supernatant of mouse neuroblastoma cells transiently transfected with expression plasmids encoding amino acids 33 to 632 of the GP ectodomain or a truncated version of the ectodomain that lacks the mucin domain (amino acids 312 to 462). The plasmids (21, 22) were generously provided by E. Ollmann Saphire, Scripps Research Institute, La Jolla, CA. RABV glycoprotein was purified as described previously. Ninety-six-well Maxisorb plates (Nunc) were coated overnight with 200 μl of cell culture supernatant or 200 ng of purified RABV G per well, washed three times with PBST (PBS with 0.05% Tween 20), and then blocked for 2 to 3 h with PBST containing 5% nonfat dry milk. Plates were then incubated with the test sera diluted 1:200 in PBST at 4°C. The following day the plates were washed three times with PBST, and 200 μl goat anti-mouse IgG conjugated to HRP (1:10,000 dilution) was added per well. Two hours later the plates were washed with PBST and developed with SigmaFast o-phenylenediamine substrate. The enzymatic reaction was stopped with 3 M H2SO4, and absorption was read at 490 nm.
To determine virus-neutralizing antibody levels against RABV in sera from immunized mice, a modified rapid fluorescent focus inhibition test (RFFIT) was performed. Briefly, RABV strain CVS-11, at a concentration to achieve an MOI of 1 at 24 h postinfection in the negative control, was added to 3-fold serial dilutions of sera or WHO standard in Cellgro Complete serum-free medium (Mediatech) in 96-well plates, and the mixtures were incubated at 37°C for 1 h. Medium was removed from 96-well plates of mouse neuroblastoma cells grown in RPMI (Mediatech) supplemented with 10% FBS (Atlanta Biologicals) and 1% penicillin-streptomycin, and the mixtures were transferred to the cell plates. After 24 h of incubation at 37°C, cells were fixed with 80% acetone and stained with FITC-anti-RABV N (Fujirebio Diagnostics Inc.). The percent infected cells per well was determined, and international units of antibody were calculated based on the WHO standard, by which the dilution of the WHO standard that results in a 50% tissue culture inhibitory dose for the challenge virus is equivalent to 2 IU of neutralizing antibody.
RESULTS
Generation of RABV vaccines encoding ZEBOV GP.
The BNSP RABV vaccine vector (Fig. 1) was derived from the SAD B19 vaccine strain, which was attenuated by tissue culture passage and has been used as a live oral vaccine for wildlife in Europe (7, 49, 50). The construct was engineered to contain a novel RABV stop-start transcription signal sequence flanked by unique BsiWI and NheI restriction sites between the nucleoprotein (N) and phosphoprotein (P) genes for introduction of foreign genes (29). While BNSP is avirulent after peripheral administration in mice, it retains neurovirulence after i.c. inoculation. Therefore, a further-attenuated derivative, BNSP333, was generated that contained an Arg→Glu change at amino acid 333 of the RABV G (29). The 333 mutation has been shown to greatly attenuate neurovirulence of previous RABV vaccine vectors in adult mice, so BNSP333 was chosen as the parental virus for these studies.
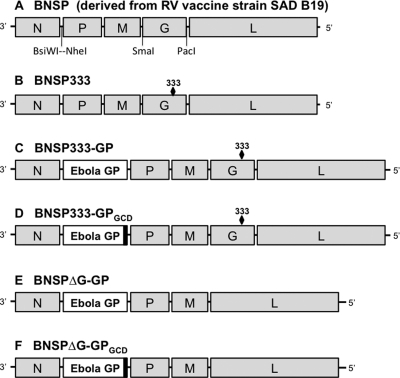
Fig. 1.
Virus constructs. Negative-sense RNA genomes are illustrated for the parental RABV vaccine constructs, BNSP (A) and BNSP333 (B) (28), and four RABV vaccine vectors expressing Zaire Ebola virus strain Mayinga GP with (C and D) or without RABV G (E and F). The 333 mutation results in an Arg→Glu change at amino acid 333 of RABV G, which has been shown to greatly attenuate neurovirulence of RABV vaccine vectors in adult mice (28, 29). ZEBOV GP is expressed authentically (C and E) or with the RABV GCD fused to its ectodomain and transmembrane domain (D and F). The GCD is depicted by a black box.
Two BNSP333 constructs encoding ZEBOV strain Mayinga GP were generated (Fig. 1). BNSP333-GP encodes unmodified ZEBOV GP, while BNSP333-GPGCD encodes the GP ectodomain and transmembrane domain fused to the RABV G cytoplasmic domain (GCD). The GCD construct was generated to maximize the likelihood that efficient incorporation of GP into virions would occur, which is critical for the potential development of inactivated vaccines. Finally, two additional constructs were generated by the deletion of the RABV G gene, BNSPΔG-GP and BNSPΔG-GPGCD. RABV G is responsible for viral attachment and entry and a critical mediator of neurovirulence (37). Therefore, deletion of G results in viruses that are severely growth restricted and require recovery and propagation in trans-complementing BSR cells expressing RABV G.
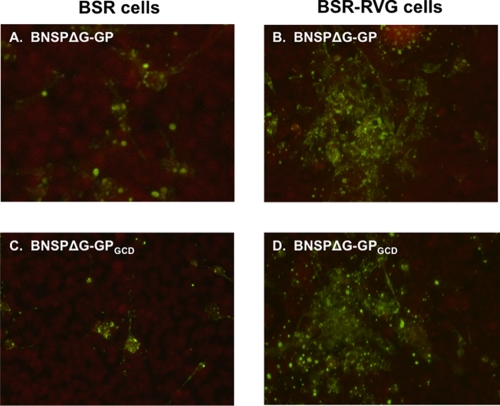
Infectious virus was readily recovered by transfection of each of the four plasmid constructs by utilizing standard methods as described previously (29, 38). Virus yields for BNSP333-GP and BNSP333-GPGCD exceeded 108 FFU/ml, while BNSPΔG-GP and BNSPΔG-GPGCD reached virus concentrations of 106 FFU/ml, which were concentrated to 107 FFU/ml. To evaluate the in vitro replication potential of the ΔG viruses, virus spread was assessed by monitoring growth in wild-type BSR cells and trans-complementing BSR cells expressing RABV G. Cells were infected at a multiplicity of infection of 0.01 with BNSPΔG-GP and BNSPΔG-GPGCD. After 2 days of incubation, cells were immunostained for expression of RABV N. As expected, the RABV G-expressing cells supported efficient virus spread, with numerous foci of infected cells apparent (Fig. 2B and D). In contrast, infection of unmodified BSR cells with BNSPΔG-GP or BNSPΔG-GPGCD resulted in a different pattern of replication (Fig. 2A and C). Specifically, single infected cells or an occasional neighboring cell were found to be infected, indicating that these viruses were growth restricted as intended. However, these results indicate some limited spread of the G-deleted virus, most likely mediated by ZEBOV GP.
