Summary
After presenting an analysis of the principal antiseptics used for the local treatment of burns, highlighting their toxicity and the limitations of their antibacterial effectiveness, we describe the therapeutic protocol used in our burns centre (where antibacterial treatment consists exclusively of antibiotics for both local and systemic use). We review the data regarding actual and predicted mortality, and mortality due to septicaemia during the years 2000-2003.
Keywords: local, treatment, burns, antibiotics
Abstract
Les Auteurs, après avoir analysé les principaux antiseptiques utilisés pour le traitement local des brûlures et souligné leur toxicité et les limitations de leur efficacité antibactérienne, décrivent le protocole thérapeutique utilisé dans leur centre des brûlés (où le traitement antibactérien consiste exclusivement en des antibiotiques pour l’emploi local et systémique). Ils considèrent en outre les données sur la mortalité réelle et prévue, et la mortalité due à la septicémie pendant les années 2000-2003.
The toxicity and limitations of the antibacterial effectiveness of antiseptics
The debate on the use of antiseptics or antibiotics in the local antibacterial treatment of burns is still open. In general, it is believed that antibiotics are responsible for the selection of resistant strains, while the same cannot be said of antiseptics when both antibiotics and antiseptics are applied to lesions in insufficient concentrations. 1The current literature offers many studies on the toxicity and the limitations of the antimicrobial effectiveness of the principal antiseptics used until the present day.
For example, we know that in burns covering more than 20% of the total body surface area (TBSA), povidone iodine interferes with thyroid function and may cause metabolic acidosis owing to kidney poisoning, which can even be fatal. 2In addition, it cannot be used on “secreting” burns, since - being inhibited by organic substances (including blood) - it loses its antibacterial effectiveness.3 It may also not be active against “epidemic” methicillin-resistant Staphylococci aurei(E-MRSA) and Pseudomonas, as it is subject, among other things, to contamination by opportunistic pathogens of the Pseudomonadaceae family (Burkholderia Cepacia, formerly known as Pseudomonas Cepacia). 3, 4
With regard to mafenide acetate, we know that the inhibition of carbonic anhydrase that it causes at the level of the renal tubules leads to excretion of bicarbonate and chlorine, with consequent metabolic acidosis and compensatory hyperventilation. In the late 1970s higher mortality was reported in relation to respiratory complications following treatment of burns in over 30% TBSA. 5In the early 1970s descriptions began to appear of superinfections, due especially to Providencia Stuartii(Enterobacteriaceae), that were resistant to treatment with antibiotics. Superinfections caused by fungi were also observed. According to Monafo, these superinfections were the result of the considerable selection caused by routine use of mafenide acetate. 2
The history of the use of silver as an antiseptic in the treatment of burns since the mid-1960s until the present day is emblematic.
