Summary
Even if calculating the exact cost of burn treatment is a very hard task, the study of cost analysis provides financial perspective. We performed a cost analysis study in our burn centre to respond to questions about total patient treatment cost and the length of hospital stay. We reviewed all patients admitted to the Gulhane Military Medical Academy Burn Centre in Ankara, Turkey, between March 2005 and August 2008. Forty-three patients with major burns were identified on the basis of the study criteria. The data regarding total treatment cost and the length of hospital stay for each type of burn (flame, scald, electric) were collected at the end of the study. The average total body surface area burned was 36 ± 7%.. The average duration of hospital stay was 73 ± 33 days. Patients with electrical burns stayed longer in hospital than patients with other types of burn injuries. Each one per cent of burn corresponded to a mean hospital stay of two days. The overall mean total cost was $US 15,250. The mean total cost of electrical burns was the highest, with $US 22,501 ± 24,039. Even if the costs associated with burn injury are higher than some other well-known health-related problems, they have not been much studied. Reports have produced different results, but it should be kept in mind that although the results of cost analysis studies may vary they must be performed in all newly established burn centres in order to form a financial overview.
Keywords: BURN, COST ANALYSIS, HEALTH ECONOMICS
Abstract
Quoique le calcul du coût exact du traitement des brûlures soit un tâche très difficile, l’étude de l’analyse des coûts fournit certaines perspectives économiques financières. Nous avons effectué une étude comparative des coûts dans notre centre de brûlures afin de répondre à des questions sur le coût total du traitement des patients et sur la durée de l’hospitalisation. Nous avons examiné les dossiers de tous les patients admis au Centre des Brûlés de l’Académie Médicale Militaire Gulhane à Ankara, en Turquie, entre mars 2005 et août 2008. Quarante-trois patients gravement brûlés ont été identifiés sur la base des critères de l’étude et toutes les données sur le coût total du traitement et la durée de l’hospitalisation, pour chaque catégorie de brûlure (flamme, ébouillantement, électricité) ont été recueillies à la fin de l’étude. La surface corporelle brûlée moyenne était de 36 ± 7%. La durée moyenne de l’hospitalisation était de 73 ± 33 jours. Les patients atteints de brûlures électriques sont restés plus longtemps à l’hôpital que les patients atteints d’autres types de brûlures. Chaque un pour cent de surface corporelle brûlée correspondait à une durée moyenne de séjour à l’hôpital de deux jours. Le coût total moyen était de $US 15.250. Le coût total moyen pour les brûlures électriques était le plus élevé ($US 22.501 ± 24.039). Quoique les coûts associés aux brûlures soient plus élevés que ceux de certains autres problèmes sanitaires bien connus, ils sont peu étudiés et présentent une large variété de résultats. Il faut quand même tenir compte du fait que malgré la diversité des résultats des études de l’analyse des coûts, il faut continuer à les effectuer dans tous les centres des brûlés nouvellement créés afin d’avoir une perspective économique générale.
Introduction
The consequences of severe burns include mortality, morbidity, and economic and social costs, which are paid by burn victims, their families, health authorities, and society in general. The primary concerns following an acute burn are mortality and morbidity. The primary concerns change into secondary concerns regarding the economic and social costs of burns in time.
Burn care is the one of the costliest areas of health care.1 Long hospital stays, multiple operations, and expensive equipment requirements make it expensive.2 Although any attempt to draw up an exact list of costs is a very hard task, evaluations of the economic efficiency of burns treatment should be made in order to obtain financial data regarding burn centres or units.
There are several cost methodologies, such as direct or indirect cost via the Human Capital theory.3,4 Even in computing direct costs, many variables - including room costs, staff costs, pharmaceutical costs, and dressing costs - influence the cost accounting process.1 The final results of cost analysis studies may differ even within the same country because every study has its specific list of costs.
However, although these studies may not give the precise economic costs of acute burn care, they provide a financial perspective for both patients and hospital administrators.
Gulhane Military Medical Academy Burn Centre was established in 1976. It was the first burn centre in Turkey and has been receiving burn patients with major injuries from all over the country for nearly 35 years. Turkey now has over 10 burn centres and 20 burns units, but there is a limited number of up-to-date studies concerning burn costs.5 This is the first cost analysis study dealing with our burn centre.
The aim of our study was to identify the current direct costs of acute burn treatment in our burn centre n order to respond to questions about total patient treatment costs and the duration of hospital stay.
