Summary
A detailed description, based on direct personal experience with burn patients, is provided of techniques for the prevention of scar contractures in various parts of the body
Keywords: rehabilitation, burned, patients, prevention, scarring
Abstract
Les Auteurs fournissent une description détaillée, basée sur leur expérience personale directe avec les patients brûlés, des techniques pour la prévention des contractures cicatricielles en diverses zones du corps.
Introduction
The prevention of scar contractures must be initiated in the acute phase, including:
– postural alignment, associated with the use of ortheses
– passive mobilization
Postural alignment
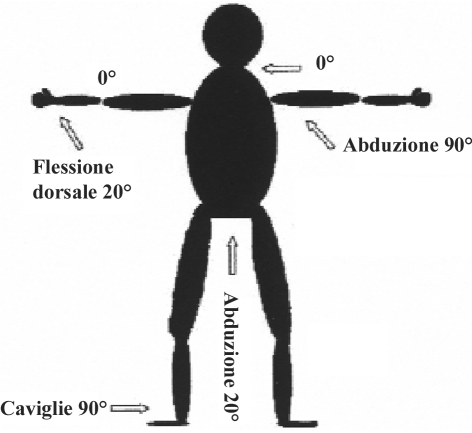
Fig. 1 illustrates the “theoretical” postural alignment proposed in the majority of texts dealing with burn patient rehabilitation. It is however our experience that it is no simple matter to achieve this ideal posture, unless we are handling a patient who is continuously sedated and immobile, and lying on a bed that is twice the normal size!
Fig. 1.
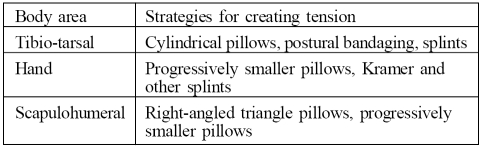
We will in particular consider here the three body areas that in our experience create the greatest problems. For each of them we will illustrate (see chart below) the strategies we use in our Department to create the correct tension in the body areas affected by the burn.
Table.
Tibio-tarsal
It is easy to maintain the tibio-tarsal joint at 90° ( Fig. 2 ) by creating a pillow to place at the foot of the bed ( Fig. 3 ) and using a special little arch to raise the sheets. If this is not enough to maintain the required posture, it may be useful to create a “posture medication” by establishing the position with adhesive bandages ( Fig. 4 ) or by making “stays” (using the same adhesive bandage or cloth strapping) that start from the head of the metatarsus and are anchored to the proximal third of the leg ( Fig. 5 ).
Fig. 2.
Fig. 3.
Fig. 4.

Fig. 5.
Scapulohumeral
When the upper limbs are affected, it may for various reasons be difficult to keep the shoulder abducted at 90° with the elbow and wrist extended - because of the edge of the bed, the absence of functional support, or the presence of cumbersome apparatus around the bed.
We can therefore attempt to achieve a compromise between ideal posture and what can actually be realized ( Fig. 6 ), using scalene right-angled triangular pillows that make it possible to position the shoulder (using a single device) at 90°, 60°, or at least 30° abduction, depending on the patient’s condition ( Fig. 7 )
Fig. 6.
Fig. 7.
To make this kind of pillow it is necessary place one on top of each other two layers of foam rubber (total thickness, c. 10 cm) and to cut these to the shape of the patient (Figs. 8 , 9 , 10 ).
Fig. 8.
Fig. 9.
Fig. 10.
These pillows must be used in association with progressively smaller pillows to support the hand and forearm and thus prevent shoulder intrarotation (Figs. 11 , 12 ).
Fig. 11.
Fig. 12.

The elbow can be held bent to 90°: in our experience contractures at this level are more easily reducible than contractures in the shoulder and hand.
In order to control contractures in the armpit, whether or not associated with contracting scars in the elbow, in the post-acute phase and the sequelae phase, we have used a commercially widely available articulated shoulder splint, with good patient compliance (Figs. 13 , 14 ).
Fig. 13.
Fig. 14.
