Summary
Burns of the front of the chest and abdomen and sometimes the front of the neck and axilla, mostly caused by flame in domestic accidents, are very common in Egypt. If deep, these burns can produce breast deformity in females either in childhood or in adolescence. This work considers 74 female breasts in 55 patients who had post-burn breast deformities due to accidents in childhood or early adulthood. The patients’ median age was 21 years (range, 13 to 42 years). The cause was scalding in 18 patients and flame in 37. The following conditions were found: upward contracture in 26 breasts (35%), 21 patients; downward contracture in 32 breasts (43%), 25 patients; and loss or distortion of the nipple/areola complex in 16 breasts (22%), 9 patients. Surgical correction included: Z-plasty, scar revision, scar excision and reconstruction by local flap or skin graft, and use of tissue expanders. Adequate projection of the reconstructed breast with the creation of a normal-looking inframammary fold was obtained. There were no major complications. Two patients had partial skin loss of the split-thickness graft, and partial loss of edges of the areola occurred in three cases. The burns thus caused various degrees of breast deformity and the corrective surgery varied accordingly. It is concluded that in such cases the general rules of scar revision have to be applied, correcting the contracture by Z-plasty or else by a local flap, if available, or by a split-thickness graft if the surrounding area is affected by post-burn scarring or if a large defect appears after complete release. Tissue expanders play a role in some if the scar area is surrounded by normal healthy tissue.
Keywords: BREAST DEFORMITY; BURN, RECONSTRUCTION
Abstract
Les brûlures de l’aspect antérieur du thorax et de l’abdomen et parfois de l’aspect antérieur du cou et des aisselles, causées dans la majorité des cas par les flammes surtout dans les accidents domestiques, sont très communes en Egypte. Ces brûlures, si profondes, peuvent produire une déformation au sein chez les femmes, soit en enfance soit en adolescence. Les Auteurs prennent en considération 74 seins féminins dans 55 patientes qui ont subi une déformation post-brulure au sein à cause d’un accident pendant l’enfance ou les premières années de l’âge adulte. L’âge médian des patientes était de 21 (variation, de 13 à 42 ans). Dans 18 patientes la cause a été l’ébouillantement et dans 37 la flamme. Les patientes présentaient les conditions suivantes: contracture en haut, 26 seins (35%), 21 patientes; contracture en bas, 32 seins (43%), 25 patientes; perte ou distorsion du complexe mamelon/aréole, 16 seins (22%), 9 patientes. La correction chirurgicale comprenait la plastie en Z, la révision de la cicatrice, l’excision de la cicatrice et sa reconstruction par lambeau local ou greffe cutanée, avec l’utilisation de prothèses d’expansion. Il a été possible d’obtenir une projection adéquate du sein reconstruit, avec la création du pli mammaire. Aucune complication majeure ne s’est vérifiée. Deux patientes ont subi la perte partielle de la greffe cutanée d’épaisseur variable et en trois cas il y a eu la perte partielle des bords de l’aréole. Les brûlures ont donc causé des malformations plus ou moins importantes et les techniques chirurgicales de correction changeait en fonction de ces variations. Les Auteurs concluent que dans ces cas il faut suivre les règles générales de la révision des cicatrices, c’est-à-dire corriger les contractures moyennant la plastie en Z ou un lambeau local, si disponible, ou avec une greffe à épaisseur variable si la zone corporelle adjacente est atteinte de cicatrisation post-brulure ou si un grand défaut se manifeste après la libération complète. Les expanseurs tissulaires jouent un rôle dans certains cas si la zone cicatricielle est entourée de tissus normaux sains.
Introduction
Burns of the anterior chest wall can cause significant distortion to the developing breast. Whenever the breast analogue has been damaged, varying degrees of malposition or apparently smaller size may occur. The breast bud is very rarely damaged by the skin burn of the chest wall. Loss or distortion of the areola and nipple complex due to burn does not necessarily indicate that the underlying gland will not develop or that lactation will not occur after pregnancy. 1 The deformed breast already represents a serious aesthetic impairment for the patient which can result in corresponding emotional trauma. Surgical intervention may therefore be indicated for functional, aesthetic, and emotional reasons, which may often overlap.2 The burn may hide the breast underneath owing to tight scarred skin but is rarely the cause of a smaller breast.
A wide range of procedures has been described to deal with these problems. The techniques include scar excision, release and skin grafts, skin graft with post-operative splint or a silicone conformer, single or multistage skin flaps from the surrounding available normal skin, latissimus dorsi myocutaneous flap with or without implant, expanders, and implants.3 The repair procedure should not be performed until breast development is reasonably well advanced for fear of causing further destruction.4
Patients and methods
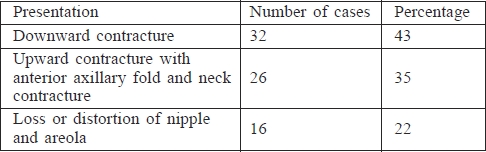
Between May 2004 and January 2009, a study was conducted of 74 breasts in 55 female patients presenting post-burn breast deformity dating from childhood or early adulthood. The surgical procedures were carried out at Minia and Assiut University Hospitals and the Assiut Burn Centre in Egypt. The patients’ median age was 21 years, ranging between 13 and 42 years. All the patients provided a complete history and were subjected to routine clinical, local, and general examinations and laboratory investigations. Scalding was the cause in 18 patients and 37 had flame burns. The customary written consent was obtained from all patients after explanation of the procedure. The different presentations of the patients were as follows: upward contracture with anterior axillary fold and neck contracture, 26 breasts (35%), 21 patients; downward contracture due to abdominal wall flame burn, 32 breasts (43%), 25 patients; loss or distortion of nipple/areola complex, 16 breasts (22%), 9 patients (Table I).
Table I. The various presentations.
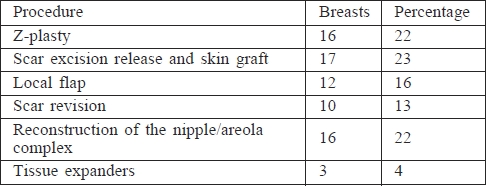
All the patients were operated upon under general anaesthesia. The procedures performed were the following: multiple Z-plasty, 16 breasts (22%); release and skin graft, 17 breasts (23%); release and reconstruction by local flap from the abdominal wall, 12 breasts (16%); scar revision, 10 breasts (13%); reconstruction of nipple/areola complex, 16 breasts (22%); and use of tissue expanders, 3 breasts (4%) (Table II).
Table II. The various procedures.
The technique of nipple reconstruction by the windmill technique (adopted by Dipirro in 19705) The patient’s breast was examined to determine the area which contained the nipple sensation compared to the normal sensation in the healthy side. Modified (four rectangular flaps) star flaps were then designed to build up the nipple with excision of the scarred areas in between the flaps, and the resulting round raw area of the donor site of the flap was covered by a split-thickness skin graft which turned darker in time and became similar in appearance to the areola (Figs. 1 - 8).
Fig. 1a. Nipple reconstruction by excision of the four triangular areas, closure of the four rectangular flaps together, and splitthickness graft for the areola region.
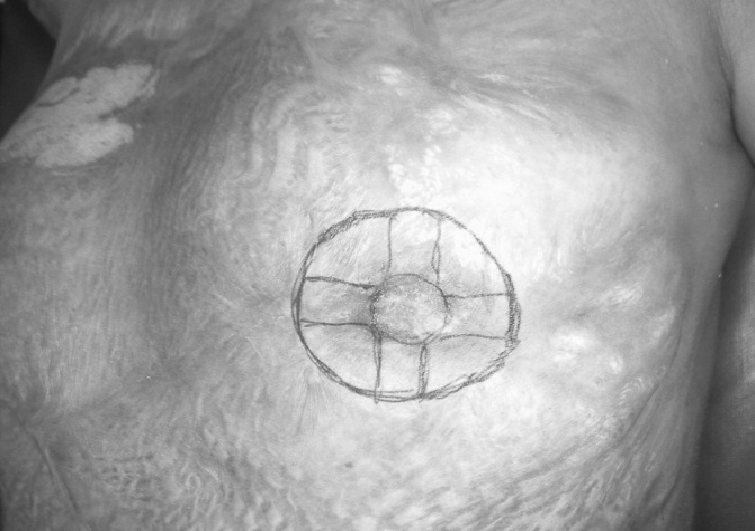
Fig. 8a. Downward displacement of the nipple/areola complex, and after release and skin graft.
Fig. 1b. Nipple reconstruction by excision of the four triangular areas, closure of the four rectangular flaps together, and splitthickness graft for the areola region.

