Abstract
Attention to the effect of a patient's literacy skills on health care interactions is relatively new. So too are studies of either structural or personal factors that inhibit or support a patient's ability to navigate health services and systems and to advocate for their own needs within a service delivery system. Contributions of the structural environment, of interpersonal dynamics, and of a variety of psychological and sociological factors in the relationship between patients and providers have long been under study. Less frequently examined is the advocacy role expected of patients. However, the complex nature of health care in the U.S. increasingly requires a proactive stance.
This study examined whether four literacy skills (reading, numeracy, speaking, and listening) were associated with patient self-advocacy, a component of health literacy itself, when faced with a hypothetical barrier to scheduling a medical appointment. While all literacy skills were significantly associated with advocacy when examined in isolation, greater speaking and listening skills remained significantly associated with better patient advocacy when all four skills were examined simultaneously. These findings suggest that speaking and listening skills and support for such skills may be important factors to consider when developing patient activation and advocacy skills.
Keywords: literacy, advocacy, patient activation, speaking, listening
Introduction
Over the past thirty years, patient-provider relationships have undergone a transformation. Once viewed as the passive recipient of care, the patient has increasingly been called upon to take an active role in dialogue and decision-making and to engage in collaborative partnerships with caregivers. The importance of the active participation of patients in medical dialogue and decision-making has long been under study and is widely supported (Byrne & Long, 1976). Participatory engagement is promoted for ethical reasons, out of respect for autonomy, and for practical purposes based on efficacious outcomes.
Research has demonstrated, for example, that activated patients, those who participate and collaborate in the decision-making process and who share responsibility for decisions around treatment are more satisfied with their medical encounter overall, are more likely to perform self-management behaviors, have higher quality of life scores, and are more satisfied with and more likely to adhere to treatment protocols (Ballard-Reisch, 1990; Hibbard, Mahoney, Stock, & Tusler, 2007; Mosen, Hibbard, Sobel, & Remmers, 2007; D. L. Roter, Stashefsky-Margalit, & Rudd, 2001). Participatory decision-making has also been linked to improvements in disease control and to physical and emotional health status, functioning, and pain control (Greenfield, Kaplan, Ware, Yano, & Frank, 1988; Kaplan, Greenfield, & Ware, 1989; Stewart, 1995). One study, for example, found that “active” patients reported less discomfort, greater alleviation of symptoms, and more improvement in their general medical condition compared to more “passive” patients (Brody, Miller, Lerman, Smith, & Caputo, 1989).
Related to patient activation and participatory decision-making is the concept of patient self-advocacy, where individuals demonstrate an increased assertiveness or willingness to challenge providers or other medical authority, and to actively participate in decision-making to ensure they receive the care and treatment they feel best meets their needs (Brashers & Klingle, 1992). It can be argued that patient self-advocacy is, in fact, an important element of health literacy, defined by the Institute of Medicine as “the degree to which individuals have the capacity to obtain, process, communicate and understand basic health information and services needed to make appropriate health decisions” (Institute of Medicine, 2004). Research has identified a differential willingness and / or ability of some individuals to advocate for themselves or to actively participate in health care decisions (Bartlett, 1993; Beisecker & Beisecker, 1990; Brashers, Haas, & Neidig, 1999; Jackson, 1992). In fact, a recent study by Hibbard suggested that roughly 12% of their adult sample reported being passive recipients of care and were not playing an active role (Hibbard, Mahoney, Stockard, & Tusler, 2005). Other research has found that self-advocacy and patient activation are more likely to occur when individuals are faced with chronic or life-threatening illness, when such actions become even more relevant (Braden, 1990, 1991). Such findings suggest a need to identify factors that may contribute to the willingness or ability of individuals to participate in and advocate for their own health care needs.
A wide variety of contextual, demographic, and psychological factors that contribute to or inhibit patient participation have long been studied. Few, however, have addressed the contribution of literacy skills (D. L. Roter & Rudd, 1998). At the same time, there are many reasons to suspect that an association exists. First, medical care is intimidating for individuals with low literacy (Baker, et al., 1996), and many patients may harbor a sense of shame that makes disclosure of their low literacy more difficult (Institute of Medicine, 2004; Parikh, Parker, Nurss, Baker, & Williams, 1996). Second, limitations in oral and written communication make full participation difficult, and patients with limited literacy may be less likely to challenge or ask questions of a provider (Baker, et al., 1996; Paasche-Orlow & Wolf, 2007). Finally, individuals with low literacy may have less knowledge of health conditions, which limits their ability to take an active role in their care (Cooper, Beach, & Clever, 2005).