Fig. 2.
Results of the virus spread assay indicate ΔG viruses are growth restricted. BSR cells (A and C) or trans-complemented BSR cells expressing RABV G (B and D) were infected at an MOI of 0.001 with BNSPΔG-GP (A and B) or BNSPΔG-GPGCD (C and D). Three days later, cells were fixed and immunostained for intracellular RABV nucleoprotein. Fluorescence microscope magnification, ×10.
Expression of ZEBOV GP by recombinant RABV vaccines.
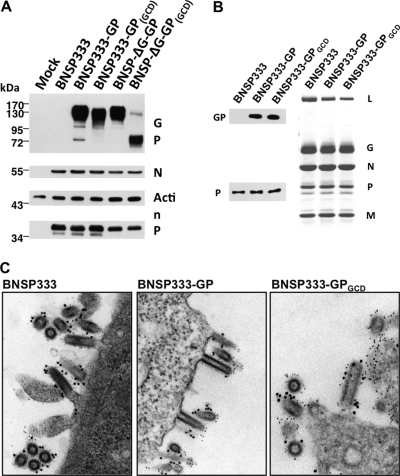
To analyze whether ZEBOV GP is efficiently expressed by RABV vectors, BSR cells were infected at an MOI of 2 to 5 with BNSP333-GP, BNSP333-GPGCD, the G-deleted viruses BNSPΔG-GP or BNSPΔG-GPGCD, or BNSP333 as a control. As shown in Fig. 3A, BNSP333-GP, BNSP333-GPGCD, and the G-deleted virus BNSPΔG-GP expressed a protein of the expected size of ZEBOV GP as early as 24 h after infection. Interestingly, for the G-containing viruses the signal for GP was most prominent after 24 h and had decreased at 72 h, potentially indicating its efficient removal with budding RABV from the infected cell. This phenomenon was not detected for the G-deleted virus BNSPΔG-GP, potentially because of slower growth and release of virus particles. In the case of BNSPΔG-GPGCD we detected only a very weak signal for full-length GP after 48 h, but another prominent GP-specific band of around 70 kDa was detected. Whereas the reason for the failure of expression of larger amounts of GP containing the RABV G CD is unknown for this particular virus, the low expression level of GP is reflected by a reduced immune response of this construct (see below and Fig. 5A and B), indicating that the amount of expressed full-length GP is critical for protection against ZEBOV challenge.
Fig. 3.
Expression of GP by RABV vaccine constructs in vitro. (A) Western blot analysis of GP expressed by the indicated viruses at 24 to 72 h. Infected cell lysates were separated by SDS-PAGE and transferred to nitrocellulose membranes. Blots were probed with polyclonal monkey anti-EBOV. (B) Coomassie blue-stained SDS-PAGE gel of purified virus particles with the indicated RABV proteins. The Western blots were probed with anti-EBOV sera or anti-RABV P sera. (C) BSR cells were infected with the indicated viruses and analyzed by dual-label immunogold electron microscopy. RABV G was detected by primary rabbit anti-RABV G followed by secondary anti-rabbit IgG labeled with 15-nm gold particles. ZEBOV GP was detected by primary human anti-GP antibody followed by secondary anti-human IgG labeled with 5-nm gold particles. Magnification, ×150,000 (BNSP333 and BNSP333-GP); ×210,000 (BNSP333-GPGCD).
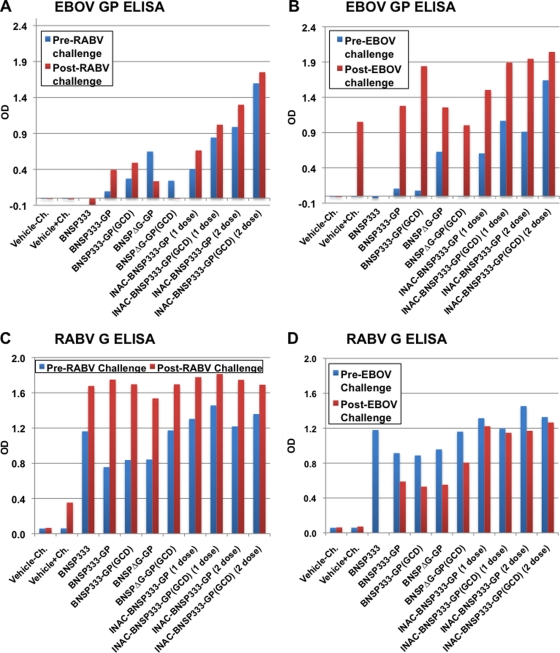
Fig. 5.
RABV vaccines expressing GP induce RABV G- and ZEBOV GP-specific antibodies. Groups of 10 BALB/c mice were immunized i.m. with 5 × 105 FFU of indicated live virus or 10 μg of inactivated virus on day 0 (1 dose) or on days 0 and 14 (2 dose) for two independent challenge experiments. Serum was drawn on day 30 postimmunization (blue bars) before RABV challenge (A and C) or MA-EBOV challenge (B and D), pooled, and analyzed by ELISA directed against ZEBOV GP at a 1:200 dilution (A and B) or RABV G at a 1:300 dilution (C and D). After RABV or MA-EBOV challenge, serum was collected, pooled, and tested in the same manner (red bars). Vehicle-Ch, mice immunized with vehicle but not challenged; Vehicle+Ch, mice immunized with vehicle and challenged with the indicated virus.