Hand
In the hand it is absolutely imperative to prevent oedema from blocking it in a “negative position” - the ideal thing would be to construct as early as day 2 a splint made of some thermoplastic material (with multiperforations) in the safety position (intrinsic plus), with the metacarpo-phalangeals (MP) bent between 60 and 90°, the proximal and distal interphalangeals (PIP, DIP) extended, and the thumb in opposition ( Fig. 15 ).
Fig. 15.
To protect the skin as it is healing, in the absence of medication it is advisable to insert a thin layer of gauze between the skin and the splint; the splint is then fixed with an adhesive bandage and worn throughout the night and in all moments of inactivity during the day.
An orthesis, or splint, is a device applied over or around a weakened body segment to provide support and to increase or replace functional capacity. It can be:
static
progressive/static
dynamic
functional
The device is made using low-temperature thermoplastic materials, which offer the advantage of being light, washable, variable in thickness, perforated, and transparent to X-rays.
In burn patients the splint is necessary to:
ensure healing with the correct skin tension
counteract scar contractures
control scar hypertrophy (together with contact media)
substitute for active movements in the event of neuromuscular lesions
Close collaboration between physiotherapist and nurse is necessary both during the programming of the positioning and removal of splints and in the prevention of complications.
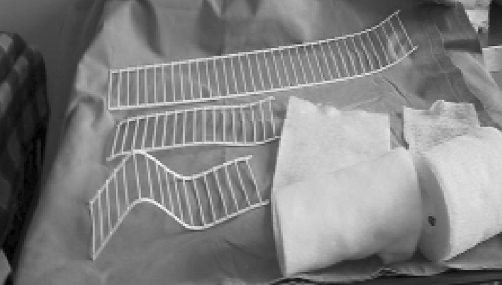
If thermoplastic splints are not available, it is possible to use Kramer splints, which have to be cut, modelled (MP bent between 90 e 60°, PIP and DIP extended), lined with gauze or cotton, and fixed in place with an adhesive bandage (Figs. 16 , 17 , 18 ).
Fig. 16.
Fig. 17.
Fig. 18.
It may be useful to make a series of progressively smaller pillows: starting with a strip of foam rubber approximately 10 cm wide, three progressively smaller segments are made which are placed one on top of the other and fixed in position with adhesive plasters or bandages ( Fig. 19 ). These are used with or without the above-described devices and make it possible to maintain the hand open and in the discharge position.
Fig. 19.
The making and positioning of the pillows are part of the physiotherapist’s and nurse’s joint tasks.
We will now briefly describe the correct position to prevent flexion contractures of the cervical rachis, which it is relatively simple to maintain in extension by placing a small cushion at the level of the scapulae ( Fig. 20 ) or by allowing the head to rest directly on the mattress. There may be some difficulty due to pain felt by the patient and to the presence of the tracheostomy. It is therefore important, at least during the day, not to place one or more pillows under the head of a patient with burns in the front of the neck.
Fig. 20.
Passive mobilization
With regard to passive mobilization in the acute phase, this must be performed:
analytically
slowly and steadily, starting from each single joint and then endeavouring to place the entire muscular chain in a state of tension
as often as possible during the day
during balneotherapy in a state of narcosis
The passive mobilization achieved during balneotherapy - all the better if associated with narcosis - enables the physiotherapist to evaluate the actual articular limitations: without medication and in the absence of pain (thus eliminating patient resistance), it is possible to achieve greater articular control.
Passive mobilization under narcosis requires maximum collaboration between nurse, physiotherapist, and anaesthetist ( Fig. 21 ).
Fig. 21.
In the post-acute phase the above programme is supplemented with some simple stretching exercises that the patient has to perform several times a day.
The fight against scar contractures continues and becomes more direct in the sequelae phase.
Let us recall that the evolution of a burn scar can be divided into an acute phase (2-6 months) and an evolutionary phase (12-24 months).
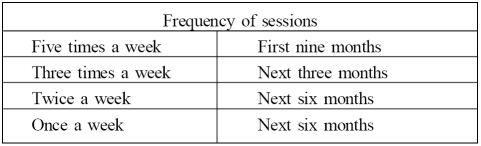
Treatment requires the preparation of a programme of daily sessions for about one year which progressively decrease in frequency the course of time (see chart below) and become routine follow-up checks until complete stabilization of the scar.