Methods
A retrospective review was performed of all patients admitted to the Gulhane Military Medical Academy Burn Centre between Mach 2005 and August 2008. The patients were identified through the hospital patient administration system. We treated 300 acute burn patients during this period. In order to minimize accounting discrepancies and variations, the study was conducted according to the following criteria.
Patients with the following characteristics were included in the study:
> 15% total body surface area (TBSA) burned;
deep second-degree burns and/or third-degree burns;
non-governmental social security (hospital discharge costs paid by the patients themselves).
The following were excluded:
patients who had concomitant trauma;
patients transferred from other burn centres after more than seven days;
patients with a concomitant disease and needing hospitalization in other clinics;
patients who died during the period of treatment.
On the basis of these criteria 43 patients were included in our study.
The data regarding the length of hospital stay and the numbers of operations for each type of burn (flame, scald, electricity) were obtained from the patient files. The total amount spent for each of these 43 patients was obtained from Gulhane Military Medical Academy accounts office. For each in-patient the amount includes: cost per occupied bed day, dressings, medicine and injection charges, lab tests and examination charges, blood and blood products, surgical treatment and associated material charges, meals and beverage charges, and special nutrition charges. The amounts paid to the hospital accounts office were in Turkish lire and were converted to US dollars at the current exchange rate. The cost of drugs, blood, and blood products which were not provided by our hospital were calculated by determining the bills and prescriptions in the patients’ files. The amount of these payments was also changed to American dollars and added to the hospital bill.
The results of the data were gathered when data collection was complete and tested by statistical analyses. All analyses were undertaken with SPSS for Windows ver.15.0 statistical software. In order to compare variables such as hospital stay, operation numbers, and costs in relation to specific burn types, the Kruskal-Wallis variant test was used. The Bonferroni-adjusted Mann-Whitney U-test was used to identify the differences between the variables, and a p value below 0.05 was regarded as statistically significant.
Results
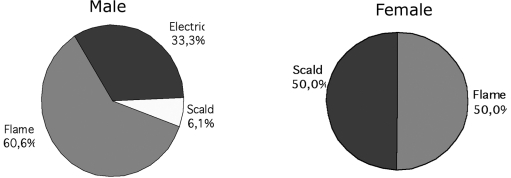
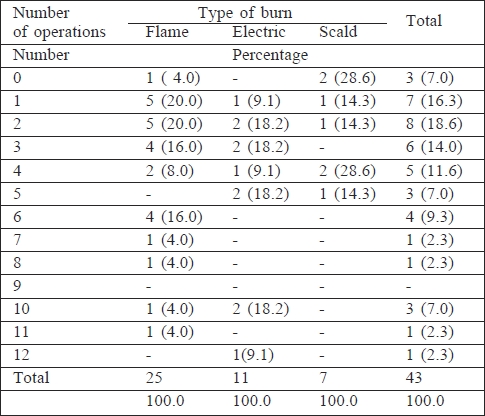
Of the 43 patients, 33 were men (76.7%) and 10 were women (23.3%). The patients’ ages ranged from one to 54 years old. The mean age was 26.76 ± 13.81 years for men and 28.60 ± 16.53 years for women. Distribution of patients’ sex in relation to the type of burn is shown in Fig. 1. The mean number of operations was 4.2 ± 1.9. Electricity burns required more operations than other types of burn while scald burns needed fewer. The difference between the number of operation required in relation to burn types was not statistically significant (p > 0.05). Details of operation numbers are presented in Table I.
Fig. 1. Sex distribution in relation to type of burn.
Table I. Number of surgical operations in relation to type of burn.
The average number of days of hospital stay was 73 ± 33 days. Statistical correlation between the days of hospital stay and burn type was borderline (p = 0.053). The Bonferroni-adjusted Mann-Whitney U-test was used to identify the source of this correlation. The statistical correlation between the days of hospital stay after an electricity burns and after scald burns was borderline (p = 0.020). Although patients with electrical burns stayed longer in hospital than patients with other types of burn injury, we did not find any statistically significant correlation (p > 0.05). The details regarding duration of hospital stay are given in Table II.
Table II. Duration of hospital stay in relation to type of burn.