While the vast majority of research around patient activation and patient self-advocacy has focused on the patient-provider interaction and communication inside the examination room (Ghods, et al., 2008; D. Roter & Larson, 2002) and in the pharmacy setting (Cavaco & Roter, 2010), patient activation and advocacy are equally important for such tasks as navigation of the health care setting, including obtaining medical appointments within appropriate timeframes and with preferred providers. Furthermore, most studies to date have focused on a narrow understanding of health literacy, using measures that approximate reading skills alone without attention to speaking, listening, and math skills (Institute of Medicine, 2004). A limited number of studies, however, have demonstrated an association between listening skills and health outcomes including risk of coronary heart disease (Martin, et al., 2011), asthma management (Rosenfeld, et al., 2010), and comprehension of cancer messages (Mazor, et al., 2010) suggesting that measures of the oral exchange may further inform our understanding of literacy skills and health outcomes. Identifying the range of literacy skills associated with patient activation and advocacy may help to identify individuals who may benefit most from targeted interventions and may also provide insight into additional strategies for promoting activation and advocacy in the health care setting. The objective of this study was to examine whether literacy skills, independently and in combination, are associated with patient self-advocacy when faced with a hypothetical barrier to scheduling a medical appointment.
Methods
Study Population
Participants were offspring of pregnant women enrolled in the National Collaborative Perinatal Project (NCPP) between 1959 and 1966 (Niswander & Gordon, 1972). In 2001, the New England Family Study (NEFS) was established to locate and interview the now-adult cohorts of the Providence, Rhode Island and Boston, Massachusetts NCPP sites (n=17,921). As part of the NEFS, 914 participants in their mid 40s were selected in 2004 for a study designed to assess pathways linking education and health (Gilman, et al., 2008); literacy was a central pathway of this study. Of these, 618 (67.6%) were successfully located and interviewed.
Measures
Patient advocacy
Interviewers read the following text to study participants: “Joe's doctor told him that he would need to return in two weeks to find out whether or not his condition had improved. But when Joe asked the receptionist for an appointment, he was told that it would be over a month before the next available appointment.” Interviewers then asked two questions, “What should Joe do?” and after the respondent had given an answer they asked a probe: “What else should Joe do?” All answers were recorded on audio-tape and subsequently transcribed.
Coding of transcriptions
Categories ranging from counterproductive to proactive were articulated in advance. Using written coding rules, two researchers independently coded the transcriptions of each response into one of 4 categories: proactive, somewhat proactive, passive and counterproductive. Individuals were coded as proactive if they recommended actions to take before leaving the doctor's office that would likely result in getting an appointment in the two week time frame. Examples of proactive activities included asking the receptionist to speak with the doctor while Joe waited or suggesting that Joe engage the doctor directly to rectify the situation. Individuals who suggested obtaining a follow-up visit with another provider within the same practice or office within the two-week time frame were also coded as proactive. An individual was coded as somewhat proactive if they recommended that Joe accept the appointment in one month but asked to be put on a waiting list, or asked the staff to check with the doctor at a later time to see if accommodations should or could be made for an earlier appointment. Individuals were coded as passive if they recommended taking the appointment in a month or taking no other action than telling the receptionist that the doctor had told him to return in two weeks. Individuals were coded as counterproductive if they recommended leaving without any appointment or going to an urgent care clinic or emergency room for follow-up care.
We created an additional fifth category called “becomes proactive” to capture those individuals who in their initial response were coded as counterproductive, passive or somewhat proactive, but who recommended proactive behaviors in response to the probe (e.g., “If that didn't work, I would ask to speak to the doctor directly.”) As a result, we had five mutually exclusive categories for analyses: counterproductive, passive, somewhat proactive, becomes proactive, and proactive.
We computed the inter-rater agreement statistic Cohen's kappa (Cohen, 1960) based on initial ratings (both for 4-category and 5-category ratings). After initial ratings, the two researchers discussed responses that were rated differently and resolved the differences.
Literacy
We measured four literacy skills: reading comprehension, numeracy, oral language (speaking), and aural language (listening). Reading comprehension, oral language, and aural language were assessed using subtests of the Woodcock Johnson III (WJ III), a standardized test normed against a representative U.S. population, ages 24 months to 90 years and older (Woodcock, McGrew, & Mather, 2001b). Grade equivalent scores (GE) were used in these analyses, and ranged from kindergarten (0.0) to 18.0. While the WJ III tests are cognitive measures, and not measures of literacy or health literacy per se, in the absence of validated measures of the oral and aural exchange, these subtests represent the best available measures to assess these constructs quickly and reliably. Numeracy was assessed using an eight-item scale adapted from Lipkus et al. (Lipkus, Samsa, & Rimer, 2001) as described below.