Problems in the sequelae phase include articular limitations, muscolo-tendinous contractures, muscular hypotrophy, and the formation of scar tissue.
The physiotherapist’s objectives in the sequelae phase are to:
– orient the scarring process
– prevent incorrect posture
– assist the patient’s return to normal social life
All this requires a personalized rehabilitation plan that takes into account age, sex, the features of the burn disease (depth, site, etc.), concomitant pathologies, and patient motivation.
In particular, our programme to combat scar contractures includes:
– massage with base cream
– passive kinesitherapy
– use of splints and bandages
– stretching exercizes
– posture re-education (“three-square” method)
– vacuum therapy
Massage
Massage is performed with light rubbing movements, using base cream with extreme gentleness; it is always associated with passive kinesitherapy ( Fig. 22 ).
Table.
Fig. 22.
Of the various techniques available we also use stretching and pressure, in the first phase of sequelae (until the scar shows the first signs of stabilization); in the very advanced phase of sequelae, we also use pétrissage, plastic massage, and pincer-rouler to work on deeper, more persistent formations.
Passive kinesitherapy
Passive kinesitherapy must be performed after the removal of coverings and garments, preceded by and applied together with massage with base cream and effected gently and slowly, starting from a single segment and terminating with the entire muscular chain in a state of tension (Figs. 23 , 24 , 25 , 26 ); it must be progressive and comply with the following criteria:
Fig. 23.

Fig. 24.

Fig. 25.

Fig. 26.
– beginning with reduced articular movement
– maintenance of position
– massage of scar
– gradual increase of articular range
It must be effected slowly, rhythmically, steadily, and evenly; the greater the contracture, the slower and more prolonged the degree of traction.
For passive mobilization to be effective, it is necessary to obtain the right tension in the right direction, in order to increase the length of the scar, achieving a fair balance between, on the one hand, patience, slowness, and respect of the tissues and the patient’s pain and, on the other, constancy, perseverance, continuity, and decisiveness. In our experience, it is better to avoid rapid or brusque mobilization that might lacerate the scar tissue and therefore interfere with the process of cicatrization.
Splints and bandages
To maintain the results of treatment sessions, it may prove useful to create a splint. In particular, in contracting scars affecting the back and the palm of the hand, we train the patient to alternate during the day the thermoplastic splint ( Fig. 27 ) (applied to create tension in the open position) and a basic fist bandage ( Fig. 28 ) made of adhesive bandaging (for the creation of tension in the clenched position).
Fig. 27.
Fig. 28.
Stretching
It is essential for the patient to learn how to perform at home a programme of lengthening and tension-creating exercises in body parts affected by scar contractures.
This programme must be constantly reviewed and adjusted by the physiotherapist in order to check the correct performance of the individual exercises and their suitability at that particular stage in the rehabilitation process.
“Three-square” method of posture re-education
This method is based on the procedures to place the body part in a state of global muscular tension using three postures ( Fig. 29 ):
Fig. 29.
– first patient supine with the other two at 90°
– second patient sitting with the trunk turned 90° to the other two
– third patient in state of tension with trunk bent 90°
Bolster pillows and support belts are used but are gradually eliminated. This method has been used in our facility for about six years in order to contain and progressively eliminate static postural irregularities, particularly in patients with trunk and armpit burns.
Vacuum therapy
This form of physical therapy is useful to counteract cicatricial adherences. It makes use of negative pressures ranging from 60 to 140 mBar. In our facility we use this technique as soon as the burn scar is less inflamed and the skin is less fragile. Application begins from healthy pericicatricial tissue and progressively spreads to other adjacent areas but avoiding any part that still looks very inflamed.
The time of application ranges from 5 to 15-20 min, depending on the extent and inflammatory state of the scar being treated. It is possible to use handpieces of various sizes ( Fig. 30 ).
Fig. 30.
Before treatment it is advisable to apply a thin layer of base cream or Vaseline oil in order to facilitate the movement of the heads of the device and to prevent unnecessary and harmful traumas ( Fig. 31 ).
Fig. 31.