Incorporation of ZEBOV into budding RABV virions.
The utilization of killed (inactivated) virions for a dual RABV/EBOV vaccine requires the incorporation of RABV G as well as ZEBOV GP into budding virions. To analyze incorporation of the ZEBOV GP protein into RABV virions, BSR cells were infected with BNSP333, BNSP333-GP, or BNSP333-GPGCD, and virus was isolated from the supernatants of the infected cells by filtration and concentration followed by purification over 20% sucrose. Viral proteins were separated by SDS-PAGE and detected by Coomassie blue staining (Fig. 3B). The same pattern of the RABV proteins was detected for all three recombinant viruses, but no additional protein of the expected size for ZEBOV GP was detected in the viral particles. The lack of detection of GP may be due to lower incorporation levels or to GP running as a more diffuse band than the other RABV proteins due its heavy glycosylation. However, analysis of the recombinant virions by Western blotting with serum from a ZEBOV-infected rhesus monkey detected ZEBOV GP in both BNSP333-GP and BNSP333-GPGCD particles, whereas no signal was detected for the control RABV (BNSP333). No differences in the amount of incorporated GP were detected, indicating no advantage of the RABV CD for incorporation of ZEBOV GP.
The incorporation of GP into RABV virions was also assessed by electron microscopy (Fig. 3C). BSR cells were infected with BNSP333, BNSP333-GP, or BNSP333-GPGCD and analyzed by dual-label immunogold electron microscopy with anti-RABV G (15-nm gold particles) and anti-ZEBOV GP (5 nm). BNSP333 virions demonstrated characteristic bullet-shaped structures and were only labeled by anti-RABV G, as expected. Both BNSP333-GP and BNSP333-GPGCD virions were also found to form a similar bullet shape. Furthermore, each virus was found to react with anti-RABV G and anti-ZEBOV GP antibodies. These results further confirmed that the GP is incorporated into the RABV virion and that this event is not dependent on the presence of the GCD, suggesting that inactivated virions may serve as effective antigens for induction of immunity to GP.
Pathogenicity of RABV vaccines expressing ZEBOV GP in mice.
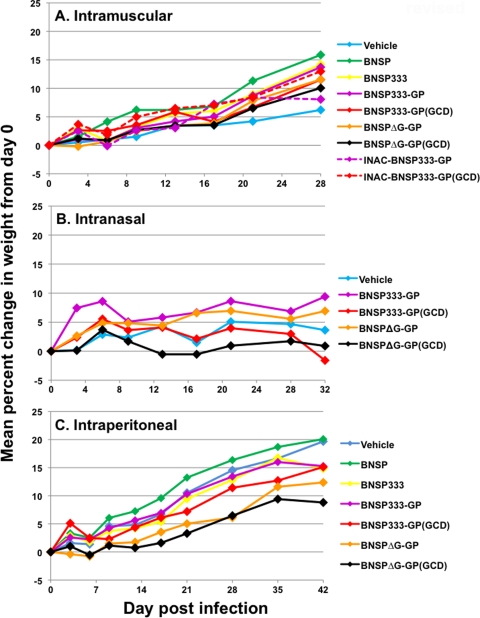
BNSP333, the parent of the viruses described here, is avirulent after peripheral and i.c. inoculation of adult mice (29). To determine if expression of ZEBOV GP resulted in altered virulence phenotypes in mice, we assessed pathogenicity after inoculation by multiple routes (Fig. 4). Groups of adult mice were injected with 1 × 105 to 1 × 106 FFU of the indicated viruses by the i.m., i.n., or i.p. route. Mice were monitored daily for 4 to 6 weeks for any clinical signs or indications of morbidity. In addition, mice were weighed periodically to assess general health status. No mouse inoculated with BNSP333-GP, BNSP333-GPGCD, BNSPΔG-GP, or BNSPΔG-GPGCD developed any clinical signs, indicating that expression of ZEBOV GP did not result in any unexpected viral virulence. Furthermore, analysis of the mean percent change in weight showed no differences between groups of mice inoculated with vehicle, BNSP, BNSP-333, or the GP-expressing viruses (Fig. 4).
Fig. 4.
RABV vaccine viruses expressing GP are avirulent in mice after peripheral inoculation. (A) Groups of five BALB/c mice were inoculated i.m. with 5 × 105 FFU live virus on day 0 or with 10 μg inactivated virus on days 0 and 14. Data are representative of two experiments. (B) Groups of 5 SW mice were inoculated with 1 × 105 FFU of the indicated viruses. Data are representative of two experiments. (C) Groups of eight BALB/c mice were inoculated i.p. with 1 × 106 FFU of the indicated viruses. Mice inoculated by each route were monitored daily for signs of morbidity and weighed periodically for the indicated time period.
Neurovirulence was also evaluated for the vaccine candidates by i.c. injection of highly susceptible suckling mice (Table 1). Five-day-old suckling mice were inoculated with serial dilutions of BNSP, BNSP-333, BNSP333-GP, or BNSP333-GPGCD and monitored for signs of encephalitis for 21 days. As expected, BNSP and BNSP-333 were lethal, as they retained neurovirulence, and BNSP333-GP and BNSP333-GPGCD shared a similar level of virulence. In contrast to these observations, i.c. inoculation with BNSPΔG-GP or BNSPΔG-GPGCD with the highest dose possible, 6 × 104 FFU, resulted in no clinical signs or lethality. These results indicate that the in vitro growth restriction observed for the ΔG viruses greatly attenuates neurovirulence, suggesting that they may have an increased safety profile versus the parental RABV vaccine, BNSP-333.
Table 1.