• Moyer, 1965 - silver nitrate (0.5% solution). We list below the main aspects of this solution:
1. Physiological (isotonic) solution cannot be used in the preparation as this would cause precipitation of silver chloride. However, distilled water makes 0.5% silver nitrate solution extremely hypotonic. This hypotonia causes the absorption of a large volume of water and the loss of sodium, chlorine, and potassium. The result is a marked hydroelectrolytic imbalance. 2
2. Many Gram-negative bacteria can reduce nitrate into nitrite, the absorption of which can occasionally cause methemoglobinaemia. The last case caused by silver nitrate dates back to 1968, 6although one new case has in fact been reported. 7
3. The medication covering the lesion must be moistened every 3-4 h and changed twice a day, which increases mechanical trauma for the patient and the nursing time. It would seem however that the effects on the reduction of the infections are due more to the frequent change in medication and the high level of cleanliness using this technique than to the actual use of silver. 8
• Fox, 1968 - silver sulphadiazine (2% cream). The main features of this antiseptic can be summarized as follows:
1. It is not to be used in patients with a G6PD deficit in whom the sulphamide component can cause haemolytic anaemia. 9
2. It is not to be used in patients who are sensitive to metals, in whom silver can cause allergic reactions. 10
3. There have been reports of medullary toxicity levels high enough to lead to temporary but severe leucopenia. 11
4. As long ago as 1980 it was believed to be responsible for plasmidic resistance to Enterobacteriaceae; 2in the same years (1978-85), plasmidic-type resistance to antibiotics following routine use was also found in strains of Pseudomonas aeruginosa. 8
5. It causes the formation of a moist, macerated, non-uniform eschar that promotes bacterial colonization in extensive burns and is difficult to treat surgically. 12
• Monafo, 1976 - silver sulphadiazine (1%) + cerium nitrates (2.2%) As silver sulphadiazine offered insufficient protection against the growth of Gram-positive bacteria in patients with extensive burns, a combination was introduced with cerium nitrate (a rare earth metal), in the belief that together the two substances might have a synergic effect. 13The results in the literature, however, are not consistent but contradictory, both in vitroand in vivo. 8, 12, 14One of the advantages is thought to be the hardening of the eschar due to the precipitation of calcium carbonate and phosphate caused by cerium. The calcification of the eschar would block bacterial colonization and also permit a long delay (8-12 weeks) before proceeding to surgery. 15But who is willing to wait all this time before operating on a major burns victim?
• Slow release silver (Acquacel Ag; Acticoat). Currently it is believed that silver, in the ionic form used in former formulations (Ag+), is deactivated by the organic fluids in the lesions and must therefore be frequently replaced. Thus, it is the constant replacement through frequent medications that ensures its effectiveness. The new formulations, in which silver is present in either ionic (Acquacel Ag) or nanocrystalline form, allow further release of silver when this is used up in the interaction with the lesion. The continuous release of silver makes it possible to leave the medication in situ for a few days (3 to 7), with decreased mechanical trauma for the patient and decreased nursing time. However, these procedures make it more difficult to inspect the lesion. 16Antibacterial activity towards E-MRSA, Pseudomonas aeruginosa, and Staphylococcus aureushas been reported. 1It is however too early to assess the effect on bacterial resistance, in view of its current non-routine use - the first study on the bacterial resistance caused by silver sulphadiazine appeared at least ten years after it began to be used, and for at least four years no such phenomena were reported. 8
Local treatment of burns with antibiotics
Our protocol for the local treatment of burns consists of bathing in running water with debridement (on hospitalization, frequently during the course of the disease, and before surgery) and successive medication with antibiotics for topical or systemic use. With regard to partial-thickness burns, the most frequently used routine treatments are with gentamicin, rifamycin S.V., and the chloramphenicol-collagenase association. A multi-centre study (conducted in 11 Italian burn centres) in the years 1992-1993, published in 1994, 17highlighted chloramphenicol’s absolute lack of antibacterial activity, meaning that when chloramphenicol is associated with collagenase it adds nothing to the latter’s activity (enzymatic debridement). Conversely, both gentamicin (which we use for brief periods and for exposed face burn treatment) and rifamycin S.V. (also used for brief periods and as a compress) maintain good antibacterial activity. Now, ten years after the above-mentioned study, a new multi-centre study would be very useful.