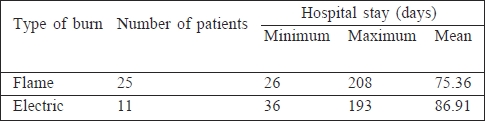
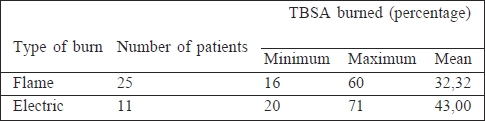
Each one per cent of burn corresponded to a mean hospital stay of two days. The various durations of hospital stay were respectively 1.3 days, 2.3 days, and two days. The difference between burn types with regard to stay per 1 of burn surface area was not statistically significant (p > 0.05). The average TBSA burned was 36 ± 7%. The average TBSA burned was highest in electrical burns and almost equal in scald burns and flames. There was no statistically significant difference with regard to TBSA and burn type (p > 0.05) (Table III).
Table III. Total body surface area burned in relation to type of burn.
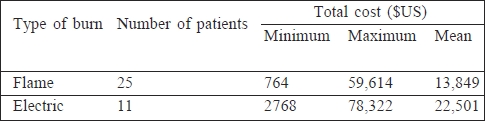
The overall mean total cost was $US 15,250 US dollars. The mean total cost of flame burns was $US 13,849 ± 16,523. The mean total cost of electricity burns was $US 22,501 ± 24,039. The mean total cost of scald injuries was the lowest ($US 8894 ± 5694). Even if electricity burns cost a considerable sum, we did not find any statistically significant differences between the burn types (p > 0.05) (Table IV).
Table IV. Total cost in relation to type of burn.
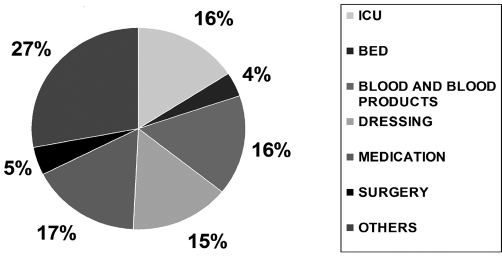
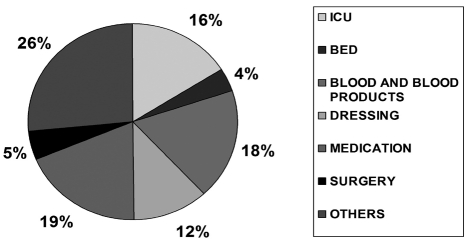
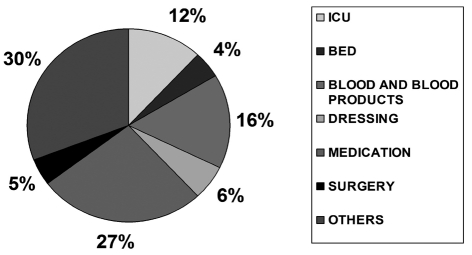
The Intensive Care Unit (ICU), blood, blood products, and medication were the main cost drivers. The cost drivers are presented in charts for each burn subgroup (Figs. 2 - 4).
Fig. 2. Distribution of cost drivers in flame burns.
Fig. 4. Distribution of cost drivers in scalds.
Fig. 3. Distribution of cost drivers in electric burns.
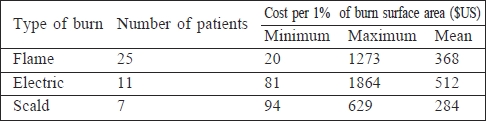
The patients paid on average $US 426 per day. The costs of each one per cent burned of TBSA were respectively $US 368, 512, and 284 for flame, electrical, and scald burns. We did not find any significant statistical difference in cost between burn for each one per cent (p > 0.05). The details of cost per one per cent are shown in Table V.
Table V. Cost per one per cent of burn surface area in relation to type of burn.
Discussion
The costs associated with burn injury are higher than those of some other well-known health-related problems such as stroke and AIDS in industrial countries.6,7 The essential point of cost analysis is to establish adequate detailed registering and archiving of patient files, which should include details of operations, drug orders, and complications as well as basic baseline demographic and injury characteristics. We used the hospital patient administration system based on the ICD code, i.e. the International Classification of Diseases, or more specifically the International Statistical Classification of Diseases and Related Health Problems) code and our burn centre archive. Several studies have been conducted based on the ICD code system, the national code system, etc.8,9
Determining the payer’s status is another important component of cost studies. We treated 300 acute major burn patients from March 2005 to August 2008. We could include only 43 of these patients because hospitalization costs for soldiers in our hospital are covered by the Turkish Military Forces. There was no hospital discharge bill for these patients to include in this study. We conducted the study using the records of patients whose discharge bill they paid themselves. Every country has its own social insurance system. Hospital reimbursement for burns treatment is different from country to country. Even within one country, different social insurance systems can reimburse different amounts for the total hospitalization of burn patients. In Turkey reimbursement for burns is usually not sufficient to cover all hospital costs related to acute burn therapy. The total amount spent, as reported by the accounts office at Gulhane Military Medical Academy, reflects only partial cover of the actual cost. This constitutes a handicap for our study.