ΔG viruses have at least a 6,000-fold reduction in neurovirulence compared to parental RABV vaccine as measured by the LD50 in suckling mice
| Virus | Dose (FFU) | Survivala (%) | Mean (± SE) endpoint (days) |
|---|---|---|---|
| BNSP | 105 | 0 | 6.9 ± 0.3 |
| 103 | 0 | 7.9 ± 0.2 | |
| 101 | 10 | 10.2 ± 0.5 | |
| BNSP333 | 105 | 0 | 9.4 ± 0.2 |
| 103 | 0 | 9.5 ± 0.2 | |
| 101 | 20 | 10.5 ± 1.3 | |
| BNSP333-GP | 105 | 0 | 9.2 ± 0.2 |
| 103 | 0 | 9.6 ± 0.2 | |
| 101 | 10 | 11.4 ± 0.7 | |
| BNSP333-GPGCD | 105 | 0 | 9.5 ± 0.3 |
| 103 | 0 | 9.7 ± 0.2 | |
| 101 | 30 | 11.0 ± 1.8 | |
| BNSPΔG-GP | 6 × 104 | 100 | NA |
| BNSPΔG-GPGCD | 6 × 104 | 100 | NA |
Five-day-old Swiss Webster mice (n = 10) were inoculated i.c. with the indicated dose of virus and monitored for signs of encephalitis for 21 days. NA, not applicable.
RABV vaccines expressing ZEBOV GP induce humoral immunity to RABV and ZEBOV in mice.
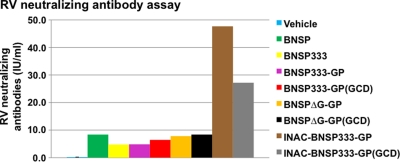
To analyze the immunogenicity of the GP-expressing vaccine candidates, groups of 10 mice were immunized i.m. with vehicle or 5 × 105 FFU of BNSP, BNSP333, BNSP333-GP, BNSP333-GPGCD, BNSPΔG-GP, or BNSPΔG-GPGCD. In addition, immunogenicities of inactivated virus preparations generated by the methods used to produce the current inactivated human RABV vaccine were examined. Specifically, virus inactivation was performed by treatment of virus stocks with a 1:2,000 dilution of beta-propiolactone overnight at 4°C followed by 30 min of incubation at 37°C. Groups of 10 mice were immunized with 10 μg of inactivated BNSP333-GP or BNSP333-GPGCD on day 0 (1 dose) or on days 0 and 14 (2 dose). On day 30 postimmunization, serum was isolated from immunized mice and humoral immunity was assessed by ELISAs for RABV G and ZEBOV GP. The results in Fig. 5A and C and B and D (independent experiments of 10 mice each that were later challenged with RABV or MA-EBOV, respectively) indicate that immunization with BNSP333-GP, BNSP333-GPGCD, or BNSPΔG-GP induced ZEBOV GP-specific antibodies in both experiments, but the strongest immune responses were detected in sera of mice immunized with the killed RABV particles containing GP. BNSPΔG-GPGCD induced a low GP-specific antibody response in one experiment (Fig. 5A) but not in the second experiment (Fig. 5B), indicating apparent weakened immunogenicity. RABV G-specific antibody responses were also detected (Fig. 5C and D). Interestingly, differences detected for the RABV G-specific humoral responses by ELISA were less pronounced but again slightly higher for killed vaccines (Fig. 5C). Sera from mice immunized with the above viruses contained RABV-neutralizing antibodies in the range of 5 to 45 IU, indicating that the GP-specific antibody response did not interfere with the development of immunity to RABV G (Fig. 6).
Fig. 6.
RABV vaccines expressing GP induce protective levels of RABV G-specific neutralizing antibodies. Groups of five BALB/c mice were immunized i.m. with 5 × 105 FFU of the indicated live virus on day 0 or with 10 μg of inactivated virus on days 0 and 14 (2 dose). Serum was drawn on day 28 and analyzed in a RABV neutralization assay; results are expressed as IU/ml. The 0.5-IU level is considered protective by WHO standards.
RABV vaccines expressing ZEBOV GP confer protection from RABV and ZEBOV challenge.
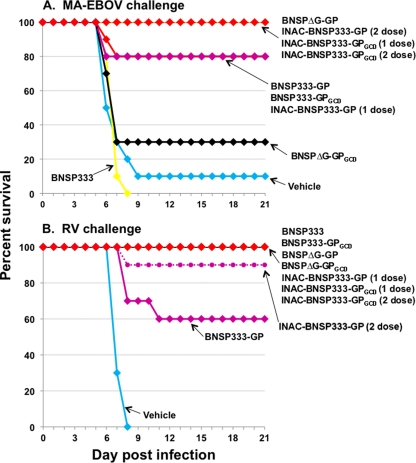
Based on the strong immunogenicity induced against RABV G and ZEBOV GP, we next examined the ability of immunization to confer protection against virulent RABV and MA-EBOV challenge (Fig. 7). The groups of mice for which results are shown in Fig. 5 were challenged i.p. with 1,000 PFU of MA-EBOV on day 77 postimmunization (Fig. 5B and D) or with the highly virulent RABV virus strain CVS-N2c on day 50 postimmunization (Fig. 5A and C). All mice were periodically weighed and monitored for clinical signs and indicators of morbidity for 21 days.
Fig. 7.
RABV vaccines expressing GP confer protection from EBOV and RABV. Two groups of 10 BALB/c mice were immunized i.m. with 5 × 105 FFU of the indicated live virus or 10 μg of inactivated virus on day 0 (1 dose) or on days 0 and 14 (2 dose). (A) On day 77 postimmunization, groups of 10 mice were challenged i.p. with 1,000 PFU of MA-EBOV. Mice were monitored for morbidity for 21 days. (B) On day 50 postimmunization, groups of 10 mice were challenged i.m. with virulent RABV virus strain CVS-N2c and monitored for morbidity for 21 days.