Oral language was assessed by the WJ III achievement test “Story Recall,” where participants listen to a pre-recorded short story (1–3 paragraphs) and are then asked to repeat the story back to the interviewer. The administration of this test is similar to commonly used “teach-back” methods that providers use to gauge patient communication, understanding and recall of health messages and instructions. Scores are based on the correct number of words or phrases spoken (Woodcock, et al., 2001b). “Story Recall” is designed to measure aspects of oral language including language development and meaningful memory. “Story recall” has a median reliability of 0.89.
Aural language, or listening comprehension, was assessed by the WJ III achievement test “Understanding Directions,” where participants are given an illustrated drawing and are asked to follow pre-recorded directions to point to objects in the picture (e.g., “point to the blue book on the shelf”). Difficulty increases as drawings become more complex and the tasks increase in number of components. Scores (grade level equivalents) are based on the number of correct tasks completed. This test was selected for its similarity to experiences in the health care setting, where providers give patients a set of instructions for taking their medicine or preparing for a medical procedure, for example. “Understanding directions” has a median reliability of 0.90.
Reading comprehension was assessed using the “Passage Comprehension” test from the WJ III Tests of Achievement—a cloze test, where individuals fill in missing words from a sentence. The one-year test-retest reliability was 0.92 and validation against the reading composite scores of the Kaufman Test of Educational Achievement (Kaufman, 1985) and the Wechsler Individual Achievement Test (Wechsler, 1992) show good validity with correlations of 0.81 and 0.78, respectively (Woodcock, McGrew, & Mather, 2001a).
Numeracy was assessed using an eight-item scale. Two items were selected from general numeracy questions developed by Schwartz and colleagues (Schwartz, Woloshin, Black, & Welch, 1997), and the remaining six were selected from an expanded seven-item numeracy scale developed by Lipkus and colleagues, where similar questions were asked within a health context. The eight items focused on such tasks as discerning differences in magnitudes of health risks, performing mathematical operations on risk magnitudes, and converting percentages to proportions. Participants were provided a pencil and paper to perform calculations and responses were open-ended. The proportion of our sample who responded correctly to each item is similar to that found in other samples. Numeracy scores were calculated based on the total number of correct responses (range: 0–8). The decision not to implement the full Lipkus scale, while not ideal, was dictated by constraints on the total number of items in the questionnaire that were beyond our control. Psychometric properties of the 8-item scale are similar to the original scale (Schonlau, et. al. In press).
Analyses
We examined descriptive statistics of the full sample and by patient advocacy rating group. We tested the hypothesis of no relationship between each demographic variable or literacy skill and the 5-level rating category using ANOVAs (for continuous variables) and chi-square tests (for categorical variables).
In order to characterize the relationship between literacy skills and patient advocacy, we modeled the separate and joint relationships between patient literacy skills and their propensity to be proactive while adjusting for socio-demographic variables. We conducted partial ordered logistic regression analyses with the 5-level patient advocacy as the outcome because the proportional odds assumption needed for ordinary ordered logistic regression analyses was not met for some demographic characteristics. (Lall, Campbell, Walters, & Morgan, 2002; Peterson & Harrell Jr., 1990) However, the interpretation of coefficients from partial and ordinary ordered logistic regression is identical in that the odds ratios compare the odds of between two levels of patient advocacy (e.g., becomes proactive and higher versus somewhat active and lower) for a one unit increase in the independent variable (e.g., speaking). All analyses controlled for age, education (number of years), gender, race /ethnicity (non-Hispanic White, non-Hispanic black, Hispanic/other), and income level (<20K, 20–60K,>60K) (Schonlau, et al., In press).
To ensure that results were robust, we repeated the analyses using as the outcome the 4-category patient advocacy measure (proactive, somewhat proactive, passive, counterproductive) defined based on the initial question only, ignoring the probe. All analyses were done in Stata Version 11.1 including partial ordered logistic regression (Williams, 2006).
Results
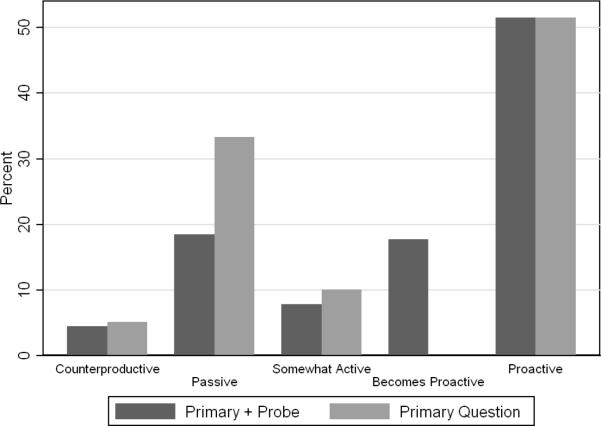
The distributions of respondents by the 4- and 5-level patient advocacy groups are shown in Figure 1. Most people rated “become proactive” were initially scored as “passive” based on the primary question. The majority of individuals were rated as “proactive” (51.5%), followed by “passive” (18.4%), becomes proactive” (17.7%). and “somewhat proactive” (10.1%). Only 5.1% were rated as counterproductive. The inter-rater reliability kappa for the primary question (4 categories) and the 5-category variable were 80% and 79%, respectively.