Fig. 1c. Nipple reconstruction by excision of the four triangular areas, closure of the four rectangular flaps together, and splitthickness graft for the areola region.

Fig. 2a. Post-burn breast and axillary contraction after release by multiple Z-plasty.
Fig. 2b. Post-burn breast and axillary contraction after release by multiple Z-plasty.

Fig. 3a. Upward displacement of the nipple/areola complex and after release by multiple Z-plasty.
Fig. 3b. Upward displacement of the nipple/areola complex and after release by multiple Z-plasty.
Fig. 4a. Downward displacement of the nipple/areola complex and marking of new site.
Fig. 4b. Downward displacement of the nipple/areola complex and marking of new site.
Fig. 4c. Reconstruction by transposition flap with upward repositioning of nipple/areola complex.
Fig. 5a. Post-burn breast contraction + distortion of the nipple areola complex.

Fig. 5b. After release and reconstruction by rotational flap from the abdominal wall.

Fig. 6a. Post-burn breast contraction + obliteration of the inframammary sulcus.

Fig. 6b. After release and splitthickness skin graft.

Fig. 7a. Severe bilateral postburn contraction.
Fig. 7b. After release and splitthickness skin graft.
Fig. 8b. Downward displacement of the nipple/areola complex, and after release and skin graft.