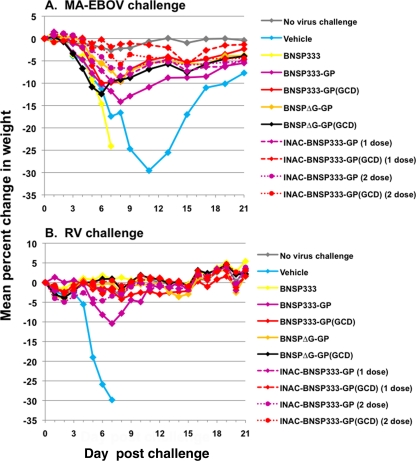
All BNSP333-immunized and 9 out of 10 vehicle-immunized mice succumbed to lethal MA-EBOV infection. Complete protection from MA-EBOV lethality was conferred by immunization with BNSPΔG-GP, INAC-BNSP333-GP (2 dose), INAC-BNSP333-GPGCD (1 dose), and INAC-BNSP333-GPGCD (2 dose). In addition, BNSP333-GP, BNSP333-GPGCD, and INAC-BNSP333-GP (1 dose) conferred 80% protection. BNSPΔG-GPGCD, which conferred the weakest level of protection, still induced 30% survival. As indicated above, this virus did express only very small amounts of GP (Fig. 3A) and had a lesser response by ZEBOV GP-specific ELISA (Fig. 5A and B). Therefore, the lower level of protection was not unexpected and correlates with the immunogenicity data. Analysis of weight loss after MA-EBOV challenge, which is an additional indicator of vaccine efficacy, suggested that the inactivated vaccines promoted stronger resistance to EBOV, as weight loss was minimal over the course of challenge, particularly for INAC-BNSP333-GPGCD (Fig. 8). We also analyzed the ZEBOV GP-specific antibody responses by ELISA after MA-EBOV challenge (Fig. 5B). As expected, the GP-specific antibodies increased after challenge in all surviving mice. Interestingly, the increases were most prominent in the live virus-vaccinated groups, which previously had the lowest responses, indicating that the high levels of GP-specific antibodies in mice immunized with the killed virions greatly restricted ZEBOV replication.
Fig. 8.
Weight loss after challenge with EBOV or RABV. Two groups of 10 BALB/c mice were immunized i.m. with 5 × 105 FFU of the indicated live virus or 10 μg of inactivated virus on day 0 (1 dose) or on days 0 and 14 (2 dose). (A) On day 77 postimmunization, groups of 10 mice were challenged i.p. with 1,000 PFU of MA-EBOV. Mice were weighed daily for 9 days and every other day until day 21. (B) On day 50 postimmunization, groups of 10 mice were challenged i.m. with virulent RABV virus strain CVS-N2C and weighed daily for 21 days.
The results of the virulent RABV challenge were equally promising. Seven of nine vaccine preparations conferred 100% protection (Fig. 7B), and INAC-BNSP333-GP (2 dose) conferred 90% protection. BNSP333-GP conferred 60% protection. It should be noted that challenge with 5 ×106 FFU RABV CVS-N2c is a very stringent model. Analysis of RABV G-specific antibodies after RABV challenge indicated a limited rise in levels. Taken together, these studies demonstrate live and inactivated vaccine candidates confer complete or substantial protection against lethal MA-EBOV and RABV challenge, and the mechanism of protection appears to be largely dependent on antibodies directed against EBOV GP and RABV G, respectively.
DISCUSSION
We generated various live and killed RABV vaccines expressing ZEBOV GP and compared their GP expression, safety, immunogenicity, and protective efficacy in mice. Our results indicate that ZEBOV GP is efficiently expressed by RABV vectors in the presence or absence of RABV G. In addition, GP is incorporated into RABV virions, and this incorporation is not dependent, or apparently enhanced, by the addition to GP of the RABV GCD. These results are somewhat surprising, because foreign proteins have been proposed to require addition of the GCD for RABV incorporation (32, 33). However, Siler et al. showed that the CD of CD4 promoted efficient incorporation of hepatitis C virus E2 into RABV virions (39). The successful incorporation of GP into RABV particles permits the use of inactivated virions as a means to vaccinate against ZEBOV. It also suggests that BNSPΔG-GP viruses would have the capability for limited virus spread mediated by GP in the absence of RABV G, which was confirmed by our in vitro findings, although the ΔG viruses were completely avirulent after i.c. challenge of mice.
To initially determine the immunogenicity of our RABV/EBOV vaccine candidates, we examined humoral immunity against GP. Somewhat surprisingly, we found that the inactivated vaccine preparations consistently induced higher levels of GP-specific antibodies as measured by ELISA compared to the live virus vaccines. BNSP333-GP, BNSP333-GPGCD, and BNSPΔG-GP induced low but detectable antibody responses in two experiments, while BNSPΔG-GPGCD induced detectable antibody levels in one of two experiments. In contrast, INAC-BNSP333-GP and INAC-BNSP333-GPGCD induced high levels of antibodies by a single vaccination that could be effectively boosted with a second vaccination. The presence of GCD appeared to confer a slight enhancement in induction of antibody levels in the killed vaccine preparations. Importantly, the prechallenge antibody levels in mice immunized with inactivated vaccines were similar to the level observed after challenge for the single vehicle-immunized mouse that survived MA-EBOV challenge. It is unclear why the inactivated vaccines induce higher levels of antibodies to GP than live virus, but this is advantageous, since inactivated vaccines are preferred for use in humans based on enhanced safety. One explanation could be that the antigen load is higher in the killed vaccines and that the live vaccines are so attenuated upon peripheral administration that their replication results in little additional antigen load. Alternatively, RABV G may be expressed earlier in the G-containing viruses and interfere with the antibody response to GP. The latter explanation is supported by the fact that such great differences as seen for the anti-GP humoral responses were not detected for the RABV G-specific immune response (Fig. 5C and D). Further examination of the immune response to these killed and live vaccine candidates is warranted.