Figure 1.
Ratings (%) based on the primary question (4 groups) and primary question with an additional group for “becomes proactive” in the probe (5 groups)
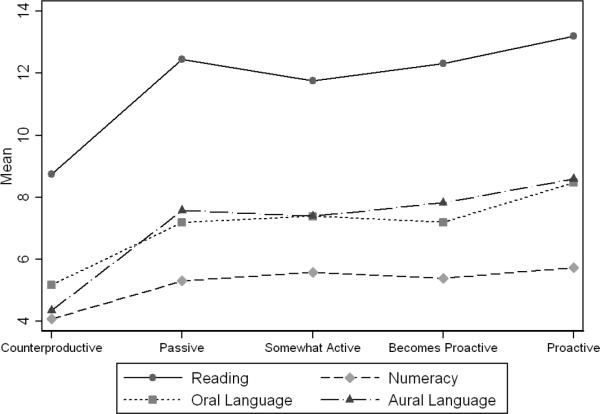
Table 1 shows demographic characteristics as well as average reading, listening, speaking and numeracy skills overall and in each of the 5 groups. Figure 2 shows average literacy skills by rating group. Respondents in the counterproductive group generally had noticeably lower literacy skills, although there were significant differences in literacy skills between those in other levels of patient activation (e.g., passive, somewhat active) compared to proactive (Table 1). Counterproductive respondents were more likely to be male, less educated, non-white and were less likely to be in the highest income bracket. Socio-demographic differences among the other four groups were less pronounced.
Table 1.
Demographic and Health Literacy covariates in each of 5 patient advocacy groups.1
| Full sample | Proactive | Becomes Proactive | Somewhat Proactive | Passive | Counterproductive | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| N | 586 | 302 | 104 | 46 | 108 | 26 | |||||||
| Age, years | 42.5 | 1.8 | 42.6 | 1.8 | 42.3 | 1.9 | 42.4 | 2.1 | 42.4 | 1.7 | 42.5 | 1.6 | 0.66 |
| Education, years | 13.7 | 2.6 | 13.9 | 2.7 | 13.9 | 2.7 | 13.6 | 2.9 | 13.2 | 2.0 | 11.9 | 2.0 | <0.001 |
| Race | 0.045 | ||||||||||||
| White | 78.4 | 81.4 | 80.6 | 67.4 | 78.7 | 53.9 | |||||||
| Black | 16.3 | 15.0 | 13.6 | 23.9 | 14.8 | 34.6 | |||||||
| Hispanic/other | 5.3 | 3.7 | 5.8 | 8.7 | 6.5 | 11.5 | |||||||
| Male | 39.9 | 38.1 | 37.5 | 37.0 | 43.5 | 61.5 | 0.17 | ||||||
| Income category | <0.001 | ||||||||||||
| Less than 20,000 | 37.7 | 37.1 | 35.6 | 45.7 | 35.2 | 50.0 | |||||||
| 20,000–60,000 | 9.8 | 7.7 | 6.7 | 8.7 | 11.1 | 42.3 | |||||||
| More than 60,000 | 52.5 | 55.2 | 57.7 | 45.7 | 53.7 | 7.7 | |||||||
| Literacy Skills2 | |||||||||||||
| Reading | 12.6 | 4.8 | 13.2 | 4.6 | 12.3 | 4.8 | 11.8* | 4.7 | 12.4 | 4.9 | 8.7** | 4.7 | <0.001 |
| Numeracy | 5.5 | 1.8 | 5.7 | 1.8 | 5.4* | 1.8 | 5.6 | 1.6 | 5.3* | 2.0 | 4.1** | 2.1 | <0.001 |
| Speaking | 7.8 | 1.8 | 8.5 | 4.7 | 7.2* | 4.3 | 7.4 | 4.6 | 7.2* | 3.9 | 5.2** | 3.2 | 0.002 |
| Listening | 8.0 | 4.3 | 8.6 | 4.3 | 7.8 | 3.8 | 7.4 | 4.1 | 7.6* | 4.5 | 4.4** | 2.2 | <0.001 |
For continuous variables, standard deviations (SD) are also shown. p-values are based on ANOVAs (for continuous variables) or chi-square tests (for categorical variables) testing the hypothesis of no relationship between the demographic or literacy variable and the 5-level patient advocacy outcome.
