Summary
Burn care is not reserved uniquely to burns. Several diseases have the symptomatology, clinical presentation, complications, treatment requirements, and outcome of burns. Such diseases are: 1. Stevens-Johnson disease; 2. Lyell’s syndrome; 3. bacterial fasciitis; 4. skin necrosis combined with coagulation disturbances; 5. pemphigoid; and 6. subacute cutaneous lupus erythematosus.
Keywords: diseases, mimicking, burn, treatment
Abstract
Les soins des brûlures ne sont pas limités uniquement aux brûlures. Il y a plusieurs maladies qui possèdent la symptomatologie, la présentation clinique, les complications, les exigences de traitement et les résultats des brûlures. Ces maladies sont les suivantes : 1. maladie de Stevens-Johnson ; 2. syndrome de Lyell ; 3. fasciite bactérienne ; 4. nécrose cutanée unie à des troubles de la coagulation ; 5. pemphigoïde ; 6. lupus érythémaeux cutané subaigu.
Introduction
Several skin lesions present like burns. Disruption of the skin layers or its blood supply due to any reason produces similar lesions that mimic a burn injury. Some of these diseases are Stevens-Johnson disease, Lyell’s syndrome, erythema multiforme, necrotizing fasciitis, automatic skin necrosis and coagulation disturbances (purpura fulminans, coumarin-induced skin necrosis syndrome), pemphigoid, and subacute cutaneous lupus erythematosus. All of these diseases affect the function and viability of skin and underlying tissues in a way resembling the loss of skin in burns. Patients suffering from any of these diseases should be admitted to a burn care unit (BCU). 1, 2
Burns-mimicking diseases
Stevens-Johnson disease
Stevens-Johnson disease presents as a hypersensitivity erythema with a sudden onset. It is characterized by erythematous, multicentric circular lesions also called “target lesions ”, which have a positive Nikolsky’s sign. It can involve all the body surface but is usually present in the hands, feet, and mucous membranes. The cause of Stevens- Johnson disease is unknown. 3Several viruses have been suspected, such as the herpes viruses, the Epstein-Barr virus, and HIV. 4The presence of a connective tissue disease, lymphoma, cancer, or Wegener’s granulomatosis would seem to be a frequent feature. The administration of certain drugs 5, 6, 7has been implicated as a cause of the disease (Figs. 1 , 2 ).
Fig 1.
Fig 2. Patient suffering from Stevens-Johnson syndrome.
Lyell’s syndrome - toxic epidermal necrosis
This condition also presents as a systemic toxicity syndrome with a sudden onset. The lesions are macular and have irregular limits and a darker centre. These lesions also have a positive Nikosky’s sign. The aetiology of the syndrome is likewise unknown but has an immunological basis and is provoked by drugs 8, 9, 10, 11(sulphonamide, anti-epileptic, allopurinol, penicillins, paracetamol), chemical agents, and Gram-positive toxins. There is a female-to-male predominance of 3 to 2 (Figs. 3 , 4 ).
Fig 3.
Fig 4. Patient suffering from Lyell’s syndrome.
Erythema multiforme
Erythema multiforme presents with symmetrical, target lesions without blisters and usually involves the extremities without mucosal lesions. It develops after an upper respiratory infection, otitis, herpes, or mucoplasma.
Necrotizing fasciitis
This condition presents as a necrosis of fascia and subcutaneous tissue and may involve muscle and overlying skin. 12, 13It is caused by Streptococcus, Staphylococcus, Enterococcus, Bacteroides, and clostridial bacteria.
Scalded skin syndrome
This is a syndrome mainly observed in infancy (Ritter’s disease) and childhood; the lesions are caused by intraepidermal splitting in the granular layer of the dermis. No epidermal necrosis is present, but it can be accompanied by blister formation with a positive Nikolsky’s sign. The cause is the exfoliative staphylococcal toxin.