Although humoral immunity when measured in a GP-specific ELISA appeared to be low for the live vaccine candidates, each conferred protection from MA-EBOV that appeared to correlate with antibody levels. BNSP333-GP, BNSP333-GPGCD, and BNSPΔG-GP induced 80 to 100% protection, while BNSPΔG-GPGCD, which did not induce detectable antibody levels prior to MA-EBOV challenge, conferred 30% protection, suggesting that an additional mediator(s) of protection may exist. It should be noted that these were single immunizations followed by MA-EBOV challenge on day 77, so the protection model was stringent and likely involved GP-specific antibodies and a T-cell-dependent memory immune response, as reflected in the increase of GP antibodies after challenge (Fig. 5B). Inactivated vaccines also conferred complete or 80% protection from MA-EBOV. Two indications suggest that the inactivated vaccines conferred an enhanced level of protection from MA-EBOV. First, mice immunized with inactivated vaccine had a lower relative rise in GP-specific antibodies after MA-EBOV challenge than mice immunized with live vaccines. Second, vaccination with inactivated vaccines, particularly BNSP333-GPGCD, appeared to confer less weight loss after MA-EBOV challenge, which is believed to be a sign of decreased disease severity, suggesting stronger protective immunity. Nearly all vaccines also induced complete protection from virulent RABV challenge, and the ELISA results correlated with the observed level of protection. Interestingly, both BNSPΔG-GP and BNSPΔG-GPGCD induced strong levels of G-specific antibodies and protection from RABV challenge, which is presumably mediated by the G present in the virions supplied by the trans-complementing cell line.
As with all vaccines and particularly live viral vaccines, the demonstration of safety and attenuation is paramount. Our results indicate that peripheral administration of BNSP333-GP, BNSP333-GPGCD, BNSPΔG-GP, and BNSPΔG-GPGCD to over 190 mice resulted in no morbidity or apparent clinical signs, demonstrating that these viruses retain an attenuation phenotype. It is important to note that while the ZEBOV Mayinga strain, the source of GP for our RABV/EBOV viruses, is avirulent in mice and required passage and genetic adaptation to produce MA-EBOV, the mutations responsible for virulence in mice were localized to EBOV viral protein 24 and nucleoprotein (9). Therefore, the GP sequence used in the vaccines studied here does have the capability to mediate disease in mice, indicating that mice are an appropriate species to evaluate pathogenicity of the RABV/EBOV vaccine candidates. Similar to the BNSP333 parent virus, BNSP333-GP and BNSP333-GPGCD retained neurovirulence in suckling mice after i.c. inoculation, although there was no sign of increased neurovirulence mediated by the expression of ZEBOV GP. This level of neurovirulence may preclude the use of these live vaccines in humans, based on experience with prior live virus vaccines for neurovirulent viruses. In contrast, BNSPΔG-GP and BNSPΔG-GPGCD were avirulent after i.c. inoculation and at least 6,000-fold reduced for neurovirulence from BNSP333 as measured by the 50% lethal dose (LD50). As such, BNSPΔG-GP, which conferred 100% protection from RABV and EBOV challenge, may warrant consideration for use in humans after further study of its attenuation and immunogenicity.
While the live vaccines described here have potential for use in humans, the most expeditious route to licensure and utilization of a RABV/EBOV vaccine would clearly be to pursue inactivated vaccine candidates. RABV inactivated by beta-propiolactone has been used to vaccinate humans since 1978 and has an excellent safety record (35). The RABV/EBOV viruses described here were inactivated by the same method as the current human vaccine and were found to be strongly immunogenic and protective after immunization with a single dose of 10 μg. The current human vaccine is administered without adjuvant in a compressed three-dose regimen (days 0, 7, and 21 to 28). Two inactivated RABV vaccines are currently used in the United States; they are manufactured by Novartis Vaccines and Diagnostics (Marburg, Germany) and Sanofi Pasteur (Lyon, France). Several additional manufacturers serve other markets. Based on the efficient replication of BNSP333-GP and BNSP333-GPGCD in tissue culture and the existing manufacturing process and capability of RABV vaccines, production of inactivated RABV/EBOV would appear to be feasible and potentially more simplified than some existing EBOV vaccine candidates (14). Furthermore, our combination of a desired biodefense vaccine (EBOV) with limited financial incentive for development because of limited market potential and an approved and financially viable vaccine such as RABV vaccine is a unique and potentially important factor in the commercialization of this EBOV vaccine. It is important to note that an inactivated RABV/EBOV vaccine would offer a distinct advantage for use in Africa over existing EBOV vaccine candidates, because it would afford protection from two diseases. The World Health Organization reports an estimated 24,000 deaths per year in Africa from RABV, and this number is believed to be a considerable underestimate (6, 20, 37). Therefore, use of our bivalent vaccines would offer an increased return on investment in public health.
A second intriguing application of these RABV-vectored EBOV vaccines would be their development for use in threatened NHP populations, which are highly susceptible to lethal EBOV outbreaks. Field research over the past decade has indicated that lethal EBOV outbreaks have affected chimpanzee and particularly Western gorilla populations in Gabon and the Democratic Republic of Congo (1, 23, 24, 47, 48). In fact, it has been suggested that EBOV is contributing to the endangered status of the Western gorilla and that vaccination is needed to protect NHP populations in endemic areas (47). With the successful history of vaccination of wildlife against RABV by using dispersed baits containing the SAD B19 vaccine strain (parent virus of the RABV/EBOV vaccines described here), one could consider using the live-attenuated RABV/EBOV vaccines in a similar manner for protection of NHPs in Africa from EBOV. Of note, SAD B19 was safe after a single oral application of 1.5 × 108 FFU in 10 chimpanzees of ages 3.5 to 8 years (54). The growth restriction, decreased neurovirulence, and protective efficacy of BNSPΔG-GP suggest that it may be a lead candidate for wildlife vaccination and offer an increased level of safety above the SAD B19 vaccine. The safety, stability, and efficacy of a RABV/EBOV vaccine would require exhaustive study of the target NHP species and in other animals that might encounter the vaccine baits. However, the introduction of SAD B19 RABV vaccine into Europe and safe dispersal of over 70 million vaccine baits since the 1980s provide a framework for this endeavor. Inactivated RABV/EBOV vaccines could also be considered for use in endemic NHPs, and again, would have fewer safety concerns, but achieving broad coverage to widely dispersed animals would be challenging. Nevertheless, if conservation authorities determine that vaccination of NHPs against EBOV is a necessary action and appropriate resources were provided, obstacles to the use of live or killed vaccines could be overcome. In addition to the protection of threatened NHPs, vaccination of NHP populations in endemic areas might also offer an additional, critical benefit to humans. The interaction of humans and infected NHPs has been associated with transmission of EBOV to humans and initiation of subsequent outbreaks, so prevention of disease in NHPs may also serve to limit EBOV transmission into the human population.