In full-thickness burns with necrotic eschar in elderly or diabetic patients, or when the location of the burn, its extent, and the patient’s general conditions are so compromised that surgical escharectomy is risky, we use salicylate Vaseline in various concentrations (5-20%), impregnated with antibiotics, applied through incisions in the eschar itself to facilitate penetration both in and under it. The initial choice of which antibiotic to add to the salicylate Vaseline for a specific patient is made on the basis of the results of the antibiograms carried out on germs isolated from the burns of patients hospitalized in the immediately previous period. Subsequently, the antibiotic can be used to which any germs isolated from the patient are sensitive. 18, 19
In full-thickness burns with granulating surfaces, before or during completion of surgical therapy, we use a fatty antibiotic-impregnated gauze as a compress, in relation to the antibiogram. During the process of becoming chronic, when there are limited residual areas of deepithelialization and/or infected granulation (generally by Staphylococcus aureus), these are treated with polyurethane foam (which associates debriding action with absorption of burn secretions) and with the antibiotic to which the germ has proved sensitive. As a final point, a gradual and predetermined release system has been devised that guarantees an antibiotic concentration which maintains aseptic conditions for five days following a single administration associated with keratinocyte sheets. The antibiotic we used, applied on a polymer coated with a drug-permeable membrane, was vancomycin, which thus proved to be non-toxic to cultured keratinocytes. 20, 21
Analysis of burn patient data in the period 2000-2003
Our analysis regarded patients of all ages and burned body surface areas hospitalized in our burns centre during the period 2000-2003.
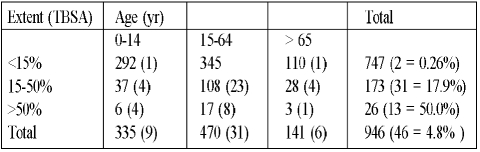
Table I presents the cases of septicaemia (in parentheses) as well as the total number of patients distributed by age and burn extent.
Table I. Distribution by extent/age in burn patients hospitalized in 2000-2003.
As can be seen, the number of cases of septicaemia - as might be expected - increased in relation to the extent of the burn.
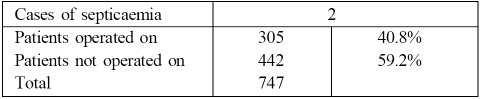
In particular, in the group of burns between 15 and 50% TBSA, the average burn surface was 35% (SD ± 10). Although the septicaemia rate (0.26%) in the group of patients with burns in less than 15% TBSA was predictably very low, about 40% of such patients were treated surgically because their burns, though limited in area, involved a higher risk of infection, as they were deep and subject to more intense manipulation ( Table II ).
Table II. Burns in <15% TBSA - distribution by surgical treatment.
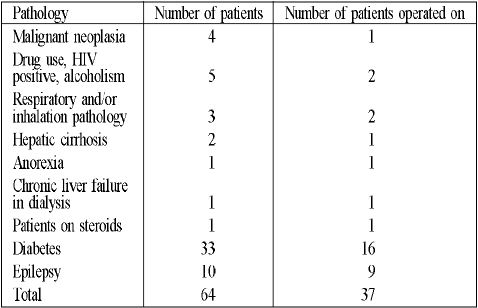
The patients subjected to surgery included many with pathologies favouring infection who presented a dual risk - there were altogether 64 of these immunodepressed patients (8.5%) ( Table III ).
Table III. Burns in <15% TBSA - distribution by pathologies with infective risk.
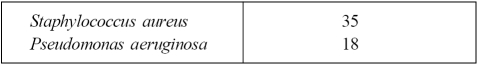
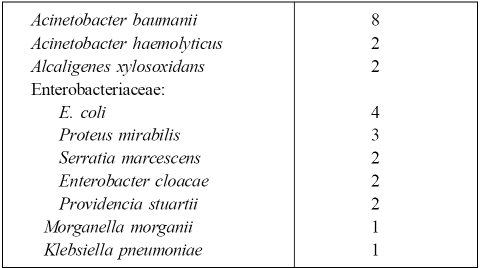
The main germs isolated from the blood cultures were, as might have been expected, Staphylococcus aureus and Pseudomonas aeruginosa ( Table IV ), accompanied by other Gram-positive ( Table V ) and Gram-negative ( Table VI ) germs, generally opportunistic pathogens, in cases of septicaemia that in the majority of cases were polymicrobial.
Table IV. Germs isolated from blood cultures.
Table V. Other Gram-positive germs isolated.
Table VI. Other Gram-negative germs isolated.