Automatic skin necrosis / purpura fulminans / coumarin-induced skin necrosis
This form manifests itself with an acute haemorrhagic necrosis. It is provoked by dysfunction of the protein C anticoagulant system, antithrombin 3, and the factor V Leiden. It is inherited as an autosomal dominant trait and is idiopathic, with an incidence of 6% in our country (Greece). The causative agents are mainly drugs (non-steroid anti-inflammatory, antibiotics) or an acute severe infection (meningococci, staphylococci, streptococci, Rickettsia) (Figs. 5 , 6 ).
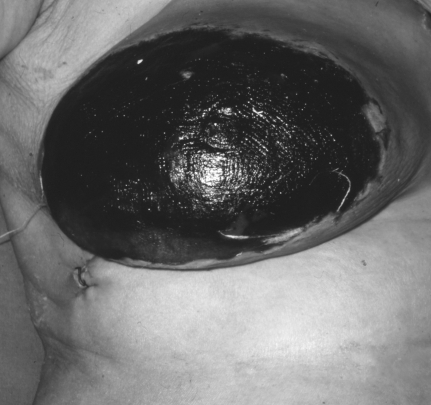
Fig 5.
Fig 6. Automatic skin disease.
Pemphigoid
This is primarily a dermatological disease. It presents with flaccid blisters and surrounding erythema and involves the mucosa. 14, 15Its aetiology has an immunological base, although drugs (penicillamine, captopril) and herpes virus infections have been accused.
Subacute cutaneous lupus
Skin involvement in lupus is well known. It presents with erythematous, round, scaling lesions involving the face, scalp, and mucosa; bullous lesions are rare. The aetiology is unknown, and there is a predominance of females over males. 16
Therapeutic approach
Hospitalization of these patients in a BCU provides the necessary environment, temperature (30-32 oC), humidity, and infrared lamps to prevent infection. Topical therapy should be applied as in burns. Depending on the pathology, drug therapy should be stopped, as in the case of Stevens-Johnson and Lyell’s syndrome (steroids, aciclovir, azathioprine), or initiated, as in the case of necrotizing fasciitis, scalded skin syndrome, and pemphigoid. Heparin and clotting factor replacement should be given in cases of purpura fulminans. Emergency escharotomy followed by surgery is mandatory in necrotizing fasciitis 17and in all diseases that cause full-thickness lesions. Plasmapheresis has been recommended in cases of pemphigoid and Lyell’s syndrome.
Discussion and conclusion
In such cases, high mortality and morbidity can be diminished by proper handling and hospitalization in a BCU. The lesions necessitate similar care to burns, along with fluid resuscitation and dietary instructions. Patients suffering from these diseases therefore benefit from admittance to a BCU, where they can receive topical and systemic therapy similar to that given to burns patients.
References
- 1.Trent J.T., Kirsner R.S., Romanelli P., Kerdel F.A. Use of SCORTEN to accurately predict mortality in patients with toxic epidermal necrolysis in the United States. Arch. Dermatol. 2004;140:890–2. doi: 10.1001/archderm.140.7.890. [DOI] [PubMed] [Google Scholar]
- 2.Cornish P., Mittmann N., Gomez M., Cartotto R.C., Fish J.S. Cost of medications in patients admitted to a burn center. Am. J. Clin. Dermatol. 2003;4:861–7. doi: 10.2165/00128071-200304120-00005. [DOI] [PubMed] [Google Scholar]
- 3.Stevens-Johnson syndrome and toxic epidermal necrolysis:Oncologic considerations. Clin. J. Oncol. Nurs. 2004;8:27–30. 55–55. doi: 10.1188/04.CJON.27-30. [DOI] [PubMed] [Google Scholar]