Several cost methodologies exist, such as direct or indirect cost via the Human Capital theory.3,4 Direct cost is related to hospital cost. Indirect costs, including loss of working days, reflect the burden of burns on society. Since ours is a military hospital, most of the patients’ hospital costs are covered by the military forces’ budget. We therefore conducted a direct cost analysis, aiming to form a financial perspective rather than give the exact cost of burns. In the process we compared our results with those present in the literature.
The overall mean total cost was $US 15,250 per patient. This total cost is at variance with other reports in the literature. Loftus found a cost of $US 46,069 per patient and other studies produced different total costs.8-10 Hemington- Gorse et al. found the cost per in-patient for five days’ admission to be €16,705 ($US 22,329).7 Onarheim et al. found that the direct cost of each in-patient, with a mean total period of hospitalization of 11.3 days, was €11,800 ($US 15,772). The variance among the costs of the various items affects the final costs and creates the differences between studies. The use of certain specific highcost items such as skin substitutes considerably affects the total that is directly spent. The total spent can be five times that of the conventionally treated patient.8 We found that ICU charges, blood and blood products, medication, and generic charges were the main cost drivers in total burn costs. Patil found the mean daily cost of ICU treatment to be Australian $700.74.11 The average cost in US$ per patient day in UK was $1512, in France $934, in Germany $726, and in Hungary $280.12 Total burn cost can be reduced by avoiding unnecessary ICU bedding. Patil defined blood and blood products as a hidden cost driver,11 but we found this driver to be a distinctive cost item, especially in major burns, as Eldad also found.13 Effective management of blood and blood products can help in reducing burn costs. Medication, especially antibiotics, increases total burn costs. This major cost driver can be reduced by controlling the use of antibiotics. Surgical treatment, in contrast, accounted for only 5% of the total cost. Dressing changes cost more than surgical treatment, and the use of appropriate dressings can reduce the cost of using this item.14
The recommended duration of hospital stay in a burn centre is one day per 1 TBSA.15 In our study it was two days. Major burn injuries usually require surgical interventions such as serial debridement, skin grafting procedures, and local or free flap surgery. Such operations directly affect the length of hospital stay. The depth of burn injuries is another determinant of both cost and duration of hospital stay. Scalds usually cause superficial burns rather than other types of burn and therefore need fewer operations and a shorter hospital stay. Electrical injuries, in contrast, involve burns requiring surgery to remove damaged muscle or even amputation, which means additional operations and an extension of hospital stay.
Several studies have been published about the cost of scalds, which are preventable and mostly seen in the paediatric population.16,17 Griffiths et al. investigated the financial costs of paediatric scald burns and found a cost of £1850 per case with less than 10 TBSA burns.16 This contrasts with the mean total cost of scalds in our study, which was $US 8894. The cost per one per cent was therefore $US284. The burn surface areas in our patients varied between 17 and 60% with a mean of 32% TBSA. The percentage of burn surface area is a critical determinant of total hospital cost, because of high-cost dressing needs.
We applied statistical analysis to this study, the results of which revealed high standard deviation values for each variable. The high standard deviation values indicate that the data of each variable are spread out over a large range of values. Our study was retrospective and the patient population sample was not uniform. For example, the total spent on two patients with same burn type and percentage varied because of the burn’s depth and localization. The use of non-conventional treatment modalities such as skin substitutes and flap surgery requires separate calculation on an individual patient basis.8 It is very hard to apply statistical analysis in such studies.
Conclusion
This study showed that the calculation of the cost of acute burn injury was more difficult than it may seem. Adequate archiving of patient records must be the first step taken by a newly established burns centre for cost analysis studies. To reflect the real cost of burns, the accounts offices in burns centres and hospitals should have all the patients’ hospital bills, regardless of payer status. The type of study (direct, indirect...) should be determined with this purpose in mind. It should be borne in mind that even if the results of cost analysis studies may vary they nevertheless must be performed in every newly established burns centre in order to form an accurate financial overview.