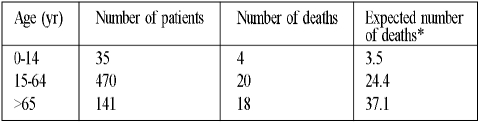
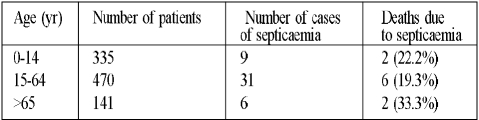
Table VII shows the distribution of deaths in relation to age and all burn percentages, with a comparison to predicted mortality (Probit analysis). As can be seen, the best results were obtained in the group of patients over 65 years old, with a reduction in the death rate of about 50%. Good results were also obtained in other age groups.22 To conclude ( Table VIII ), while not all deaths were caused by septicaemia, not all septicaemic patients died - among our cases septicaemia was not in fact the leading cause of death.
Table VII. Distribution in relation to death.
Table VIII. Septicaemia as a cause of death.
Conclusion
After bacterial colonization, infection, and sepsis of the burn area, septicaemia is the severest form of infection arising from contamination of a burn. This contamination, whether originating from the patient (skin, faeces, oropharynx, 16%) or from the environment, medical personnel, or other patients (84%), can be counteracted only by using various means at the same time. The principal means are the sterility of the environment and of the medications, the strengthening of the organism’s defence mechanisms, and surgical coverage of the burn surface.23 Among these remedies, pharmacological anti-infective treatment clearly plays an important role. This must make use of non-toxic material possessing an antibacterial effect that targets the micro-organism in question, in non-fluctuating concentrations at the level of the lesion and capable of encouraging selection of resistant micro-organisms. The analysis of the main antiseptics in use and the results we obtained as regards general mortality and secondary mortality due to septicaemia provide evidence of the advisability of continuing to use antibiotics in the local treatment of burns.
References
- 1.Dunn K., Edwards-Jones V. The role of Acticoat with nanocrystalline silver in the management of burns. Burns. 2004;30:S1–S9. doi: 10.1016/s0305-4179(04)90000-9. [DOI] [PubMed] [Google Scholar]
- 2.Monafo W.W., Ayvazian V.H. Terapia clinica. Clin. Chir. Nord Am. 1980;11:1288–1305. [Google Scholar]
- 3.Agolini G., Micali G., Raitano A. Antisettici e chemioterapici nella terapia topica delle ustioni. Riv. Ital. Chir. Plastica. 1998;30:233–67. [Google Scholar]
- 4.Nicoletti G., Nicolosi V.M. “Dizionario di batteriologia umana normale e patologica” (3rd edition) 1998. [Google Scholar]
- 5.Lloyd J.R. Ustioni: progressi nella terapia e prospettive di studio. Clin. Chir. Nord Am. 1978;10:133–52. [Google Scholar]
- 6.Winkley J.H., Weibel L., Davies W.D., Johnston M. Il trattamento locale delle ustioni. Clin. Chir. Nord Am. 1969;1:1416–25. [Google Scholar]
- 7.Trong-Duo Chou, Gibran N.S., Urdahl K., Lin E.Y., Heimbach D., Engrav L.H. Methemoglobinaemia secondary to topical silver nitrate therapy - a case report. Burns. 1999;25:549–52. doi: 10.1016/s0305-4179(99)00031-5. [DOI] [PubMed] [Google Scholar]
- 8.Klasen H.J. A historical review of the use of silver in the treatment of burns. II. Renewed interest for silver. Burns. 2000;26:131–38. doi: 10.1016/s0305-4179(99)00116-3. [DOI] [PubMed] [Google Scholar]
