Abstract
Objective
To evaluate the feasibility and accuracy of existing point-of-care (POC) HIV tests performed by an untrained patient compared to the routinely used HIV POC test offered to patients in two urban emergency departments (ED).
Methods
From April 2008 through December 2009, patients, who had completed a standard HIV oral fluid test performed by a trained healthcare professional and who were unaware of their results, were recruited to perform a rapid POC HIV test. Patients were given a choice of the oral fluid or the finger-stick blood POC. Evaluation of acceptability to perform the mechanics of the test was accessed by questionnaire. For the “self-test,” the participant obtained his/her own sample and performed the test. The patient’s results were compared to standard oral fluid results obtained by the health care professional.
Results
Overall, 478 of 564 (85%) patients receiving a standard oral fluid HIV test volunteered, with a mean age of 38–39 years. Ninety-one percent of participants chose oral fluid and 9% chose blood (p<0.05). Self-test results were 99.6% concordant with health care professionals’ test results. For the self-testers, 94% of oral fluid testers and 84.4% of blood testers reported trusting the self-administered test result “very much.” Furthermore, 95.6% of oral fluid group and 93.3% of the blood group would “probably” or “definitely” perform a test at home, if available.
Conclusions
This study demonstrated that a significant proportion of patients offered a self-HIV POC volunteered and preferred using oral fluid. Patients’ results agreed with standard HIV POC results. The majority of participants trusted their results and would perform a POC HIV test at home, given the opportunity.
Introduction
Background
Implementation of the Centers for Disease Control and Prevention guidelines for an “opt-out” policy under which HIV testing be normalized and that it be offered routinely for those patients 13–64 years of age who are in contact with primary care has not been well implemented. .1–6
Importance
Our hypothesis was that if patients could be encouraged to perform their own HIV rapid test during the lengthy waiting periods after triage procedures in the emergency departments (ED), significant staff time and money might be saved; however, only if feasibility and accuracy could be demonstrated.
Goals
Our objective was to evaluate the feasibility and accuracy of existing point-of-care(POC) HIV tests performed by untrained patients compared to results of an oral fluid POC HIV tests performed by health care professionals in urban EDs.
Methods
Setting
Two urban EDs in Baltimore, MD. ED 1 is an inner-city ED, with 60,000 visits/year, whose population is socioeconomically disadvantaged, comprised of > 75% African Americans, 15% injection drug users, and has a 11~12% HIV prevalence and a 2~3% newly recognized HIV infection rate. ED 2 serves an ethnically and socio-economically diverse urban population, with 50,000 visits/year and 30–35% African Americans. It has a high Sexually Transmitted Disease prevalence, with significant rates of high risk behaviors, and a 0.3% newly recognized HIV infection rate.
Study Design and Selection of Participants
From April 2008 through December 2009, patients who had already completed a standard HIV OraQuick Advance HIV1/2 test (oral fluid) test (OraSure, Bethlehem, PA) performed by a trained healthcare professional (either laboratory worker, ED 1, or trained healthcare worker, ED 2) and who were unaware of their result were recruited to volunteer for the study to perform one of two different rapid POC HIV tests (self-test). The two types of tests were explained to the patient. The Institutional Review Board of Johns Hopkins University approved the study and written consent was obtained. Patients aged 18 to 64 years, without a previous HIV diagnosis, were eligible. Consented patients were given a choice of performing either the oral fluid test or the Unigold test (Trinity, Berkeley, CA) (blood test). The oral fluid test required the patient to collect oral fluid, add the swab to a test vial, and wait 20 minutes to read the test result. The blood test required the patient to perform a spring-lancet finger-stick, collect 40 ul of blood in a capillary tube, dispense it onto a cartridge, add 4 drops of wash solution, and read the result in at least 10 minutes, but no more than 12 minutes. Both assays required the development of two lines for interpretation of a positive test, one control line and one test line.
Methods of measurement
The primary outcome was the overall evaluation of self-testing for HIV and was accessed by a questionnaire administered by a research assistant to evaluate the acceptability of performing the test by themselves, the confidence of the participant in the sample collection process and results they reported, as well as their overall satisfaction with performing the test, often in the format of a Likert scale. The secondary outcome was the agreement of the self-test result compared to the standard oral test.