Conclusion
In our experience, rehabilitative treatment, if correctly performed, can make contracting scar sequelae less invalidating, reduce to a minimum the number and the invasiveness of surgical operations in the burn sequelae phase, and favour the early return to normal social life of seriously burned persons.
References
- 1.Kottke F.J., Stillwell G.K., Lehmann J.F. In: "Trattato di terapia fisica e riabilitazione" chap. 50 translation 3rd American edition of “Handbook of Physical Medicine and Rehabilitation”. Verducci Editore., editor. Vol. 2 W.B. Saunders; Philadelphia: 1982. [Google Scholar]
- 2.Combi, Silvello, Torelli Donati, Baruffaldi, Preis. Le ustioni e il loro trattamento. B & G Editori; 1997. Trattamento riabilitativo del paziente ustionato. [Google Scholar]
- 3.Arena D., Giraudo L. Atti XIII Congresso Nazionale Società Italiana delle Ustioni La cicatrice patologica, Giuseppe De Nicola Editore, Naples. Giuseppe De Nicola Editore; Naples: 1998. L’allineamento posturale e la mobilizzazione del paziente ustionato in fase acuta. pp. 359–66. [Google Scholar]
- 4.Odoni R., Boero O., Conte S. Atti XIII Congresso Nazionale Società Italiana delle Ustioni La cicatrice patologica, Giuseppe De Nicola Editore, Naples. Giuseppe De Nicola Editore; Naples: 1998. Riabilitazione e splinting secondo il fisiatra. pp. 102–7. [Google Scholar]
- 5.Pajardi G., Foucher G., Buch N., Stutzmann S. “La rigidità della mano: chirurgia e ortesi”. Springer-Verlag Italia; Milan: 2001. pp. 11–11. [Google Scholar]
- 6.Giuliano L. La rieducazione della mano: aspetti generali. Dispensa per il terzo anno del Corso di laurea per Fisioterapisti, Università degli Studi di Torino. :13.
- 7.Arena D., Giraudo L., Conte S., Ottino O., Sarzi L. Rehabilitation of burn patients at the discharge stage: Our experience. Ann. Burns and Fire Disasters. 2003;16:144–5. [Google Scholar]
- 8.Corbara L., Biondo R., Freschi R., Monagheddu S. Atti XIII Congresso Nazionale Società Italiana delle Ustioni La cicatrice patologica. Giuseppe De Nicola Editore; Naples: 1998. Dalla dimissione da un centro Grandi Ustionati al raggiungimento della stabilizzazione degli esiti dell’ustione. Percorso riabilitativo. pp. 371–6. [Google Scholar]
- 9.Giancaspro M., Arena D., Verkimpe-Morelli N., Morelli U., Stella M., Bollero D. Il trattamento del paziente grande ustionato con la rieducazione posturale metodo “Les trois équerres”: proposta di protocollo operativo. Abstracts 15th Congresso Nazionale Società Italiana Ustioni,Rimini, April. 2002:38–38.
- 10.Verkimpe-Morelli N., Morelli U. Dispense del corso teorico pratico di rieducazione posturale “Metodo Les Trois Equerres”, Turin. 2002:13.
- 11.Magliacani G., Stella M., Castagnoli C. Atti XIII Congresso Nazionale Società Italiana delle Ustioni,La cicatrice patologica. Giuseppe De Nicola Editore; Naples: 1998. Classificazione delle cicatrici patologiche. pp. 68–68. [Google Scholar]
- 12.Stella M., Castagnoli C., Trombotto C., Calcagni M., Magliacani G., Teich Alasia S. Interrelationship between immunocompetent and structural cells in post-burn scars. Eur. J. Plast. Surg. 1998;21:8–13. [Google Scholar]
- 13.Marchi-Lipski F., Duviau F. Possibilità della cinesiterapia nelle cicatrici. “Medicina Riabilitativa”. Encycl. Med. Chir., Elsevier, Paris. 2004:26-275-A-10-6. [Google Scholar]
- 14.Corsi A., Grisolia G.A. Il trattamento degli esiti cicatriziali da ustioni con vacuumterapia: prime esperienze cliniche. Dispense del C.U. pediatrico, Ospedale Anna Meyer, Florence, s. d. :1–4.