- 9.Eldad A., Neuman A., Weinberg A., Benmeir P., Rotem M., Wexler M.R. Silver-sulphadiazine-induced haemolytic anaemia in a glucose-6-phosphate dehydrogenase-deficient burn patient. Burns. 1991;17:430–2. doi: 10.1016/s0305-4179(05)80083-x. [DOI] [PubMed] [Google Scholar]
- 10.Fraser-Moodie A. Sensitivity to silver in a patient treated with silver sulphadiazine (Flamazine). Burns. 1992;18:74–5. doi: 10.1016/0305-4179(92)90128-h. [DOI] [PubMed] [Google Scholar]
- 11.Gamelli R.L., Paxton T.P., O’Reilly M. Bone marrow toxicity by silver sulphadiazine. Surg. Gynec. Obstet. 1993;177:115–20. [PubMed] [Google Scholar]
- 12.De Gracia C.G. An open study comparing topical silver sulphadiazine and topical sulphadiazine-cerium nitrate in the treatment of moderate and severe burns. Burns. 2001;27:67–74. doi: 10.1016/s0305-4179(00)00061-9. [DOI] [PubMed] [Google Scholar]
- 13.Monafo W.W., Ayvazian V.H., Skinner A.M. Control of infection in major burn wounds by cerium nitrate/silver sulphadiazine. Burns. 1976;3:104–7. [Google Scholar]
- 14.Di Francesco-Eklund F., Barisoni D. Sulfadiazina argento vs cerio sulfadiazina: studio batteriologico. Abstracts 12th Congresso Nazionale SIUST Catania. 1996
- 15.Boeckx W., Blondeel Ph. N., Vandersteen K., Dewolf-Peteers C., Schmitz A. Effect of cerium nitrate-silver sulphadiazine on deep dermal burns: A histological hypothesis. Burns. 1992;18:456–62. doi: 10.1016/0305-4179(92)90177-v. [DOI] [PubMed] [Google Scholar]
- 16.Montone A., Marianetti M. La medicazione delle ustioni dermiche con Acquacel Ag. Nostra esperienza. Wound Care Times. 2004;2:2–6. [Google Scholar]
- 17.Dioguardi , et al. Monitoraggio microbiologico del paziente ustionato e studio della citotossicità degli antisettici topici di più comune impiego clinico. Atti 11° Congresso Nazionale SIUST, Bari , November. 1994:13–38.
- 18.Masellis M. Association of salicylic Vaseline with antiseptics or antibiotics in topical treatment of burns. “Care of the Burn Wound”, International Congress, Geneva, 1983. 1985:1–6.
- 19.Napoli B., D’Arpa N., Iaia A., Sferrazza G., Masellis M. Antibiotic salicylate vaseline: A topical treatment of choice in burned diabetic patients? Annals of Burns and Fire Disasters. 1999;12:146–9. [Google Scholar]
- 20.Giannola L.I., De Caro V., Adragna E., Giandalia G., Giannola G., D’Arpa N., Napoli B., D’Amelio L., Genovese M., Lombardo C., Masellis M. Applicazione di un sistema di rilascio modificato contenente antibiotici associato a lamine di cheratinociti poste su pazienti ustionati. Part I. Atti 47° Convegno Nazionale SICPRE, Palermo September. 1998:9–12.
- 21.D’Arpa N., Napoli B., D’Amelio L., Genovese M., Masellis M., Giannola L.I., De Caro V., Adragna E., Giandalia G., Giannola G. Applicazione di un sistema di rilascio modificato contenente antibiotici associato a lamine di cheratinociti poste su pazienti ustionati. Part II. Atti 47° Convegno Nazionale SICPRE, Palermo September. 1998:13–15.
- 22.Rashid A., Khanna A., Gowar J.P., Bull J.P. Revised estimates of mortality from burns in the last 20 years at the Birmingham burns centre. Burns. 2001;27:723–30. doi: 10.1016/s0305-4179(01)00034-1. [DOI] [PubMed] [Google Scholar]
- 23.Barisoni D. “Le ustioni e il loro trattamento”. 1984. [Google Scholar]