Data collection
The standard oral fluid test was performed first. As a psychological consideration, the “self-test” was not performed by the patient until the results of the standard oral fluid tests results were available; however, the patient did not know the standard test result. For the self-test, the participant obtained his/her own sample, performed the test, and interpreted the results without instruction from the study coordinator. Study coordinators observed the performance of the self-test and recorded any difficulties encountered by the patients. Patients were given large plasticized instruction templates to use as visual aids for the sample collection and the testing procedure. Patients were provided with a $10 department store coupon for their time.
Primary Data Analysis
Standard HIV results were made immediately available to patients after the performance and their interpretation of their HIV self-test. Questionnaire results and observational information were recorded in an SPSS database. Data analysis was performed by SAS, version 9.1 (SAS Institute Inc., Cary, NC). Weighted kappa statistic was calculated to determine the level of agreement in testing results performed by health care workers/professionals and patients themselves. Difference of specific perception or attitude toward two different self-testing modalities and its 95% confidence interval (CI) was calculated to determine the significant difference in perception or attitude in patients tested between two methods. Statistical significant level was set at 0.05, 2-sided.
Results
Characteristics of Study Participants
Overall, 478/565 (85%) patients who volunteered had just received the standard oral fluid HIV test. Ninety-one percent of participants chose the oral fluid test and 9% chose the blood test (p<0.05). The demographics of the groups are presented in Table 1.
Table 1.
Demographic characteristics of participants for self-testing for HIV by two rapid HIV testing modalities.
| Characteristics | Categories | Oral Self-Test n= 433 |
Finger-stick Self- Test n= 45 |
|---|---|---|---|
| Age (years) | Mean ± S.D. | 38.5±12.7 | 37.2±13.0 |
| Gender | Male | 179 (41.3%) | 19 (42.2%) |
| Female | 254 (58.7%) | 26 (57.8%) | |
| Race | African American | 300 (69.3%) | 29 (64.4%) |
| White | 125 (28.9%) | 14 (31.1%) | |
| Others | 8 (1.8%) | 2 (4.5%) |
Primary Outcome of Collection and Performance
Ninety-seven percent of participants in the oral test group reported oral fluid “not at all hard to collect” while 84% stated blood was “not at all hard to collect” from the finger-stick (Table 2). Similarly, 98.8% of oral group and 82.2% of the finger-stick group indicated the sample collection was “not at all painful to collect,” while 96.3% of the oral fluid testers and 80.0% of the finger-stick patients reported the test “was not hard at all to perform the test correctly” (Table 2).
Table 2.
Attitudes participants toward two rapid HIV testing modalities after completion of performing self-test for HIV.
| Attitudes | Categories | Rapid HIV Testing Method
|
Difference in proportion (95% CI) | |
|---|---|---|---|---|
| Oral Self- Test n=433 |
Finger- stick Self-Test n=45 |
|||
| Self-collecting specimen was | Not hard at all | 421 (97.2%) | 38 (84.4%) | 12.8% (2.1%, 23.5%) |
| Self-collecting specimen was | Not painful at all | 428 (98.8%) | 37 (82.2%) | 16.6% (5.4%, 27.8%) |
| Self-collecting specimen was | Not unpleasant at all | 422 (97.5%) | 39 (86.7%) | 10.8%, (0.8%, 20.8%) |
| Self-performing the test | Not hard at all | 417 (96.3%) | 36 (80.0%) | 16.3% (4.5%, 28.1%) |
| Self-test result was | Definitely correct | 407 (94.0%) | 39 (86.7%) | 7.3% (-2.9%, 17.5%) |
| Trust self-test result | Very much | 392 (90.5%) | 38 (84.4%) | 6.1% (-4.9%, 17.0%) |
| Trust health care worker test result | Very much | 398 (91.9%) | 36 (80.0%) | 11.9% (-0.1%, 23.9%) |
| Feel in control of own health | Very much | 370 (85.5%) | 37 (82.2%) | 3.2% (-8.4%, 14.9%) |
| If available over-the-counter | Definitely test at home | 379 (87.5%) | 37 (82.2%) | 5.3% (-6.3%, 16.9%) |
| Recommend to a friend a self test for HIV | Definitely would | 407 (94.0%) | 38 (84.4%) | 9.6% (-1.3%, 20.4%) |
Trust
Results from the questionnaires about the trust of the test result and the testing process indicated that 94.0% on the oral fluid and 86.7% of the finger-stick testers reported they felt their test result was “definitely correct (Table 2). Ninety-one percent of patients in the oral group and 84.4% of patients in the blood group trusted the self-administered test result “very much.” For the oral fluid volunteers, 85.5% reported they “felt very much in control of their health,” while this was reported by 82.2% of the finger-stick group (Table 2).