Within each literacy skill, pairwise testing was conducted comparing each level of patient advocacy to proactive
p<0.05 Health literacy skill significantly different from proactive (Pairwise testing)
p<0.01 Health literacy skill significantly different from proactive (Pairwise testing)
Figure 2.
Mean Scores for each of 4 literacy skills by rating group
Ordered logistic regression requires a proportional odds assumption. If satisfied, the proportional odds assumption implies that a single coefficient for each independent variable is sufficient. If not satisfied, the number of coefficients equals the number of categories in the dependent variable minus one. Each coefficient refers to the increase in odds for a different combination of ordered categories: proactive versus the combined remainder, proactive and becomes proactive versus the combined remainder, and so forth. A partial proportional odds model requires multiple coefficients (equivalently, multiple odds ratios) only for independent variables where the proportional odds assumption is not satisfied. Here, the proportional odds assumption was satisfied for all literacy measures in adjusted regression models, but it was not satisfied for income and for some models for black race/ethnicity (those models in Table 2 where coefficients are not identical). For these characteristics, we present all odds ratios. For example, for a one unit increase in listening in model 6, the odds of proactive versus all other categories combined increase by a factor of 1.06 (or increase by 6%). Because the proportional odds assumption is met for listening, the odds increase by the same factor for all other combinations (e.g., the highest three versus the lowest two categories).
Table 2.
Partial ordered logistic regressions showing the relationship between individual literacy skills and increasing levels of patient advocacy
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5† | Model 6† | |
|---|---|---|---|---|---|---|
| n=528 | n=566 | n=509 | n=520 | n=486 | n=497 | |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Reading | 1.05 (1.00–1.09)* | 1.01 (0.95–1.06) | ||||
| Numeracy | 1.14 (1.02–1.07)* | 1.05 (0.91–1.22) | ||||
| Speaking | 1.07 (1.03–1.11)** | 1.05 (1.01–1.10)* | 1.05 (1.00–1.10)* | |||
| Listening | 1.07 (1.02–1.12)** | 1.05 (.98–1.12) | 1.06 (1.00–1.13)* | |||
| Education (years) | 1.05 (0.98–1.13) | 1.04 (0.98–1.11) | 1.04 (0.97–1.12) | 1.05 (0.98–1.13) | 1.01 (0.93–1.09) | 1.02 (0.95–1.10) |
| Age (years) | 1.10 (1.00–1.20)* | 1.08 (0.99–1.17) | 1.11 (1.01–1.22) | 1.12 (1.02–1.23)* | 1.14 (1.03–1.26)** | 1.13 (1.03–1.25)* |
| Sex | ||||||
| Male | 0.65 (0.46–0.92)* | 0.64 (0.46–0.90)** | 0.73 (0.51–1.03) | 0.75 (0.54–1.05) | 0.68 (0.46–0.99)* | 0.73 (0.52–1.04) |
| Female | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Race/ethnicity | ||||||
| Hispanic | 0.44 (0.19–1.02) | 0.43 (0.22–0.84)* | 0.47 (0.21–1.05) | 0.50 (0.23–1.09) | 0.41 (0.19–0.93)* | 0.47 (0.21–1.02) |
| Black | ||||||
| OR11 | 0.41 (0.18–0.91)* | 0.85 (0.53–1.37) | 0.83 (0.50–1.38) | 0.41 (0.18–0.92)* | 0.90 (0.53–1.53) | 0.90 (0.53–1.53) |
| OR22 | 1.05 (0.57–1.92) | 0.85 (0.53–1.37) | 0.83 (0.50–1.38) | 1.08 (0.59–1.98) | 0.90 (0.53–1.53) | 0.90 (0.53–1.53) |
| OR33 | 0.83 (0.47–1.45) | 0.85 (0.53–1.37) | 0.83 (0.50–1.38) | 0.90 (0.52–1.57) | 0.90 (0.53–1.53) | 0.90 (0.53–1.53) |
| OR44 | 0.94 (0.55–1.59) | 0.85 (0.53–1.37) | 0.83 (0.50–1.38) | 1.02 (0.60–1.73) | 0.90 (0.53–1.53) | 0.90 (0.53–1.53) |
| White | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Income | ||||||
| Less than $20,000 | ||||||
| OR1 | 0.05 (0.01–0.26)** | 0.06 (0.01–0.29)** | 0.05 (0.01–0.24)** | 0.05 (0.01–0.27)** | 0.06 (0.01–0.32)** | 0.05 (0.01–0.24)** |
| OR2 | 0.61 (0.28–1.30) | 0.65 (0.32–1.34) | 0.71 (0.33–1.50) | 0.65 (0.31–1.37) | 0.81 (0.36–1.86) | 0.76 (0.35–1.65) |
| OR3 | 0.66 (0.32–1.38) | 0.71 (0.36–1.39) | 0.69 (0.34–1.39) | 0.64 (0.31–1.29) | 0.82 (0.38–1.77) | 0.72 (0.35–1.48) |
| OR4 | 0.85 (0.42–1.73) | 1.01 (0.52–1.97) | 0.93 (0.47–1.86) | 0.90 (0.45–1.78) | 1.14 (0.54–2.38) | 1.05(0.52–2.09) |
| $20,000–60,000 | ||||||
| OR1 | 0.16 (0.03–0.73)* | 0.13 (0.03–0.56)** | 0.16 (0.03–0.73)* | 0.15 (0.03–0.68)* | 0.18 (0.04–0.86)* | 0.18 (0.04–0.86)* |
| OR2 | 1.09 (0.68–1.74) | 0.90 (0.57–1.43) | 0.93 (0.58–1.49) | 1.07 (0.67–1.72) | 0.99 (0.61–1.63) | 1.06 (0.65–1.72) |
| OR3 | 0.90 (0.59–1.38) | 0.83 (0.54–1.25) | 0.79 (0.51–1.21) | 0.86 (0.56–1.33) | 0.81 (0.51–1.28) | 0.86 (0.55–1.34) |