The early and late post-operative results were evaluated, with the patients being questioned directly about their opinion on the result of the operation in the immediate post-operative phase and after six months, with the help of the pre-operative photographs. Z-plasty was used in 8 patients in the axillae to allow the breast to drop down to the level of the normal breast, and a transposition flap from the abdomen was used to slightly elevate the pulled down breast; the medial flap was axial based on the superficial superior epigastric artery and the lateral one was a random flap.
Results
The results of treatment in the early post-operative period and after 6 months were evaluated in order to establish a clear concept as regards the most appropriate treatment. This also served to provide patients’ response and their level of satisfaction. Adequate projection of the reconstructed breast, with the creation of a normal-looking inframammary fold, was obtained. There were no major complications (i.e., nipple loss, haematoma, infection, or major loss of skin flaps). Two patients had partial skin loss of the split-thickness graft, and partial loss of edges of the areola occurred in three cases. No blood transfusions were necessary in any case, and the estimated blood loss per case averaged less than 50 cc.
Discussion
Post-burn breast deformity sometimes follows extensive chest burns.6 Such burns cause various degrees of breast deformity and the surgical technique of correction varies in relation to these variations. The local fasciocutaneous flap is a good option in the treatment of post-burn breast deformities from both the patient’s and the surgeon’s point of view, as it gives better results and creates fewer complications. Also, it can be considered as a first-line choice if there is breast atrophy and a breast implant is to be inserted. 7 A sliding skin flap from the abdomen is based superiorly, laterally, or medially to the inframammary sulcus, at a level that allows the tissue to be brought upwards onto the chest wall according to need. This requires an ample blood supply, not a single vessel, from the two intricate networks of arteries that supply the anterior abdominal wall. This flap has given excellent results and offers two advantages: first, it builds up the inframammary line if this is lost as a consequence of the burn, and the second advantage is the gradual stretching of the overlying skin over the fixed inframammary fold, resulting in improvement of the fold.8
The general rules of scar revision should be applied in cases of post-burn breast deformity. The contracture should be released by Z-plasty if it is linear. A local flap, if available, should be used or a split-thickness skin graft if the surrounding area is affected by tight scarring hiding the breast or by leukoderma. In our patients we used various techniques according to the degree of breast deformity, so each case should be treated on its merits. Skin graft in the upper half of the breast offers a better prognosis than a graft in the lower half and the inframammary groove, which nearly always develops re-contraction. Graft hyperpigmentation usually improves after nearly a year. Tsoutsos et al. used artificial skin (Integra) together with tissue expanders in a multistaged procedure in the reconstruction of post-burn breast deformity in a single case with good results.9 However, Integra is very expensive for low- and middle-income countries.
Conclusion
Burns cause various degrees of breast deformity and the surgical technique of correction varies accordingly. The general rules of scar revision should be applied, correcting the contracture by Z-plasty or by local flap if available or split-thickness graft if the adjacent area is affected by post-burn scarring or if a large defect appears after complete release. Tissue expanders have a role to play in some cases if the scar area is surrounded by normal healthy tissue.
Acknowledgments
The authors have declared that there is no conflict of interest.
References
- 1.Kunert P., Schneider W., Flory J. Principles and procedures in female breast reconstruction in the young child’s burn injury. Aesth Plast Surg. 1988;12:101–101. doi: 10.1007/BF01576922. [DOI] [PubMed] [Google Scholar]
- 2.Bohmert H., Gabka C. In: Aesthetic Plastic Surgery of the Breast. 1. Bohmert Heinz, Gabka Christian., editors. Thieme Medical Publisher; 1997. [Google Scholar]
- 3.Garner W.L., Smith D.J. Reconstruction of burns of the trunk and breast. Clinics in Plastic Surgery. 1992;16:683–691. [PubMed] [Google Scholar]
- 4.Pensler J.M., Haab R.L., Parry S.W. Reconstruction of the burned nipple areola complex. Plast Reconstruct Surg, 1986;78:480–480. doi: 10.1097/00006534-198610000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Dipirro M.E., Dipirro E. Reconstruction of the nipple and areola after a burn: Case report. Plast Reconstr Surg. 1970;46:299–300. doi: 10.1097/00006534-197009000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Ozgur F., Gokalan I., Mavili E. et al. Reconstruction of post-burn breast deformities. Burns. 1992;18:504–509. doi: 10.1016/0305-4179(92)90186-x. [DOI] [PubMed] [Google Scholar]
- 7.Saker W.M. Local fasciocutanous flap in managing post-burn breast deformities. Egypt J Plast Reconstr Surg. 2002;26:233–239. [Google Scholar]
- 8.Vasconez L.O., Lejour M., Mabel G. Breast reconstruction with flaps. In: Vasconez L.O., Lejour M., Mabel G., editors. Atlas of Breast Reconstruction. 1. JB Lippincott Company; 1991. pp. 32–52. [Google Scholar]
- 9.Tsoutsos D., Stratigos A., Gravvanis A. et al. Burned breast reconstruction by expanded artificial dermal substitute. J Burn Care & Research. 2007;28:530–532. doi: 10.1097/BCR.0B013E318053DAC5. [DOI] [PubMed] [Google Scholar]