References
- 1.Wheeler J.R., Van Harrison R., Wolfe R.A. et al. The effect of burn severity and institutional differences on the costs of care. Med Care. 1983;31:1192–1203. doi: 10.1097/00005650-198312000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Torrati F.G., Rossi L.A., Ferreira E., Dalri MCB M.C.B. et al. Analysis of cost of dressing in the care of burn patients. Burns. 2000;26:289–293. doi: 10.1016/s0305-4179(99)00132-1. [DOI] [PubMed] [Google Scholar]
- 3.Klarman H.E., Francis J., Rosenthal G.D. Cost-effectiveness analysis applied to the treatment of chronic renal disease. Med Care. 1968;6:48–54. [Google Scholar]
- 4.Robinson J.C. Philosophical origins of the economic valuation of life. Milbank Quarterly. 1986;64:133–155. [PubMed] [Google Scholar]
- 5.Açikel C., Eren F., Çeliköz B. Bir Yanik Ünitesinde Yatarak Tedavi Edilen Akut Yanikli Hastalarin Maliyeti. Türk Plast Rekonstr Est Cer Derg. 2002;10:186–189. [Google Scholar]
- 6.Lopez Bastida J., Serrano Aguilar P., Monton A. et al. The economic burden of stroke in Spain. Value Health. 2003;6:615–615. [Google Scholar]
- 7.Lopez Bastida J., Oliva Moreno J., Perestelo Perez L. et al. Determinants of health care costs in ambulatory patients living with HIV/AIDS. Value Health. 2005;8:A23–A23. [Google Scholar]
- 8.Onarheim H., Jensen S.A., Rosenberg B.E. et al. The epidemiology of patients with burn injuries admitted to Norwegian hospitals in 2007. Burns. 2009;35:1142–1146. doi: 10.1016/j.burns.2009.06.191. [DOI] [PubMed] [Google Scholar]
- 9.Hemington-Gorse S.J., Potokar T.S., Drew P.J. et al. Burn care costing: The Welsh experience. Burns. 2009;35:378–382. doi: 10.1016/j.burns.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Loftus J. Cost analysis of a major burn. NZ Med J. 1991;104:488–490. [PubMed] [Google Scholar]
- 11.Patil V., Dulhunty J.M., Udy A. et al. Do burn patients cost more? The intensive care unit costs of burn patients compared with controls matched for length of stay and acuity. J Burn Care Res. 2010;31:598–602. doi: 10.1097/BCR.0b013e3181e4d6a4. [DOI] [PubMed] [Google Scholar]
- 12.Negrini D., Sheppard L., Mills H. et al. International Programme for Resource Use in Critical Care (IPOC) - a methodology and initial results of cost and provision in four European countries. Acta Anaesthesiol Scand. 2006;50:72–79. doi: 10.1111/j.1399-6576.2006.00901.x. [DOI] [PubMed] [Google Scholar]
- 13.Eldad A., Stern Z., Neuman R.A. et al. The cost of an extensive burn survival. Burns. 1993;19:235–238. doi: 10.1016/0305-4179(93)90157-4. [DOI] [PubMed] [Google Scholar]
- 14.Atiyeh B.S., Dham R., Kadry M. et al. A benefit-cost analysis of moist exposed burn ointment. Burns. 2002;28:659–663. doi: 10.1016/s0305-4179(02)00075-x. [DOI] [PubMed] [Google Scholar]
- 15.Gillespie R., Carrol W., Dimick A.R. et al. Diagnosis-related groupings (DGRs) and wound closure: Round table discussion. J. Burn Care Rehabil. 1987;8:199–209. doi: 10.1097/00004630-198705000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Griffiths H.R., Thornton K.L., Clements C.M. et al. The cost of a hot drink scald. Burns. 2006;32:372–374. doi: 10.1016/j.burns.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 17.Shields B.J., Comstock R.D., Fernandez S.A. et al. Healthcare resource utilization and epidemiology of pediatric burn-associated hospitalizations, United States 2000. J Burn Care Res. 2007;28:811–826. doi: 10.1097/BCR.0b013e3181599b51. [DOI] [PubMed] [Google Scholar]