| OR4 | 1.09 (0.74–1.62) | 1.02 (0.69–1.49) | 1.00 (0.67–1.49) | 1.04 (0.70–1.54) | 1.05 (0.69–1.58) | 1.08 (0.72–1.62) |
| $60,000 + | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
In model 5, a joint test of reading, numeracy, speaking and listening is significant (p=0.03). In model 6, a joint test of speaking and listening is significant (p<0.001)
p<0.05
p<0.01
OR1: Proactive/becomes proactive/somewhat active/passive vs. counterproductive
OR2: Proactive/becomes proactive/somewhat active vs. passive/counterproductive
OR3: Proactive/becomes proactive vs. somewhat active/passive/counterproductive
OR4: Proactive vs. becomes proactive/somewhat active/passive/counterproductive
Partial ordered logistic regression results suggested that all individual literacy skills were associated with higher patient advocacy even after adjusting for covariates (Table 2, Models 1–4). Because numeracy has a smaller range (0–8) than the other three literacy variables (0–18), a one-unit increase in numeracy is a much larger increase than a one-unit increase for other literacy variables.
Model 5 examines all four literacy skills together. Only speaking was significantly associated with patient advocacy. A one unit grade-level increase in speaking skills increased the odds of a higher level of patient activation by 5%. A joint test of all four literacy skills on patient advocacy was significant, p=0.003.
Because literacy variables are moderately correlated, ranging from 0.37 (speaking-numeracy) to 0.60 (reading-numeracy) with all other correlations ranging between 0.43–0.47 (Schonlau, et al., In press), we eliminated non-significant literacy variables from the model, specifically reading and numeracy to minimize multicollinearity (model 6). The remaining 2 variables, speaking and listening, were independently significant (p=0.047 and p=0.041 respectively) and a joint test of speaking and listening on patient advocacy was highly significant (p=0.0001). For example, a one unit grade-level increase in speaking skills and a one unit grade-level increase in listening skills increased the odds of proactive versus all other categories combined in the range of patient activation by 5% and 6% respectively.
To ensure that the results were robust, we repeated the analysis using the 4 category patient advocacy based on the initial question only (thus ignoring the probe). The results were qualitatively identical. Individual literacy variables adjusted for demographics remained significant. When considered jointly adjusted for demographic variables, speaking and listening were the only two skills significantly associated with patient advocacy.
Discussion
A single grade-level increase in speaking and listening skills is associated with a 5% and 6% increase in the odds of a patient being more proactive, respectively, even after adjusting for education and other socio-demographic covariates. Although reading and numeracy were independently associated with patient advocacy, our findings suggest that they are less important than literacy skills related to the oral exchange (speaking and listening). These findings were robust in that they held for both the five-level measure of patient advocacy, which included information from both the primary question “What should Joe do?” and the probe “What else should Joe do?” as well as the four-level measure, which utilized responses from the primary question only.
There are several limitations of this study worth noting. First, our sample consists of individuals in their early to mid-40s, living in Providence, RI and Boston, MA and as a result, may not be generalizable. All respondents were born in the United States, and the interviews were conducted in English; it is not clear whether similar associations between literacy skills and patient advocacy skills would be found among the foreign-born and non-English-speakers. There is also the potential for non-response bias, due to a 67% response rate, although previous analyses on this cohort suggest that there are few demographic differences between those who were located and interviewed and those who were not. It is also possible that responses to our vignette may differ slightly from those that may occur in “real life” scenarios. Individuals may feel more comfortable reporting proactive behaviors in a research setting, but it is not clear whether they would act in the same manner in a physician's office, when interacting with office staff and perceiving power differentials between themselves and medical personnel.