The studies described here demonstrate the utility and potential of the RABV vaccine vector platform for development of live and killed vaccines against ZEBOV and potentially other hemorrhagic fever viruses or biodefense agents. Presently, the immunogenicity and protective efficacy of the RABV/EBOV vaccines require examination in NHPs to determine if these candidate vaccines, particularly the inactivated vaccines, merit evaluation in humans. Further investigation in mice or NHPs is warranted as to the role of humoral and cellular immunity in protection by the various vaccine candidates, in order to understand differences in the induction of immunity by replication-competent, replication-deficient, and inactivated vaccines and correlates of immunity to EBOV. Finally, RABV vaccine candidates encoding GP from additional EBOV species and potentially additional hemorrhagic fever viruses will be generated to produce a multivalent, cross-protective vaccine.
ACKNOWLEDGMENTS
These studies were supported, in part, by the NIAID Division of Intramural Research and internal funds of the Jefferson Vaccine Center, TJU, to M.J.S.
We thank Russ Byrum and Kurt Cooper for technical assistance. The EBOV GP expression plasmids utilized for the GP ELISA were generously provided by E. Ollmann Saphire, Scripps Research Institute, La Jolla, CA.
Footnotes
Published ahead of print on 17 August 2011.
REFERENCES
- 1. Bermejo M., et al. 2006. Ebola outbreak killed 5000 gorillas. Science 314: 1564. [DOI] [PubMed] [Google Scholar]
- 2. Bray M., Davis K., Geisbert T., Schmaljohn C., Huggins J. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178: 651–661 [DOI] [PubMed] [Google Scholar]
- 3. Bukreyev A., et al. 2009. Chimeric human parainfluenza virus bearing the Ebola virus glycoprotein as the sole surface protein is immunogenic and highly protective against Ebola virus challenge. Virology 383: 348–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bukreyev A. A., Dinapoli J. M., Yang L., Murphy B. R., Collins P. L. 2010. Mucosal parainfluenza virus-vectored vaccine against Ebola virus replicates in the respiratory tract of vector-immune monkeys and is immunogenic. Virology 399: 290–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cenna J., et al. 2008. Immune modulating effect by a phosphoprotein-deleted rabies virus vaccine vector expressing two copies of the rabies virus glycoprotein gene. Vaccine 26: 6405–6414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cleaveland S., Fevre E. M., Kaare M., Coleman P. G. 2002. Estimating human rabies mortality in the United Republic of Tanzania from dog bite injuries. Bull. World Health Organ. 80: 304–310 [PMC free article] [PubMed] [Google Scholar]
- 7. Conzelmann K. K., Cox J. H., Schneider L. G., Thiel H. J. 1990. Molecular cloning and complete nucleotide sequence of the attenuated rabies virus SAD B19. Virology 175: 485–499 [DOI] [PubMed] [Google Scholar]
- 8. DiNapoli J. M., et al. 2010. Respiratory tract immunization of non-human primates with a Newcastle disease virus-vectored vaccine candidate against Ebola virus elicits a neutralizing antibody response. Vaccine 29: 17–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ebihara H., et al. 2006. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2: e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Faber M., et al. 2005. A single immunization with a rhabdovirus-based vector expressing severe acute respiratory syndrome coronavirus (SARS-CoV) S protein results in the production of high levels of SARS-CoV-neutralizing antibodies. J. Gen. Virol. 86: 1435–1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Faul E. J., et al. 2009. Rabies virus-based vaccines induce high levels of neutralizing antibody and poly-functional CD8+ T cells, and protect rhesus macaques from AIDS-like disease after SIVmac251 challenge. Vaccine 28: 299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Faul E. J., Wanjalla C. N., McGettigan J. P., Schnell M. J. 2008. Interferon-beta expressed by a rabies virus-based HIV-1 vaccine vector serves as a molecular adjuvant and decreases pathogenicity. Virology 382: 226–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Foley H. D., McGettigan J. P., Siler C. A., Dietzschold B., Schnell M. J. 2000. A recombinant rabies virus expressing vesicular stomatitis virus glycoprotein fails to protect against rabies virus infection. Proc. Natl. Acad. Sci. U. S. A. 97: 14680–14685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Geisbert T. W., Bausch D. G., Feldmann H. 2010. Prospects for immunisation against Marburg and Ebola viruses. Rev. Med. Virol. 20: 344–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Geisbert T. W., et al. 2008. Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine 26: 6894–6900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Geisbert T. W., et al. 2009. Single-injection vaccine protects nonhuman primates against Marburg virus and three species of Ebola virus. J. Virol. 83: 7296–7304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gomme E. A., Faul E. J., Flomenberg P., McGettigan J. P., Schnell M. J. 2010. Characterization of a single-cycle rabies virus-based vaccine vector. J. Virol. 84: 2820–2831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hensley L. E., et al. 2010. Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebola virus species. PLoS Pathog. 6: e1000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johnson E., Jaax N., White J., Jahrling P. 1995. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int. J. Exp. Pathol. 76: 227–236 [PMC free article] [PubMed] [Google Scholar]
- 20. Knobel D. L., du Toit J. T., Bingham J. 2002. Development of a bait and baiting system for delivery of oral rabies vaccine to free-ranging African wild dogs (Lycaon pictus). J. Wildl. Dis. 38: 352–362 [DOI] [PubMed] [Google Scholar]
- 21. Lee J. E., et al. 2008. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 454: 177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee J. E., et al. 2008. Complex of a protective antibody with its Ebola virus GP peptide epitope: unusual features of a V lambda X light chain. J. Mol. Biol. 375: 202–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Le Gouar P. J., et al. 2009. How Ebola impacts genetics of Western lowland gorilla populations. PLoS One 4: e8375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leroy E. M., et al. 2004. Multiple Ebola virus transmission events and rapid decline of central African wildlife. Science 303: 387–390 [DOI] [PubMed] [Google Scholar]