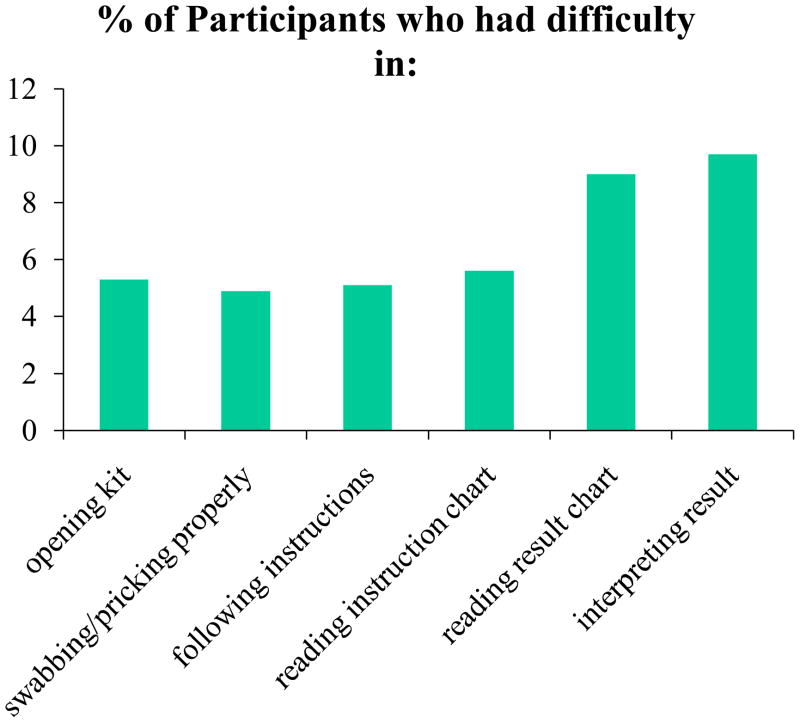
Ninety-eight percent of participants in the oral test group and 100% of the blood test group reported they would “definitely” or “probably recommend” self-testing to a friend, whereas 95.6% oral fluid testers and 93.3% of the blood testers would “probably” or “definitely” perform a test at home, if it were available (Table 2). Recorded observations of test performance difficulties by the study coordinators indicated that approximately 5–10% of patients encountered some difficulties in opening kits, obtaining samples, reading instructions and results, and interpreting results (Figure 1).
Figure 1.
Observed difficulties in self-testing process for HIV in participants.
Secondary outcome
Self-test results were 99.6% (476/478) over all concordant with health care workers’ test results (weighted kappa= 0.75, 95% CI: 0.41, 1.00). There was one “indeterminate” blood self-test, which had to be repeated due to insufficient blood. Upon repeat, it was negative and agreed with the standard test. One oral fluid self-test was interpreted as non-reactive by the patient, but was graded as “reactive” by the standard-of-care test. A subsequent western blot was found to be non-reactive.
There were three reactive self-tests performed by patients, which agreed correctly with the standard-of-care tests. The first one was a 45-year-old male who was determined to be previously positive in the patient’s medical record from five years earlier, although the patient claimed not to know that. The second one was a 58-year-old male. The third positive test was from a 28-year-old pregnant female, not known to be HIV positive. Additionally, there was one 56-year-old female, who was a “known HIV positive,” whose self-test and the standard POC test were both negative; the patient disclosed her positive HIV status afterward. That patient had an undetectable viral load and was on HAART.