- 4.Stevens-Johnson syndrome after immunization with smallpox, anthrax, and tetanus vaccines. Mayo Clin. Proc. 2004;79:1193–6. doi: 10.4065/79.9.1193. [DOI] [PubMed] [Google Scholar]
- 5.Mockenhaupt M., Kelly J.P., Kaufman D., Stern R.S., SCAR Study Group. The risk of Stevens-Johnson syndrome and toxic epidermal necrolysis associated with nonsteroidal anti-inflammatory drugs: A multinational perspective. J. Rheumatol. 2003;30:2234–40. [PubMed] [Google Scholar]
- 6.Laffitte E., Nenadov Beck M., Hofer M., Hohl D., Panizzon R.G. Severe Stevens-Johnson syndrome induced by contrast medium iopentol (Imagopaque). Br. J. Dermatol. 2004;150:376–8. doi: 10.1111/j.1365-2133.2003.05763.x. [DOI] [PubMed] [Google Scholar]
- 7.Narayanan V.S., Mamatha G.P., Ashok L., Rajashekar N. Stevens-Johnson syndrome due to I.V. ceftriaxone - a case report. Indian J. Dent. Res. 2003;14:220–3. [PubMed] [Google Scholar]
- 8.Bygum A., Gregersen J.W., Buus S.K. Acetaminophen-induced toxic epidermal necrolysis in a child. Pediatr. Dermatol. 2004;21:236–8. doi: 10.1111/j.0736-8046.2004.21309.x. [DOI] [PubMed] [Google Scholar]
- 9.Schmutz J.L., Barbaud A., Trechot P. Toxic epidermal necrolysis and celecoxib (Celebrex). Ann. Dermatol. Venereol. 2004;131:107. doi: 10.1016/s0151-9638(04)93559-4. [DOI] [PubMed] [Google Scholar]
- 10.Aguiar D., Pazo R., Duran I., Terrasa J., Arrivi A., Manzano H., Martin J., Rifa J. Toxic epidermal necrolysis in patients receiving anticonvulsants and cranial irradiation: A risk to consider. J. Neurooncol. 2004;66:345–5. doi: 10.1023/b:neon.0000014538.31561.bc. [DOI] [PubMed] [Google Scholar]
- 11.Spornraft-Ragaller P., Ragaller M., Meurer M. Toxic epidermal necrolysis induced by NSAID. J. Rheumatol. 2003;62:474–5. doi: 10.1007/s00393-003-0535-6. [DOI] [PubMed] [Google Scholar]
- 12.Praba-Egge A.D., Lanning D., Broderick T.J., Yelon J.A. Necrotizing fasciitis of the chest and abdominal wall arising from an empyema. J. Trauma. 2004;56:1356–61. doi: 10.1097/01.ta.0000042157.00868.2e. [DOI] [PubMed] [Google Scholar]
- 13.Jensen S.L., Amato J.E., Hartstein M.E., Breer W.A. Bilateral periorbital necrotizing fasciitis. Arch. Dermatol. 2004;140:664–6. doi: 10.1001/archderm.140.6.664. [DOI] [PubMed] [Google Scholar]
- 14.Yasuda H., Tomita Y., Shibaki A., Hashimoto T. Two cases of subepidermal blistering disease with anti-p200 or 180-kD bullous pemphigoid antigen associated with psoriasis. Dermatology. 2004;209:149–55. doi: 10.1159/000079602. [DOI] [PubMed] [Google Scholar]
- 15.Yeh S.W., Usman A.Q., Ahmed A.R. Profile of autoantibody to basement membrane zone proteins in patients with mucous membrane pemphigoid: Long-term follow-up and influence of therapy. Clin. Immunol. 2004;112:268–72. doi: 10.1016/j.clim.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Perera G.K., Black M.M., McGibbon D.H. Bullous subacute cutaneous lupus erythematosus. Clin. Exp. Dermatol. 2004;29:265–7. doi: 10.1111/j.1365-2230.2004.01498.x. [DOI] [PubMed] [Google Scholar]
- 17.Catena F., La Donna M., Ansaloni L., Agrusti S., Taffurelli M. Necrotizing fasciitis: A dramatic surgical emergency. Eur. J. Emerg. Med. 2004;11:44–8. doi: 10.1097/00063110-200402000-00009. [DOI] [PubMed] [Google Scholar]