- 25. Mahanty S., Bray M. 2004. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect. Dis. 4: 487–498 [DOI] [PubMed] [Google Scholar]
- 26. McGettigan J. P., et al. 2001. Rabies virus-based vectors expressing human immunodeficiency virus type 1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J. Virol. 75: 4430–4434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McGettigan J. P., et al. 2006. Enhanced humoral HIV-1-specific immune responses generated from recombinant rhabdoviral-based vaccine vectors co-expressing HIV-1 proteins and IL-2. Virology 344: 363–377 [DOI] [PubMed] [Google Scholar]
- 28. McGettigan J. P., et al. 2003. Functional human immunodeficiency virus type 1 (HIV-1) Gag-Pol or HIV-1 Gag-Pol and Env expressed from a single rhabdovirus-based vaccine vector genome. J. Virol. 77: 10889–10899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McGettigan J. P., et al. 2003. Second-generation rabies virus-based vaccine vectors expressing human immunodeficiency virus type 1 gag have greatly reduced pathogenicity but are highly immunogenic. J. Virol. 77: 237–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McGettigan J. P., Sarma S., Orenstein J. M., Pomerantz R. J., Schnell M. J. 2001. Expression and immunogenicity of human immunodeficiency virus type 1 Gag expressed by a replication-competent rhabdovirus-based vaccine vector. J. Virol. 75: 8724–8732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McKenna P. M., et al. 2004. Immunogenicity study of glycoprotein-deficient rabies virus expressing simian/human immunodeficiency virus SHIV89.6P envelope in a rhesus macaque. J. Virol. 78: 13455–13459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mebatsion T., Conzelmann K. K. 1996. Specific infection of CD4+ target cells by recombinant rabies virus pseudotypes carrying the HIV-1 envelope spike protein. Proc. Natl. Acad. Sci. U. S. A. 93: 11366–11370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mebatsion T., Finke S., Weiland F., Conzelmann K. K. 1997. A CXCR4/CD4 pseudotype rhabdovirus that selectively infects HIV-1 envelope protein-expressing cells. Cell 90: 841–847 [DOI] [PubMed] [Google Scholar]
- 34. National Research Council 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC [Google Scholar]
- 35. Plotkin S. A. 1980. Rabies vaccine prepared in human cell cultures: progress and perspectives. Rev. Infect. Dis. 2: 433–448 [DOI] [PubMed] [Google Scholar]
- 36. Sanchez A., Geisbert T. W., Feldmann H. 2007. Filoviridae: Marburg and Ebola viruses, p. 1409–1448 In Knipe D. M., Howley P. M., Griffin D. E. (ed.), Fields virology, 5th ed., vol. 1 Lippincott Williams & Wilkins, Philadelphia, PA [Google Scholar]
- 37. Schnell M. J., McGettigan J. P., Wirblich C., Papaneri A. 2010. The cell biology of rabies virus: using stealth to reach the brain. Nat. Rev. Microbiol. 8: 51–61 [DOI] [PubMed] [Google Scholar]
- 38. Schnell M. J., Mebatsion T., Conzelmann K. K. 1994. Infectious rabies viruses from cloned cDNA. EMBO J. 13: 4195–4203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Siler C. A., et al. 2002. Live and killed rhabdovirus-based vectors as potential hepatitis C vaccines. Virology 292: 24–34 [DOI] [PubMed] [Google Scholar]
- 40. Smith M. E., et al. 2006. Rabies virus glycoprotein as a carrier for anthrax protective antigen. Virology 353: 344–356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Snook A. E., et al. 2008. Guanylyl cyclase C-induced immunotherapeutic responses opposing tumor metastases without autoimmunity. J. Natl. Cancer Inst. 100: 950–961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sullivan N. J., et al. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424: 681–684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sullivan N. J., Martin J. E., Graham B. S., Nabel G. J. 2009. Correlates of protective immunity for Ebola vaccines: implications for regulatory approval by the animal rule. Nat. Rev. Microbiol. 7: 393–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sullivan N. J., Sanchez A., Rollin P. E., Yang Z. Y., Nabel G. J. 2000. Development of a preventive vaccine for Ebola virus infection in primates. Nature 408: 605–609 [DOI] [PubMed] [Google Scholar]
- 45. Sun Y., et al. 2009. Protection against lethal challenge by Ebola virus-like particles produced in insect cells. Virology 383: 12–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tan G. S., et al. 2005. Strong cellular and humoral anti-HIV Env immune responses induced by a heterologous rhabdoviral prime-boost approach. Virology 331: 82–93 [DOI] [PubMed] [Google Scholar]
- 47. Vogel G. 2007. Conservation. Scientists say Ebola has pushed Western gorillas to the brink. Science 317: 1484. [DOI] [PubMed] [Google Scholar]
- 48. Vogel G. 2006. Ecology. Tracking Ebola's deadly march among wild apes. Science 314: 1522–1523 [DOI] [PubMed] [Google Scholar]
- 49. Vos A., et al. 1999. An update on safety studies of SAD B19 rabies virus vaccine in target and non-target species. Epidemiol. Infect. 123: 165–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vos A., Pommerening E., Neubert L., Kachel S., Neubert A. 2002. Safety studies of the oral rabies vaccine SAD B19 in striped skunk (Mephitis mephitis). J. Wildl. Dis. 38: 428–431 [DOI] [PubMed] [Google Scholar]
- 51. Warfield K. L., et al. 2003. Ebola virus-like particles protect from lethal Ebola virus infection. Proc. Natl. Acad. Sci. U. S. A. 100: 15889–15894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Warfield K. L., et al. 2007. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J. Infect. Dis. 196(Suppl. 2): S430–S437 [DOI] [PubMed] [Google Scholar]
- 53. Wirblich C., Schnell M. J. 2011. Rabies virus (RV) glycoprotein expression levels are not critical for pathogenicity of RV. J. Virol. 85: 697–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. World Health Organization 1993. Report of the Fourth WHO Consultation on Oral Immunization of Dogs against Rabies. WHO/Rab.Res./93.42 WHO, Geneva, Switzerland [Google Scholar]