Limitations
There are several limitations to this study. Since these were primarily urban hospital EDs, the results may not be generalizable to a population with different demographics. The design of the study, which required the patient to have just had a HIV POC test and collected the oral fluid for the standard test, probably biased the validity of the participants who chose the oral fluid test. Since very few patients tested positive, those who interpreted their test as negative may have been influenced by their expectation that the test would be negative. Our selection of specific candidate tests may have also played a role in the patients’ choices. Use of some other finger-stick POC HIV tests that require a smaller specimen volume and use a format more suitable to self-use, may have produced different results and attitudes than the test choices selected for this study.
The large plastic direction cards may have provided more detailed instructions that might not be available to the general self-testers in actual practice, although they appeared to be useful and could be useful in a commercial self-test kit format. The use of an incentive for the patients’ time could have biased and influenced the volunteer rate. Further study will be required to determine whether self-testing would ever be able to be put into practice in EDs to increase the number of patients who know their HIV status. Additionally, as we only reported three positive HIV results with self-testers using the rapid tests, it was impossible to determine the psychological impact of having participants learn their positive HIV status at their own hands. The participants’ testing difficulties, as observed and recorded by the study coordinators, may have been under or over reported and further study is required to determine the actual ability of patients to perform self-testing for HIV. Lastly, since most participants chose the oral fluid test, it was difficult to determine whether use of this finger-stick blood test could be useful for self-testing by patients.
Discussion
This pilot study demonstrated that a significant number of patients offered a POC HIV self-test in the ED would volunteer to perform their own HIV test. The 85% volunteer rate needs replication, especially in light of the fact that the participants already had a HIV test. Since ED clinicians are often time-constrained and frequently have barriers and inadequate staff support to assist with offering routine HIV screening to patients,5, 7–11 our team sought to study the acceptability and plausibility of having patients “perform” their own POC HIV test in an ED setting. However, we did not measure the acceptability of patients, who had never had a HIV test, to agree to perform a self-POC HIV self-test, due to the study design. We acknowledge we did not measure the willingness of patients to volunteer for HIV testing, but merely the attempt to perform the mechanics of the test procedure. Although patients who had already agreed to an HIV test are a biased sample, and different tests formats might have produced different results, we believe that we did gain some valuable insight into the willingness of a patient to perform the manipulation of the kit reagents in carrying out the laboratory aspect of the test procedure and interpretation of the results. Future studies will assess the volunteer aspect of agreeing to a HIV test and performing the POC test at the beginning of the ED visit.
Our hypothesis was that the performance of a oral fluid HIV POC test is relatively simple, e.g. it is CLIA waived, rated simple enough to be performed by minimally trained health care workers, and could be performed by patients themselves. We believed that with adequate instructional materials, patients would be able to perform the test themselves with proper oversight from ED staff regarding interpretation after the test was performed. We were not surprised that over 90% chose to perform the oral fluid test, yet for those who chose the finger-stick test, acceptance and trust measures were remarkably similar.
Although up to ~10% of patients were observed by research assistants to have some difficulties during the testing process, self reports of ease in the sample collection and testing process were quite high, especially in the oral fluid group, which ranged above 90%. However, even in the finger-stick group, reports for sample collection and testing were all above 80%. The recorded observations of “some difficulty” experienced by the patient in different aspects of the test are important and may affect the likelihood that users will be able to meet Food and Drug Administration criteria for home-use HIV tests.
For the oral fluid group, there appeared to be a similar high (91%) “trust of results” between the health care worker and the self-test, but the finger-stick testers trusted their own results (91.7%) more than the health care worker results (77.8%). It was gratifying that over 80% of volunteers reported feeling “being in control of own health” and that 82–94% reported that they would “definitely test at home” and “recommend to a friend,” if such an “over-the-counter test” were available. More study of this type approach will be required, but results from this pilot study were highly encouraging.