As one of the first studies to examine the independent and combined effects of four literacy skills on patient advocacy, this study provides important insight for further research and practice. First, these findings highlight a current gap in research that focuses primarily on reading and, increasingly, numeracy. By not assessing speaking and listening skills, there is significant potential to overlook important issues that may inform the development of supports to improve patient activation and advocacy. Such gaps may be filled by newer measures, including the Health Literacy Skills Instrument (HLSI), which uses a skill-based approach to measure individual health literacy, assessing information seeking skills, and other skills related to health care maintenance and system navigation (McCormack et al., 2010). Use of such skills-based measures, which include similar stimuli to the scenario presented here, have strong potential to elucidate complex relationships between literacy skills, health literacy and patient activation, and to help clarify the extent to which these are separate or overlapping constructs.
Second, our findings highlight the importance of patient activation and advocacy for a range of health-related tasks that extend beyond the patient-provider interaction in the examination room. For example, the roles of patient activation and advocacy are necessary for successfully accomplishing tasks such as navigating the health care system, obtaining medical appointments within specified time frames and with preferred providers, and advocating on behalf of themselves or family members in other health settings such as the pharmacy.
The hypothetical situation presented to study participants was related to obtaining a physician appointment within a given timeframe. Although hypothetical, many study participants reported having undergone similar experiences with their own provider suggesting that this may be a potential barrier to care, and a potential area to develop or expand supports that may improve patient activation and advocacy. Although further conceptual work is needed to better understand the relationships, the results of this study suggest that speaking and listening skills may be important factors to consider when developing patient activation and advocacy supports and highlights the need to further develop health care system and physician processes that may facilitate patient advocacy. While patient-focused supports may be warranted, simple steps, such as having doctors tell their patients to check back with them if there are any problems scheduling an appointment, may facilitate more proactive self-advocacy behaviors and may reduce some of the challenges and poor health outcomes related to waiting too long for an appointment, seeking care elsewhere or not at all.
Acknowledgement
This work was supported by NHLBI grant 1R21HL094297-01 (Martin).
References
- Baker DW, Parker R, Williams MV, Pitkin K, Parikh N, Coates W, et al. The health care experience of patients wtih low literacy. Arch Fam Med. 1996;5:329–334. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- Ballard-Reisch DS. A Model of Participative Decision Making for Physician-Patient Interaction. Health Communications. 1990;2(2):91–104. [Google Scholar]
- Bartlett CL. Communication disorders in adults with AIDS. In: Ratzan SC, editor. AIDS : effective health communication for the 90s. Taylor & Francis; Washington, D.C.: 1993. pp. 189–200. [Google Scholar]
- Beisecker AE, Beisecker TD. Patient information-seeking behaviors when communicating with doctors. [Comparative Study] Medical care. 1990;28(1):19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- Braden CJ. Learned self-help response to chronic illness experience: a test of three alternative learning theories. [Research Support, U.S. Gov't, P.H.S.] Scholarly inquiry for nursing practice. 1990;4(1):23–41. discussion 43–25. [PubMed] [Google Scholar]
- Braden CJ. Patterns of change over time in learned response to chronic illness among participants in a systemic lupus erythematosus self-help course. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Arthritis care and research : the official journal of the Arthritis Health Professions Association. 1991;4(4):158–167. doi: 10.1002/art.1790040405. [DOI] [PubMed] [Google Scholar]
- Brashers DE, Haas SM, Neidig JL. The patient self-advocacy scale: measuring patient involvement in health care decision-making interactions. Health communication. 1999;11(2):97–121. doi: 10.1207/s15327027hc1102_1. [DOI] [PubMed] [Google Scholar]
- Brashers DE, Klingle RS. The influence of activism on physician-patient communication. Speech Communication Association Annual Meeting.1992. [Google Scholar]
- Brody D, Miller S, Lerman C, Smith D, Caputo G. Patient perception of involvement in medical care: relationship to illness attitudes and outcomes. J Gen Intern Med. 1989;5(1):29–33. doi: 10.1007/BF02599549. [DOI] [PubMed] [Google Scholar]
- Byrne PS, Long BEL. Doctors talking to patients : a study of the verbal behaviour of general practitioners consulting in their surgeries. Her Majesty's Stationery Office; London: 1976. [Google Scholar]
- Cavaco A, Roter D. Pharmaceutical consultations in community pharmacies: utility of the Roter Interaction Analysis System to study pharmacist-patient communication. [Review] The International journal of pharmacy practice. 2010;18(3):141–148. [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement. 1960;20:37–46. [Google Scholar]