Additionally, there are many psychological issues for HIV self testing that require careful analysis and discussion, but further study of such premises may provide insight into the practicality of such practices in the future. Patient-centered care is under discussion by many health care reformers 13–15 and future comparative effectiveness research will add information to these considerations.16,17
In summary, volunteer rates to perform the self-test for HIV were very high, most participants preferred using oral fluid over blood, and self-testing appeared to be highly acceptable to patients seen in an ED setting. Patients’ self-testing results were 99.6% concordant with those obtained by healthcare professionals. The majority of participants trusted their results and would perform a POC HIV test at home, if given the opportunity.
Acknowledgments
Funding: NIBIB, NIH U-54EB007958; U01 AI068613
Reference List
- 1.Glynn M, Lee L, McKenna M. The status of national HIV case surveillance, United States. Public Health Rep. 2007;122:63–71. doi: 10.1177/00333549071220S110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. [Accessed November 3, 2010];HIV and AIDS in the United States: A Picture of Today’s Epidemic. http://www.cdc.gov/hiv/topics/surveillance/united_states.htm. Last Modified July 10, 2010.
- 3.Centers for Disease Control and Prevention. Missed opportunities for earier diagnosis of HIV infections: South Carolina, 1997–2005. MMWR Morb Mortal Wkly Rep. 2006;55:1269–1272. [PubMed] [Google Scholar]
- 4.Hsieh Y-H, Rothman RE, Newman-Toker DE, Kelen GD. National estimation of rates of HIV serology testing in US emergency departments 1993–2005: baseline prior to the 2006 Centers for Disease Control and Prevention recommendations. AIDS. 2008;22:1–8. doi: 10.1097/QAD.0b013e328310e066. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh Y-H, Jung JJ, Shahan JB, Moring-Parris D, Kelen GD, Rothman RE. Emergency medicine resident attitudes and perceptions of HIV testing before and after a focused training program and testing implementation. Acad Emerg Med. 2009:16. doi: 10.1111/j.1553-2712.2009.00507.x. In press. [DOI] [PubMed] [Google Scholar]
- 6.Branson B, Handsfield H, Lampe M, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 7.Irvin C, Flagel B, Fox J. The emergency department is not the ideal place for routine HIV testing. Ann Emerg Med. 2007;49:722. doi: 10.1016/j.annemergmed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 8.McKenna M. HIV testing: should the emergency department take part? Ann Emerg Med. 2007;49:190–192. doi: 10.1016/j.annemergmed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Borg K. To test or not to test? HIV, emergency departments, and the new Centers for Disease Control and Prevention guidelines. Ann Emerg Med. 2007;49:573–574. doi: 10.1016/j.annemergmed.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Rothman R, Ketlogetswe K, Dolan T, Wyer P, Kelen G. Preventive care in the emergency department: should emergency departments conduct routine HIV screening? A systematic review. Acad Emerg Med. 2003;10:278–285. doi: 10.1111/j.1553-2712.2003.tb02004.x. [DOI] [PubMed] [Google Scholar]
- 11.Brown J, Shesser R, Simon G. Establishing an ED HIV screening program: lessons learned from the front lines. Acad Emerg Med. 2007;14:658–661. doi: 10.1197/j.aem.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 12.Prost A, Griffiths CJ, Anderson J, Wright D, Hart GJ. Feasibility and acceptability of offering rapid HIV tests to patients registering with primary care in London (UK): a pilot study. Sex Transm Inf. 2009;85:326–329. doi: 10.1136/sti.2008.033233. [DOI] [PubMed] [Google Scholar]
- 13.Rittenhouse DR, Shortell SM. The patient-centered medical home. JAMA. 2009;301:2038–2040. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- 14.Crossing the Quality Chasm: A New Health System for the 21st Centruy. 2001. [Google Scholar]
- 15.Epstein RM, Peters E. Beyond information, Exploring patients’ preferences. JAMA. 2009;302:195–197. doi: 10.1001/jama.2009.984. [DOI] [PubMed] [Google Scholar]
- 16.Brook RH. Possible outcomes of comparative effectiveness research. JAMA. 2009;302:194–195. doi: 10.1001/jama.2009.996. [DOI] [PubMed] [Google Scholar]
- 17.Kuehn BM. Institute of Medicine outlines priorities for comparative effectiveness research. JAMA. 2009;302:936–937. doi: 10.1001/jama.2009.1186. [DOI] [PubMed] [Google Scholar]