- Cooper LA, Beach MC, Clever SL. Participatory decision-making in the medical encounter and its relationship to patient literacy. In: Schwartzberg JG, VanGeest JB, Wang CC, editors. Understanding health literacy: Implications for medicine and public health. AMA Press; Chicago, IL: 2005. pp. 141–154. [Google Scholar]
- Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Journal of general internal medicine. 2008;23(5):600–606. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman S, Martin L, Abrams D, Kawachi I, Kubzansky L, Loucks E, et al. Educational attainment and smoking: A causal association? International Journal of Epidemiology. 2008;37(3):615–624. doi: 10.1093/ije/dym250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield S, Kaplan S, Ware J, Yano E, Frank H. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- Hibbard J, Mahoney E, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42(4):1443–1463. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard J, Mahoney E, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Services Research. 2005;40(6–1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . Health Literacy: A Prescription to End Confusion. National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- Jackson L. Information complexity and medical communication: The effect of technical language and amount of information in a medical message. Health Communication. 1992;4(197-210) [Google Scholar]
- Kaplan S, Greenfield S, Ware JJ. Assessing the effects of physician patient interactions on the outcomes of chronic disease. Medical Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- Kaufman AS. Kaufman Test of Educational Achievement: Comprehensive Form Manual. American Guidance Service; 1985. [Google Scholar]
- Lall R, Campbell MJ, Walters SJ, Morgan K. A review of ordinal regression models applied on health-related quality of life assessments. [Research Support, Non-U.S. Gov't] Statistical methods in medical research. 2002;11(1):49–67. doi: 10.1191/0962280202sm271ra. [DOI] [PubMed] [Google Scholar]
- Lipkus I, Samsa G, Rimer B. General performance on a numeracy scale among highly educated samples. Medical Decision Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Martin L, Schonlau M, Haas A, Derose K, Rudd R, Loucks E, et al. Literacy skills and calculated 10-year risk of coronary heart disease. Journal of General Internal Medicine. 2011;26(1):45–50. doi: 10.1007/s11606-010-1488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazor KM, Calvi J, Cowan R, Costanza ME, Han PK, Greene SM, et al. Media messages about cancer: what do people understand? [Research Support, N.I.H., Extramural] Journal of Health Communication. 2010;15(Suppl 2):126–145. doi: 10.1080/10810730.2010.499983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack L, Bann C, Squires L, Berkman N, Squire C, Schillinger D, et al. Measuring Health Literacy: A Pilot Study of a New Skills-Based Instrument. Journal of Health Communication. 2010;15:51–71. doi: 10.1080/10810730.2010.499987. [DOI] [PubMed] [Google Scholar]
- Mosen D, Hibbard J, Sobel D, Remmers C. Is patient activation associated with better health outcomes for adults with cardiovascular disease?. 13th Annual HMO Research Network Conference.2007. [Google Scholar]
- Niswander KR, Gordon M. The Women and Their Pregnancies: the Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. National Institute of Health; Washington, D.C.: 1972. [Google Scholar]
- Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- Parikh N, Parker R, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Educ Couns. 1996;27(1):33–39. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- Peterson B, Harrell F., Jr. Partial proportional odds models for ordinal response variables. Applied Statistics. 1990;39(2):205–217. [Google Scholar]
- Rosenfeld L, Rudd R, Emmons K, Acevedo-Garcia D, Martin L, Buka S. Beyond reading alone: The relationship between aural literacy and asthma management. Patient Educ Couns. 2010 doi: 10.1016/j.pec.2010.02.023. DOI:10.1016/j.pec.2010.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient education and counseling. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Roter DL, Rudd R. Patient literacy: a barrier to quality of care. J Gen Intern Med. 1998;13:850–851. doi: 10.1046/j.1525-1497.1998.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Stashefsky-Margalit R, Rudd R. Current perspectives on patient education in the US. [Historical Article] Patient education and counseling. 2001;44(1):79–86. doi: 10.1016/s0738-3991(01)00108-2. [DOI] [PubMed] [Google Scholar]
- Schonlau M, Martin L, Haas A, Pitkin Derose K, Rudd R. Patients' Literacy Skills: More than just reading ability. Journal of health communication. doi: 10.1080/10810730.2011.571345. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L, Woloshin S, Black W, Welch G. The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine. 1997;127:966–971. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Stewart M. Effective physician-patient communication and health outcomes: A review. Can Med Assoc J. 1995;152:1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Individual Achievement Test. Psychological Corporation; San Antonio, TX: 1992. [Google Scholar]
- Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata Journal. 2006;6(1):58–82. [Google Scholar]
- Woodcock RW, McGrew KS, Mather N. Technical Manual. Woodcock-Johnson III. Riverside Publishing; Itasca, IL: 2001a. [Google Scholar]
- Woodcock RW, McGrew KS, Mather N. Woodcock-Johnson III Tests of Achievement. Riverside Publishing; Itasca, IL: 2001b. [Google Scholar]